
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Mohammad Noori | -- | 2120 | 2023-07-26 00:11:59 | | | |
| 2 | Rita Xu | -4 word(s) | 2116 | 2023-07-26 04:17:28 | | |
Video Upload Options
A rapidly expanding global population and a sizeable portion of it that is aging are the main causes of the significant increase in healthcare costs. Healthcare in terms of monitoring systems is undergoing radical changes, making it possible to gauge or monitor the health conditions of people constantly, while also removing some minor possibilities of going to the hospital. The development of automated devices that are either attached to organs or the skin, continually monitoring human activity, has been made feasible by advancements in sensor technologies, embedded systems, wireless communication technologies, nanotechnologies, and miniaturization being ultra-thin, lightweight, highly flexible, and stretchable. Wearable sensors track physiological signs together with other symptoms such as respiration, pulse, and gait pattern, etc., to spot unusual or unexpected events.
1. Introduction
2. Performance Comparison among Wearable Energy Harvesters
3. Applications of Wearable Energy Harvesters
3.1. Heart Rate Monitoring
3.2. Respiration Monitoring
3.3. Movement Tracking
3.4. Sleep Monitoring
3.5. Fall Detection
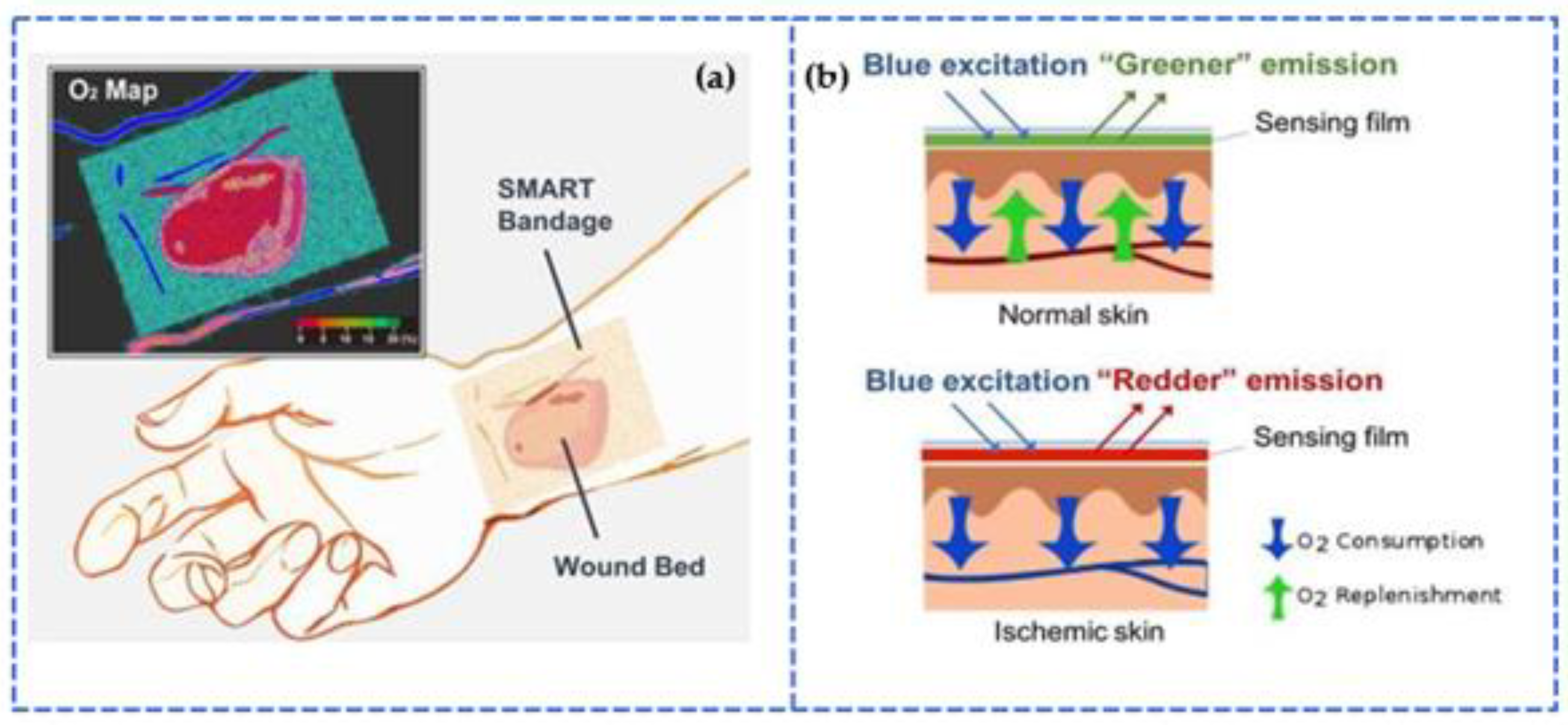
3.6. Smart Bandages
References
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130.
