Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Alfredo Parra-Lucares | -- | 3522 | 2023-08-23 18:51:26 | | | |
| 2 | Sirius Huang | Meta information modification | 3522 | 2023-08-24 03:20:25 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Parra-Lucares, A.; Villa, E.; Romero-Hernández, E.; Méndez-Valdés, G.; Retamal, C.; Vizcarra, G.; Henríquez, I.; Maldonado-Morales, E.A.J.; Grant-Palza, J.H.; Ruíz-Tagle, S.; et al. The Hallmarks of Atrial Fibrillation. Encyclopedia. Available online: https://encyclopedia.pub/entry/48390 (accessed on 07 February 2026).
Parra-Lucares A, Villa E, Romero-Hernández E, Méndez-Valdés G, Retamal C, Vizcarra G, et al. The Hallmarks of Atrial Fibrillation. Encyclopedia. Available at: https://encyclopedia.pub/entry/48390. Accessed February 07, 2026.
Parra-Lucares, Alfredo, Eduardo Villa, Esteban Romero-Hernández, Gabriel Méndez-Valdés, Catalina Retamal, Geovana Vizcarra, Ignacio Henríquez, Esteban A. J. Maldonado-Morales, Juan H. Grant-Palza, Sofía Ruíz-Tagle, et al. "The Hallmarks of Atrial Fibrillation" Encyclopedia, https://encyclopedia.pub/entry/48390 (accessed February 07, 2026).
Parra-Lucares, A., Villa, E., Romero-Hernández, E., Méndez-Valdés, G., Retamal, C., Vizcarra, G., Henríquez, I., Maldonado-Morales, E.A.J., Grant-Palza, J.H., Ruíz-Tagle, S., Estrada-Bobadilla, V., & Toro, L. (2023, August 23). The Hallmarks of Atrial Fibrillation. In Encyclopedia. https://encyclopedia.pub/entry/48390
Parra-Lucares, Alfredo, et al. "The Hallmarks of Atrial Fibrillation." Encyclopedia. Web. 23 August, 2023.
Copy Citation
Atrial fibrillation (AF) is a prevalent cardiac condition predominantly affecting older adults, characterized by irregular heartbeat rhythm. The condition often leads to significant disability and increased mortality rates.
atrial fibrillation
electrophysiology
1. Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia worldwide, with a global prevalence of around 1%, reaching nearly 10% in individuals over 80 years old [1]. It is characterized by a chaotic atrial rhythm derived from irregular electrical activity in different ectopic trigger sites, such as the pulmonary veins (PV) and the left atrium (LA) [2]. It is a significant cause of disability and death, especially in the elderly population, due to the development of complications, such as strokes, frequent hospitalizations, and bleeding associated with anticoagulant therapy [3]. This population is highly relevant, given that the primary risk factor for the onset of AF is age [4].
The therapeutic approach in AF has been a subject of debate for decades regarding the management of heart rate versus heart rhythm [5]. Initially, it was established that there was no difference between one therapeutic approach and another, leading to a preference for rate control over rhythm control due to the low rate of effectiveness and the proarrhythmic complications associated with antiarrhythmic drugs (AAD) [6]. However, over time, evidence began to demonstrate that AF progresses through different stages of the disease via electrical and structural remodeling phenomena that intensify with the passage of years [7]. Recent studies have highlighted the advantages of early conversion to sinus rhythm in patients with this arrhythmia [8][9][10].
Based on the above, it can be concluded that the restoration of sinus rhythm may reverse a series of electrophysiological and molecular mechanisms that underlie the natural progression of the disease, through which a patient transitions from paroxysmal AF episodes to the final stage of permanent AF [11].
2. The Hallmarks of Atrial Fibrillation
The clinical classification of AF is principally based on whether the episode terminates spontaneously or not, and the duration of the episode, progressing from paroxysmal, persistent, long persistent to permanent AF [1]. Recently, new classification systems for AF have been proposed [12]. Nonetheless, their pathophysiological correlate is still uncertain. The classical clinical categories have proven distinct behaviors that may reflect the underlying molecular mechanisms [13], although they are still not fully understood.
This section will describe the pathophysiological continuum that explains the origin, maintenance, progression, and stabilization of AF, with the key aspects that have been described for each of the clinical stages, which will be referred to as “hallmarks”. Researchers also propose an “at risk” stage, analogous to what exists for heart failure (HF) [14] that is based on the genetic susceptibility and non-AF remodeling that may lead in some people to the development of this disease. It must be noted that AF has several clinical presentations that do not always follow this order (Figure 1).
