Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Raghad AL-Ishaq | -- | 3240 | 2023-08-31 14:44:42 | | | |
| 2 | Jason Zhu | -287 word(s) | 2953 | 2023-09-01 07:33:49 | | | | |
| 3 | Jason Zhu | -16 word(s) | 2937 | 2023-10-19 04:56:51 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Al-Ishaq, R.K.; Kubatka, P.; Büsselberg, D. Sweeteners and Gut Microbiome. Encyclopedia. Available online: https://encyclopedia.pub/entry/48702 (accessed on 16 January 2026).
Al-Ishaq RK, Kubatka P, Büsselberg D. Sweeteners and Gut Microbiome. Encyclopedia. Available at: https://encyclopedia.pub/entry/48702. Accessed January 16, 2026.
Al-Ishaq, Raghad Khalid, Peter Kubatka, Dietrich Büsselberg. "Sweeteners and Gut Microbiome" Encyclopedia, https://encyclopedia.pub/entry/48702 (accessed January 16, 2026).
Al-Ishaq, R.K., Kubatka, P., & Büsselberg, D. (2023, August 31). Sweeteners and Gut Microbiome. In Encyclopedia. https://encyclopedia.pub/entry/48702
Al-Ishaq, Raghad Khalid, et al. "Sweeteners and Gut Microbiome." Encyclopedia. Web. 31 August, 2023.
Copy Citation
Worldwide, the demand for natural and synthetic sweeteners in the food industry as an alternative to refined sugar is increasing. This has prompted more research to be conducted to estimate its safety and effects on health. The gut microbiome is critical in metabolizing selected sweeteners which might affect overall health. Recently, more studies have evaluated the relationship between sweeteners and the gut microbiome.
sweeteners
non-nutritive sweeteners
steviol
saccharin
gut microbiome
1. Sweeteners and the Gut Microbiome
1.1. Steviol Glycoside
Stevia rebaudiana is a shrub found mainly in South America, specifically in Brazil and Paraguay [1]. It belongs to the family Asteraceae, and it is used as a natural and non-caloric sweetener because of its high sweetness intensity, which is caused by steviol glycosides [2]. Purified steviol glycoside extracts have been used in the food industry as sweeteners in many regions [3]. The European Food Safety Authority (EFSA) thus reported the acceptable daily intake of steviol glycosides to be 4 mg/kg/day [4][5]. The leaves of Stevia rebaudiana contain several diterpene glycosides, such as rubusoside and steviolbioside [6]. Multiple in vitro studies have supported the metabolization of stevia extracts by the gut microbiome [7]. Bacteroides species in the gut play an important role in metabolizing two of the main components of Stevia rebaudiana by hydrolyzing rebaudioside A and stevioside to steviol in the gut [8]. This suggests that neither component is absorbed in the upper gastrointestinal tract [9]. Using the portal vein, the absorbed steviol reaches the liver for further metabolism to steviol glucuronide and is excreted in the urine [10].
1.2. Glycyrrhizin
One of the 300 active licorice compounds is glycyrrhizin, a triterpene saponin glycoside [11]. It is used as an herbal product in medicine due to its anticancer and anti-inflammatory activities [12]. It has a high sweetness intensity (up to 200 times sweeter than sucrose) [13]. Ingestion of less than 100 mg/day of glycyrrhizin is considered safe [14]. Due to its poor oral bioavailability, glycyrrhizin is metabolized by the gut microbiome [15]. Both Eubacterium and Bacteroides species are involved in the de-glycosylation of glycyrrhizin to a major product, glycyrrhizic acid, and a minor product, 18β-glycyrrhetic acid 3-O-monoglucuronide [16]. After that, both products reach the liver for further conjugation and reduction [17]. Both biliary and urinary excretions occur to the major parts of the products, respectively [18].
1.3. Neohesperidin Dihydrochalcone
Neohesperidin dihydrochalcone (NHDC) is a natural sweetener found mainly in the skin of citrus fruits; it possesses high stability and solubility [19]. It is obtained and processed from its parent flavanone, neohesperidin, and has a sweetness intensity 250–1800 times higher than sucrose [20]. Despite that, the usage of NHDC as a replacement for sucrose is limited in the food industry due to its flavor formulation, texture, and size [21]. Although not widely known, the metabolism of NHDC by the gut microbiome has been discussed in the literature [22]. The metabolism starts with NHDC being deglycosylated to hesperidin dihydrochalcone 4′-β-glycoside, transforming into an aglycone. The final step of NHDC metabolism is the hydrolysis of the aglycone to propionic acid and phloroglucinol [23]. The products are then excreted either through urine or bile [24]. Figure 1 and Figure 2 summarize and provide an overview of the three natural sweeteners and their metabolism by the gut microbiome.
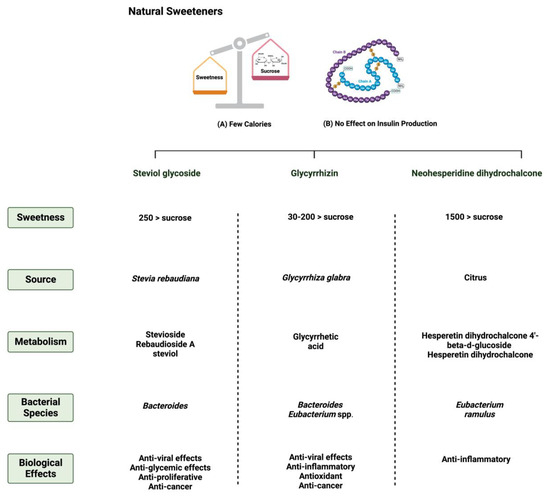
Figure 1. Overview illustration of natural sweeteners. The figure describes two of the main features of natural sweeteners. It also shows the sweetness intensity, the source of natural sweeteners, their metabolism by the gut microbiome, and their main biological effects. Created with BioRender.com (accessed on 15 July 2023).