- Wang, Y.; Yu, Y.; Wei, X.; Narita, F. Self-Powered Wearable Piezoelectric Monitoring of Human Motion and Physiological Signals for the Postpandemic Era: A Review. Adv. Mater. Technol. 2022, 7, 2200318.
- Fan, Z.; Zhang, Y.; Pan, L.; Ouyang, J.; Zhang, Q. Recent developments in flexible thermoelectrics: From materials to devices. Renew. Sustain. Energy Rev. 2020, 137, 110448.
- Mo, X.; Zhou, H.; Li, W.; Xu, Z.; Duan, J.; Huang, L.; Hu, B.; Zhou, J. Piezoelectrets for wearable energy harvesters and sensors. Nano Energy 2019, 65, 104033.
- Dagdeviren, C.; Joe, P.; Tuzman, O.L.; Park, K.-I.; Lee, K.J.; Shi, Y.; Huang, Y.; Rogers, J.A. Recent progress in flexible and stretchable piezoelectric devices for mechanical energy harvesting, sensing and actuation. Extrem. Mech. Lett. 2016, 9, 269–281.
- Seneviratne, S.; Hu, Y.; Nguyen, T.; Lan, G.; Khalifa, S.; Thilakarathna, K.; Hassan, M.; Seneviratne, A. A Survey of Wearable Devices and Challenges. IEEE Commun. Surv. Tutor. 2017, 19, 2573–2620.
- Dassanayaka, D.G.; Alves, T.M.; Wanasekara, N.D.; Dharmasena, I.G.; Ventura, J. Recent Progresses in Wearable Triboelectric Nanogenerators. Adv. Funct. Mater. 2022, 32, 2205438.
- Nasiri, S.; Khosravani, M.R. Progress and challenges in fabrication of wearable sensors for health monitoring. Sens. Actuators A Phys. 2020, 312, 112105.
- Heikenfeld, J.; Jajack, A.; Rogers, J.; Gutruf, P.; Tian, L.; Pan, T.; Li, R.; Khine, M.; Kim, J.; Wang, J.; et al. Wearable sensors: Modalities, challenges, and prospects. Lab Chip 2018, 18, 217–248.
- An, B.W.; Shin, J.H.; Kim, S.-Y.; Kim, J.; Ji, S.; Park, J.; Lee, Y.; Jang, J.; Park, Y.-G.; Cho, E.; et al. Smart Sensor Systems for Wearable Electronic Devices. Polymers 2017, 9, 303.
- Zoui, M.A.; Bentouba, S.; Stocholm, J.G.; Bourouis, M. A Review on Thermoelectric Generators: Progress and Applications. Energies 2020, 13, 3606.
- An, B.W.; Hyun, B.G.; Kim, S.-Y.; Minji, K.; Lee, M.-S.; Lee, K.; Koo, J.B.; Chu, H.Y.; Bae, B.-S.; Park, J.-U. Stretchable and transparent electrodes using hybrid structures of graphene-metal nanotrough networks with high performances and ultimate uniformity. Nano Lett. 2014, 14, 6322–6328.
- Lee, M.S.; Lee, K.; Kim, S.Y.; Lee, H.; Park, J.; Choi, K.H.; Kim, H.K.; Kim, D.G.; Lee, D.Y.; Nam, S.; et al. High-performance, transparent, and stretchable electrodes using graphene-metal nanowire hybrid structures. Nano Lett. 2013, 13, 2814–2821.
- Kim, J.; Lee, M.-S.; Jeon, S.; Kim, M.; Kim, S.; Kim, K.; Bien, F.; Hong, S.Y.; Park, J.-U. Highly Transparent and Stretchable Field-Effect Transistor Sensors Using Graphene-Nanowire Hybrid Nanostructures. Adv. Mater. 2015, 27, 3292–3297.
