Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Nandini Vishwakarma | -- | 1911 | 2023-08-30 04:38:53 | | | |
| 2 | Alfred Zheng | Meta information modification | 1911 | 2023-08-30 05:58:32 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Vishwakarma, N.; Goud, R.B.; Tirupattur, M.P.; Katwa, L.C. The Long-Term Cardiovascular Effects of COVID-19. Encyclopedia. Available online: https://encyclopedia.pub/entry/48619 (accessed on 08 February 2026).
Vishwakarma N, Goud RB, Tirupattur MP, Katwa LC. The Long-Term Cardiovascular Effects of COVID-19. Encyclopedia. Available at: https://encyclopedia.pub/entry/48619. Accessed February 08, 2026.
Vishwakarma, Nandini, Reshma B. Goud, Myna Prakash Tirupattur, Laxmansa C. Katwa. "The Long-Term Cardiovascular Effects of COVID-19" Encyclopedia, https://encyclopedia.pub/entry/48619 (accessed February 08, 2026).
Vishwakarma, N., Goud, R.B., Tirupattur, M.P., & Katwa, L.C. (2023, August 30). The Long-Term Cardiovascular Effects of COVID-19. In Encyclopedia. https://encyclopedia.pub/entry/48619
Vishwakarma, Nandini, et al. "The Long-Term Cardiovascular Effects of COVID-19." Encyclopedia. Web. 30 August, 2023.
Copy Citation
COVID-19 had stormed through the world in early March of 2019, and on 5 May 2023, SARS-CoV-2 was officially declared to no longer be a global health emergency. The rise of new COVID-19 variants XBB.1.5 and XBB.1.16, a product of recombinant variants and sub-strains, has fueled a need for continued surveillance of the pandemic as they have been deemed increasingly infectious. This has caused an increase in hospitalizations, a strain in resources, and a rise of concern for public health. In addition, there is a growing population of patients experiencing cardiovascular complications as a result of post-acute sequelae of COVID-19.
COVID-19
SARS-CoV-2
long COVID
cardiovascular disease
1. Introduction
Cardiovascular disease (CVD) continues to be the leading cause of death globally, affecting more than 19 million people yearly. In the first year of the SARS-CoV-2 pandemic, the number of CVD deaths increased from 874,613 in 2019 to 928,741 in 2020, the highest rise of single-year cases since 2015 [1]. In 2022, Xie et al. found that COVID-19 patients showed elevated risks and experienced increased incidences of CVD in a 12-month period [2]. With an increasing number of patients presenting with adverse cardiac outcomes, such as myocarditis, arrhythmias, and myocardial injury, further investigation into the effects of COVID-19 on cardiac health is needed. Since the emergence of COVID-19 in 2019, the global impact of this viral infection has been extensive, causing widespread morbidity and mortality [3]. COVID-19 can also affect more vulnerable populations, such as pregnant individuals, to a higher degree. The group recently reviewed how COVID-19 infection can worsen cardiovascular health during and after the gestational period, especially as long-term effects can disproportionately impact vulnerable groups [4]. This complex issue necessitates comprehensive investigation to understand the virus’s influence on molecular, cellular, and organ tissue systems. This information can then in turn be translated to improve both maternal and fetal health. Initially, the focus was primarily on one or two variants; however, subsequent waves and mutations have presented new challenges [5]. From the beginning, COVID-19 has evolved with thousands of variants and mutations. Before, COVID-19 was simply a respiratory infection, but now people know that all organ systems are infected.