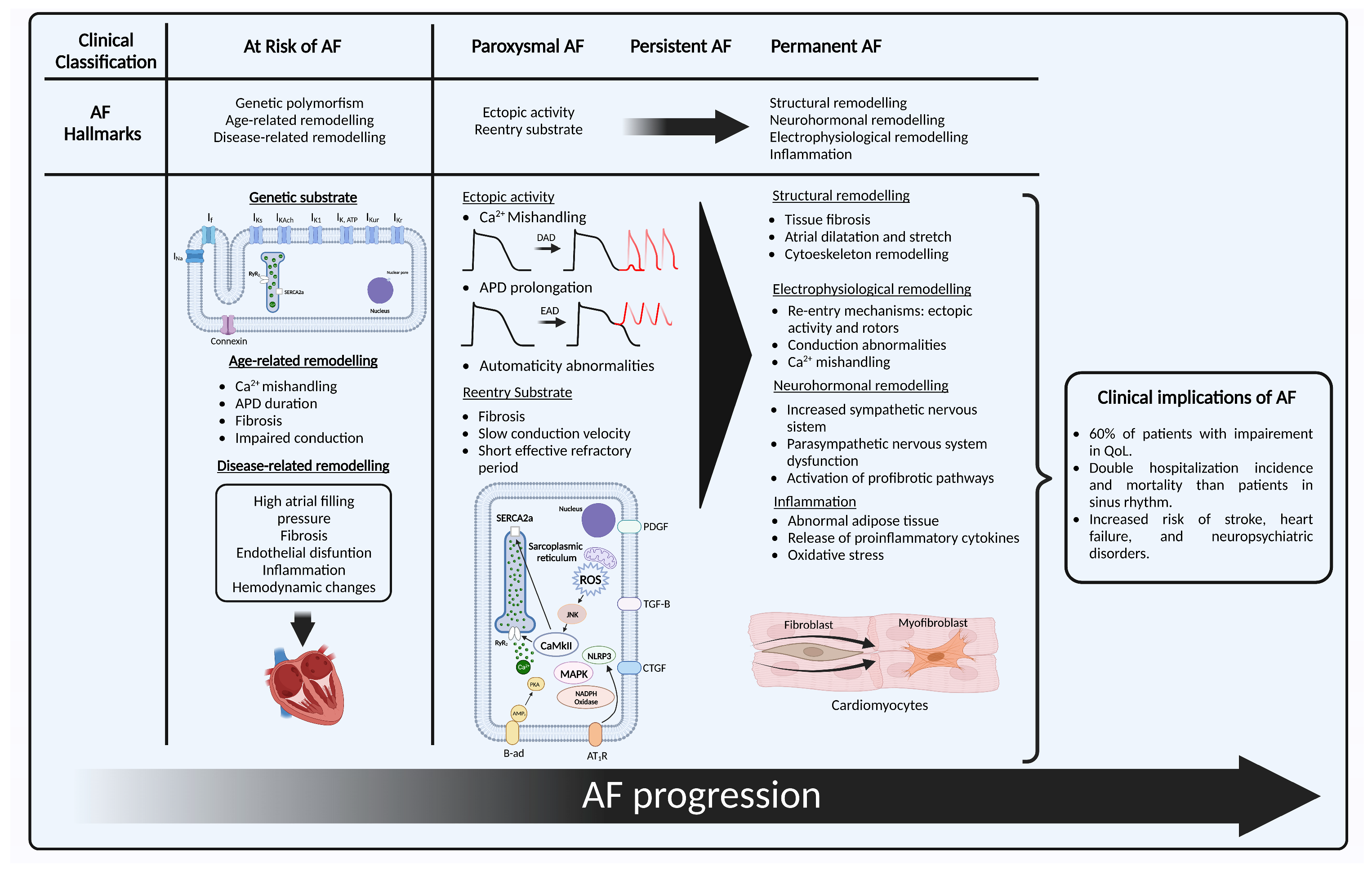
Figure 1. Representation of AF hallmarks with their clinical correlate. First, “at risk of AF” with its three hallmarks: (1) genetic substrate shows a cardiomyocyte with the main structures in which genetic variants for ion channel and non-ion channel genes that have shown association with the development of AF: IK1 current (KCNJ2), IKs (KCNE1, KCNE2, KCNE3, KCNE4, KCNE5, KCND3, KCNQ1), IKAch (KCNJ5), IKur (KCNA5), IKr (KCNH2), IKATP (ABCC9), If (HCN4), INa (SCN1B, SCN2B, SCN3B, SCN5A, SCN10A), connexin 40 (GJA5), connexin 43 (GJA1), and nucleoporin 155 (NUP155); (2) age-related remodeling; (3) disease-related remodeling; next to it the clinical stages of AF, with the initial hallmarks of paroxysmal AF: (1) ectopic activity secondary to DAD, EAD or automaticity abnormalities; (2) re-entry and some of its intracellular mechanisms of perpetuation; and the hallmarks of persistent and permanent AF that include structural, electrophysiological, and neurohormonal remodeling, and inflammation. Created with BioRender.com (accessed on 28 May 2023). AF: atrial fibrillation; DAD: delayed afterdepolarization; EAD: early afterdepolarization; APD: action potential duration; SERCA2a: sarcoplasmic reticulum Ca2+-adenosine triphosphate; RyR2: ryanodine receptors; CaMKII: Ca2+/calmodulin-dependent protein kinase II; PDGF: platelet-derived growth factor; TGF-β: transforming growth factor β; MAPK: mitogen-activated protein kinase; AMP: adenosine-monophosphate; β-ad: β-adrenergic receptor; AT1-R: angiotensin receptor 1; NLRP3: NACHT, LRR, and PYD domain containing protein 3 inflammasome; ROS: radical oxygen species.
2.1. At Risk for Atrial Fibrillation
2.1.1. Genetic Substrate
To develop AF, the well-known ectopic activity needs a histological and electrophysiological substrate. Several genetic polymorphisms and mutations have been identified that encode genes associated with ion channel function, calcium handling, transcription factors, and cardiac development and function that have been described elsewhere [15]. Nonetheless, for most people, these associations do not explain the entirety of the disease and only place them as a group that is at risk of developing AF [16]. Familial AF adds up to only 10–15% of AF cases [15], and generally present an earlier onset, in people that may lack traditional risk factors, which has also been called lone-AF. These monogenic paradigms have helped to gain understanding of the mechanisms that generate AF in an otherwise healthy tissue.
2.1.2. Age-Related Remodeling
Age is one of the most well-known risk factors for developing AF, with a lifetime risk of 40% and 50% of patients with AF aged 75 and older [17]. Age-related cardiomyocyte loss produces fibrosis [18], and the automaticity in the sinoatrial node involves hyperpolarization-activated cyclic nucleotide-gated (HCN) channels, whose expression ha shown an age-dependent increase in animal models, which may have a role in atrial ectopy [11]. Other electrophysiological and conduction changes that lead to Ca2+ mishandling, prolongation in the action potential duration (APD), effective refractory period (ERP) depolarization, and connexin downregulation also promote arrhythmogenesis [19]. In addition, older patients have a higher incidence of cardiovascular comorbidities like hypertension, HF, and valvular heart disease, and their atrial tissue has been exposed for a longer period to different stressors and remodeling processes [18].
2.1.3. Disease-Related Remodeling
Environmental factors play a key role in the development of AF in most patients. It is estimated that hypertension, in particular high systolic blood pressure, is responsible for 14% of all cases of AF [20]. Obesity provides a proinflammatory, metabolic, and comorbid context that leads these patients to be at high risk of developing cardiovascular disease (CVD) [21]. Insulin resistance is linked to endothelial dysfunction that results from a mismatch between mitogen-activated protein kinase (MAPK) and phosphatidylinositol 3-kinase (PI3K) pathways, which increases endothelial cell death and inflammation [22], and in diabetes, hyperglycaemia leads to advanced glycation end products that lead to fibrosis and hypertrophy. Other factors like lifestyle and diet have shown harmful, but also potentially protective effects in susceptibility to AF [22]. Regarding cardiovascular comorbidities, HF is associated with increased atrial filling pressure that lead to atrial dilation and wall stretch. This histologically translates to a “tear and scar” mechanism that generates fibrosis [23]. A similar situation occurs with valvular heart diseases.
