
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Jakob Gubensek | -- | 3007 | 2023-08-16 11:11:52 | | | |
| 2 | Rita Xu | -1926 word(s) | 1081 | 2023-08-16 11:23:46 | | | | |
| 3 | Rita Xu | Meta information modification | 1081 | 2023-08-16 11:25:35 | | |
Video Upload Options
Arterial calcifications are present in about 20% of patients with end-stage kidney disease and they reduce the possibility of arterio-venous fistula (AVF) formation and maturation and increase the likelihood of distal ischemia. Arterial assessment is of utmost importance if researchers are to create distal radiocephalic AVFs in the elderly patients whenever possible without burdening them with futile surgical attempts. A grading system is proposed for quantifying the severity of calcifications in the arteries of the arm with ultrasound exam.
1. Introduction
Arterial calcifications are common in patients end-stage kidney disease (ESKD) on dialysis. Risk factors for arterial calcification include advanced age, diabetes, smoking, deranged CKD-related mineral and bone disease (MBD), as well as hypertension and hyperlipidemia [1][2][3]. The presence of arterial calcifications worsens the prognosis of patients with CKD and increases the likelihood of cardiovascular events [4][5]. Furthermore, arterial calcifications also reduce the possibility of arterio-venous fistula (AVF) formation and maturation and increase the likelihood of complications, especially distal ischemia [6][7][8][9]. This is a significant disadvantage, as AVF is the optimal vascular access for patients on maintenance hemodialysis and thus their lifeline.
In a large biopsy study radial artery calcifications were reported in 21% of patients [2], whil a smaller biopsy study reported a 20% prevalence of calcifications [3]. Some large contemporary cohorts on preoperative vascular mapping report similar prevalence rates. Srivastava reported a 9% prevalence of calcifications in the radial artery [10], while the group reported a much higher 20% prevalence in elderly patients [11]. Arterial calcifications represent a significant clinical problem among elderly and diabetic patients and influence the decision of where to place an AVF.
2. How to Assess Calcified Arteries
It was shown that preoperative ultrasound examination of the arteries often significantly changes the surgical plan, particularly when radio-cephalic AVF is planned [12]. The question that must be answered by clinical and ultrasound examination is: if an adequate vein is available, when should a calcified radial artery be declared too calcified and therefore an AVF creation attempt futile?
2.1. B-Mode Ultrasound
Ultrasound mapping of vessels is considered as standard of care for preoperative evaluation of arteries (and veins) in the developed world. With B-mode ultrasound calcifications of the arterial wall can readily be seen and also quantified. There is no commonly accepted grading scale for quantifying calcifications in upper extremity arteries. Nevertheless, there are several grading scales used in the literature. The intensity of the calcifications might be most important in assessing the suitability of the artery for creation of vascular access, as severe circumferential calcifications make the artery incompressible for clamping, make the creation of the anastomosis much more difficult and outcomes are much worse. Based on existing literature [1][13][14][15] and clinical experience, a semiquantitative calcifications grading scale can be proposed for arteries of the arm (see Table 1 and Figure 1).