- Lou, Z.; Wang, L.; Jiang, K.; Wei, Z.; Shen, G. Reviews of wearable healthcare systems: Materials, devices and system integration. Mater. Sci. Eng. R Rep. 2019, 140, 100523.
- Osman, A.; Lu, J. 3D printing of polymer composites to fabricate wearable sensors: A comprehensive review. Mater. Sci. Eng. R Rep. 2023, 154, 100734.
- Lu, Y.; Lou, Z.; Jiang, K.; Chen, D.; Shen, G. Recent progress of self-powered wearable monitoring systems integrated with microsupercapacitors. Mater. Today Nano 2019, 8, 100050.
- Lim, H.; Kim, H.S.; Qazi, R.; Kwon, Y.; Jeong, J.; Yeo, W. Advanced Soft Materials, Sensor Integrations, and Applications of Wearable Flexible Hybrid Electronics in Healthcare, Energy, and Environment. Adv. Mater. 2019, 32, e1901924.
- Lou, Z.; Wang, L.; Shen, G. Recent Advances in Smart Wearable Sensing Systems. Adv. Mater. Technol. 2018, 3, 1800444.
- Li, Q.; Zhang, L.; Tao, X.; Ding, X. Review of Flexible Temperature Sensing Networks for Wearable Physiological Monitoring. Adv. Healthc. Mater. 2017, 6, 1601371.
- Khalid, S.; Raouf, I.; Khan, A.; Kim, N.; Kim, H.S. A Review of Human-Powered Energy Harvesting for Smart Electronics: Recent Progress and Challenges. Int. J. Precis. Eng. Manuf. Technol. 2019, 6, 821–851.
- Gowthaman, S.; Chidambaram, G.S.; Rao, D.B.G.; Subramya, H.V.; Chandrasekhar, U. A Review on Energy Harvesting Using 3D Printed Fabrics for Wearable Electronics. J. Inst. Eng. Ser. C 2016, 99, 435–447.
- Rocha, J.G.; Goncalves, L.M.; Rocha, P.F.; Silva, M.P.; Lanceros-Mendez, S. Energy Harvesting From Piezoelectric Materials Fully Integrated in Footwear. IEEE Trans. Ind. Electron. 2009, 57, 813–819.
- Alagumalai, A.; Shou, W.; Mahian, O.; Aghbashlo, M.; Tabatabaei, M.; Wongwises, S.; Liu, Y.; Zhan, J.; Torralba, A.; Chen, J.; et al. Self-powered sensing systems with learning capability. Joule 2022, 6, 1475–1500.
- Lou, Z.; Li, L.; Wang, L.; Shen, G. Recent Progress of Self-Powered Sensing Systems for Wearable Electronics. Small 2017, 13, 1701791.
- Yan, Y. Recent advances in electrostatic sensors and instruments for industrial measurement and monitoring. In Proceedings of the 2016 IEEE Student Conference on Research and Development (SCOReD), Kuala Lumpur, Malaysia, 13–14 December 2016; pp. 1–2.
- Pu, X.; Zhang, C.; Wang, Z.L. Triboelectric nanogenerators as wearable power sources and self-powered sensors. Natl. Sci. Rev. 2022, 10, nwac170.
- Li, Z.; Cui, Y.; Zhong, J. Recent advances in nanogenerators-based flexible electronics for electromechanical biomonitoring. Biosens. Bioelectron. 2021, 186, 113290.
- Yan, Y.; Hu, Y.; Wang, L.; Qian, X.; Zhang, W.; Reda, K.; Wu, J.; Zheng, G. Electrostatic sensors—Their principles and applications. Measurement 2020, 169, 108506.
- Romero, E.; Warrington, R.O.; Neuman, M.R. Energy scavenging sources for biomedical sensors. Physiol. Meas. 2009, 30, R35–R62.
- Wang, W.; Yu, A.; Zhai, J.; Wang, Z.L. Recent Progress of Functional Fiber and Textile Triboelectric Nanogenerators: Towards Electricity Power Generation and Intelligent Sensing. Adv. Fiber Mater. 2021, 3, 394–412.
- Gao, M.; Wang, P.; Jiang, L.; Wang, B.; Yao, Y.; Liu, S.; Chu, D.; Cheng, W.; Lu, Y. Power generation for wearable systems. Energy Environ. Sci. 2021, 14, 2114–2157.