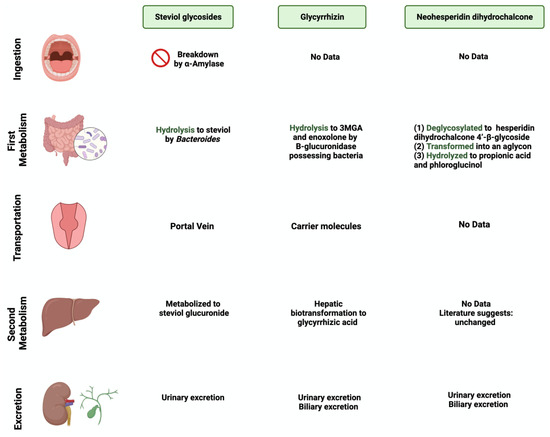
Figure 2. Overview illustration of natural sweetener consumption and metabolism. The figure is divided into different sites of metabolism for each of the natural sweeteners. Created with BioRender.com (accessed on 15 July 2023).
1.4. Saccharin
Saccharin (1,1-dioxo-1,2-benzothiazol-3-one), also known as E954, is a non-caloric sweetener used widely in the food industry [25]. It is found either in an acid form or bound to calcium or sodium (higher stability and solubility) [26]. Saccharin’s sweetness intensity is 300 times higher than sucrose [27]. The FDA considers saccharin consumption to be safe due to its inability to be metabolized by the body [28]. Once consumed, most of the ingested saccharin (85–95%) is absorbed and bound reversibly to plasma proteins when excreted in the urine. The rest passes through the GI tract to be eliminated, unchanged, in the feces [9]. Due to this, studies have investigated the influence of saccharin on gut microbiome composition. The administration of 90 mg of saccharin in rats did not alter the total number of anaerobic bacteria, but eliminated specific anaerobic groups in the cecal contents [29].
Additionally, rats receiving a 2.5% dose of saccharin inhibited the growth of three Escherichia coli strains and three Lactobacillus species [30]. These studies may suggest that even if the body does not metabolize the sweeteners, their consumption impacts the gut microbiome’s composition and function, which might alter the host’s health status. However, recent studies using advanced technologies are required in order to assess saccharin’s safety and effectiveness and to address the controversial results in the literature.
1.5. Sucralose
Sucralose, or E-955, is a low-caloric, non-nutritive synthetic sweetener and is very similar in structure to sucrose [31]. However, sucralose is formed when the three hydroxyl groups attached to the sucrose molecule are replaced by chlorine atoms [32]. It is 600 times sweeter than sucrose [33]. Like saccharin, sucralose is not metabolized by the body; however, unlike saccharin, most ingested sucralose passes through the GI tract to be eliminated in the feces. The rest reaches the kidneys for urinary excretion [34]. The administration of sucralose influences its abundance in the gut microbiome. The relative abundance of Clostridium cluster XIVa was affected in mice given 15 mg of sucralose/kg [35].
Additionally, sucralose administration for six months influenced the abundance of 14 different taxonomic levels, as well as the regulation of amino acids and chronic inflammation, in C57BL/6 mice [36]. This shows the urgent need for further research to investigate the observed effects on humans. Figure 3 and Figure 4 summarize and provide an overview of the two synthetic sweeteners and their metabolism by the gut microbiome.
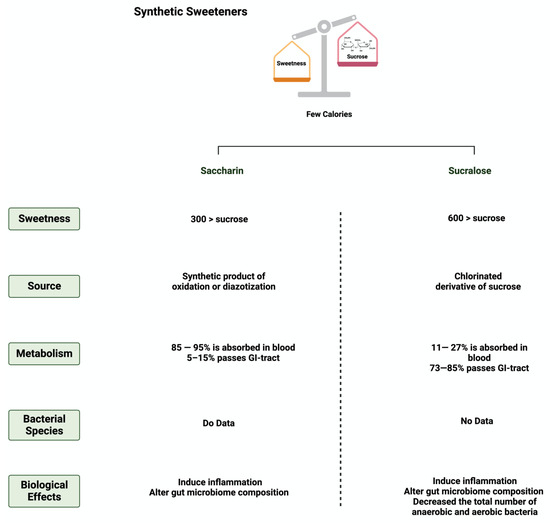
Figure 3. Overview illustration of synthetic sweeteners. The figure describes the main features of synthetic sweeteners. It also shows the sweetness intensities, the sources of the synthetic sweeteners, their metabolism by the gut microbiome, and their main biological effects. Created with BioRender.com (accessed on 15 July 2023).
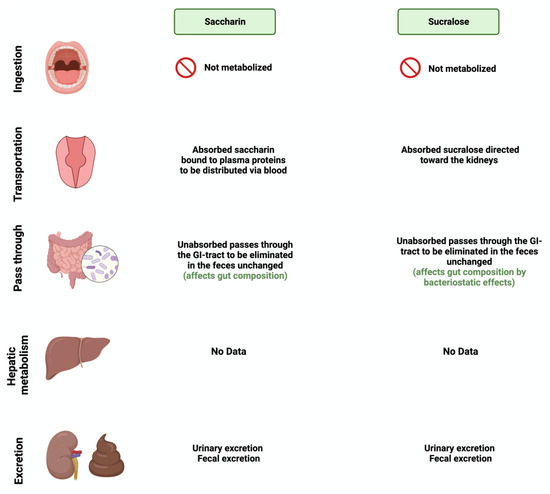
Figure 4. Overview illustration of synthetic sweetener consumption and metabolism. The figure is divided into different sites of metabolism for each of the synthetic sweeteners. Created with BioRender.com (accessed on 15 July 2023).
2. Sweeteners’ Role in Gastrointestinal Cancers
The effect of natural and synthetic sweeteners on the development of organ-specific cancer has been discussed for years [37]. With the continued rise in the consumption rate of sweeteners worldwide, several reports have supported the positive influence of sweeteners on the development and progression of GI cancer [38].
