Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Matteo Maurina | -- | 1674 | 2023-08-07 09:03:48 | | | |
| 2 | Rita Xu | -12 word(s) | 1662 | 2023-08-07 10:15:52 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Maurina, M.; Benedetti, A.; Stefanini, G.; Condorelli, G.; Collet, C.; Zivelonghi, C.; Smits, P.C.; Paradies, V. Coronary Vascular Function and Invasive Physiology Assessment. Encyclopedia. Available online: https://encyclopedia.pub/entry/47718 (accessed on 07 February 2026).
Maurina M, Benedetti A, Stefanini G, Condorelli G, Collet C, Zivelonghi C, et al. Coronary Vascular Function and Invasive Physiology Assessment. Encyclopedia. Available at: https://encyclopedia.pub/entry/47718. Accessed February 07, 2026.
Maurina, Matteo, Alice Benedetti, Giulio Stefanini, Gianluigi Condorelli, Carlos Collet, Carlo Zivelonghi, Pieter C. Smits, Valeria Paradies. "Coronary Vascular Function and Invasive Physiology Assessment" Encyclopedia, https://encyclopedia.pub/entry/47718 (accessed February 07, 2026).
Maurina, M., Benedetti, A., Stefanini, G., Condorelli, G., Collet, C., Zivelonghi, C., Smits, P.C., & Paradies, V. (2023, August 07). Coronary Vascular Function and Invasive Physiology Assessment. In Encyclopedia. https://encyclopedia.pub/entry/47718
Maurina, Matteo, et al. "Coronary Vascular Function and Invasive Physiology Assessment." Encyclopedia. Web. 07 August, 2023.
Copy Citation
A considerable number of patients with angina or myocardial ischemia have no significant coronary artery disease on invasive angiography. Several steps towards a better comprehension of the pathophysiology of these conditions, angina or ischemia with non-obstructive coronary arteries (ANOCA/INOCA), have been made.
ANOCA
INOCA
MINOCA
vasospastic angina
microvascular angina
1. Introduction
A considerable number of patients with anginal symptoms or myocardial ischemia on noninvasive testing present no significant coronary artery stenosis on coronary angiography [1]. The absence of significant coronary artery disease (CAD) often terminates the diagnostic workup for cardiac causes. In some cases, symptoms are attributed to non-cardiac conditions such as gastrointestinal or psychiatric disorders, leading to erroneous diagnoses and inappropriate treatments [2]. In recent years, the pathophysiology of angina or ischemia with non-obstructive coronary arteries (ANOCA/INOCA) have been investigated, and several steps have been made towards a better comprehension of these conditions. Nevertheless, several gaps in knowledge still remain.
2. Definitions
The concomitant presence of typical angina and absence of significant stenosis on coronary angiography has been historically defined as “Cardiac Syndrome X” (CSX) due to uncertainty about its mechanism [3]. The better understanding of this condition led to the replacement of the term “CSX” with microvascular angina (MVA) [4], which encompasses patients with coronary vasomotor dysfunction consisting of microvascular spasm and/or impaired vasodilatation [5][6]. While microvascular spasm can be inferred in patients with typical angina and ischemic electrocardiogram (ECG) changes during a spasm provocative test [7], impaired vasodilator reserve due to coronary microvascular dysfunction (CMD) is characterized by a low coronary flow reserve (CFR) [5]. Differently, a transient reduction in coronary blood flow (CBF) secondary to a spasm in the epicardial coronary arteries, previously referred to as “Prinzmetal” or “variant” angina, defines the condition of vasospastic angina (VSA) [7][8][9][10].
Recently, the term “ANOCA” has been coined to include all the clinical conditions determined by anginal symptoms without evidence of significant CAD on coronary angiography. When anginal symptoms are associated with documented myocardial ischemia, the term “INOCA” applies. Finally, in the presence of a universal criteria-defined myocardial infarction (MI) with no significant coronary stenosis and no other overt cause at presentation, the definition of “myocardial infarction with non-obstructive coronary artery” (MINOCA) can be used [11]. A comprehensive diagram including the abovementioned definitions is provided by Figure 1.