While the exact mechanism of how COVID-19 affects the heart is not concrete, the following proposed mechanism highlights a direct and indirect pathway taken. The structure of SARS-CoV-2 consists of two spike proteins that bind to Angiotensin I-converting enzyme 2 (ACE2) receptors. Upon entry to the cells, SARS-CoV2 downregulates ACE2 and upregulates TNF-α, an inflammatory cytokine. The downregulation of ACE2 inhibits Angiotensin 1–7 but promotes Angiotensin II (Ang II), which is known for its hypertensive properties [6][7]. This, in turn, promotes TGF-β1, which increases collagen production and ultimately leads to fibrosis and heart failure. Additionally, when SARS-CoV-2 enters the cell, it causes direct damage to the myocardium [6][7]. Different cardiac cells have different interactions with SARS-CoV-2. Endothelial cells that line the vessels of the heart have increased rates of apoptosis due to the virus. This, in turn, causes blood clots to form along with the blockage of arteries. Furthermore, the direct invasion of pericytes, which help regulate endothelial function, can lead to dysfunction and apoptosis as well [8]. Cardiomyocytes affected via the ACE2 receptor and acting through an endosomal protease-dependent pathway increase cytokine production, sarcomere destruction, and apoptosis.
2. Long Term Implications
2.1. Long COVID
In April 2020, researchers first became aware of post-COVID-19 syndrome when patients noticed residual symptoms [9]. Understanding the long-term effects of COVID-19 can provide a more comprehensive picture of the disease’s impact beyond the acute phase. It will allow healthcare professionals, researchers, policymakers, and the general-public to grasp the full spectrum of health consequences associated with COVID-19, ranging from physical to social to psychological implications. It is also crucial to understand how COVID-19 can impact individuals of all demographics. Adding in the factors of race, sex, and underlying comorbidities adds complexities to the problem at hand and, in turn, makes this public health emergency a complex scientific problem. To find a solution, or at least come close to one, people need to tackle the problem from all angles. Investigating the long-term effects of COVID-19 fuels scientific research and advancements in understanding the disease, and it facilitates ongoing studies to identify underlying mechanisms, risk factors, and potential treatment options. By studying long-term effects, researchers can contribute to the collective knowledge base and facilitate the development of evidence-based guidelines for prevention, treatment, and long-term care.
Post-COVID-19 syndrome, Long COVID, or post-acute sequelae of COVID-19 (PASC) is the persistence of COVID-19 infection/symptoms after 12 weeks involving multi-organ systems [10]. It has been estimated that at least 65 million people present with Long COVID, the highest age group affected being 36- to 50-year-olds. As more studies are being conducted and findings are being uncovered, people have learned that possible signs and symptoms are cardiovascular, thrombotic, and cerebrovascular disease, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), dysautonomia, postural orthostatic tachycardia syndrome (POTS), and type 2 diabetes. These symptoms can carry on for years, and some even for a lifetime (ME/CFS and dysautonomia) [11].
In more recent months, there have been new observations of the manifestation of long-term effects. In a recent study based in the UK and Hong Kong, after 21 days (about 3 weeks), there was a greater risk for many extrapulmonary conditions, such as heart failure, deep vein thrombosis, and atrial fibrillation [12]. As time has passed, there is reason to believe that the potential long-term effects of COVID-19 can become another public health emergency. Another meta-analysis points out the most common long-term effects from 6 months post-infection, and the majority align with the clinical symptoms. These include fatigue, hair loss, headache, and dyspnea [13]. As there are many biological implications for the immune response in the body, studies were performed to indicate whether these immune markers were still present in the body post-COVID-19 infection. A study based in France noted that for those whose symptoms had not fully resolved, there was still no indication of physiological irregularities, such as lymphopenia [14]. Lymphopenia has been found to be an indicator of the severity of disease progression in COVID-19 patients [15]. In terms of cardiovascular disease, evidence depicts cardiovascular outcomes to be significantly higher after COVID-19 compared to pre-exposure, supporting the idea that there is an increase in adverse cardiovascular outcomes due to COVID-19 [2].
2.2. Long-Term Cardiovascular Complications
While the immediate impacts of COVID-19 infection are well-documented, the long-term consequences, especially in relation to cardiovascular health, remain a topic of ongoing research. In addition to the various extrapulmonary conditions that can stem from COVID-19, there are many cardiac complications that arise from COVID-19, which is a significant concern. COVID-19 can lead to several cardiovascular manifestations, ranging from mild symptoms to severe adverse effects [16]. As shown in Figure 1, these emerge as risks of conditions that are of higher severity when compared to acute conditions and may lead to further complications.