| Calcification Grade | B-Mode Image | Color Doppler Image | Appropriateness for Fistula Creation |
|---|---|---|---|
| none | smooth vessel wall, clear separation of intima and media |
homogenous signal | yes |
| mild | minor wall structure irregularities, increased echogenicity with spotty calcifications but without distal shadowing | homogenous signal | yes |
| moderate | irregular wall structure, intermittent calcifications with distal shadowing or linear calcifications with incomplete distal shadowing | partly homogenous signal (drop outs <50% of visible artery length) | likely |
| severe | irregular wall structure with diminished separation from surrounding tissue, continuous calcification of the wall with distal shadowing | very patchy (drop outs >50% of visible artery length) or almost absent signal | Not likely/careful consideration |
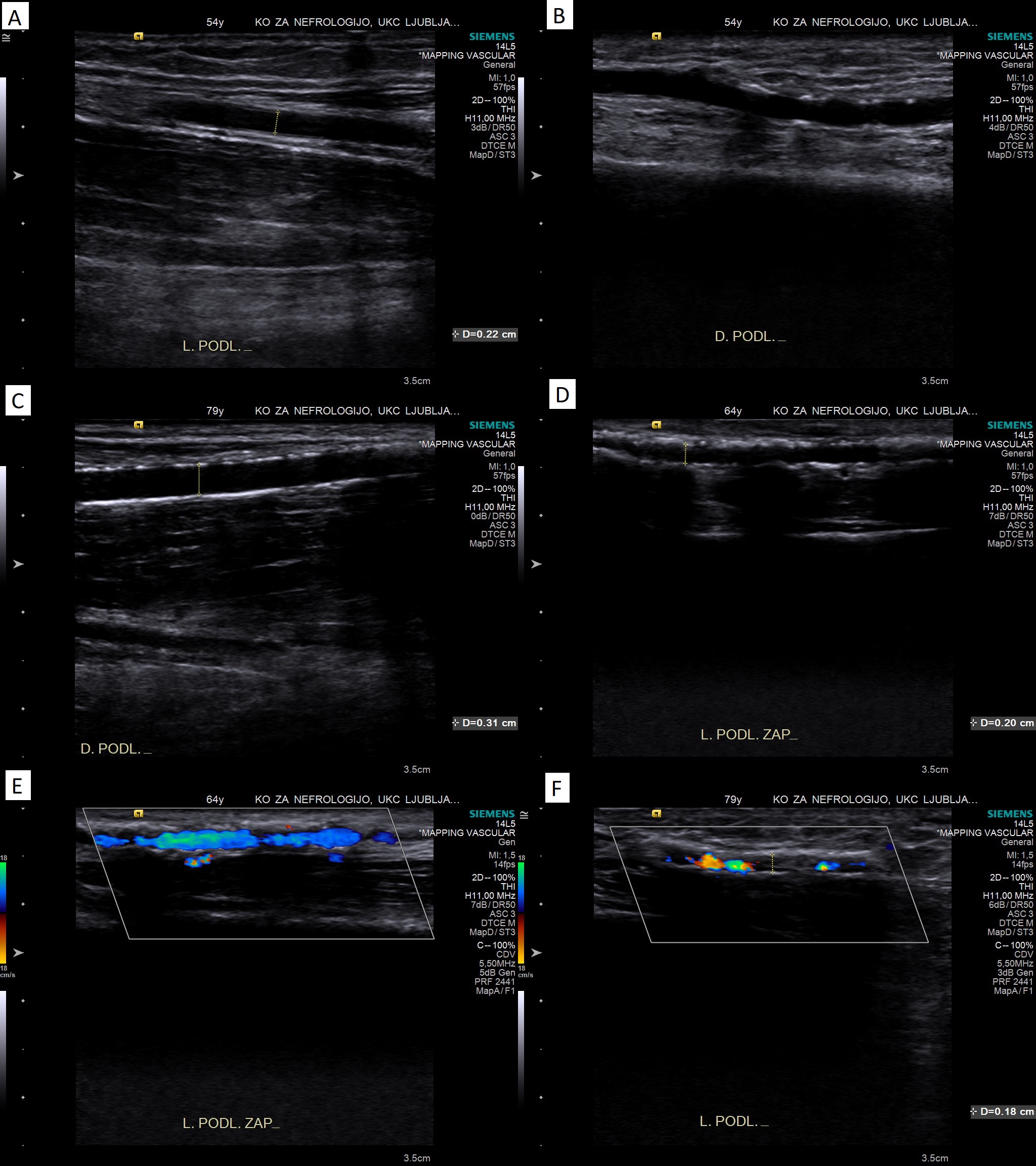
Figure 1. Illustrative B-mode and color Doppler images of the proposed grading of severity of calcifications. Panel A: no calcifications (clear separation of intima and media); panel B: mild calcifications (increased echogenicity/spotty calcifications without distal shadowing); panel C: moderate calcifications (linear calcifications with incomplete distal shadowing); panel D: severe calcifications (diminished separation from surrounding tissue, continuous calcification with distal shadowing); panel E: partly homogenous color Doppler signal in a calcified artery; panel F: very patchy color Doppler signal in a calcified artery.