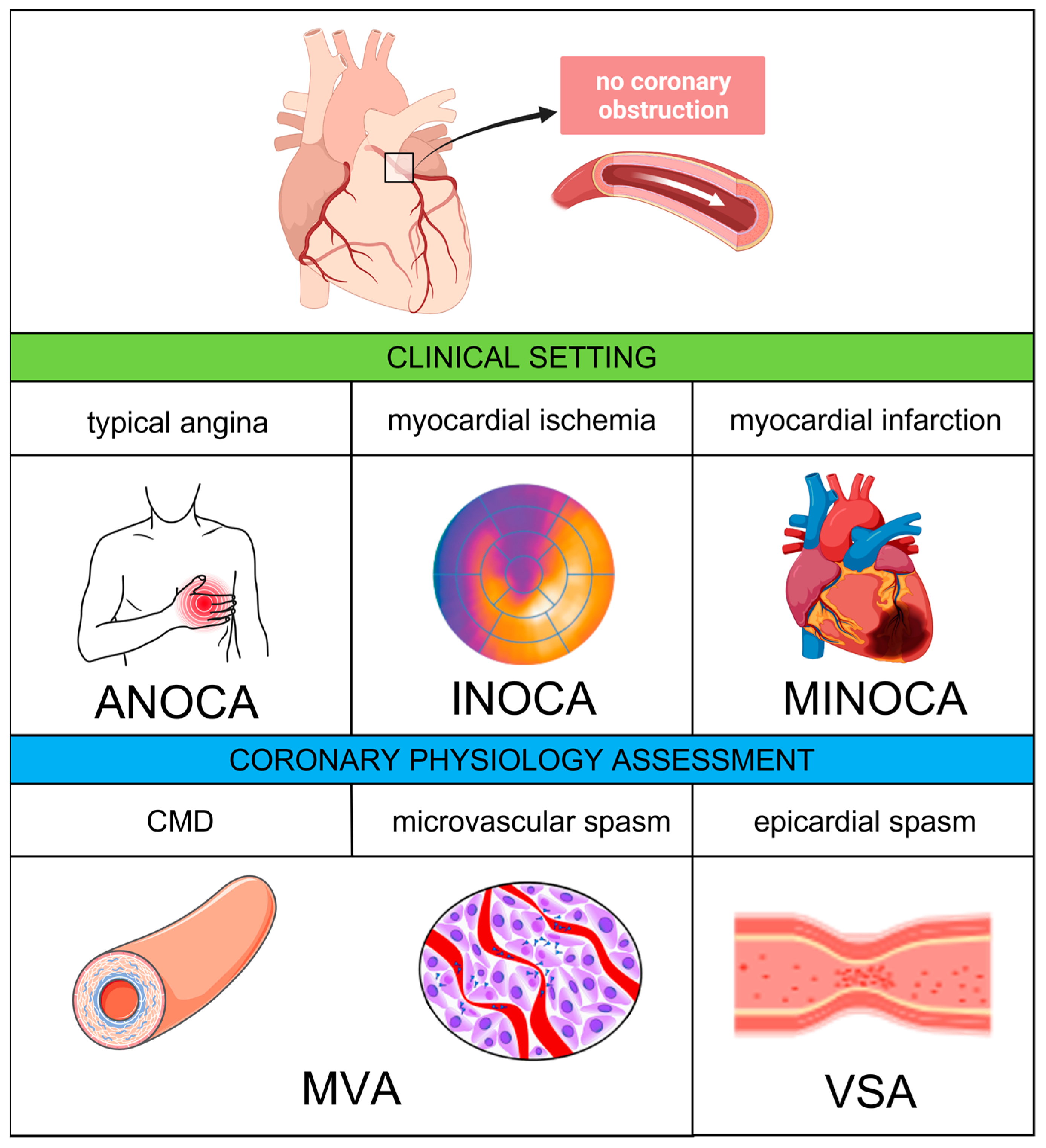
Figure 1. Coronary vascular dysfunction—clinical settings and pathophysiological mechanisms. Abbreviations: ANOCA, angina with non-obstructive coronary arteries; CMD, coronary microvascular dysfunction: INOCA, ischemia with non-obstructive coronary arteries; MINOCA, myocardial with non-obstructive coronary arteries; MVA, microvascular angina; VSA, vasospastic angina.
