Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Kyra Kaiser | -- | 2354 | 2023-08-17 17:39:25 | | | |
| 2 | Camila Xu | Meta information modification | 2354 | 2023-08-18 05:48:33 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Kaiser, K.G.; Delattre, V.; Frost, V.J.; Buck, G.W.; Phu, J.V.; Fernandez, T.G.; Pavel, I.E. Modern Antimicrobial Applications of Nanosilver. Encyclopedia. Available online: https://encyclopedia.pub/entry/48183 (accessed on 07 February 2026).
Kaiser KG, Delattre V, Frost VJ, Buck GW, Phu JV, Fernandez TG, et al. Modern Antimicrobial Applications of Nanosilver. Encyclopedia. Available at: https://encyclopedia.pub/entry/48183. Accessed February 07, 2026.
Kaiser, Kyra G., Victoire Delattre, Victoria J. Frost, Gregory W. Buck, Julianne V. Phu, Timea G. Fernandez, Ioana E. Pavel. "Modern Antimicrobial Applications of Nanosilver" Encyclopedia, https://encyclopedia.pub/entry/48183 (accessed February 07, 2026).
Kaiser, K.G., Delattre, V., Frost, V.J., Buck, G.W., Phu, J.V., Fernandez, T.G., & Pavel, I.E. (2023, August 17). Modern Antimicrobial Applications of Nanosilver. In Encyclopedia. https://encyclopedia.pub/entry/48183
Kaiser, Kyra G., et al. "Modern Antimicrobial Applications of Nanosilver." Encyclopedia. Web. 17 August, 2023.
Copy Citation
Silver has an extensive history because it has been used for multiple millennia spanning from the Before Common Era (B.C.E) to the present day. This long-term use of silver stemmed from its anti-deteriorative activity and led to its recognition as the most important antimicrobial agent (i.e., antibacterial, antiviral, antiparasitic, and antifungal) that predated antibiotics.
nanosilver
antimicrobial applications
physicochemical properties
1. Brief History of Silver (Ag) and Its Old Antimicrobial Applications
Silver has an extensive history because it has been used for multiple millennia spanning from the Before Common Era (B.C.E) to the present day (Table 1) [1][2][3]. This long-term use of silver stemmed from its anti-deteriorative activity and led to its recognition as the most important antimicrobial agent (i.e., antibacterial, antiviral, antiparasitic, and antifungal) that predated antibiotics [4][5][6][7][8][9].
Table 1. Overview of the knowledge and applications of silver (Ag) throughout major historical periods. Both household and medical applications are listed, as household use of silver contributed to the foundation of using silver as a therapeutic agent.
| Silver B.C.E. [1][4][7] |
Silver Pre-Industrialization [1][7] |
Silver during and Post Industrialization [8] |
|
|---|---|---|---|
| Knowledge |
|
|
|
| Applications |
|
|
|
Before Common Era (B.C.E.): The usage of silver for antibacterial purposes in B.C.E. civilizations was primarily through the preservation of food items in silver containers or the addition of a silver coin to beverages for long-term storage [1][9]. A fundamental discovery was the correlation between containers made of silver and food items remaining safe for consumption. Rulers of various nations (Alexander the Great and Cyrus the Great) only consumed water that was kept in silver vessels [1][6][10][11]. Even though bacteria were not known at that time, this connection between the slower decomposition of food with silver containers and cutlery contributed to the medical advancements seen today [8]. Due to the difficulty of interpretation of ancient texts, there are varying claims of the first recorded attempt of using silver as a therapeutic remedy. One of the oldest examples is a reference to silver as a therapeutic agent in 1500 B.C.E, during the Han dynasty in China [12]. Other recorded instances of medical procedures using silver include the 69 B.C.E. Roman Pharmacopeia describing a silver nitrate (AgNO3)-based medicine, the practice of Hippocrates using silver leaf for wound care, and an ancient medical system (Ayurveda) from India listing silver as a therapy component for multiple diseases [1][4][8][13].