Current classification includes subclinical AF defined as an individual without symptoms attributable to AF, in whom AF is not previously diagnosed and presents an atrial high-rate episode detected by an insertable cardiac or wearable monitor [1]. It is still not clear in which patients the use of devices for primary prevention might be beneficial, but many predictors and risk factors have been identified that include but are not limited to the aforementioned [24]. Guidelines recommend an opportunistic screening in patients with 65 years old or more [1]. Nonetheless, considering the rapidly growing wearable technology and artificial intelligence AF models, researchers believe that defining a group of patients at risk of AF, which has a clear pathophysiological basis, may prove useful for early detection strategies of AF.
2.2. Paroxysmal Atrial Fibrillation
During normal atrial action potential, the cardiac voltage-dependent Na+ channel produces the depolarizing current (INa) that triggers the activation of L-type Ca2+ channels that is responsible for the calcium-induced calcium release from the sarcoplasmic reticulum (SR). Ca2+ is released by ryanodine receptors (RyR2), its uptake into the SR is mediated by the SR Ca2+-adenosine triphosphate (SERCA2a), and inside the SR it is bound to calsequestrin. SERCA2a function is limited by the inhibitory subunit phospholamban. Meanwhile, delayed-rectifier K+ currents (IKr, IKs, IKur) and the transient-outward K+ current (Ito) control the repolarization and determine the action potential duration (APD) [25].
The hallmarks in paroxysmal AF are the focal ectopic activity and a re-entry substrate prone to abnormal conduction, that are major determinants in AF onset and perpetuation [7]. PVs are the main source of ectopic activity in AF [26]. Their structure has branching fibres with limited lateral coupling and abrupt changes in their orientation. This provides an adequate anatomic substrate for spontaneous activity and re-entry. In patients with AF, PVs have shown a shorter effective refractory period (ERP), lower voltage, shorter muscle sleeves, slower conduction, and more complex signals [27]. These characteristics make them prone to develop delayed afterdepolarizations (DAD) or early afterdepolarizations (EAD) [11].
A longer APD allows L-type Ca2+ channels to recover from inactivation, which causes EAD. This may be due to loss of repolarizing K+ current, or a persistent or late Na+ current, such as in long-QT syndrome type 3 [28]. DADs are originated mainly from the abnormal release of Ca2+ from the SR during diastole, which is then exchanged for extracellular Na+ by the Na+-Ca2+ exchanger type 1 (NCX1) that leads to cell depolarization when it reaches a threshold [13]. Automatism abnormalities may also be a causing or perpetuating factor, since HCN channels that control automatism in the sinoatrial node have shown an increased expression in patients with AF. Nonetheless, their role in this disease is still not fully understood [11].
Regarding the second hallmark, the determinants for conduction are the structural integrity, cell-to-cell coupling, and the rapid phase of Na+-current. Alterations in these factors may come from fibrosis and fibroblasts differentiation into myofibroblasts that may promote ectopic activity; mutations of repolarizing K+ channels that produce a gain of function, some nucleoporin mutations (Nup155); and Na+ channel loss of function that can reduce the ERP and lead to a substrate favorable for re-entry [11].
The development of these two hallmarks is independent, and in some patients one of them may be dominant. Most of them respond well to pulmonary vein isolation (PVI), but some may experience recurrence [29]. When AF is established, it generates electrical and structural changes that promote its own maintenance, progression, and stabilization [30][31].
2.3. Persistent Atrial Fibrillation
Persistent AF (PeAF) is defined as AF that is continuously sustained beyond 7 days [1]. The progression to this stage has been associated with cardiovascular events, hospitalizations, and death [32]. It has structural and electrophysiological differences by means of which AF can sustain itself and progress [33]. These are classified into four hallmarks: Structural remodeling, electrophysiological remodeling, neurohormonal remodeling, and inflammation.
2.3.1. Structural Remodeling
Fibrosis plays a central role in the pathogenesis of AF. Atrial fibrous-tissue content, and therefore left atrial wall thickness, is increased in patients with PeAF and atrial scarring, and correlates with clinical outcomes [34]. It is classified in reparative and interstitial fibrosis. The first occurs due to the replacement of lost cardiomyocytes, while the second occurs in response to cardiac inflammation or pressure overload, and is sub-classified into reactive fibrosis, which indicates the deposition of extracellular matrix without cell replacement, and infiltrative fibrosis as seen in amyloidosis [22][35].
There are many profibrotic pathways that are upregulated in patients with AF [35]. Increased angiotensin II plays a key role in atrial remodeling by binding to angiotensin receptor 1 (AT1-R) that leads to the activation of the MAPK pathway, which regulates the expression of transforming growth factor β (TGF-β), connective tissue growth factor (CTGF) [36], plasminogen activator inhibitor (PAI-1), and matrix metalloproteinases, that are proinflammatory and profibrotic [35]. TGF-β promotes the synthesis of collagen fibres by cardiac fibroblasts and their differentiation into myofibroblasts. In addition, AT1-R is coupled with G protein that activates phospholipase C to mediate the increase in Ca2+ in the cytoplasm, which also promotes fibroblast proliferation and differentiation [37].
Experimental models have demonstrated that suppressing this pathway leads to a reduction in interstitial fibrosis by inhibiting both the mineralocorticoid receptor and the AT1-R [38][39]. This correlates with clinical trials, that have shown the efficacy of the inhibition of this axis for primary prevention of AF, especially in hypertension and heart failure populations, and in preventing AF recurrence after cardioversion and in patients with paroxysmal AF under medical therapy [40][41][42][43], which suggest a potential role for these therapeutic targets in AF secondary prevention. Nonetheless, this has not shown a reduction in mortality [44].
Another key component that suffers from AF remodeling is the sarcomeric cytoskeleton. This organelle supports mechanical contraction, signal transduction, and the transport of ubiquitinated proteins. AF generates mechanical stress and cytoskeletal protein damage that reach a failure in the protein quality control system [15].
Fibrosis leads to AF perpetuation in numerous ways. First, the excess of extracellular matrix creates a physical barrier for conduction, which induces re-entry. Second, the proliferation of fibroblasts and their differentiation into myofibroblasts lead to myofibroblast–cardiomyocyte interaction, that induce re-entry and spontaneous focal activity. Third, slowing conduction and APD reduction induce spontaneous depolarization. These alterations make the ideal substrate for AF.