3. Epidemiology and Prognostic Implications
The absence of significant coronary obstruction is frequent in patients experiencing angina and myocardial ischemia. With regard to ANOCA, numerous data show that its prevalence ranges from 30% to 50% among patients undergoing coronary angiography [1][12][13][14], with a female preponderance [14][15][16]. Interestingly, these percentages seem to remain stable over time despite improvements in the definition and detection of this condition [12]. Nevertheless, the correct characterization of symptoms has a central role, since the presence of typical angina is a predictor of significant CAD, while atypical symptoms are more often associated with the absence of coronary obstruction [1][13]. When a non-invasive stress test confirms the presence of significant myocardial ischemia in patients with angina, the percentage of patients without significant CAD decreases [1][17]. The prevalence of MINOCA has been reported to range between 2% and 10% of all Mis [18][19][20][21][22], while coronary obstruction is found in more than 90% [23]. Interestingly, women have a higher chance of a negative coronary angiography than men also in the setting of MI [18].
Notably, none of these conditions is benign. In addition to impaired quality of life, several studies reported an increased risk of adverse events in patients with ANOCA and INOCA [24][25][26]. The available data show a 1.3 higher risk of death and a 3–4-fold higher risk of hospitalization for cardiovascular events in ANOCA patients as compared with asymptomatic individuals [14][25], while the Women’s Ischemia Syndrome Evaluation (WISE) study demonstrated a 10-year risk of all-cause death of 13% and 2.8% in patients with INOCA and in control healthy individuals, respectively [27]. In MINOCA patients, the prognosis is influenced by the underlying mechanism and the extent of myocardial dysfunction. Overall, the risk of mortality in patients with MINOCA is estimated to be about 1%, 3% and 4% in hospital, at 1 year and at 3 years, respectively [22][28][29]. Finally, the absence of significant coronary obstruction on coronary angiography may lead the treating physician to wrongly reassure patients or discontinue the medical therapy, with a potential negative impact on symptoms and quality of life.
4. Pathophysiology
Among the main pathophysiological mechanisms deemed responsible for ANOCA/INOCA and MINOCA, vascular spasm and CMD play an important role.
4.1. Epicardial and Microvascular Vasospasm
Epicardial vasospasm is a pathologic condition characterized by a transient reduction of CBF due to a spasm in the epicardial coronary arteries. This phenomenon is responsible for recurrent attacks of chest pain similar to those occurring in patients with obstructive CAD; however, these episodes often happen at rest rather than under exertion, and effort tolerance is generally preserved [30]. While initially referred to as “Prinzmetal” or “variant” angina due to its differences from classical effort angina, the exact definition of the pathophysiology of this phenomenon led to the introduction of the term “VSA”.
The hyperreactivity of vascular smooth cells (VSCs) is thought to play a central role in the pathophysiology of VSA. VSCs’ contraction is mediated by the phosphorylation and dephosphorylation of myosin light chains (MLCs). MLC dephosphorylation, in particular, is inhibited by rho-kinase, which has been shown to be hyper-expressed in the spastic cells [31][32]. This hypothesis is supported by preliminary studies suggesting that the use of rho-kinase inhibitors effectively prevents acetylcholine (Ach)-induced coronary spasms [33]. The occurrence of anginal symptoms at night, when the vagal tone is higher, and the induction of spasm by Ach suggest that dysregulation in the autonomic nervous system may be involved as well in the pathophysiology of VSA [8][34]. Other potential mechanisms include endothelial dysfunction with dysregulation of the nitric oxide synthases, magnesium deficiency, oxidative stress, inflammation and genetic polymorphisms [8]. Coronary spasm often occurs at the level of an atherosclerotic plaque, probably because the endothelial dysfunction, leading to an imbalance between vasodilator and vasopressor stimuli [35], can act as a trigger for local injury, ischemic damage and MI [36]. However, even healthy vessels can be affected.