Pre-industrialization: From B.C.E until the first Industrial Revolution in 1760, silver was used as a novel medical therapy for a broad spectrum of ailments (e.g., ulcers, wound infections, impure blood, heart palpitations, poor breath, epilepsy, and irritation) [1][14]. For example, Pliny the Elder, a Roman physician, described silver within his 79 C.E. (Common Era) book, Natural History (Book XXXIII), as an effective healing agent within plasters and for wound closing [11][15]. Ambroise Paré, a French surgeon considered among the fathers of surgery, who served for multiple kings (Henry II, Francis II, Charles IX, and Henry III), used silver and other materials to construct ocular prosthetics [4][16]. Wealthier individuals in the Middle Ages, who regularly used silver utensils, overexposed themselves to silver and developed argyria (Figure 1), a rare skin condition that changes the color of skin, eyes, nails, and internal organs to a permanent blue-grey [1][17][18].

Figure 1. Comparison of an argyria-like skin color characteristic to topical cyanosis (right), versus a simulated standard hand coloring in a healthy patient (left).
During industrialization: Key events such as the discovery of bacteria by Anton Leeuwenhoek in 1676 and the technological advancements associated with the Industrial Revolution in 1760 led to a transformation of medicine [2][19]. As antibiotics did not yet exist in the medical field, physicians used other agents (e.g., silver, mercury, copper, arsenic, and sulfur compounds) that were later deemed as beneficial, harmful, or entirely ineffective as therapeutic remedies [20]. Public attitudes toward health care were also drastically changed with the first public hospital, Bellevue Hospital, being officially established in New York City, in 1736 [21]. The concept of vaccination had its roots in 1796 through the work of physician Edward Jenner, who made the connection between patients who previously contracted cowpox and their immunity to smallpox [22]. He inoculated an 8-year-old boy with material from the cowpox lesions and concluded that the boy was protected from the illness [22]. This was the origin of transmittable protection, as in vaccination [23]. Vaccines were the most advanced medical agent, up until the 19th century, when the first antibiotic was discovered [24].
Post industrialization: In the 19th century, the physician Robert Koch made the claim that a certain bacterium can cause a specific disease. This led to Koch’s four postulates and the Germ Theory as it is seen today [25][26]. Following this, the physician Paul Ehrlich synthesized the first antimicrobial compound, salvarsan, in 1910 [24][27][28]. The physician scientist Alexander Fleming discovered the first true antibiotic to treat bacterial infections, penicillin, in 1928 [24][27][28]. Penicillin became available to the public later, in 1945 [29]. In this time, colloidal silver was being employed in hospital settings as an antibacterial agent, and silver salts were being administered to treat various infections and ailments (e.g., conjunctivitis, gonorrhea, gastroenteritis, syphilis, nicotine dependence, and mental illness) [8]. The German physician, Carl Siegmund Franz Credé, formulated in 1881 a 2% AgNO3 solution for neonatal conjunctivitis, which was so effective that it almost ended visual loss from the disease [8][30]. Other AgNO3 applications in the 1800s included therapies for burns, ulcers, compound fractures, and infections [1][31]. Physician Marion Sims employed to resolve the dilemma of post-delivery vesico-vaginal fistulas (when silk sutures failed) and administered silver-coated catheters during the healing period [1][31]. Colloidal silver (i.e., Ag particles suspended within a liquid) was first employed in 1891, by the surgeon B.C. Crede, as an antiseptic measure on wounds [1][12][32].