2.3.2. Electrophysiological Remodeling
The main components of this hallmark include a SR Ca2+ overload and Ca2+ spontaneous release. Adrenergic stimulation, AT-1R, and oxidative stress cause the activation of the Ca2+/calmodulin-dependent protein kinase II (CaMKII) and protein kinase A (PKA), that phosphorylates RyR2 and phospholamban, increasing intracellular Ca2+. A reduced expression, hyperphosphorylation of the inhibitory interacting proteins phospholamban or atrial-specific sarcolipin lead to an increase in the activity of SERCA2a [11]. Meanwhile, a high atrial rate causes the accumulation of intracellular Ca2+, which activates the Ca2+-dependent calcineurin/nuclear factor of activated T cells (NFAT), that leads to a decreased Ca2+ current, which shortens the APD. Increased intracellular Ca2+ upregulates the expression of K+ channels, which also shorten the APD [45]. A reduced APD increases the likelihood of DAD that may lead to spontaneous atrial ectopic activity [25]. The intracellular spontaneous calcium release is favored by RyR2 dysfunction that increases its opening probability. This can be due to loss of RyR2-associated calmodulin, or of juntophilin-2. Its hyperphosphorylation by CaMKII at Ser2814, 2808 or 2030 by PKA promotes RyR2 dysfunction [11].
Uncertainty remains regarding the precise electrophysiological mechanism that sustains AF. Three main mechanisms have been described, and they are not mutually exclusive [46].
-
Rotors: a re-entry mechanism that consists of a localized circular or spiral wavefront that rotates around an anatomical or functional obstacle, having heterogeneous conduction velocity and an unexcitable center that causes an irregular propagation of electrical activity.
-
Ectopic foci: abnormal regions within the atria that initiate electrical impulses spontaneously or in response to triggers.
-
Multiple wavelets: numerous re-entry circuits in the atria, that can interact with each other, merge, or divide.
2.3.3. Neurohormonal Remodeling
Increased sympathetic nervous system activity has been observed in patients with AF, secondary to an increase in atrial sympathetic nerve densities [47]. β-adrenergic stimulation causes different Ca2+ handling effects, including the activation of PKA and CaMKII that can cause EAD, SR Ca2+ overload, and Ca2+ spontaneous release, with the consecutive increase in spontaneous ectopic activity. Automaticity can be enhanced via α-adrenergic effect, which reduces IK1 activity, or for β-adrenergic activation which creates a self-promoting mechanism.
These patients also develop parasympathetic nervous system dysfunction, with a downregulation of M2 receptors, that lead to decreased responsiveness to acetylcholine (ACh) stimulation, and reduced vagal tone due to reduced ACh release from autonomic ganglia which modulate the electrical activity of PV [48].
As previously mentioned, AF leads to an increase in angiotensin II, that activates the MAPK and TGF-β signaling pathways. Another involved hormonal pathway in AF is atrial natriuretic peptide (ANP) dysregulation. ANP bind to natriuretic peptide receptor (NPR) type A, B, and C. NPR-A and -B have been linked with anti-remodeling effects; meanwhile, NPR-C internalizes them for their breakdown in lysosomes [49]. These peptides are involved in inflammation, oxidative stress, endothelial dysfunction, increase in the renin-angiotensin aldosterone system, and hypertension, all of which promote atrial remodeling [50]. Patients with AF have high levels of ANP, which has been associated with adverse outcomes [51].
2.3.4. Inflammation and Oxidative Stress
There is a close relationship between inflammation and the development of AF [52]. Multiple inflammatory mediators like IL-1β, IL-6, IL-8, IL-10, and TNF-α have increased levels in patients with AF [53]. Damaged cells lead to the activation of the NACHT, LRR, and PYD domain containing protein 3 inflammasome (NLRP3), that mediates a proinflammatory response with the release of IL-1β and IL-18. In animal models, NLRP3 has shown Ca2+ mishandling, APD abbreviation, and structural remodeling [11], and its genetic suppression prevents the development of AF [54].
Inflammation increases oxidative stress, which can directly affect ion channels and AP. In addition, NADPH oxidase can produce reactive oxygen species (ROS) that lead to myocyte apoptosis, fibrosis, and inflammation. They could also mediate the phosphorylation of RYR2 via CaMKII oxidation, that may provoke Ca2+ mishandling [22]. Separately, mitochondria and Ca2+ have a close relationship, regulating ATP synthesis and the production of ROS [55].
Another factor that has gained recent interest in AF progression is epicardial adipose tissue (EAT). It covers 80% of the heart’s surface and promotes local inflammation by producing proinflammatory cytokines and adipokines and has been associated with generation of fibrosis [56].
2.4. Permanent Atrial Fibrillation
Permanent AF is defined as AF accepted by the physician and the patient when no further rhythm control strategy will be undertaken [1]. This clinical decision may be taken under numerous reasons that go beyond the sole AF progression. There is not a single factor that turns AF from “reversible” to “non-reversible”, but rather the establishment and progression of the aforementioned that evolve until the return to sinus rhythm may not prove beneficial.
Recent trials have shown better outcomes for patients with a restored sinus rhythm compared with only rate control in patients with AF and associated HF or cardiomyopathy [57][58]. Therefore, it is key to aim for an early rhythm control to prevent this cascade of events, and the adverse clinical outcomes for patients.
3. Clinical Implications of Atrial Fibrillation
AF is associated with various complications, impaired quality of life, and increased morbidity and mortality. Understanding the clinical implications of AF is crucial for effective management and treatment.
3.1. Quality of Life
Impaired quality of life (QoL) has been reported in at least 60% of patients with AF, but only 17% experience disabling symptoms, having a higher impact in women, younger patients, and those with comorbidities [59]. Furthermore, the ORBIT AF cohort study [60], that evaluated patients with the AF-specific quality of life questionnaire (AFECQT) concluded that female sex and a New York Heart Association HF classification III or IV were the factors most strongly associated with impairment in daily activities.
3.2. Hospitalizations
Patients with AF have an annual hospitalization rate of 10–40%. It is estimated that 30% of patients are hospitalized once a year, and 10% are hospitalized at least twice a year, representing a two-fold incidence compared to patients in sinus rhythm (37.5% vs. 17.5%) [61]. The most frequent causes of these hospitalizations are stroke (49%), non-cardiac causes (43%), and bleeding (8%) [60].
3.3. Increased Risk of Mortality
The risk of mortality is described as 1.5–3.5 times higher compared to patients in sinus rhythm [62]. Additionally, AF patients have other cardiovascular risk factors and comorbidities that independently increase their mortality. In the Framingham Cohort Study [63], AF was associated with an odds ratio (OR) of 1.5 in men and 1.9 in women for mortality, and the risk of AF-related mortality did not significantly vary with age. In the RELY study [64], which randomized 18,113 patients, a total of 1371 deaths occurred within an average follow-up period of 400 days, resulting in an annual mortality rate of 3.84%. The main cause of death was cardiac (37.35%), including both sudden cardiac death (22.25%) and progressive HF (15.1%). Vascular aetiology deaths (10.14%) were mainly reported as due to stroke/peripheral embolism (7%), bleeding (2.84%), and pulmonary embolism (0.29%). Non-cardiovascular causes accounted for 35.81% of deaths and were primarily attributed to cancer (13.93%), respiratory failure (5.76%), infections (4.45%), and indeterminate causes (2.77%).