2.1. Apoptosis
Apoptosis is programmed cell death characterized by morphological and biochemical changes [39]. Its involvement in various processes, such as immune system development, makes it an essential physiological process [40]. When unregulated, it plays a role in the development of several diseases, such as autoimmune diseases, neurodegenerative disorders, and cancers [41]. Sweeteners have been reported to influence the process of apoptosis in cancers [42]. Steviol, a colonic metabolite, inhibits apoptosis in GI cancer cells as effectively as 5-fluorouracil (100 ug/mL) through the mitochondrial apoptotic pathway [43]. Additionally, in one study, steviol administration at a 1000 ug/mL concentration effectively reduced cell viability and induced apoptosis in colon cancer cells [44][45]. The results of a study that investigated the effect of 17 steviol derivatives on different cancer cell lines showed a potent cytotoxic effect of those derivatives on the cell lines [46]. Glycyrrhizin is also reported to possess apoptotic activities on GI cancers [47]. The administration of glycyrrhizin on SW48 colorectal cancer cells induced apoptosis as the levels of regulator proteins such as Bax expression increased and Bcl-2 levels decreased [48]. HT-29 colon cancer cells treated with different concentrations of glycyrrhiza glabra L. reported the induction of apoptosis at a concentration of 200 μg/mL [49][50]. Additionally, Wister rats administered 15 mg/kg of glycyrrhizic acid were reported to induce apoptosis, suppress precancerous lesion development, and reduce inflammation [51]. In a different study, the oral administration of glycyrrhizic acid (15 mg/kg) in Wister rats once a week for 15 weeks induced apoptosis by enhancing the expression of cleaved caspase 3 [52]. The induction of apoptosis through pro-caspases 3, 8, and 9 was reported in gastric cells treated with glycyrrhizic acid [53]. The sweetener neohesperidin dihydrochalcone, administered to an APC min/+ transgenic mouse model, inhibited colorectal tumorigenesis and induced apoptosis [54]. Phloroglucinol (PG), a metabolite of NHDC, induced apoptosis in HT-29 cells via overexpressed caspase-3 and caspase-8, modified Bcl-2 family proteins, and cytochrome c release [55]. In another study, PG protected mice’s intestinal damage from ionizing radiation by increasing apoptosis by affecting the p53, Bax, Bak, Bcl-2, and Bcl-XS/L proteins [56] The literature still lacks the evidence to show the underlying mechanism of the observed effect of sweeteners on GI cancers. Figure 5 summarizes the effect of sweeteners on the apoptotic pathway.
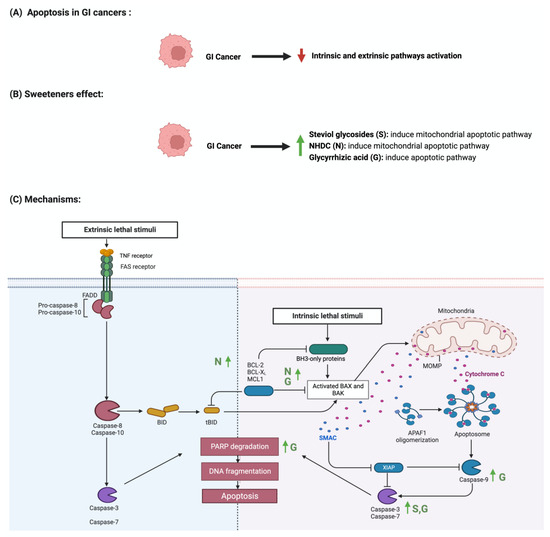
Figure 5. Illustrations of the influence of sweeteners on the apoptotic pathway in GI cancers. The figure highlights the pathological changes in apoptosis due to GI cancer, the sweeteners’ effects, and the mechanisms through which the sweeteners target the pathway. Created with BioRender.com (accessed on 15 July 2023).
2.2. The Nuclear Factor-κB Pathway
The nuclear factor-κB (NF-κB) pathway regulates genes that regulate inflammatory and immune responses [57]. In cancer, NF-κB promotes cellular proliferation and metastasis and suppresses apoptosis [58]. Although not abundantly discussed in the literature, multiple reports support the role of sweeteners in NF-κB pathway regulation [59]. Stevioside administration to a colon carcinoma cell line (Caco-2) suppressed the expression of inflammatory cytokines IL-6, TNF-a, and NF-κB [60]. Additionally, the administration of glycyrrhizic acid inhibited NF-κB expression, which led to the deactivation of inflammatory mediators in colon cells [50][61]. In Wister rats, the administration of 15 mg/kg of oral glycyrrhizic acid reduced the expression of NF-κB, nitric oxide synthase (iNOS), and cyclooxygenase-2 (COX-2) [52]. Neohesperidin dihydrochalcone, along with the two other sweeteners, influenced NF-κB expression. Oral administration of neohesperidin dihydrochalcone in mice for six days attenuated the expression of NF-κB [62]. Neohesperidin dihydrochalcone inhibited the induced NF-κB expression in paraquat-induced acute liver injury [63]. More efforts and standardized steps are required in order to conduct more research in this field and to understand the underlying mechanism of this effect. Figure 6 summarizes the effects of sweeteners on NF-κB expression.
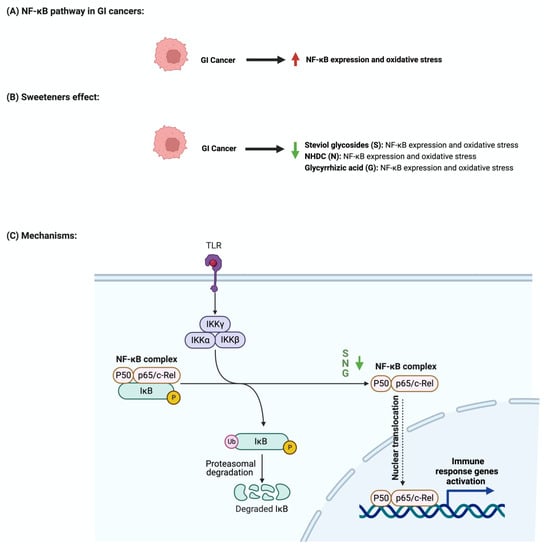
Figure 6. Illustrations of the influence of sweeteners on NF-κB in GI cancers. The figure highlights the pathological changes in NF-κB due to GI cancer, the sweeteners’ effects, and the mechanisms through which the sweeteners target the pathway. Created with BioRender.com (accessed on 15 July 2023).