Several studies suggest that a spasm can also occur at the level of the microcirculation. Mohri et al. showed that lactate was produced during a spasm provocation test in patients with angina attack and ischemic ECG changes without significant epicardial coronary obstruction [37]. Sun et al. confirmed these findings demonstrating the occurrence of myocardial ischemia (typical angina, ischemic ECG changes and lactate production) in patients undergoing the spasm provocative test without angiographic evidence of an epicardial spasm [38]. These data support the hypothesis that, in the absence of an epicardial spasm, patients with chest pain and ECG changes during the spasm provocative test suffer from microvascular spasm. Of note, it should be considered that patients with non-diagnostic Ach-test results may be affected by CMD [7]. Finally, one of the main characteristics of both epicardial and microvascular vasospasms is the resolution of symptoms due to vasodilation in response to nitrates.
4.2. Coronary Microvascular Dysfunction
CMD is a condition that is characterized by reduced CFR either due to increased minimal microvascular resistance (MVR) or high resting flow due to the altered non-endothelial-dependent vasomotion of the coronary microvasculature (<500 μm) [39][40][41][42]. Based on the underlying mechanism, two clinical entities can be distinguished, structural and functional CMD. The main structural changes associated with CMD are the thickening of the arterioles’ wall with a reduction in the lumen area, the increase in perivascular fibrous tissue and the decrease in the vascular density (capillary rarefaction), leading to high MVR. Additionally, non-endothelial-dependent mechanisms such as the impaired relaxation of VSCs, higher susceptibility of VSCs to vasoconstrictor stimuli and abnormal autonomic activity may be involved [43][44]. These abnormalities lead to an increase in the MVR and an insufficient increase in CBF under physiological stress, contributing to an imbalance between oxygen demand and supply, resulting in myocardial ischemia [5][41].
The parameter that expresses the ability of the coronary microcirculation to increase CBF under stress conditions is the CFR, defined as the ratio of the CBF during maximal vasodilation to the corresponding value at rest. Unlike other parameters used to assess the hemodynamic significance of a coronary stenosis, such as fractional flow reserve (FFR) and instantaneous wave-free ratio (iFR), CFR provides complementary information about the overall functional status of the coronary circulation. There can be a correlation between FFR, iFR and CFR in certain cases; for example, if a coronary stenosis is severe enough to limit CBF, then FFR, iFR and CFR may all be found to be altered. By contrast, other conditions, such as the presence of collateral circulation or CMD, may alter this relationship. In the case of well-developed collaterals supplying adequate CBF to the affected territory, CFR may remain preserved even in the case of an FFR and/or iFR significant stenosis. Furthermore, an altered CFR may suggest CMD in symptomatic patients with non-hemodynamically significant coronary stenosis at FFR and/or iFR assessment [45][46].
Typically, patients with CMD due to altered microvascular architecture present with low CFR and high MVR values. However, a proportion of patients with functional CMD may exhibit low CFR/low MVR and high resting CBF values. The mechanism responsible for this specific subset of CMD is still unclear, as this might be due to either a reduced myocardial efficiency or uncoupled CBF [47]. Structural changes in the coronary microvascular have been shown to be more prevalent in patients with classical cardiovascular risk factors, including hypertension, hyperlipidemia, smoking and diabetes mellitus (DM). Moreover, they have been correlated with other conditions, including renal impairment, coronary atherosclerosis, ventricular hypertrophy, and other cardiomyopathies [5][48].