3.4. Stroke and Embolism
Patients with AF have an increased risk of stroke up to 5 times, accounting for 20–30% of strokes, and is suspected of being the cause of most cryptogenic strokes [65]. Ischemic stroke or transient ischemic attack (TIA) represents the initial manifestation of AF in 2–5% of patients [66]. AF-related strokes have a higher risk of disability and mortality when compared to stroke patients in general [67]. Patients with AF also have higher risk of systemic embolism, affecting the lower extremities (60%), the mesenteric region (30%), and upper extremities (10%) [68].
3.5. Heart Failure
The incidence of HF has been reported as 33%, 44%, and 56% in patients with paroxysmal, persistent, and permanent AF, respectively [69]. Additionally, both preserved (HFpEF) and reduced (HFrEF) ejection fraction HF are at least twice as common in patients with AF compared to those in sinus rhythm, with HFpEF being more frequently associated [70]. In the Framingham Heart Study, about 30% of HFpEF patients had AF, and it is estimated that 62% of HFpEF patients will develop AF at some point in their lives, which is significantly higher than in HFrEF patient cohorts [71]. In a Swedish HF registry of 41,466 patients, it was concluded that AF was more prevalent with higher ejection fractions. However, patients with AF had a similar increase in the risk of death, HF hospitalization, and stroke compared to patients in sinus rhythm, regardless of ejection fraction [72].
3.6. Neuropsychiatric Disorders
Depression has been described in 16–20% of patients, and there is a higher risk of cognitive impairment and vascular dementia (HR 1.4 and 1.6, respectively) independent of prior stroke history [73].
Regarding subclinical AF, the estimated incidence is 30% depending on the screening method used [74]. Its clinical significance is mainly related to three conditions: The risk of cerebral and systemic embolism, arrhythmia burden over a certain period, and the possibility of progression to clinical AF [75].
Given the clinical implications described for AF and considering its increasing prevalence in parallel with population aging, it is currently considered a public health problem with significant associated healthcare costs.
References
- Hindricks, G.; Potpara, T.; Dagres, N.; Bax, J.J.; Boriani, G.; Dan, G.A.; Fauchier, L.; Kalman, J.M.; Lane, D.A.; Lettino, M.; et al. 2020 ESC Guidelines for the Diagnosis and Management of Atrial Fibrillation Developed in Collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the Diagnosis and Management of Atrial Fibrillation of the European Society of Cardiology (ESC) Developed with the Special Contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498.
- Cheniti, G.; Vlachos, K.; Pambrun, T.; Hooks, D.; Frontera, A.; Takigawa, M.; Bourier, F.; Kitamura, T.; Lam, A.; Martin, C.; et al. Atrial Fibrillation Mechanisms and Implications for Catheter Ablation. Front. Physiol. 2018, 9, 1458.
- Michaud, G.F.; Stevenson, W.G. Atrial Fibrillation. N. Engl. J. Med. 2021, 384, 353–361.
- Kornej, J.; Börschel, C.S.; Benjamin, E.J.; Schnabel, R.B. Epidemiology of Atrial Fibrillation in the 21st Century. Circ. Res. 2020, 127, 4–20.
- Prystowsky, E.N. Rate Versus Rhythm Control for Atrial Fibrillation: Has the Debate Been Settled? Circulation 2022, 146, 1561–1563.
- Wyse, D.G.; Waldo, A.L.; DiMarco, J.P.; Domanski, M.J.; Rosenberg, Y.; Schron, E.B.; Kellen, J.C.; Greene, H.L.; Mickel, M.C.; Dalquist, J.E.; et al. A Comparison of Rate Control and Rhythm Control in Patients with Atrial Fibrillation. N. Engl. J. Med. 2002, 347, 1825–1833.
- Heijman, J.; Voigt, N.; Nattel, S.; Dobrev, D. Cellular and Molecular Electrophysiology of Atrial Fibrillation Initiation, Maintenance, and Progression. Circ. Res. 2014, 114, 1483–1499.
- Kirchhof, P.; Camm, A.J.; Goette, A.; Brandes, A.; Eckardt, L.; Elvan, A.; Fetsch, T.; van Gelder, I.C.; Haase, D.; Haegeli, L.M.; et al. Early Rhythm-Control Therapy in Patients with Atrial Fibrillation. N. Engl. J. Med. 2020, 383, 1305–1316.
- Willems, S.; Borof, K.; Brandes, A.; Breithardt, G.; Camm, A.J.; Crijns, H.J.G.M.; Eckardt, L.; Gessler, N.; Goette, A.; Haegeli, L.M.; et al. Systematic, Early Rhythm Control Strategy for Atrial Fibrillation in Patients with or without Symptoms: The EAST-AFNET 4 Trial. Eur. Heart J. 2022, 43, 1219–1230.
- Camm, A.J.; Naccarelli, G.V.; Mittal, S.; Crijns, H.J.G.M.; Hohnloser, S.H.; Ma, C.S.; Natale, A.; Turakhia, M.P.; Kirchhof, P. The Increasing Role of Rhythm Control in Patients With Atrial Fibrillation: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2022, 79, 1932–1948.
- Nattel, S.; Heijman, J.; Zhou, L.; Dobrev, D. Molecular Basis of Atrial Fibrillation Pathophysiology and Therapy: A Translational Perspective. Circ. Res. 2020, 127, 51–72.
- Potpara, T.S.; Lip, G.Y.H.; Blomstrom-Lundqvist, C.; Boriani, G.; Van Gelder, I.C.; Heidbuchel, H.; Hindricks, G.; Camm, A.J. The 4S-AF Scheme (Stroke Risk; Symptoms; Severity of Burden; Substrate): A Novel Approach to In-Depth Characterization (Rather than Classification) of Atrial Fibrillation. Thromb. Haemost. 2021, 121, 270–278.
- Nattel, S.; Dobrev, D. Electrophysiological and Molecular Mechanisms of Paroxysmal Atrial Fibrillation. Nat. Rev. Cardiol. 2016, 13, 575–590.
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, E895–E1032.