Silver (Ag) forms: As the scientific understanding of silver expanded over the course of history, the forms of Ag utilized also shifted (Figure 2). Initially, Ag was utilized in macro form (bulk Ag metal), when casting and forging household items (e.g., vessels, jewelry, and coins), or in atomic form (salt solutions of Ag+ ions), when treating wounds and other ailments. This was followed by the development and administration of micro- or nano-forms of Ag in water (colloidal Ag), as antibiotics were not yet available [8][28]. The first colloid of Ag was synthesized in the laboratory in 1889, by the chemist M. C. Lea [33][34]. In this redox reaction, citrate-capped AgNPs were intentionally created with dimensions of about 1–100 nanometers (nm) that changed their properties when compared to the Ag+ or bulk Ag forms [35]. However, the term nanotechnology was coined much later in 1974 by the Japanese professor Norio Taniguchi [36]. The first micro- and nanoparticles were visualized and characterized in 1981, after the invention of the first scanning tunneling microscope (STM). Nowadays, ionic silver (Ag+) and nanosilver (e.g., colloidal AgNPs) are the most emphasized forms of antimicrobial silver, which kill or inhibit the growth of microorganisms including pathogenic bacteria, viruses, and fungi, but cause little to no damage to the host.
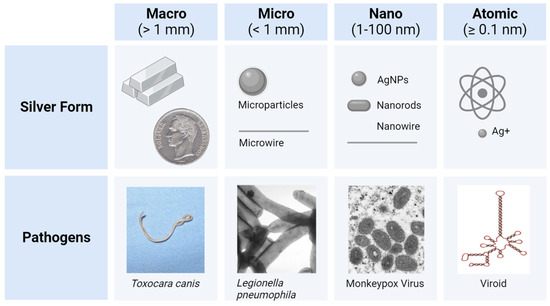
Figure 2. The forms of silver (Ag) utilized from B.C.E until present day, having sizes ranging from visible to the naked eye (1 mm and above) to approximately 0.1 nm (atomic radius and above) [35][37][38][39][40]. Various pathogens within each category (e.g., the Toxocara canis [usually 2–10 cm] and the pinworm Enterobius vermicularis [usually 1–3 mm] for macro pathogens >> 1 mm) depict a size comparison for the Ag forms [41][42][43][44]. Comparative scales are approximated.
2. Modern Antimicrobial Applications of Nanosilver
The antimicrobial activity of nanosilver such as colloidal silver nanoparticles (AgNPs) is linked to its unique, size-related physicochemical properties such as the very large surface-to-volume ratios and the potential release of Ag+ ions from the nanosurface under favorable redox conditions. These properties are currently exploited in the manufacturing of everyday consumer products and other antimicrobial applications (Figure 3) [4][5].
Antimicrobial consumer products: In 2023, 5367 consumer products have been identified worldwide as containing nanomaterials by the manufacturer, and over 1000 of these products exploit the unique properties of nanosilver (e.g., antimicrobial, optical, and catalytical) [45][46]. Antimicrobial consumer products containing silver (Figure 3) can be found in the health (24.08%), textile (17.53%), cosmetic (13.38%), appliance (9.31%), environmental (8.30%), and construction (7.93%) sectors [46]. In the last few decades, the U.S. Food and Drug Administration (FDA) has approved many of these products containing antimicrobial Ag+ and nanosilver such as AgNPs. Examples include wound dressings, facial masks, textile fibers, sanitizers, coatings of surgical tools, dental implants, and urinary catheters (Table 2) [45][47].
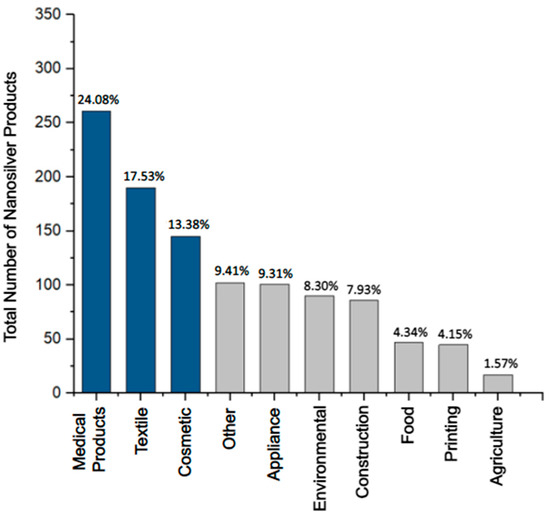
Figure 3. The most prevalent categories of consumer products containing nanosilver (U.S. FDA-approved and non-approved) make up 1084 registered products [46]. The top three sectors, the medical-, textile-, and cosmetics-related products (dark blue), are the most prominent categories, making up ~55% of the total number of consumer products containing nanosilver. The lesser seven categories (grey) make up ~45% of products.