2.3. Cellular Cycle Arrest
The development and function of every tissue depend on the cellular decision to transition from a proliferative to an arrested state [64]. Cancerous cells dysregulate cell cycle arrest and continue to undergo uncontrolled cellular growth [65]. The effect of sweeteners on cellular cycle arrest is scarcely reported in the literature. In a study that investigated the effect of steviol on gastric (HGC-27) and colorectal (Caco-2) cancer cells, it was reported that an increase in the expression of p53 and a decrease in the level of cyclin D occurred. Additionally, the researcher reported that steviol treatment caused G1 arrest in both cell lines [43][44]. Glycyrrhizic acid administration to different gastric cancer cell lines (e.g., MGC-803, BGC-823, SGC-7901) induces cell cycle arrest through the downregulation of G1 phase proteins such as cyclin D1, D2, D3, E1, and E2 [50][53]. In addition, 18β-glycyrrhetinic acid, another metabolite of glycyrrhizin, promoted gastric cancer cell autophagy and induced cell cycle arrest in the G0/G1 phase in a transplanted nude mouse model modulating the miR-328-3p/STAT3 signaling pathway [66]. Similar results were also reported for other cancers, such as cervical cancer [67]. Additional information regarding the observed effect was not reported for other sweeteners, which shows that more collaborative efforts are needed in order to pursue more research in this field. Figure 7 summarizes the effects of sweeteners on cell cycle arrest.
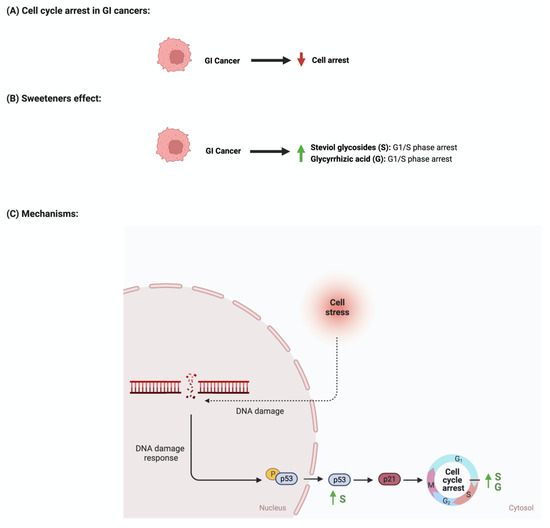
Figure 7. Illustrations of the influence of sweeteners on cell cycle arrest in GI cancers. The figure highlights the pathological changes in cell cycle arrest due to GI cancer, the sweeteners’ effects, and the mechanisms through which the sweeteners target the pathway. Created with BioRender.com (accessed on 15 July 2023).
2.4. Synthetic Sweeteners and GI Cancers
Discussing those two sweeteners raises many questions about their associated risk with gastrointestinal cancers. In an Italian cohort comprising 230 patients with histologically confirmed gastric cancer, after correcting for confounding factors, the researchers reported a lack of adverse effects of saccharin on the risk of developing neoplasms [68]. Additionally, a review paper that discussed 22 cohorts and 46 case–control studies on the effects of sweeteners on different cancers concluded that there was a lack of evidence, but there was a link between saccharin, sucralose, and other sweeteners and cancer risks [69]. Additionally, a study that used the intestinal epithelial cell line Caco-2 to investigate the effects of commonly used sweeteners reported that the administration of saccharin induced apoptosis at a lower concentration (100 uM), while at a higher concentration (1000 uM), it induced cellular death. The same effect was not observed for sucralose [70]. However, other studies reported negative effects of sucralose on colorectal cancer. A murine model administered 1.5 mg/mL of sucralose for six weeks reported a significant increase in the number and size of colorectal tumors. Also, these researchers reported an effect on the gut microbiome and inflammatory markers (TNFa, IL-1b, IL-6, IL-10, and TLR4/Myd88/NF-kB signaling) [71]. The list of studies discussing this effect is growing. However, more efforts from the research community are needed in order to address those differences in a systemic and mechanistic way, as well as to standardize the protocol to be followed and the appropriate dosage used, as it directly affects people’s health through food intake. Figure 8 illustrates the effects of synthetic sweeteners on GI cancers.
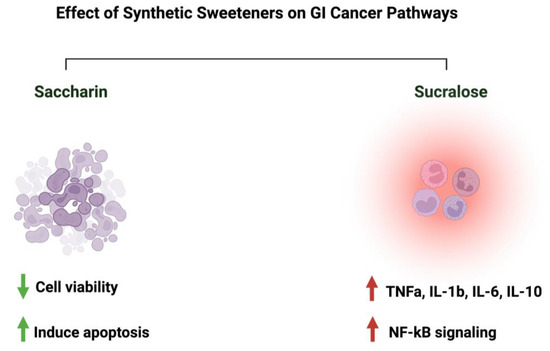
Figure 8. Summary of the influence of synthetic sweeteners on GI cancers. The figure highlights the sweeteners’ positive or negative effects on GI-targeted pathways. Created with BioRender.com (accessed on 15 July 2023).
3. Safety of Sweeteners and Challenges in the Field
Recently, the discussion about the safety of one of the commonly used sweeteners in the food industry, “aspartame”, and its possible carcinogenic nature raised more questions about the safety of other sweeteners. Here, and in most of the reported articles, it has been shown that these natural and synthetic sweeteners lack genotoxicity and carcinogenicity and are safe when consumed in moderation [72][73][74][75]. Throughout our research in the literature, most of the utilized concentrations/dosages of the sweeteners did not show adverse negative effects on the model which was used. However, some reports linked the consumption of specific sweeteners to cancer development [71]. Those results show the urgent need to address the field’s main issues. First, protocol standardization, starting from the model used, mode of administration of the sweeteners, duration of the experiment, bioinformatics tools to interpret the results, and estimation of safety measures, is critical to ensure productivity and reproducibility. Second, “recommended dosage” determination, while considering other factors such as geographical location and age, might help us to understand those sweeteners’ consumption rates. Third, guidelines and regulatory process evaluation are crucial to ensure manufacturing safety. Fourth, the possible synergistic effects of sweeteners need further investigation, as these might occur when consuming different products that contain different sweetener types and dosages.
Currently, people are more aware of their health in terms of food and always search for “healthier” and low-caloric options as alternatives while maintaining a sweet taste. The controversy regarding the safety of sweeteners raises another important question: what would be the alternative to using sweeteners? Would researchers go back to refined sugar, or move toward natural compounds such as flavonoids and phytochemicals? What are the safety and taste estimates of the consumption of those alternatives compared to sweeteners? researchers have reported the positive effects of flavonoids on GI cancers and the gut microbiome for years. However, more efforts are required in order to evaluate whether they will be a “better” alternative, considering their bioavailability [76][77][78][79]. Additionally, the effect of this “better” alternative on the gut microbiome needs more attention.