While different findings on the coronary function tests (CFTs) may suggest that coronary microvascular spasm and CMD might represent two separated entities, an anomalous vasodilatory response has been proven in patients presenting the abovementioned risk factors and predisposition for structural abnormalities [48], suggesting that both non-endothelial-dependent and endothelial-dependent alterations may coexist in patients with MVA. Importantly, the coexistence of CMD and VSA portends a worse prognosis.
References
- Patel, M.R.; Peterson, E.D.; Dai, D.; Brennan, J.M.; Redberg, R.F.; Anderson, H.V.; Brindis, R.G.; Douglas, P.S. Low Diagnostic Yield of Elective Coronary Angiography. N. Engl. J. Med. 2010, 362, 886–895.
- Phan, A.; Shufelt, C.; Merz, C.N.B. Persistent Chest Pain and No Obstructive Coronary Artery Disease. JAMA 2009, 301, 1468–1474.
- Agrawal, S.; Mehta, P.K.; Bairey Merz, C.N. Cardiac Syndrome X: Update 2014. Cardiol. Clin. 2014, 32, 463–478.
- Villano, A.; Lanza, G.A.; Crea, F. Microvascular angina: Prevalence, pathophysiology and therapy. J. Cardiovasc. Med. 2018, 19 (Suppl. 1), e36–e39.
- Jansen, T.P.; Konst, R.E.; Elias-Smale, S.E.; Oord, S.C.v.D.; Ong, P.; de Vos, A.M.; van de Hoef, T.P.; Paradies, V.; Smits, P.C.; van Royen, N.; et al. Assessing Microvascular Dysfunction in Angina With Unobstructed Coronary Arteries. J. Am. Coll. Cardiol. 2021, 78, 1471–1479.
- Crooijmans, C.; Jansen, T.; Konst, R.; Woudstra, J.; Appelman, Y.; Ruijter, H.D.; Onland-Moret, N.; Meeder, J.; de Vos, A.; Paradies, V.; et al. Design and rationale of the NetherLands registry of invasive Coronary vasomotor Function Testing (NL-CFT). Int. J. Cardiol. 2023, 379, 1–8.
- Ong, P.; Camici, P.G.; Beltrame, J.F.; Crea, F.; Shimokawa, H.; Sechtem, U.; Kaski, J.C.; Merz, C.N.B.; Coronary Vasomotion Disorders International Study Group (COVADIS). International standardization of diagnostic criteria for microvascular angina. Int. J. Cardiol. 2018, 250, 16–20.
- Picard, F.; Sayah, N.; Spagnoli, V.; Adjedj, J.; Varenne, O. Vasospastic angina: A literature review of current evidence. Arch. Cardiovasc. Dis. 2019, 112, 44–55.
- Vancheri, F.; Longo, G.; Vancheri, S.; Henein, M. Coronary Microvascular Dysfunction. J. Clin. Med. 2020, 9, 2880.
- Prinzmetal, M.; Kennamer, R.; Merliss, R.; Wada, T.; Bor, N. Angina pectoris I. A variant form of angina pectoris: Preliminary report. Am. J. Med. 1959, 27, 375–388.
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018, 138, e618–e651.
- Patel, S.; Fung, M.; Liang, Z.; Butalia, S.; Anderson, T.J. Temporal Trends of the Prevalence of Angina With No Obstructive Coronary Artery Disease (ANOCA). Can. J. Cardiol. 2023, 39, 63–70.
- Patel, M.R.; Dai, D.; Hernandez, A.F.; Douglas, P.S.; Messenger, J.; Garratt, K.N.; Maddox, T.M.; Peterson, E.D.; Roe, M.T. Prevalence and predictors of nonobstructive coronary artery disease identified with coronary angiography in contemporary clinical practice. Am. Heart J. 2014, 167, 846–852.e2.
- Jespersen, L.; Hvelplund, A.; Abildstrøm, S.Z.; Pedersen, F.; Galatius, S.; Madsen, J.K.; Jørgensen, E.; Kelbaek, H.; Prescott, E. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur. Heart J. 2012, 33, 734–744.