“Silver wound dressings” represent the most web-searched (n = 2214—Table 2) and one of the most heavily used consumer products containing Ag in the medical sector. A large variety of U.S. FDA-approved (e.g., Silverlon, Aquacel Ag Advantage, and Acticoat) and non-approved wound dressings are offered through prescriptions as well as over the counter [48][49][50]. Silver-based wound dressings are used as both preventative and curative measures against bacterial infection of acute and chronic wounds. Textiles, the second most widespread application of nanosilver, have been used in many types of clothing (e.g., facemasks, socks, shirts, athletic wear, and towels) [45]. An illustrative example associated with nanosilver use is disinfectants in facemasks to prevent the spread of pathogens and the formation of malodor caused by bacterial colonies that inhabit the surface of the skin [51]. Manufacturers of cosmetics, the third largest sector, have employed nanosilver for the same antimicrobial benefits [52]. Nanosilver can be found in lotions, face masks, soaps, sunscreens, etc. [45].
Because the adverse effects of Ag on human health are not yet fully understood, concerns have been raised about the growing exposure to nanosilver during the manufacture or prolonged utilization of nanosilver-based consumer products [53]. Furthermore, the environmental health impacts of nanosilver remain under debate as nanosilver properties can change in the environment, leading to altered toxicity and stability [54][55][56]. The regulation of nanosilver-based consumer products has been compounded by the challenging task of tracking products that do not specify the nanomaterial as an ingredient, especially when in minute quantities, and by the product distribution under different brand names [57]. Nevertheless, the integration of nanosilver into consumer products continues to experience a vertiginous increase. An estimated 1000 tons of nanosilver is produced worldwide [58].
Table 2. The top applications of antimicrobial silver (Ag) together with illustrative products for each of the three major categories: health, textiles, and cosmetics. The vendor, the number of PubMed search results and selected key words, Ag form, [Ag quantities], product purpose, and U.S. FDA approval status are reported [49][59][60].
| Product Type | Search Result | Vendor | [Ag] and Ag Form | Purpose | U.S. FDA Approval |
|---|---|---|---|---|---|
| Silver-based wound dressings | “silver wound dressing” n = 2214 |
|
|
|
YES |
| Ankle socks with silver | “silver textile” n = 1155 |
|
|
|
NO |
| Platinum silver nanocolloid cream | “silver cosmetic” n = 2292 |
|
|
|
NO |
Other antimicrobial applications: Lately, AgNPs and Ag+ have received increased attention due to their potential use in the fight against two major global health threats, namely antibiotic resistance and viral infections, where treatments are either limited or not available [61]. For instance, non-cytotoxic concentrations of AgNPs were reported to act against a broad spectrum of viruses of different families regardless of their tropism, clade, and resistance to antiretrovirals [61][62][63]. Relevant examples include HIV-1, hepatitis B (HBV), Tacaribe virus, herpes simplex virus, mpox, smallpox, H1N1 influenza A, respiratory syncytial viruses, vaccinia virus, and dengue virus (DENV). In these studies, AgNPs were found to bind specifically or nonspecifically to proteins in the envelope of virions and thereby deactivate them (virucidal activity). These target proteins are mainly responsible for the viral interaction with host cells [13][61][62][63]. During the pre-viral entry into host cells, AgNPs competitively attach to the cells and lyse the membrane of the virions (antiviral activity). In the case of the post-viral entry, AgNPs mainly inhibit the viral fusion with the cell membrane, and in several cases interfered with the stages of the viral replication cycle such as the synthesis of viral RNA (antiviral activity). At the molecular level, these mechanisms relied on the chemical interaction of AgNPs or Ag+ ions released by AgNPs with sulfur, nitrogen, or phosphorus-containing biomolecules including proteins and genetic material. Hence, AgNPs have multiple mechanisms of action, which suggests that resistance to AgNPs will be less likely to arise when compared to specific antiviral or antibiotic therapies [64][65][66].