Although researchers encourage more research to be conducted, there are limitations associated with this field. First, the misreporting of participants in terms of the amount/type/quantity of sweeteners consumed might affect the interpretation of the results. Second, selection bias involved in the conducted experiment/tested population would affect the generalizability of the results to the general population. Third, residual confounding shows the urgent need to develop bioinformatics tools that correct for those factors. Fourth, causality concerns are also prominent, along with how to correctly evaluate causality and differentiate it from correlation. Other limitations may include the experimental and interpretational challenges associated with linking specific bacterial species to the metabolism of sweeteners. Addressing those limitations in future studies could help us to improve the research outcomes.
4. What about Aspartame?
More controversial discussions emerged when the World Health Organization (WHO) announced aspartame as a possible carcinogen. Aspartame is a sweetener used as a replacement for sucrose due to its high sweetness intensity [80]. The effect of aspartame on the gut microbiome has been reported in limited studies. In mice (C57Bl/6) treated with different non-caloric artificial sweeteners, including aspartame, some effect on the gut microbiome abundance and metabolic pathways was reported [81]. Additionally, the fasting glucose concentrations and the abundances of Enterobacteriaceae and Clostridium leptum were increased in diet-induced obesity models treated with aspartame for eight weeks [82]. With gastrointestinal cancers being the focus of this review, using aspartame (15 and 30 mM) for HT-29 human colorectal carcinoma proved to have a pro-angiogenic effect [83]. However, consuming artificial sweeteners, including aspartame, was not associated with colorectal or stomach cancers [84]. These data show the urgent need to address those controversial results, putting into perspective the model and the concentration of aspartame used.
References
- Brahmachari, G.; Mandal, L.C.; Roy, R.; Mondal, S.; Brahmachari, A.K. Stevioside and related compounds—Molecules of pharmaceutical promise: A critical overview. Arch. Pharm. 2011, 344, 5–19.
- Carakostas, M.C.; Curry, L.L.; Boileau, A.C.; Brusick, D.J. Overview: The history, technical function and safety of rebaudioside A, a naturally occurring steviol glycoside, for use in food and beverages. Food Chem. Toxicol. 2008, 46 (Suppl. 7), S1–S10.
- Samuel, P.; Ayoob, K.T.; Magnuson, B.A.; Wölwer-Rieck, U.; Jeppesen, P.B.; Rogers, P.J.; Rowland, I.; Mathews, R. Stevia Leaf to Stevia Sweetener: Exploring Its Science, Benefits, and Future Potential. J. Nutr. 2018, 148, 1186s–1205s.
- Orellana-Paucar, A.M. Steviol Glycosides from Stevia rebaudiana: An Updated Overview of Their Sweetening Activity, Pharmacological Properties, and Safety Aspects. Molecules 2023, 28, 1258.
- Bundgaard Anker, C.C.; Rafiq, S.; Jeppesen, P.B. Effect of Steviol Glycosides on Human Health with Emphasis on Type 2 Diabetic Biomarkers: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2019, 11, 1965.
- Soejima, A.; Tanabe, A.S.; Takayama, I.; Kawahara, T.; Watanabe, K.; Nakazawa, M.; Mishima, M.; Yahara, T. Phylogeny and biogeography of the genus Stevia (Asteraceae: Eupatorieae): An example of diversification in the Asteraceae in the new world. J. Plant Res. 2017, 130, 953–972.
- Renwick, A.G.; Tarka, S.M. Microbial hydrolysis of steviol glycosides. Food Chem. Toxicol. 2008, 46 (Suppl. 7), S70–S74.
- Gardana, C.; Simonetti, P.; Canzi, E.; Zanchi, R.; Pietta, P. Metabolism of stevioside and rebaudioside A from Stevia rebaudiana extracts by human microflora. J. Agric. Food Chem. 2003, 51, 6618–6622.
- Magnuson, B.A.; Carakostas, M.C.; Moore, N.H.; Poulos, S.P.; Renwick, A.G. Biological fate of low-calorie sweeteners. Nutr. Rev. 2016, 74, 670–689.
- Ashwell, M. Stevia, Nature’s Zero-Calorie Sustainable Sweetener: A New Player in the Fight Against Obesity. Nutr. Today 2015, 50, 129–134.
- Schröfelbauer, B.; Raffetseder, J.; Hauner, M.; Wolkerstorfer, A.; Ernst, W.; Szolar, O.H. Glycyrrhizin, the main active compound in liquorice, attenuates pro-inflammatory responses by interfering with membrane-dependent receptor signalling. Biochem. J. 2009, 421, 473–482.
- Luo, P.; Liu, D.; Li, J. Pharmacological perspective: Glycyrrhizin may be an efficacious therapeutic agent for COVID-19. Int. J. Antimicrob. Agents 2020, 55, 105995.
- Roohbakhsh, A.; Iranshahy, M.; Iranshahi, M. Glycyrrhetinic Acid and Its Derivatives: Anticancer and Cancer Chemopreventive Properties, Mechanisms of Action and Structure-Cytotoxic Activity Relationship. Curr. Med. Chem. 2016, 23, 498–517.
- Omar, H.R.; Komarova, I.; El-Ghonemi, M.; Fathy, A.; Rashad, R.; Abdelmalak, H.D.; Yerramadha, M.R.; Ali, Y.; Helal, E.; Camporesi, E.M. Licorice abuse: Time to send a warning message. Ther. Adv. Endocrinol. Metab. 2012, 3, 125–138.
- Kwon, Y.J.; Son, D.H.; Chung, T.H.; Lee, Y.J. A Review of the Pharmacological Efficacy and Safety of Licorice Root from Corroborative Clinical Trial Findings. J. Med. Food 2020, 23, 12–20.
- Kim, Y.S.; Kim, J.J.; Cho, K.H.; Jung, W.S.; Moon, S.K.; Park, E.K.; Kim, D.H. Biotransformation of ginsenoside Rb1, crocin, amygdalin, geniposide, puerarin, ginsenoside Re, hesperidin, poncirin, glycyrrhizin, and baicalin by human fecal microflora and its relation to cytotoxicity against tumor cells. J. Microbiol. Biotechnol. 2008, 18, 1109–1114.
- Deutch, M.R.; Grimm, D.; Wehland, M.; Infanger, M.; Krüger, M. Bioactive Candy: Effects of Licorice on the Cardiovascular System. Foods 2019, 8, 495.