- Sharaf, B.; Wood, T.; Shaw, L.; Johnson, B.D.; Kelsey, S.; Anderson, R.D.; Pepine, C.J.; Merz, C.N.B. Adverse outcomes among women presenting with signs and symptoms of ischemia and no obstructive coronary artery disease: Findings from the National Heart, Lung, and Blood Institute–sponsored Women’s Ischemia Syndrome Evaluation (WISE) angiographic core laboratory. Am. Heart J. 2013, 166, 134–141.
- Mileva, N.; Nagumo, S.; Mizukami, T.; Sonck, J.; Berry, C.; Gallinoro, E.; Monizzi, G.; Candreva, A.; Munhoz, D.; Vassilev, D.; et al. Prevalence of Coronary Microvascular Disease and Coronary Vasospasm in Patients With Nonobstructive Coronary Artery Disease: Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2022, 11, e023207.
- Buchthal, S.D.; Hollander, J.A.D.; Merz, C.N.B.; Rogers, W.J.; Pepine, C.J.; Reichek, N.; Sharaf, B.L.; Reis, S.; Kelsey, S.F.; Pohost, G.M. Abnormal Myocardial Phosphorus-31 Nuclear Magnetic Resonance Spectroscopy in Women with Chest Pain but Normal Coronary Angiograms. N. Engl. J. Med. 2000, 342, 829–835.
- Gehrie, E.R.; Reynolds, H.R.; Chen, A.Y.; Neelon, B.H.; Roe, M.T.; Gibler, W.B.; Ohman, E.M.; Newby, L.K.; Peterson, E.D.; Hochman, J.S. Characterization and outcomes of women and men with non–ST-segment elevation myocardial infarction and nonobstructive coronary artery disease: Results from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) Quality Improvement Initiative. Am. Heart J. 2009, 158, 688–694.
- Kang, W.Y.; Jeong, M.H.; Ahn, Y.K.; Kim, J.H.; Chae, S.C.; Kim, Y.J.; Hur, S.H.; Seong, I.W.; Hong, T.J.; Choi, D.H.; et al. Are patients with angiographically near-normal coronary arteries who present as acute myocardial infarction actually safe? Int. J. Cardiol. 2011, 146, 207–212.
- Larsen, A.I.; Galbraith, P.D.; Ghali, W.A.; Norris, C.M.; Graham, M.M.; Knudtson, M.L. Characteristics and outcomes of patients with acute myocardial infarction and angiographically normal coronary arteries. Am. J. Cardiol. 2005, 95, 261–263.
- Bugiardini, R.; Manfrini, O.; De Ferrari, G.M. Unanswered Questions for Management of Acute Coronary Syndrome. Arch. Intern. Med. 2006, 166, 1391–1395.
- Pasupathy, S.; Air, T.; Dreyer, R.P.; Tavella, R.; Beltrame, J.F. Systematic Review of Patients Presenting With Suspected Myocardial Infarction and Nonobstructive Coronary Arteries. Circulation 2015, 131, 861–870.
- DeWood, M.A.; Spores, J.; Notske, R.; Mouser, L.T.; Burroughs, R.; Golden, M.S.; Lang, H.T. Prevalence of Total Coronary Occlusion during the Early Hours of Transmural Myocardial Infarction. N. Engl. J. Med. 1980, 303, 897–902.
- Gulati, M.; Cooper-DeHoff, R.M.; McClure, C.; Johnson, B.D.; Shaw, L.J.; Handberg, E.M.; Zineh, I.; Kelsey, S.F.; Arnsdorf, M.F.; Black, H.R.; et al. Adverse Cardiovascular Outcomes in Women With Nonobstructive Coronary Artery Disease. Arch. Intern. Med. 2009, 169, 843–850.
- Jespersen, L.; Abildstrom, S.Z.; Hvelplund, A.; Madsen, J.K.; Galatius, S.; Pedersen, F.; Hojberg, S.; Prescott, E. Burden of Hospital Admission and Repeat Angiography in Angina Pectoris Patients with and without Coronary Artery Disease: A Registry-Based Cohort Study. PLoS ONE 2014, 9, e93170.