The World Health Organization (WHO) has published a list of high-priority (first tier), antibiotic-resistant pathogens that present the greatest threat to human health. These include strains in the Acinetobacter, Pseudomonas, and various Enterobacteriaceae genera (Klebsiella, Escherichia coli (E. coli), Serratia, and Proteus) [67]. Most of these pathogens are Gram-negative strains that exhibit increased resistance when compared to the Gram-positive strains. Gram-negative bacteria have an outer membrane that contains lipopolysaccharide (LPS), which creates a permeability barrier against external, harmful factors [68]. For example, Pseudomonas aeruginosa (P. aeruginosa), a Gram-negative species that nanosilver-based products are commonly tested against, is listed as Priority 1 because the organism is CRITICAL due to its resistance to carbapenem antibiotics that are used as “last line” or “last resort” antibiotics [67][69]. Four of the six multi-drug-resistant (MDR) pathogens that are primarily responsible for infections originating from hospitalization are also Gram-negative bacteria, labeled as ESKAPE pathogens (Enterococcus faecium (E. faecium), Staphylococcus aureus (S. aureus), Klebsiella pneumoniae (K. pneumoniae), Acinetobacter baumannii (A. baumannii), P. aeruginosa, and Enterobacter species) [70].
References
- Alexander, J.W. History of the medical use of silver. Surg. Infect. 2009, 10, 289.
- Lane, N. The unseen world: Reflections on Leeuwenhoek (1677) ‘Concerning Little Animals’. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2015, 370, 20140344.
- Lobanovska, M.; Pilla, G. Penicillin’s Discovery and Antibiotic Resistance: Lessons for the Future? Yale J. Biol. Med. 2017, 90, 135–145.
- Barillo, D.J.; Marx, D.E. Silver in medicine: A brief history BC 335 to present. Burns 2014, 40, S3–S8.
- Mijnendonckx, K.; Leys, N.; Mahillon, J.; Silver, S.; Van Houdt, R. Antimicrobial silver: Uses, toxicity and potential for resistance. Biometals 2013, 26, 609–621.
- Barras, F.; Aussel, L.; Ezraty, B. Silver and Antibiotic, New Facts to an Old Story. Antibiotics 2018, 7, 79.
- White, R.J. An historical overview of the use of silver in wound management. Br. J. Nurs. 2001, 10, 16079.
- Medici, S.; Peana, M.; Nurchi, V.M.; Zoroddu, M.A. Medical Uses of Silver: History, Myths, and Scientific Evidence. J. Med. Chem. 2019, 62, 5923–5943.
- Turner, R.J. Is Silver the Ultimate Antimicrobial Bullet? Antibiotics 2018, 7, 112.
- Wallner, C.; Moormann, E.; Lulof, P.; Drysch, M.; Lehnhardt, M.; Behr, B. Burn Care in the Greek and Roman Antiquity. Medicina 2020, 56, 657.
- Davies, R.L.; Etris, S.F. The development and functions of silver in water purification and disease control. Catal. Today 1997, 36, 107–114.
- Sim, W.; Barnard, R.T.; Blaskovich, M.A.T.; Ziora, Z.M. Antimicrobial Silver in Medicinal and Consumer Applications: A Patent Review of the Past Decade (2007–2017). Antibiotics 2018, 7, 93.