- Isbrucker, R.A.; Burdock, G.A. Risk and safety assessment on the consumption of Licorice root (Glycyrrhiza sp.), its extract and powder as a food ingredient, with emphasis on the pharmacology and toxicology of glycyrrhizin. Regul. Toxicol. Pharmacol. 2006, 46, 167–192.
- Choi, S.; Yu, S.; Lee, J.; Kim, W. Effects of Neohesperidin Dihydrochalcone (NHDC) on Oxidative Phosphorylation, Cytokine Production, and Lipid Deposition. Foods 2021, 10, 1408.
- Winnig, M.; Bufe, B.; Kratochwil, N.A.; Slack, J.P.; Meyerhof, W. The binding site for neohesperidin dihydrochalcone at the human sweet taste receptor. BMC Struct. Biol. 2007, 7, 66.
- Prinz, P. The role of dietary sugars in health: Molecular composition or just calories? Eur. J. Clin. Nutr. 2019, 73, 1216–1223.
- Williamson, G.; Clifford, M.N. Role of the small intestine, colon and microbiota in determining the metabolic fate of polyphenols. Biochem. Pharmacol. 2017, 139, 24–39.
- Gómez-Fernández, A.R.; Santacruz, A.; Jacobo-Velázquez, D.A. The complex relationship between metabolic syndrome and sweeteners. J. Food Sci. 2021, 86, 1511–1531.
- Kwon, M.; Kim, Y.; Lee, J.; Manthey, J.A.; Kim, Y.; Kim, Y. Neohesperidin Dihydrochalcone and Neohesperidin Dihydrochalcone-O-Glycoside Attenuate Subcutaneous Fat and Lipid Accumulation by Regulating PI3K/AKT/mTOR Pathway In Vivo and In Vitro. Nutrients 2022, 14, 1087.
- Del Pozo, S.; Gómez-Martínez, S.; Díaz, L.E.; Nova, E.; Urrialde, R.; Marcos, A. Potential Effects of Sucralose and Saccharin on Gut Microbiota: A Review. Nutrients 2022, 14, 1682.
- Amin, K.A.; AlMuzafar, H.M. Alterations in lipid profile, oxidative stress and hepatic function in rat fed with saccharin and methyl-salicylates. Int. J. Clin. Exp. Med. 2015, 8, 6133–6144.
- Azeez, O.H.; Alkass, S.Y.; Persike, D.S. Long-Term Saccharin Consumption and Increased Risk of Obesity, Diabetes, Hepatic Dysfunction, and Renal Impairment in Rats. Medicina 2019, 55, 681.
- Abdelaziz, I.; Ashour Ael, R. Effect of saccharin on albino rats’ blood indices and the therapeutic action of vitamins C and E. Hum. Exp. Toxicol. 2011, 30, 129–137.
- Anderson, R.L.; Kirkland, J.J. The effect of sodium saccharin in the diet on caecal microflora. Food Cosmet. Toxicol. 1980, 18, 353–355.
- Naim, M.; Zechman, J.M.; Brand, J.G.; Kare, M.R.; Sandovsky, V. Effects of sodium saccharin on the activity of trypsin, chymotrypsin, and amylase and upon bacteria in small intestinal contents of rats. Proc. Soc. Exp. Biol. Med. 1985, 178, 392–401.
- Magnuson, B.A.; Roberts, A.; Nestmann, E.R. Critical review of the current literature on the safety of sucralose. Food Chem. Toxicol. 2017, 106, 324–355.
- AlDeeb, O.A.; Mahgoub, H.; Foda, N.H. Sucralose. Profiles Drug Subst. Excip. Relat. Methodol. 2013, 38, 423–462.
- Thomson, P.; Santibañez, R.; Aguirre, C.; Galgani, J.E.; Garrido, D. Short-term impact of sucralose consumption on the metabolic response and gut microbiome of healthy adults. Br. J. Nutr. 2019, 122, 856–862.
- Knight, I. The development and applications of sucralose, a new high-intensity sweetener. Can. J. Physiol. Pharmacol. 1994, 72, 435–439.
- Ruiz-Ojeda, F.J.; Plaza-Díaz, J.; Sáez-Lara, M.J.; Gil, A. Effects of Sweeteners on the Gut Microbiota: A Review of Experimental Studies and Clinical Trials. Adv. Nutr. 2019, 10, S31–S48.
- Bian, X.; Chi, L.; Gao, B.; Tu, P.; Ru, H.; Lu, K. Gut Microbiome Response to Sucralose and Its Potential Role in Inducing Liver Inflammation in Mice. Front. Physiol. 2017, 8, 487.
- Sylvetsky, A.C.; Rother, K.I. Trends in the consumption of low-calorie sweeteners. Physiol. Behav. 2016, 164, 446–450.
- Pan, B.; Ge, L.; Lai, H.; Wang, Q.; Wang, Q.; Zhang, Q.; Yin, M.; Li, S.; Tian, J.; Yang, K.; et al. Association of soft drink and 100% fruit juice consumption with all-cause mortality, cardiovascular diseases mortality, and cancer mortality: A systematic review and dose-response meta-analysis of prospective cohort studies. Crit. Rev. Food Sci. Nutr. 2022, 62, 8908–8919.
- Norbury, C.J.; Hickson, I.D. Cellular responses to DNA damage. Annu. Rev. Pharmacol. Toxicol. 2001, 41, 367–401.
- Elmore, S. Apoptosis: A review of programmed cell death. Toxicol. Pathol. 2007, 35, 495–516.
- Zeiss, C.J. The apoptosis-necrosis continuum: Insights from genetically altered mice. Vet. Pathol. 2003, 40, 481–495.
- Paul, S.; Sengupta, S.; Bandyopadhyay, T.K.; Bhattacharyya, A. Stevioside induced ROS-mediated apoptosis through mitochondrial pathway in human breast cancer cell line MCF-7. Nutr. Cancer 2012, 64, 1087–1094.
- Chen, J.; Xia, Y.; Sui, X.; Peng, Q.; Zhang, T.; Li, J.; Zhang, J. Steviol, a natural product inhibits proliferation of the gastrointestinal cancer cells intensively. Oncotarget 2018, 9, 26299–26308.