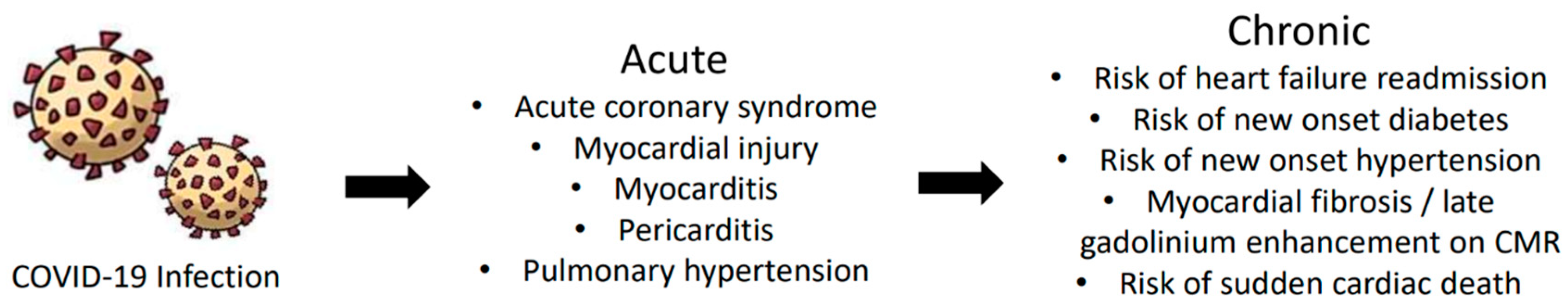
Figure 1. Acute and chronic cardiovascular complications caused by COVID-19. Many times, when patients are presented with acute cardiac symptoms due to COVID-19 infection, it can develop into chronic conditions. The most common acute manifestations are myocardial injury, myocarditis, and acute coronary syndrome. As symptoms worsen and develop, chronic conditions may arise, such as heart failure readmission, sudden cardiac death, myocardial fibrosis, onset hypertension, and diabetes.
Some individuals may continue to experience chest pain, heart palpations, and shortness of breath long after the initial infection [17]. These symptoms may be attributed to damage of the heart or ongoing inflammation. It is important to note that the long-term cardiac conditions associated with COVID-19 can affect individuals of all ages, including those with no prior history of cardiovascular disease. Even individuals with mild or asymptomatic cases may develop adverse cardiac outcomes later on. Therefore, it is crucial to monitor the cardiovascular health of all individuals who had been infected with COVID-19, regardless of the severity of their initial symptoms.
Several mechanisms have been proposed to explain the cardiovascular complications connected with long COVID. These include persistent inflammation, endothelial dysfunction, immune dysregulation, and post-viral autoimmune responses. Many studies have found that post-COVID-19 infection, there was a higher risk of individuals developing heart arrhythmias, myocardial infarction, hypertension, and heart failure. The interesting part about this phenomenon is that these conditions may occur even without any previous history of CVD [18]. A recent report indicated that a patient 67 days (about 2 months) after being diagnosed with COVID-19 had abnormal findings when a cardiac MRI was obtained, with no previous underlying conditions [19]. Another factor to consider is that cardiac abnormalities can arise regardless of the age of the patient. It has been found in studies that there is a multiorgan system inflammatory response after COVID 19 in pediatric patients.