- Lara, H.H.; Garza-Treviño, E.N.; Ixtepan-Turrent, L.; Singh, D.K. Silver nanoparticles are broad-spectrum bactericidal and virucidal compounds. J. Nanobiotechnol. 2011, 9, 30.
- Dingledine, R.; Hassel, B. A New Approach for Epilepsy. Cerebrum 2016, 2016, cer-07-16.
- Borsuk, D.E.; Gallant, M.; Richard, D.; Williams, H.B. Silver-coated nylon dressings for pediatric burn victims. Can. J. Plast. Surg. 2007, 15, 29–31.
- Hernigou, P. Ambroise Paré’s life (1510–1590): Part I. Int. Orthop. 2013, 37, 543–547.
- Jerger, S.E.; Parekh, U. Argyria. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023.
- Park, S.W.; Shin, H.T.; Lee, K.T.; Lee, D.Y. Medical concern for colloidal silver supplementation: Argyria of the nail and face. Ann. Dermatol. 2013, 25, 111–112.
- Yano, M.; Furukawa, Y. Two-dimensional constrained chaos and industrial revolution cycles. Proc. Natl. Acad. Sci. USA 2023, 120, e2117497120.
- Landecker, H. Antimicrobials before antibiotics: War, peace, and disinfectants. Palgrave Commun. 2019, 5, 45.
- Fiani, B.; Covarrubias, C.; Jarrah, R.; Kondilis, A.; Doan, T.M. Bellevue Hospital, the Oldest Public Health center in the United States of America. World Neurosurg. 2022, 167, 57–61.
- CDC.gov. Available online: https://www.cdc.gov/smallpox/history/history.html#:~:text=Edward%20Jenner%20(1749%E2%80%931823 (accessed on 25 June 2023).
- Riedel, S. Edward Jenner and the history of smallpox and vaccination. In Baylor University Medical Center Proceedings; Taylor & Francis: New York, NY, USA, 2005; Volume 18, pp. 21–25.
- Sakai, T.; Morimoto, Y. The History of Infectious Diseases and Medicine. Pathogens 2022, 11, 1147.
- National Research Council (US) Committee to Update Science, Medicine, and Animals. A Theory of Germs. In Science, Medicine, and Animals, 2nd ed.; National Academy Press: Washington, DC, USA, 2004; pp. 7–8.
- Casanova, J.-L.; Abel, L. The Genetic Theory of Infectious Diseases: A Brief History and Selected Illustrations. Annu. Rev. Genom. Hum. Genet. 2016, 14, 215–243.
- Christensen, S.B. Drugs That Changed Society: History and Current Status of the Early Antibiotics: Salvarsan, Sulfonamides, and β-Lactams. Molecules 2021, 26, 6057.
- Williams, K.J. The introduction of ‘chemotherapy’using arsphenamine–The first magic bullet. J. R. Soc. Med. 2009, 102, 343–348.
- ACS.org. Available online: https://www.acs.org/education/whatischemistry/landmarks/flemingpenicillin.html (accessed on 25 June 2023).
- Simon, J.W. Povidone-iodine prophylaxis of ophthalmia neonatorum. Br. J. Ophthalmol. 2003, 87, 1437.
- Politano, A.D.; Campbell, K.T.; Rosenberger, L.H.; Sawyer, R.G. Use of Silver in the Prevention and Treatment of Infections: Silver Review. Surg. Infect. 2013, 14, 8–20.
- NIH. Available online: https://www.nccih.nih.gov/health/colloidal-silver-what-you-need-to-know (accessed on 25 June 2023).
- Nowack, B.; Krug, H.F.; Height, M. 120 Years of Nanosilver History: Implications for Policy Makers. Environ. Sci. Technol. 2011, 45, 1177–1183.