- Brundel, B.J.J.M.; Ai, X.; Hills, M.T.; Kuipers, M.F.; Lip, G.Y.H.; de Groot, N.M.S. Atrial Fibrillation. Nat. Rev. Dis. Primers 2022, 8, 21.
- Young, L.J.; Antwi-Boasiako, S.; Ferrall, J.; Wold, L.E.; Mohler, P.J.; El Refaey, M. Genetic and Non-Genetic Risk Factors Associated with Atrial Fibrillation. Life Sci. 2022, 299, 120529.
- Weng, L.C.; Preis, S.R.; Hulme, O.L.; Larson, M.G.; Choi, S.H.; Wang, B.; Trinquart, L.; McManus, D.D.; Staerk, L.; Lin, H.; et al. Genetic Predisposition, Clinical Risk Factor Burden, and Lifetime Risk of Atrial Fibrillation. Circulation 2018, 137, 1027–1038.
- Wasmer, K.; Eckardt, L.; Breithardt, G. Predisposing Factors for Atrial Fibrillation in the Elderly. J. Geriatr. Cardiol. 2017, 14, 179.
- Laredo, M.; Waldmann, V.; Khairy, P.; Nattel, S. Age as a Critical Determinant of Atrial Fibrillation: A Two-Sided Relationship. Can. J. Cardiol. 2018, 34, 1396–1406.
- Andrade, J.; Khairy, P.; Dobrev, D.; Nattel, S. The Clinical Profile and Pathophysiology of Atrial Fibrillation: Relationships among Clinical Features, Epidemiology, and Mechanisms. Circ. Res. 2014, 114, 1453–1468.
- Vyas, V.; Lambiase, P. Obesity and Atrial Fibrillation: Epidemiology, Pathophysiology and Novel Therapeutic Opportunities. Arrhythm. Electrophysiol. Rev. 2019, 8, 28.
- Sagris, M.; Vardas, E.P.; Theofilis, P.; Antonopoulos, A.S.; Oikonomou, E.; Tousoulis, D. Atrial Fibrillation: Pathogenesis, Predisposing Factors, and Genetics. Int. J. Mol. Sci. 2021, 23, 6.
- Verhaert, D.V.M.; Brunner-La Rocca, H.P.; Van Veldhuisen, D.J.; Vernooy, K. The Bidirectional Interaction between Atrial Fibrillation and Heart Failure: Consequences for the Management of Both Diseases. Europace 2021, 23, ii40.
- Kashou, A.H.; Adedinsewo, D.A.; Noseworthy, P.A. Subclinical Atrial Fibrillation: A Silent Threat with Uncertain Implications. Annu. Rev. Med. 2022, 73, 355–362.
- Nattel, S.; Harada, M. Atrial Remodeling and Atrial Fibrillation: Recent Advances and Translational Perspectives. J. Am. Coll. Cardiol. 2014, 63, 2335–2345.
- Haïssaguerre, M.; Jaïs, P.; Shah, D.C.; Takahashi, A.; Hocini, M.; Quiniou, G.; Garrigue, S.; Le Mouroux, A.; Le Métayer, P.; Clémenty, J. Spontaneous Initiation of Atrial Fibrillation by Ectopic Beats Originating in the Pulmonary Veins. N. Engl. J. Med. 1998, 339, 659–666.
- Teh, A.W.; Kistler, P.M.; Lee, G.; Medi, C.; Heck, P.M.; Spence, S.; Morton, J.B.; Sanders, P.; Kalman, J.M. Electroanatomic Properties of the Pulmonary Veins: Slowed Conduction, Low Voltage and Altered Refractoriness in AF Patients. J. Cardiovasc. Electrophysiol. 2011, 22, 1083–1091.
- Benito, B.; Brugada, R.; Perich, R.M.; Lizotte, E.; Cinca, J.; Mont, L.; Berruezo, A.; Tolosana, J.M.; Freixa, X.; Brugada, P.; et al. A Mutation in the Sodium Channel Is Responsible for the Association of Long QT Syndrome and Familial Atrial Fibrillation. Heart Rhythm. 2008, 5, 1434–1440.
- Kottkamp, H.; Tanner, H.; Kobza, R.; Schirdewahn, P.; Dorszewski, A.; Gerds-Li, J.H.; Carbucicchio, C.; Piorkowski, C.; Hindricks, G. Time Courses and Quantitative Analysis of Atrial Fibrillation Episode Number and Duration after Circular plus Linear Left Atrial Lesions: Trigger Elimination or Substrate Modification: Early or Delayed Cure? J. Am. Coll. Cardiol. 2004, 44, 869–877.
- Wijffels, M.C.E.F.; Kirchhof, C.J.H.J.; Dorland, R.; Allessie, M.A. Atrial Fibrillation Begets Atrial Fibrillation: A Study in Awake Chronically Instrumented Goats. Circulation 1995, 92, 1954–1968.
- Goette, A.; Honeycutt, C.; Langberg, J.J. Electrical Remodeling in Atrial Fibrillation. Time Course and Mechanisms. Circulation 1996, 94, 2968–2974.
- Piccini, J.P.; Passman, R.; Turakhia, M.; Connolly, A.T.; Nabutovsky, Y.; Varma, N. Atrial Fibrillation Burden, Progression, and the Risk of Death: A Case-Crossover Analysis in Patients with Cardiac Implantable Electronic Devices. Europace 2019, 21, 404–413.
- Lau, D.H.; Linz, D.; Schotten, U.; Mahajan, R.; Sanders, P.; Kalman, J.M. Pathophysiology of Paroxysmal and Persistent Atrial Fibrillation: Rotors, Foci and Fibrosis. Heart Lung Circ. 2017, 26, 887–893.
- Beyer, C.; Tokarska, L.; Stühlinger, M.; Feuchtner, G.; Hintringer, F.; Honold, S.; Fiedler, L.; Schönbauer, M.S.; Schönbauer, R.; Plank, F. Structural Cardiac Remodeling in Atrial Fibrillation. JACC Cardiovasc. Imaging 2021, 14, 2199–2208.
- Li, C.Y.; Zhang, J.R.; Hu, W.N.; Li, S.N. Atrial Fibrosis Underlying Atrial Fibrillation (Review). Int. J. Mol. Med. 2021, 47, 9.
- Gu, J.; Liu, X.; Wang, Q.X.; Tan, H.W.; Guo, M.; Jiang, W.F.; Zhou, L. Angiotensin II Increases CTGF Expression via MAPKs/TGF-Β1/TRAF6 Pathway in Atrial Fibroblasts. Exp. Cell Res. 2012, 318, 2105–2115.