2.3. Effects of COVID-19 Vaccinations
When comparing the severities of the various variants, vaccination status plays a significant role in symptoms, risk of hospitalization, and death. In a study of unvaccinated COVID-19 patients, myocardial infarction was less present in Omicron patients compared to Alpha and Delta patients. With fully vaccinated patients, Omicron patients also showed lower rates of MI in comparison to Alpha and Delta patients [20]. Additionally, in some cases, vaccines can contribute to cardiovascular or other complications. For example, capillary leak syndrome (CLS) is a rare disease that can be triggered by SARS-CoV-2 and its vaccine. It is hypothesized to be an immune response to an infection via a cytokine storm. CLS occurs when plasma and protein leak out of the capillaries and can eventually cause hypovolemic shock or systemic hypotension. In a case study, a patient diagnosed with COVID-19 and no history of COVID-19 vaccinations suffered from a rapid progression of CLS. The patient, a fit 42-year-old male with no significant medical history, was admitted to the hospital for syncope and hypotension. Other than his blood pressure and increased levels of hemoglobin, all of his other vital signs and blood tests showed no abnormalities. However, over the course of his stay at the hospital, his blood pressure remained low, hemoglobin and hematocrit levels continued to increase, and protein levels decreased. After becoming plethoric and suffering from leg and chest pain, the patient suddenly became unresponsive and died of cardiac arrest [21]. In another case, a patient suffered from CLS after receiving their COVID-19 vaccination (Ad26.COV2.S—Johnson & Johnson vaccine). The patient experienced postvaccination side effects, and 48 h afterward was admitted to the emergency department. Ten hours after admission, the patient died. Throughout his stay, the patient’s blood pressure progressively dropped, and tests showed hemoconcentration and hypoalbuminemia [22]. These case reports, though not common, raise a question to the unknown mechanisms of both COVID infection and vaccination and how they eventually result in such fatal symptoms.
Furthermore, as variants emerge and evolve, reinfection and post-acute sequalae have become common among patients. In a study with over 5 million patients, it was demonstrated that compared to people with no reinfection, people with reinfection showed increased risks of all-cause mortality, hospitalizations, and other adverse outcomes [23]. A specific risk factor was being unvaccinated or being vaccinated before reinfection, and that risk and burden of all-cause mortality increased with the number of reinfections [23]. In terms of cardiovascular complications, people with reinfection exhibited the most risk of cardiovascular disorders after pulmonary sequelae, although the cardiovascular disorders are not specified [23], and there is limited data on cardiac conditions upon reinfection. A recent report by CDC states that reinfection-associated severe outcomes have not been previously characterized, but between September 2021-December 2022, percentages of reinfections have rapidly increased, and the United States is also seeing higher numbers of severe outcomes related to reinfection [24]. Though it may be possible that new variants are evading vaccines, vaccination and antiviral treatment are still recommended to reduce the risk of adverse COVID-19 sequelae.
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation 2023, 147, e93–e621.
- Xie, Y.; Xu, E.; Bowe, B.; Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022, 28, 583–590.
- Hiscott, J.; Alexandridi, M.; Muscolini, M.; Tassone, E.; Palermo, E.; Soultsioti, M.; Zevini, A. The global impact of the coronavirus pandemic. Cytokine Growth Factor Rev. 2020, 53, 1–9.
- Greenberg, G.C.; Vishwakarma, N.; Tirupattur, M.P.; Sprague, H.M.; Katwa, L.C. Implications of COVID-19 Pandemic on Pregnancy: Current Status and Controversies. COVID 2023, 3, 859–873.
- El-Shabasy, R.M.; Nayel, M.A.; Taher, M.M.; Abdelmonem, R.; Shoueir, K.R.; Kenawy, E.R. Three waves changes, new variant strains, and vaccination effect against COVID-19 pandemic. Int. J. Biol. Macromol. 2022, 204, 161–168.
- Katwa, L.C.; Mendoza, C.; Clements, M. CVD and COVID-19: Emerging Roles of Cardiac Fibroblasts and Myofibroblasts. Cells 2022, 11, 1316.
- Zhao, Y.-H.; Zhao, L.; Yang, X.-C.; Wang, P. Cardiovascular complications of SARS-CoV-2 infection (COVID-19): A systematic review and meta-analysis. Rev. Cardiovasc. Med. 2021, 22, 159.