- Vorobyev, S.; Vishnyakova, E.; Likhatski, M.; Romanchenko, A.; Nemtsev, I.; Mikhlin, Y. Reactivity and Chemical Sintering of Carey Lea Silver Nanoparticles. Nanomaterials 2019, 9, 1525.
- Dolai, J.; Mandal, K.; Jana, N.R. Nanoparticle Size Effects in Biomedical Applications. ACS Appl. Nano Mater. 2021, 4, 6471–6496.
- Sandhu, A. Who invented nano? Nat. Nanotechnol. 2006, 1, 87.
- Wikimedia Commons. File: Moneda Venezolana de 5 Bolivares de 1919.jpg. Available online: https://commons.wikimedia.org/wiki/File:Moneda_Venezolana_de_5_Bolivares_de_1919.jpg (accessed on 25 June 2023).
- Macroscale. Available online: https://www.sciencedirect.com/topics/engineering/macroscale (accessed on 25 June 2023).
- Microscale. Available online: https://www.sciencedirect.com/topics/engineering/microscale (accessed on 25 June 2023).
- Royal Society of Chemistry. Carbon. Available online: https://www.rsc.org/periodic-table/element/6/carbon (accessed on 25 June 2023).
- Wikimedia Commons. File: Canine Roundworm 1.JPG. Available online: https://commons.wikimedia.org/wiki/File:Canine_roundworm_1.JPG (accessed on 25 June 2023).
- Wikimedia Commons. File: Legionella Pneumophila 01.jpg. Available online: https://commons.wikimedia.org/wiki/File:Legionella_pneumophila_01.jpg (accessed on 25 June 2023).
- Wikimedia Commons. File: Monkeypox Virion—CDC.jpg. Available online: https://commons.wikimedia.org/wiki/File:Monkeypox_Virion_-_CDC.jpg (accessed on 25 June 2023).
- Wikimedia Commons. File: Viroid1.png. Available online: https://commons.wikimedia.org/wiki/File:Viroid1.png (accessed on 25 June 2023).
- The Nanodatabase. Available online: https://nanodb.dk/en/ (accessed on 25 June 2023).
- Nanotechnology Products Database. Available online: https://product.statnano.com/ (accessed on 25 June 2023).
- Johnson, J.R.; Delavari, P.; Azar, M. Activities of a nitrofurazone-containing urinary catheter and a silver hydrogel catheter against multidrug-resistant bacteria characteristic of catheter-associated urinary tract infection. Antimicrob. Agents Chemother. 1999, 43, 2990–2995.
- Silverlon Wound Contact Dressing 510(k) Premarket Notification FDA.gov. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K190343 (accessed on 25 June 2023).
- AQUACEL Ag Surgical SP Dressing 510(k) Premarket Notification FDA.gov. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?id=K152926 (accessed on 25 June 2023).
- ACTICOAT SILVER COATED DRESSING 510(k) Premarket Notification FDA.gov. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm?ID=K955453 (accessed on 25 June 2023).
- Mogilnicka, I.; Bogucki, P.; Ufnal, M. Microbiota and Malodor—Etiology and Management. Int. J. Mol. Sci. 2020, 21, 2886.
- Ong, W.T.J.; Nyam, K.L. Evaluation of silver nanoparticles in cosmeceutical and potential biosafety complications. Saudi. J. Biol. Sci. 2022, 29, 2085–2094.
- Zhang, J.; Wang, F.; Yalamarty, S.S.; Filipczack, N.; Jin, Y.; Li, X. Nano Silver-Induced Toxicity and Associated Mechanisms. Int. J. Nanomed. 2022, 17, 1851–1864.
- Benn, T.; Cavanagh, B.; Hristovski, K.; Posner, J.D.; Westerhoff, P. The Release of Nanosilver from Consumer Products Used in the Home. J. Environ. Qual. 2010, 39, 1875–1882.