2.2. Compressibility of the Artery
Compressibility of a calcified artery can be assessed prior to surgery in cross-sectional view. The ultrasound probe can be pressed at an appropriate angle so that it compresses the artery onto the bone (radius) [14]. Compressibility should be tested at several sites in the area of desired anastomosis, as calcifications are focal. This test mimics clamping the artery during surgery and can likely prevent unnecessary surgery.
2.3. Color Doppler Assessment
Different color and pulsed-wave Doppler parameters can be used to assess the suitability of the artery for AVF creation (see Table 1 and Figure 2, panel E and F). First, the homogeneity of the color Doppler signal can be assessed. Sonographic drop-out, which are visible as gaps in the color Doppler signal, are caused by dense calcifications that also cause distal shadowing [16][17]. Homogeneity or continuity of the color Doppler signal within the arterial lumen can therefore be used to assess the severity of observed arterial wall calcifications, when they are present [14].
3. Outcomes of AVFs Placed on Calcified Arteries
The available literature on radiocephalic AVF placement on calcified radial arteries is summarized in Table 2. Researchers believe that these acceptable results make construction of a radiocephalic AVF on a moderately or even severely calcified radial artery a worthwhile attempt if other conditions (vein and artery diameters) are optimal.
Table 2. Outcomes of radiocephalic AVFs placed on calcified radial arteries.
| Reference | N in the Calcified Group | Degree of Calcifications | Clinical Maturation Rate | 1-Year Secondary Patency Rate |
|---|---|---|---|---|
| Sedlacek, 2001 [18] | 25 | not graded | 80% | / |
| Georgiadis, 2014 [9] | 47 | moderate? | 89% * | 52% |
| Srivastava, 2018 [10] | 17 | not graded | 48% | / |
| Kim, 2019 [19] | 18 | mild (spoty) | 93% | / |
| Suresh Kumar, 2019 [7] | 9 | moderate/severe? | 22% | / |
| Sadasivan, 2021 [8] | 11 3 |
mild/moderate severe |
73% 33% |
/ / |
| Gubensek, 2022 [14] | 18 | moderate/severe | 67% | 66% |
* Calculated as 42/47 (2 immediate failures, 3 non-matured AVFs) [9].
4. Conclusions
Noninvasive ultrasound examination is probably the best tool for morphologic and functional assessment of the arteries. Precise evaluation of the suitability of a calcified artery for possible creation of an AVF remains a challenging task. The decision to perform a forearm AVF instead of an elbow AVF whenever possible, even in the presence of calcifications, is not only an academic or policy issue, because forearm AVFs have much fewer ischemic complications. Therefore, arterial assessment is of utmost importance if researchers are to create distal radiocephalic AVFs in the elderly patients whenever possible without burdening them with futile surgical attempts. A radial artery should probably be dismissed as too calcified when there are severe calcifications present with very patchy color Doppler and the artery is incompressible with the ultrasound probe. These may be the best predictors that the artery can be clamped and the anastomosis sutured without extreme surgical measures, although further studies are needed.
References
- Lanzer, P.; Boehm, M.; Sorribas, V.; Thiriet, M.; Janzen, J.; Zeller, T.; St Hilaire, C.; Shanahan, C. Medial vascular calcification revisited: Review and perspectives. Eur. Heart J. 2014, 35, 1515–1525.
- Chen, Z.; Zhou, Y.; Yang, T. Histopathological assessment of radial artery calcification in patients with end-stage kidney disease. Ren. Fail. 2021, 43, 362–370.
- Wang, N.; Yang, J.; Yu, X.; Hu, J.; Xing, C.; Ju, X.; Shen, X.; Qian, J.; Zhao, X.; Wang, X. Radial artery calcification in end-stage renal disease patients is associated with deposition of osteopontin and diminished expression of alpha-smooth muscle actin. Nephrology 2008, 13, 367–375.
- Chen, J.; Budoff, M.J.; Reilly, M.P.; Yang, W.; Rosas, S.E.; Rahman, M.; Zhang, X.; Roy, J.A.; Lustigova, E.; Nessel, L.; et al. Coronary artery calcification and risk of cardiovascular disease and death among patients with chronic kidney disease. JAMA Cardiol. 2017, 2, 635–643.