- Harada, M.; Luo, X.; Qi, X.Y.; Tadevosyan, A.; Maguy, A.; Ordog, B.; Ledoux, J.; Kato, T.; Naud, P.; Voigt, N.; et al. Transient Receptor Potential Canonical-3 Channel-Dependent Fibroblast Regulation in Atrial Fibrillation. Circulation 2012, 126, 2051–2064.
- Sakabe, M.; Fujiki, A.; Nishida, K.; Sugao, M.; Nagasawa, H.; Tsuneda, T.; Mizumaki, K.; Inoue, H. Enalapril Prevents Perpetuation of Atrial Fibrillation by Suppressing Atrial Fibrosis and Over-Expression of Connexin43 in a Canine Model of Atrial Pacing-Induced Left Ventricular Dysfunction. J. Cardiovasc. Pharmacol. 2004, 43, 851–859.
- Tsai, C.F.; Yang, S.F.; Chu, H.J.; Ueng, K.C. Cross-Talk between Mineralocorticoid Receptor/Angiotensin II Type 1 Receptor and Mitogen-Activated Protein Kinase Pathways Underlies Aldosterone-Induced Atrial Fibrotic Responses in HL-1 Cardiomyocytes. Int. J. Cardiol. 2013, 169, 17–28.
- Schneider, M.P.; Hua, T.A.; Böhm, M.; Wachtell, K.; Kjeldsen, S.E.; Schmieder, R.E. Prevention of Atrial Fibrillation by Renin-Angiotensin System Inhibition. J. Am. Coll. Cardiol. 2010, 55, 2299–2307.
- Ma, H.; Jiang, H.; Feng, J.; Gan, Y. Angiotensin Receptor Blocker and Calcium Channel Blocker Preventing Atrial Fibrillation Recurrence in Patients with Hypertension and Atrial Fibrillation: A Meta-Analysis. Cardiovasc. Ther. 2021, 2021, 6628469.
- Fogari, R.; Zoppi, A.; Maffioli, P.; Mugellini, A.; Preti, P.; Perrone, T.; Derosa, G. Effect of Telmisartan on Paroxysmal Atrial Fibrillation Recurrence in Hypertensive Patients with Normal or Increased Left Atrial Size. Clin. Cardiol. 2012, 35, 359–364.
- Li, T.J.; Zang, W.D.; Chen, Y.L.; Geng, N.; Ma, S.M.; Li, X.D. Renin-Angiotensin System Inhibitors for Prevention of Recurrent Atrial Fibrillation: A Meta-Analysis. Int. J. Clin. Pract. 2013, 67, 536–543.
- Chaugai, S.; Sherpa, L.Y.; Sepehry, A.A.; Arima, H.; Wang, D.W. Effect of RAAS Blockers on Adverse Clinical Outcomes in High CVD Risk Subjects with Atrial Fibrillation: A Meta-Analysis and Systematic Review of Randomized Controlled Trials. Medicine 2016, 95, e4059.
- Voigt, N.; Trausch, A.; Knaut, M.; Matschke, K.; Varró, A.; Van Wagoner, D.R.; Nattel, S.; Ravens, U.; Dobrev, D. Left-to-Right Atrial Inward Rectifier Potassium Current Gradients in Patients with Paroxysmal versus Chronic Atrial Fibrillation. Circ. Arrhythm. Electrophysiol. 2010, 3, 472–480.
- Wijesurendra, R.S.; Casadei, B. Mechanisms of Atrial Fibrillation. Heart 2019, 105, 1860–1867.
- Chen, P.S.; Chen, L.S.; Fishbein, M.C.; Lin, S.F.; Nattel, S. Role of the Autonomic Nervous System in Atrial Fibrillation: Pathophysiology and Therapy. Circ. Res. 2014, 114, 1500–1515.
- Rebecchi, M.; Panattoni, G.; Edoardo, B.; Ruvo, E.; de Sciarra, L.; Politano, A.; Sgueglia, M.; Ricagni, C.; Verbena, S.; Crescenzi, C.; et al. Atrial Fibrillation and Autonomic Nervous System: A Translational Approach to Guide Therapeutic Goals. J. Arrhythm. 2021, 37, 320–330.
- Goetze, J.P.; Bruneau, B.G.; Ramos, H.R.; Ogawa, T.; de Bold, M.K.; de Bold, A.J. Cardiac Natriuretic Peptides. Nat. Rev. Cardiol. 2020, 17, 698–717.
- Tanase, D.M.; Radu, S.; Al Shurbaji, S.; Baroi, G.L.; Costea, C.F.; Turliuc, M.D.; Ouatu, A.; Floria, M. Natriuretic Peptides in Heart Failure with Preserved Left Ventricular Ejection Fraction: From Molecular Evidences to Clinical Implications. Int. J. Mol. Sci. 2019, 20, 2629.
- Brady, P.F.; Chua, W.; Nehaj, F.; Connolly, D.L.; Khashaba, A.; Purmah, Y.J.V.; Ul-Qamar, M.J.; Thomas, M.R.; Varma, C.; Schnabel, R.B.; et al. Interactions Between Atrial Fibrillation and Natriuretic Peptide in Predicting Heart Failure Hospitalization or Cardiovascular Death. J. Am. Heart Assoc. 2022, 11, 22833.
- Zhou, X.; Dudley, S.C. Evidence for Inflammation as a Driver of Atrial Fibrillation. Front. Cardiovasc. Med. 2020, 7, 62.
- Scott, L.; Li, N.; Dobrev, D. Role of Inflammatory Signaling in Atrial Fibrillation. Int. J. Cardiol. 2019, 287, 195–200.
- Li, N.; Brundel, B.J.J.M. Inflammasomes and Proteostasis Novel Molecular Mechanisms Associated With Atrial Fibrillation. Circ. Res. 2020, 127, 73–90.
- Mason, F.E.; Pronto, J.R.D.; Alhussini, K.; Maack, C.; Voigt, N. Cellular and Mitochondrial Mechanisms of Atrial Fibrillation. Basic. Res. Cardiol. 2020, 115, 72.
- Abe, I.; Teshima, Y.; Kondo, H.; Kaku, H.; Kira, S.; Ikebe, Y.; Saito, S.; Fukui, A.; Shinohara, T.; Yufu, K.; et al. Association of Fibrotic Remodeling and Cytokines/Chemokines Content in Epicardial Adipose Tissue with Atrial Myocardial Fibrosis in Patients with Atrial Fibrillation. Heart Rhythm. 2018, 15, 1717–1727.