- Tsai, E.J.; Čiháková, D.; Tucker, N.R. Cell-Specific Mechanisms in the Heart of COVID-19 Patients. Circ. Res. 2023, 132, 1290–1301.
- COVID.org. In Long COVID Terms and Definitions Development Explained; Department of Health and Human Services: Washington, DC, USA, 2023.
- DePace, N.L.; Colombo, J. Long-COVID Syndrome and the Cardiovascular System: A Review of Neurocardiologic Effects on Multiple Systems. Curr. Cardiol. Rep. 2022, 24, 1711–1726.
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146.
- Lam, I.C.H.; Wong, C.K.H.; Zhang, R.; Chui, C.S.L.; Lai, F.T.T.; Li, X.; Chan, E.W.Y.; Luo, H.; Zhang, Q.; Man, K.K.C.; et al. Long-term post-acute sequelae of COVID-19 infection: A retrospective, multi-database cohort study in Hong Kong and the UK. EClinicalMedicine 2023, 60, 102000.
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144.
- Davido, B.; Seang, S.; Tubiana, R.; de Truchis, P. Post–COVID-19 chronic symptoms: A postinfectious entity? Clin. Microbiol. Infect. 2020, 26, 1448–1449.
- Toori, K.U.; Qureshi, M.A.; Chaudhry, A. Lymphopenia: A useful predictor of COVID-19 disease severity and mortality. Pak. J. Med. Sci. 2021, 37, 1984–1988.
- Alqahtani, M.S.; Abbas, M.; Alsabaani, A.; Alqarni, A.; Almohiy, H.M.; Alsawqaee, E.; Alshahrani, R.; Alshahrani, S. The Potential Impact of COVID-19 Virus on the Heart and the Circulatory System. Infect. Drug Resist. 2022, 2022, 1175–1189.
- Raman, B.; Bluemke, D.A.; Lüscher, T.F.; Neubauer, S. Long COVID: Post-acute sequelae of COVID-19 with a cardiovascular focus. Eur. Heart J. 2022, 43, 1157–1172.
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265.
- Xie, Y.; Choi, T.; Al-Aly, Z. Association of Treatment With Nirmatrelvir and the Risk of Post–COVID-19 Condition. JAMA Intern. Med. 2023, 183, 554–564.
- Arabi, M.; Al-Najjar, Y.; Mhaimeed, N.; Salameh, M.A.; Paul, P.; AlAnni, J.; Abdelati, A.A.; Laswi, I.; Khanjar, B.; Al-Ali, D.; et al. Severity of the Omicron SARS-CoV-2 variant compared with the previous lineages: A systematic review. J. Cell. Mol. Med. 2023, 27, 1443–1464.
- Novotná, E.; Filipová, P.; Vonke, I.; Kuta, B.; Chrdle, A. Rapid Progression of COVID-19-Associated Fatal Capillary Leak Syndrome. Infect. Dis. Rep. 2022, 14, 884–888.
- Choi, G.-J.; Baek, S.H.; Kim, J.; Kim, J.H.; Kwon, G.-Y.; Kim, D.K.; Jung, Y.H.; Kim, S. Fatal Systemic Capillary Leak Syndrome after SARS-CoV-2Vaccination in Patient with Multiple Myeloma. Emerg. Infect. Dis. 2021, 27, 2973–2975.
- Bowe, B.; Xie, Y.; Al-Aly, Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat. Med. 2022, 28, 2398–2405.
- CDC. Trends in Laboratory-Confirmed SARS-CoV-2 Reinfections and Associated Hospitalizations and Deaths Among Adults Aged ≥18 Years—18 U.S. Jurisdictions, September 2021–December 2022; Center for Disease Control and Prevention: Atlanta, GA, USA, 2023.
More
Information
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
880
Entry Collection:
COVID-19
Revisions:
2 times
(View History)
Update Date:
30 Aug 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