- Erlandsson, H.; Qureshi, A.R.; Ripsweden, J.; Löfman, I.H.; Söderberg, M.; Wennberg, L.; Lundgren, T.; Bruchfeld, A.; Brismar, T.B.; Stenvinkel, P. Scoring of medial arterial calcification predicts cardiovascular events and mortality after kidney transplantation. J. Intern. Med. 2022, 291, 813–823.
- Schmidli, J.; Widmer, M.K.; Basile, C.; de Donato, G.; Gallieni, M.; Gibbons, C.P.; Haage, P.; Hamilton, G.; Hedin, U.; Kamper, L.; et al. Vascular Access: 2018 Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2018, 55, 753–754.
- Suresh Kumar, J.; Sajeev Kumar, K.S.; Arun Thomas, E.T.; Hareesh, K.G.; George, J. Prediction model for successful radiocephalic arteriovenous fistula creation in patients with diabetic nephropathy. Saudi J. Kidney Dis. Transpl. 2019, 30, 1058–1064.
- Sadasivan, K.; Kunjuraman, U.; Murali, B.; Yadev, I.; Kochunarayanan, A. Factors Affecting the Patency of Radiocephalic Arteriovenous Fistulas Based on Clinico-Radiological Parameters. Cureus 2021, 13, e13678.
- Georgiadis, G.S.; Georgakarakos, E.I.; Antoniou, G.A.; Panagoutsos, S.; Argyriou, C.; Mourvati, E.; Passadakis, P.; Lazarides, M.K. Correlation of pre-existing radial artery macrocalcifications with late patency of primary radiocephalic fistulas in diabetic hemodialysis patients. J. Vasc. Surg. 2014, 60, 462–470.
- Srivastava, A.; Sureka, S.K.; Prabhakaran, S.; Lal, H.; Ansari, M.S.; Kapoor, R. Role of Preoperative Duplex Ultrasonography to Predict Functional Maturation of Wrist Radiocephalic Arteriovenous Fistula: A Study on Indian Population. Indian J. Nephrol. 2018, 28, 10–14.
- Persic, V.; Ponikvar, R.; Buturovic-Ponikvar, J. Preoperative ultrasonographic mapping of blood vessels before arteriovenous fistula construction in elderly patients with end-stage renal disease. Ther. Apher. Dial. 2009, 13, 334–339.
- Kim, J.J.; Koopmann, M.; Ihenachor, E.; Zeng, A.; Ryan, T.; deVirgilio, C. The addition of ultrasound arterial examination to upper extremity vein mapping before hemodialysis access. Ann. Vasc. Surg. 2016, 33, 109–115.
- Malovrh, M. Native arteriovenous fistula: Preoperative evaluation. Am. J. Kidney Dis. 2002, 39, 1218–1225.
- Gubensek, J. Doppler ultrasound assessment of calcified radial arteries prior to radio-cephalic arterio-venous fistula placement—An observational study. J. Vasc. Access 2023, in press.
- Taylor, C.; Zielinski, L.P.; Chowdhury, M.M.; Coughlin, P.A. Defining the Role of Duplex Ultrasound Assessment to Determine Severity of Arterial Calcification: An Analysis of the Superficial Femoral Artery. J. Vasc. Ultrasound 2020, 44, 74–78.
- Rocha-Singh, K.J.; Zeller, T.; Jaff, M.R. Peripheral arterial calcification: Prevalence, mechanism, detection, and clinical implications. Catheter. Cardiovasc. Interv. 2014, 83, E212–E220.
- Pajek, J.; Malovrh, M. Preoperative ultrasound still valuable for radio-cephalic arteriovenous fistula creation? J. Vasc. Access 2017, 18 (Suppl. S1), 5–9.
- Sedlacek, M.; Teodorescu, V.; Falk, A.; Vassalotti, J.A.; Uribarri, J. Hemodialysis access placement with preoperative noninvasive vascular mapping: Comparison between patients with and without diabetes. Am. J. Kidney Dis. 2001, 38, 560–564.
- Kim, S.M.; Jung, I.M.; Kim, D.; So, Y.H. Effect of Inflow Arterial Calcification on Arteriovenous Fistula Maturation. Ann. Vasc. Surg. 2019, 58, 331–337.