- Marrouche, N.F.; Brachmann, J.; Andresen, D.; Siebels, J.; Boersma, L.; Jordaens, L.; Merkely, B.; Pokushalov, E.; Sanders, P.; Proff, J.; et al. Catheter Ablation for Atrial Fibrillation with Heart Failure. N. Engl. J. Med. 2018, 378, 417–427.
- Prabhu, S.; Taylor, A.J.; Costello, B.T.; Kaye, D.M.; McLellan, A.J.A.; Voskoboinik, A.; Sugumar, H.; Lockwood, S.M.; Stokes, M.B.; Pathik, B.; et al. Catheter Ablation Versus Medical Rate Control in Atrial Fibrillation and Systolic Dysfunction: The CAMERA-MRI Study. J. Am. Coll. Cardiol. 2017, 70, 1949–1961.
- Freeman, J.V.; Simon, D.N.; Go, A.S.; Spertus, J.; Fonarow, G.C.; Gersh, B.J.; Hylek, E.M.; Kowey, P.R.; Mahaffey, K.W.; Thomas, L.E.; et al. Association between Atrial Fibrillation Symptoms, Quality of Life, and Patient Outcomes: Results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circ. Cardiovasc. Qual. Outcomes 2015, 8, 393–402.
- Steinberg, B.A.; Kim, S.; Fonarow, G.C.; Thomas, L.; Ansell, J.; Kowey, P.R.; Mahaffey, K.W.; Gersh, B.J.; Hylek, E.; Naccarelli, G.; et al. Drivers of Hospitalization for Patients with Atrial Fibrillation: Results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Am. Heart J. 2014, 167, 735–742.e2.
- Meyre, P.; Blum, S.; Berger, S.; Aeschbacher, S.; Schoepfer, H.; Briel, M.; Osswald, S.; Conen, D. Risk of Hospital Admissions in Patients With Atrial Fibrillation: A Systematic Review and Meta-Analysis. Can. J. Cardiol. 2019, 35, 1332–1343.
- Magnussen, C.; Niiranen, T.J.; Ojeda, F.M.; Gianfagna, F.; Blankenberg, S.; Njølstad, I.; Vartiainen, E.; Sans, S.; Pasterkamp, G.; Hughes, M.; et al. Sex Differences and Similarities in Atrial Fibrillation Epidemiology, Risk Factors and Mortality in Community Cohorts: Results from the BiomarCaRE. Circulation 2017, 136, 1588.
- Benjamin, E.J.; Wolf, P.A.; D’Agostino, R.B.; Silbershatz, H.; Kannel, W.B.; Levy, D. Impact of Atrial Fibrillation on the Risk of Death. Circulation 1998, 98, 946–952.
- Marijon, E.; Le Heuzey, J.Y.; Connolly, S.; Yang, S.; Pogue, J.; Brueckmann, M.; Eikelboom, J.; Themeles, E.; Ezekowitz, M.; Wallentin, L.; et al. Causes of Death and Influencing Factors in Patients with Atrial Fibrillation: A Competing-Risk Analysis from the Randomized Evaluation of Long-Term Anticoagulant Therapy Study. Circulation 2013, 128, 2192–2201.
- Kishore, A.; Vail, A.; Majid, A.; Dawson, J.; Lees, K.R.; Tyrrell, P.J.; Smith, C.J. Detection of Atrial Fibrillation after Ischemic Stroke or Transient Ischemic Attack: A Systematic Review and Meta-Analysis. Stroke 2014, 45, 520–526.
- Svennberg, E.; Engdahl, J.; Al-Khalili, F.; Friberg, L.; Frykman, V.; Rosenqvist, M. Mass Screening for Untreated Atrial Fibrillation: The STROKESTOP Study. Circulation 2015, 131, 2176–2184.
- Essa, H.; Hill, A.M.; Lip, G.Y.H. Atrial Fibrillation and Stroke. Card. Electrophysiol. Clin. 2021, 13, 243–255.
- Bekwelem, W.; Connolly, S.J.; Halperin, J.L.; Adabag, S.; Duval, S.; Chrolavicius, S.; Pogue, J.; Ezekowitz, M.D.; Eikelboom, J.W.; Wallentin, L.G.; et al. Extracranial Systemic Embolic Events in Patients with Nonvalvular Atrial Fibrillation: Incidence, Risk Factors, and Outcomes. Circulation 2015, 132, 796–803.
- Chiang, C.E.; Naditch-Brûlé, L.; Murin, J.; Goethals, M.; Inoue, H.; O-Neill, J.; Silva-Cardoso, J.; Zharinov, O.; Gamra, H.; Alam, S.; et al. Distribution and Risk Profile of Paroxysmal, Persistent, and Permanent Atrial Fibrillation in Routine Clinical Practice: Insight from the Real-Life Global Survey Evaluating Patients with Atrial Fibrillation International Registry. Circ. Arrhythm. Electrophysiol. 2012, 5, 632–639.
- Kotecha, D.; Lam, C.S.P.; Van Veldhuisen, D.J.; Van Gelder, I.C.; Voors, A.A.; Rienstra, M. Heart Failure With Preserved Ejection Fraction and Atrial Fibrillation: Vicious Twins. J. Am. Coll. Cardiol. 2016, 68, 2217–2228.
- Santhanakrishnan, R.; Wang, N.; Larson, M.G.; Magnani, J.W.; McManus, D.D.; Lubitz, S.A.; Ellinor, P.T.; Cheng, S.; Vasan, R.S.; Lee, D.S.; et al. Atrial Fibrillation Begets Heart Failure and Vice Versa: Temporal Associations and Differences in Preserved versus Reduced Ejection Fraction. Circulation 2016, 133, 484–492.
- Sartipy, U.; Dahlström, U.; Fu, M.; Lund, L.H. Atrial Fibrillation in Heart Failure With Preserved, Mid-Range, and Reduced Ejection Fraction. JACC Heart Fail. 2017, 5, 565–574.
- Kwok, C.S.; Loke, Y.K.; Hale, R.; Potter, J.F.; Myint, P.K. Atrial Fibrillation and Incidence of Dementia. Neurology 2011, 76, 914–922.
- Gherasim, L. Subclinical Atrial Fibrillation, Embolic Risk, and Anticoagulant Treatment. Maedica 2018, 13, 261.
- Alturki, A.; Marafi, M.; Russo, V.; Proietti, R.; Essebag, V. Medicina Subclinical Atrial Fibrillation and Risk of Stroke: Past, Present and Future. Medicina 2019, 55, 611.
More
Information
Subjects:
Others
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
699
Revisions:
2 times
(View History)
Update Date:
24 Aug 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