- Liu, R.; Zuo, H.; Sun, J.; Bei, S. A Review on Electrostatic Monitoring. In Proceedings of the 2017 International Conference on Sensing, Diagnostics, Prognostics, and Control, Shanghai, China, 16–18 August 2017; pp. 128–131.
- Cadei, A.; Dionisi, A.; Sardini, E.; Serpelloni, M. Kinetic and thermal energy harvesters for implantable medical devices and biomedical autonomous sensors. Meas. Sci. Technol. 2013, 25, 012003.
- Prasad, R.V.; Devasenapathy, S.; Rao, V.S.; Vazifehdan, J. Reincarnation in the Ambiance: Devices and Networks with Energy Harvesting. IEEE Commun. Surv. Tutor. 2013, 16, 195–213.
- Xu, Y.; Hu, X.; Kundu, S.; Nag, A.; Afsarimanesh, N.; Sapra, S.; Mukhopadhyay, S.C.; Han, T. Silicon-Based Sensors for Biomedical Applications: A Review. Sensors 2019, 19, 2908.
- Wu, Z.; Cheng, T.; Wang, Z.L. Self-Powered Sensors and Systems Based on Nanogenerators. Sensors 2020, 20, 2925.
- Zou, Y.; Raveendran, V.; Chen, J. Wearable triboelectric nanogenerators for biomechanical energy harvesting. Nano Energy 2020, 77, 105303.
- Yin, R.; Wang, D.; Zhao, S.; Lou, Z.; Shen, G. Wearable Sensors-Enabled Human–Machine Interaction Systems: From Design to Application. Adv. Funct. Mater. 2021, 31, 2008936.
- Yao, S.; Swetha, P.; Zhu, Y. Nanomaterial-Enabled Wearable Sensors for Healthcare. Adv. Healthc. Mater. 2017, 7, 1700889.
- Kakria, P.; Tripathi, N.K.; Kitipawang, P. A Real-Time Health Monitoring System for Remote Cardiac Patients Using Smartphone and Wearable Sensors. Int. J. Telemed. Appl. 2015, 2015, 373474.
- Wood, M.A.; Ellenbogen, K.A. Cardiac Pacemakers from the Patient’s Perspective. Circulation 2002, 105, 2136–2138.
- Ali, A.; Pasha, R.A.; Sheeraz, M.A.; Butt, Z.; Elahi, H.; Khan, A.A. Investigation of Electrical Properties for Cantilever-Based Piezoelectric Energy Harvester. Adv. Sci. Technol. Res. J. 2019, 13, 76–85.
- Park, S.W.; Das, P.S.; Chhetry, A.; Park, J.Y. A Flexible Capacitive Pressure Sensor for Wearable Respiration Monitoring System. IEEE Sens. J. 2017, 17, 6558–6564.
- Dinh, T.; Nguyen, T.; Phan, H.-P.; Nguyen, N.-T.; Dao, D.V.; Bell, J.; Dinh, T.; Nguyen, T.; Phan, H.-P.; Nguyen, N.-T.; et al. Stretchable respiration sensors: Advanced designs and multifunctional platforms for wearable physiological monitoring. Biosens. Bioelectron. 2020, 166, 112460.
- Liu, X.; Zhao, C.; Zheng, B.; Guo, Q.; Duan, X.; Wulamu, A.; Zhang, D. Wearable Devices for Gait Analysis in Intelligent Healthcare. Front. Comput. Sci. 2021, 3, 42.
- Majumder, S.; Mondal, T.; Deen, M.J. A Simple, Low-Cost and Efficient Gait Analyzer for Wearable Healthcare Applications. IEEE Sens. J. 2018, 19, 2320–2329.
- Shelgikar, A.V.; Anderson, P.F.; Stephens, M.R. Sleep Tracking, Wearable Technology, and Opportunities for Research and Clinical Care. Chest 2016, 150, 732–743.
- Peng, M.; Ding, Z.; Wang, L.; Cheng, X. Detection of Sleep Biosignals Using an Intelligent Mattress Based on Piezoelectric Ceramic Sensors. Sensors 2019, 19, 3843.
- Li, Z.; Marks, H.; Evans, C.L.; Apiou-Sbirlea, G. Sensing, monitoring, and release of therapeutics: The translational journey of next generation bandages. J. Biomed. Opt. 2018, 24, 021201.