- Brainin, P.; Frestad, D.; Prescott, E. The prognostic value of coronary endothelial and microvascular dysfunction in subjects with normal or non-obstructive coronary artery disease: A systematic review and meta-analysis. Int. J. Cardiol. 2018, 254, 1–9.
- Kenkre, T.S.; Malhotra, P.; Johnson, B.D.; Handberg, E.M.; Thompson, D.V.; Marroquin, O.C.; Rogers, W.J.; Pepine, C.J.; Merz, C.N.B.; Kelsey, S.F.; et al. Ten-Year Mortality in the WISE Study (Women’s Ischemia Syndrome Evaluation). Circ. Cardiovasc. Qual. Outcomes 2017, 10, e003863.
- Patel, M.R.; Chen, A.Y.; Peterson, E.D.; Newby, L.K.; Pollack, C.V.; Brindis, R.G.; Gibson, C.M.; Kleiman, N.S.; Saucedo, J.F.; Bhatt, D.L.; et al. Prevalence, predictors, and outcomes of patients with non–ST-segment elevation myocardial infarction and insignificant coronary artery disease: Results from the Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA Guidelines (CRUSADE) initiative. Am. Heart J. 2006, 152, 641–647.
- Larsen, A.I.; Nilsen, D.W.; Yu, J.; Mehran, R.; Nikolsky, E.; Lansky, A.J.; Caixeta, A.; Parise, H.; Fahy, M.; Cristea, E.; et al. Long-Term Prognosis of Patients Presenting With ST-Segment Elevation Myocardial Infarction With No Significant Coronary Artery Disease (from The HORIZONS-AMI Trial). Am. J. Cardiol. 2013, 111, 643–648.
- Beltrame, J.F.; Crea, F.; Kaski, J.C.; Ogawa, H.; Ong, P.; Sechtem, U.; Shimokawa, H.; Merz, C.N.B. International standardization of diagnostic criteria for vasospastic angina. Eur. Heart J. 2015, 38, 2565–2568.
- Shimokawa, H.; Seto, M.; Katsumata, N.; Amano, M.; Kozai, T.; Yamawaki, T.; Kuwata, K.; Kandabashi, T.; Egashira, K.; Ikegaki, I.; et al. Rho-kinase-mediated pathway induces enhanced myosin light chain phosphorylations in a swine model of coronary artery spasm. Cardiovasc. Res. 1999, 43, 1029–1039.
- Kandabashi, T.; Shimokawa, H.; Miyata, K.; Kunihiro, I.; Kawano, Y.; Fukata, Y.; Higo, T.; Egashira, K.; Takahashi, S.; Kaibuchi, K.; et al. Inhibition of myosin phosphatase by upregulated rho-kinase plays a key role for coronary artery spasm in a porcine model with interleukin-1beta. Circulation 2000, 101, 1319–1323.
- Masumoto, A.; Mohri, M.; Shimokawa, H.; Urakami, L.; Usui, M.; Takeshita, A. Suppression of Coronary Artery Spasm by the Rho-Kinase Inhibitor Fasudil in Patients With Vasospastic Angina. Circulation 2002, 105, 1545–1547.
- Miwa, K.; Igawa, A.; Miyagi, Y.; Nakagawa, K.; Inoue, H. Alterations of autonomic nervous activity preceding nocturnal variant angina: Sympathetic augmentation with parasympathetic impairment. Am. Heart J. 1998, 135, 762–771.
- Laughlin, M.H.; Davis, M.J.; Secher, N.H.; Lieshout, J.J.; Arce-Esquivel, A.A.; Simmons, G.H.; Bender, S.B.; Padilla, J.; Bache, R.J.; Merkus, D.; et al. Peripheral Circulation. Compr. Physiol. 2012, 2, 321–447.
- Slavich, M.; Patel, R.S. Coronary artery spasm: Current knowledge and residual uncertainties. IJC Heart Vasc. 2016, 10, 47–53.