- Iatridis, N.; Kougioumtzi, A.; Vlataki, K.; Papadaki, S.; Magklara, A. Anti-Cancer Properties of Stevia rebaudiana; More than a Sweetener. Molecules 2022, 27, 1362.
- Vaško, L.; Vašková, J.; Fejerčáková, A.; Mojžišová, G.; Poráčová, J. Comparison of some antioxidant properties of plant extracts from Origanum vulgare, Salvia officinalis, Eleutherococcus senticosus and Stevia rebaudiana. In Vitro Cell. Dev. Biol. Anim. 2014, 50, 614–622.
- Ukiya, M.; Sawada, S.; Kikuchi, T.; Kushi, Y.; Fukatsu, M.; Akihisa, T. Cytotoxic and apoptosis-inducing activities of steviol and isosteviol derivatives against human cancer cell lines. Chem. Biodivers. 2013, 10, 177–188.
- Kabe, Y.; Koike, I.; Yamamoto, T.; Hirai, M.; Kanai, A.; Furuhata, R.; Tsugawa, H.; Harada, E.; Sugase, K.; Hanadate, K.; et al. Glycyrrhizin Derivatives Suppress Cancer Chemoresistance by Inhibiting Progesterone Receptor Membrane Component 1. Cancers 2021, 13, 3265.
- Zhang, Z.; Xu, M.; Sun, X.; Guo, X. Naturally occurring glycyrrhizin triterpene exerts anticancer effects on colorectal cancer cells via induction of apoptosis and autophagy and suppression of cell migration and invasion by targeting MMP-9 and MMP-2 expression. J. BUON 2020, 25, 188–193.
- Nourazarian, S.M.; Nourazarian, A.; Majidinia, M.; Roshaniasl, E. Effect of Root Extracts of Medicinal Herb Glycyrrhiza glabra on HSP90 Gene Expression and Apoptosis in the HT-29 Colon Cancer Cell Line. Asian Pac. J. Cancer Prev. 2015, 16, 8563–8566.
- Tuli, H.S.; Garg, V.K.; Mehta, J.K.; Kaur, G.; Mohapatra, R.K.; Dhama, K.; Sak, K.; Kumar, A.; Varol, M.; Aggarwal, D.; et al. Licorice (Glycyrrhiza glabra L.)-Derived Phytochemicals Target Multiple Signaling Pathways to Confer Oncopreventive and Oncotherapeutic Effects. Onco Targets Ther. 2022, 15, 1419–1448.
- Khan, R.; Khan, A.Q.; Lateef, A.; Rehman, M.U.; Tahir, M.; Ali, F.; Hamiza, O.O.; Sultana, S. Glycyrrhizic acid suppresses the development of precancerous lesions via regulating the hyperproliferation, inflammation, angiogenesis and apoptosis in the colon of Wistar rats. PLoS ONE 2013, 8, e56020.
- Khan, R.; Rehman, M.U.; Khan, A.Q.; Tahir, M.; Sultana, S. Glycyrrhizic acid suppresses 1,2-dimethylhydrazine-induced colon tumorigenesis in Wistar rats: Alleviation of inflammatory, proliferation, angiogenic, and apoptotic markers. Environ. Toxicol. 2018, 33, 1272–1283.
- Wang, H.; Ge, X.; Qu, H.; Wang, N.; Zhou, J.; Xu, W.; Xie, J.; Zhou, Y.; Shi, L.; Qin, Z.; et al. Glycyrrhizic Acid Inhibits Proliferation of Gastric Cancer Cells by Inducing Cell Cycle Arrest and Apoptosis. Cancer Manag. Res. 2020, 12, 2853–2861.
- Gong, Y.; Dong, R.; Gao, X.; Li, J.; Jiang, L.; Zheng, J.; Cui, S.; Ying, M.; Yang, B.; Cao, J.; et al. Neohesperidin prevents colorectal tumorigenesis by altering the gut microbiota. Pharmacol. Res. 2019, 148, 104460.
- Kang, M.H.; Kim, I.H.; Nam, T.J. Phloroglucinol induces apoptosis via apoptotic signaling pathways in HT-29 colon cancer cells. Oncol. Rep. 2014, 32, 1341–1346.
- Ha, D.; Bing, S.J.; Cho, J.; Ahn, G.; Kim, D.S.; Al-Amin, M.; Park, S.J.; Jee, Y. Phloroglucinol protects small intestines of mice from ionizing radiation by regulating apoptosis-related molecules: A comparative immunohistochemical study. J. Histochem. Cytochem. 2013, 61, 63–74.
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.C. NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2017, 2, 17023.
- Xia, Y.; Shen, S.; Verma, I.M. NF-κB, an active player in human cancers. Cancer Immunol. Res. 2014, 2, 823–830.
- Kasti, A.N.; Nikolaki, M.D.; Synodinou, K.D.; Katsas, K.N.; Petsis, K.; Lambrinou, S.; Pyrousis, I.A.; Triantafyllou, K. The Effects of Stevia Consumption on Gut Bacteria: Friend or Foe? Microorganisms 2022, 10, 744.
- Boonkaewwan, C.; Burodom, A. Anti-inflammatory and immunomodulatory activities of stevioside and steviol on colonic epithelial cells. J. Sci. Food Agric. 2013, 93, 3820–3825.
- Jain, R.; Hussein, M.A.; Pierce, S.; Martens, C.; Shahagadkar, P.; Munirathinam, G. Oncopreventive and oncotherapeutic potential of licorice triterpenoid compound glycyrrhizin and its derivatives: Molecular insights. Pharmacol. Res. 2022, 178, 106138.
- Xia, X.; Fu, J.; Song, X.; Shi, Q.; Su, C.; Song, E.; Song, Y. Neohesperidin dihydrochalcone down-regulates MyD88-dependent and -independent signaling by inhibiting endotoxin-induced trafficking of TLR4 to lipid rafts. Free Radic. Biol. Med. 2015, 89, 522–532.
- Shi, Q.; Song, X.; Fu, J.; Su, C.; Xia, X.; Song, E.; Song, Y. Artificial sweetener neohesperidin dihydrochalcone showed antioxidative, anti-inflammatory and anti-apoptosis effects against paraquat-induced liver injury in mice. Int. Immunopharmacol. 2015, 29, 722–729.