- Schäfer, B.; Tentschert, J.; Luch, A. Nanosilver in Consumer Products and Human Health: More Information Required! Environ. Sci. Technol. 2011, 45, 7589–7590.
- Levard, C.; Hotze, E.M.; Lowry, G.V.; Brown, G.E. Environmental Transformations of Silver Nanoparticles: Impact on Stability and Toxicity. Environ. Sci. Technol. 2012, 46, 6900–6914.
- Varner, K.E.; El-Badawy, A.; Feldhake, D.; Venkatapathy, R. State-of-the-Science Review: Everything Nanosilver and More. U.S. EPA: Washington, DC, USA, 2010; EP-C-05-057.
- Mueller, N.C.; Nowack, B. Exposure modeling of engineered nanoparticles in the environment. Environ. Sci. Technol. 2008, 15, 4447–4453.
- The Nanodatabase: Ankle Thin Socks with Molecules of Silver. Available online: https://nanodb.dk/en/product/?pid=7138 (accessed on 25 June 2023).
- The Nanodatabase: Platinum Silver Nanocolloid Cream. Available online: https://nanodb.dk/en/product/?pid=2905 (accessed on 25 June 2023).
- Yin, I.X.; Zhang, J.; Zhao, I.S.; Mei, M.L.; Li, Q.; Chu, C.H. The Antibacterial Mechanism of Silver Nanoparticles and Its Application in Dentistry. Int. J. Nanomed. 2020, 15, 2555–2562.
- Galdiero, S.; Falanga, A.; Vitiello, M.; Cantisani, M.; Marra, V.; Galdiero, M. Silver nanoparticles as potential antiviral agents. Molecules 2011, 16, 8894–8918.
- Rogers, J.V.; Parkinson, C.V.; Choi, Y.W.; Speshock, J.L.; Hussain, S.M. A Preliminary Assessment of Silver Nanoparticle Inhibition of Monkeypox Virus Plaque Formation. Nanoscale Res. Lett. 2008, 3, 129–133.
- Bruna, T.; Malondonado-Bravo, F.; Jara, P.; Caro, N. Silver Nanoparticles and Their Antibacterial Applications. Int. J. Mol. Sci. 2021, 22, 7202.
- Baptista, P.V.; McCusker, M.P.; Carvalho, A.; Ferreira, D.A.; Mohan, N.M.; Martins, M.; Fernandes, A.R. Nano-Strategies to Fight Multidrug Resistant Bacteria—“A Battle of the Titans”. Front. Microbiol. 2018, 9, 1441.
- Cheeseman, S.; Christofferson, A.J.; Kariuki, R.; Cozzolino, D.; Daeneke, T.; Crawford, R.J.; Truong, V.K.; Chapman, J.; Elbourne, A. Antimicrobial Metal Nanomaterials: From Passive to Stimuli-Activated Applications. Adv. Sci. 2020, 7, 1902913.
- World Health Organization. Prioritization of Pathogens to Guide Discovery, Research and Development of New Antibiotics for Drug-Resistant Bacterial Infections, Including Tuberculosis; World Health Organization: Geneva, Switzerland, 2017.
- Nikaido, H. Molecular Basis of Bacterial Outer Membrane Permeability Revisited. Microbiol. Mol. Biol. Rev. 2003, 67, 593–656.
- Papp-Wallace, K.M.; Endimiani, A.; Taracila, M.A.; Bonomo, R.A. Carbapenems: Past, Present, and Future. Antimicrob. Agents Chemother. 2011, 55, 4943–4960.
- Mulani, M.S.; Kamble, E.E.; Kumkar, S.N.; Tawre, M.S.; Pardesi, K.R. Emerging Strategies to Combat ESKAPE Pathogens in the Era of Antimicrobial Resistance: A Review. Front. Microbiol. 2019, 10, 539.
More
Information
Subjects:
Nanoscience & Nanotechnology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
634
Revisions:
2 times
(View History)
Update Date:
18 Aug 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