- Mohri, M.; Koyanagi, M.; Egashira, K.; Tagawa, H.; Ichiki, T.; Shimokawa, H.; Takeshita, A. Angina pectoris caused by coronary microvascular spasm. Lancet 1998, 351, 1165–1169.
- Sun, H.; Mohri, M.; Shimokawa, H.; Usui, M.; Urakami, L.; Takeshita, A. Coronary microvascular spasm causes myocardial ischemia in patients with vasospastic angina. J. Am. Coll. Cardiol. 2002, 39, 847–851.
- Del Buono, M.G.; Montone, R.A.; Camilli, M.; Carbone, S.; Narula, J.; Lavie, C.J.; Niccoli, G.; Crea, F. Coronary Microvascular Dysfunction Across the Spectrum of Cardiovascular Diseases. J. Am. Coll. Cardiol. 2021, 78, 1352–1371.
- Pries, A.R.; Badimon, L.; Bugiardini, R.; Camici, P.G.; Dorobantu, M.; Duncker, D.J.; Escaned, J.; Koller, A.; Piek, J.J.; de Wit, C. Coronary vascular regulation, remodelling, and collateralization: Mechanisms and clinical implications on behalf of the working group on coronary pathophysiology and microcirculation. Eur. Heart J. 2015, 36, 3134–3146.
- Crea, F.; Montone, R.A.; Rinaldi, R. Pathophysiology of Coronary Microvascular Dysfunction. Circ. J. 2022, 86, 1319–1328.
- Rahman, H.; Demir, O.M.; Khan, F.; Ryan, M.; Ellis, H.; Mills, M.T.; Chiribiri, A.; Webb, A.; Perera, D. Physiological Stratification of Patients With Angina Due to Coronary Microvascular Dysfunction. J. Am. Coll. Cardiol. 2020, 75, 2538–2549.
- Camici, P.G.; Crea, F. Coronary Microvascular Dysfunction. N. Engl. J. Med. 2007, 356, 830–840.
- Crea, F.; Camici, P.G.; Merz, C.N.B. Coronary microvascular dysfunction: An update. Eur. Heart J. 2014, 35, 1101–1111.
- Kovarnik, T.; Hitoshi, M.; Kral, A.; Jerabek, S.; Zemanek, D.; Kawase, Y.; Omori, H.; Tanigaki, T.; Pudil, J.; Vodzinska, A.; et al. Fractional Flow Reserve Versus Instantaneous Wave-Free Ratio in Assessment of Lesion Hemodynamic Significance and Explanation of their Discrepancies. International, Multicenter and Prospective Trial: The FiGARO Study. J. Am. Heart Assoc. 2022, 11, e021490.
- Cook, C.M.; Jeremias, A.; Petraco, R.; Sen, S.; Nijjer, S.; Shun-Shin, M.J.; Ahmad, Y.; de Waard, G.; van de Hoef, T.; Echavarria-Pinto, M.; et al. Fractional Flow Reserve/Instantaneous Wave-Free Ratio Discordance in Angiographically Intermediate Coronary Stenoses. JACC Cardiovasc. Interv. 2017, 10, 2514–2524.
- Nardone, M.; McCarthy, M.; Ardern, C.I.; Nield, L.E.; Toleva, O.; Cantor, W.J.; Miner, S.E. Concurrently Low Coronary Flow Reserve and Low Index of Microvascular Resistance Are Associated With Elevated Resting Coronary Flow in Patients With Chest Pain and Nonobstructive Coronary Arteries. Circ. Cardiovasc. Interv. 2022, 15, e011323.
- Taqueti, V.R.; Di Carli, M.F. Coronary Microvascular Disease Pathogenic Mechanisms and Therapeutic Options. J. Am. Coll. Cardiol. 2018, 72, 2625–2641.
More
Information
Subjects:
Cardiac & Cardiovascular Systems
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.2K
Revisions:
2 times
(View History)
Update Date:
07 Aug 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