- Stallaert, W.; Taylor, S.R.; Kedziora, K.M.; Taylor, C.D.; Sobon, H.K.; Young, C.L.; Limas, J.C.; Varblow Holloway, J.; Johnson, M.S.; Cook, J.G.; et al. The molecular architecture of cell cycle arrest. Mol. Syst. Biol. 2022, 18, e11087.
- Schwartz, G.K.; Shah, M.A. Targeting the cell cycle: A new approach to cancer therapy. J. Clin. Oncol. 2005, 23, 9408–9421.
- Li, X.; Ma, X.L.; Nan, Y.; Du, Y.H.; Yang, Y.; Lu, D.D.; Zhang, J.F.; Chen, Y.; Zhang, L.; Niu, Y.; et al. 18β-glycyrrhetinic acid inhibits proliferation of gastric cancer cells through regulating the miR-345-5p/TGM2 signaling pathway. World J. Gastroenterol. 2023, 29, 3622–3644.
- Farooqui, A.; Khan, F.; Khan, I.; Ansari, I.A. Glycyrrhizin induces reactive oxygen species-dependent apoptosis and cell cycle arrest at G(0)/G(1) in HPV18(+) human cervical cancer HeLa cell line. Biomed. Pharmacother. 2018, 97, 752–764.
- Bosetti, C.; Gallus, S.; Talamini, R.; Montella, M.; Franceschi, S.; Negri, E.; La Vecchia, C. Artificial sweeteners and the risk of gastric, pancreatic, and endometrial cancers in Italy. Cancer Epidemiol. Biomark. Prev. 2009, 18, 2235–2238.
- Pavanello, S.; Moretto, A.; La Vecchia, C.; Alicandro, G. Non-sugar sweeteners and cancer: Toxicological and epidemiological evidence. Regul. Toxicol. Pharmacol. 2023, 139, 105369.
- Shil, A.; Olusanya, O.; Ghufoor, Z.; Forson, B.; Marks, J.; Chichger, H. Artificial Sweeteners Disrupt Tight Junctions and Barrier Function in the Intestinal Epithelium through Activation of the Sweet Taste Receptor, T1R3. Nutrients 2020, 12, 1862.
- Li, X.; Liu, Y.; Wang, Y.; Li, X.; Liu, X.; Guo, M.; Tan, Y.; Qin, X.; Wang, X.; Jiang, M. Sucralose Promotes Colitis-Associated Colorectal Cancer Risk in a Murine Model Along With Changes in Microbiota. Front. Oncol. 2020, 10, 710.
- Qurratul, A.; Khan, S.A. Artificial sweeteners: Safe or unsafe? J. Pak. Med. Assoc. 2015, 65, 225–227.
- Roberts, A. The safety and regulatory process for low calorie sweeteners in the United States. Physiol. Behav. 2016, 164, 439–444.
- Chappell, G.A.; Heintz, M.M.; Borghoff, S.J.; Doepker, C.L.; Wikoff, D.S. Lack of potential carcinogenicity for steviol glycosides—Systematic evaluation and integration of mechanistic data into the totality of evidence. Food Chem. Toxicol. 2021, 150, 112045.
- Lea, I.A.; Chappell, G.A.; Wikoff, D.S. Overall lack of genotoxic activity among five common low- and no-calorie sweeteners: A contemporary review of the collective evidence. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2021, 868–869, 503389.
- Al-Ishaq, R.K.; Overy, A.J.; Büsselberg, D. Phytochemicals and Gastrointestinal Cancer: Cellular Mechanisms and Effects to Change Cancer Progression. Biomolecules 2020, 10, 105.
- Al-Ishaq, R.K.; Liskova, A.; Kubatka, P.; Büsselberg, D. Enzymatic Metabolism of Flavonoids by Gut Microbiota and Its Impact on Gastrointestinal Cancer. Cancers 2021, 13, 3934.
- Al-Ishaq, R.K.; Koklesova, L.; Kubatka, P.; Büsselberg, D. Immunomodulation by Gut Microbiome on Gastrointestinal Cancers: Focusing on Colorectal Cancer. Cancers 2022, 14, 2140.
- Samec, M.; Mazurakova, A.; Lucansky, V.; Koklesova, L.; Pecova, R.; Pec, M.; Golubnitschaja, O.; Al-Ishaq, R.K.; Caprnda, M.; Gaspar, L.; et al. Flavonoids attenuate cancer metabolism by modulating Lipid metabolism, amino acids, ketone bodies and redox state mediated by Nrf2. Eur. J. Pharmacol. 2023, 949, 175655.
- Czarnecka, K.; Pilarz, A.; Rogut, A.; Maj, P.; Szymanska, J.; Olejnik, L.; Szymanski, P. Aspartame-True or False? Narrative Review of Safety Analysis of General Use in Products. Nutrients 2021, 13, 1957.
- Suez, J.; Korem, T.; Zeevi, D.; Zilberman-Schapira, G.; Thaiss, C.A.; Maza, O.; Israeli, D.; Zmora, N.; Gilad, S.; Weinberger, A.; et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 2014, 514, 181–186.
- Palmnas, M.S.; Cowan, T.E.; Bomhof, M.R.; Su, J.; Reimer, R.A.; Vogel, H.J.; Hittel, D.S.; Shearer, J. Low-dose aspartame consumption differentially affects gut microbiota-host metabolic interactions in the diet-induced obese rat. PLoS ONE 2014, 9, e109841.
- Maghiari, A.L.; Coricovac, D.; Pinzaru, I.A.; Macasoi, I.G.; Marcovici, I.; Simu, S.; Navolan, D.; Dehelean, C. High Concentrations of Aspartame Induce Pro-Angiogenic Effects in Ovo and Cytotoxic Effects in HT-29 Human Colorectal Carcinoma Cells. Nutrients 2020, 12, 3600.
- Palomar-Cros, A.; Straif, K.; Romaguera, D.; Aragones, N.; Castano-Vinyals, G.; Martin, V.; Moreno, V.; Gomez-Acebo, I.; Guevara, M.; Aizpurua, A.; et al. Consumption of aspartame and other artificial sweeteners and risk of cancer in the Spanish multicase-control study (MCC-Spain). Int. J. Cancer 2023, 153, 979–993.
More
Information
Subjects:
Gastroenterology & Hepatology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Entry Collection:
Gastrointestinal Disease
Revisions:
3 times
(View History)
Update Date:
19 Oct 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




