Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Carmelo Biondo | -- | 1746 | 2023-06-21 10:51:53 | | | |
| 2 | Sirius Huang | Meta information modification | 1746 | 2023-06-21 11:22:52 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Mancuso, G.; Midiri, A.; Gerace, E.; Marra, M.; Zummo, S.; Biondo, C. Pathogenesis of Urinary Tract Infections. Encyclopedia. Available online: https://encyclopedia.pub/entry/45913 (accessed on 28 February 2026).
Mancuso G, Midiri A, Gerace E, Marra M, Zummo S, Biondo C. Pathogenesis of Urinary Tract Infections. Encyclopedia. Available at: https://encyclopedia.pub/entry/45913. Accessed February 28, 2026.
Mancuso, Giuseppe, Angelina Midiri, Elisabetta Gerace, Maria Marra, Sebastiana Zummo, Carmelo Biondo. "Pathogenesis of Urinary Tract Infections" Encyclopedia, https://encyclopedia.pub/entry/45913 (accessed February 28, 2026).
Mancuso, G., Midiri, A., Gerace, E., Marra, M., Zummo, S., & Biondo, C. (2023, June 21). Pathogenesis of Urinary Tract Infections. In Encyclopedia. https://encyclopedia.pub/entry/45913
Mancuso, Giuseppe, et al. "Pathogenesis of Urinary Tract Infections." Encyclopedia. Web. 21 June, 2023.
Copy Citation
Urinary tract infections (UTIs) are among the most common bacterial infections worldwide, occurring in both community and healthcare settings. Although the clinical symptoms of UTIs are heterogeneous and range from uncomplicated (uUTIs) to complicated (cUTIs), most UTIs are usually treated empirically. Bacteria are the main causative agents of these infections, although more rarely, other microorganisms, such as fungi and some viruses, have been reported to be responsible for UTIs.
uropathogens
virulence factors
pathogenesis
antibiotic resistance
1. Introduction
The urinary system consists of the kidneys, ureters, bladder, and urethra, and its main function is to filter blood by removing waste products and excess water. The urinary system plays a key role in removing the waste products of metabolism from the bloodstream. Other important functions performed by the system are the normalization of the concentration of ions and solutes in the blood and the regulation of blood volume and blood pressure [1]. In healthy people, urine is sterile or contains very few microorganisms that can cause an infection [2]. Urinary tract infections (UTIs) are infections that can occur in the urethra (urethritis), bladder (cystitis), or kidneys (pyelonephritis) and are one of the world’s most common infectious diseases, affecting 150 million people each year, with significant morbidity and high medical costs (e.g., it has been estimated that the economic burden of recurrent UTIs in the United States is more than $5 billion each year) [3][4]. Although symptomatology varies depending on the location of these infections, UTIs have a negative impact on patients’ relationships, both intimate and social, resulting in a decreased quality of life [5][6]. UTIs are classified as either uncomplicated (uUTIs) or complicated (cUTIs) [7]. uUTIs typically affect healthy patients in the absence of structural or neurological abnormalities of the urinary tract [4]. cUTIs are defined as complicated when they are associated with urinary tract abnormalities that increase susceptibility to infection, such as catheterization or functional or anatomical abnormalities (e.g., obstructive uropathy, urinary retention, neurogenic bladder, renal failure, pregnancy, and the presence of calculi) [4][8].
In both community and hospital settings, the Enterobacteriaceae family is predominant in UTIs, and the main isolated pathogen is uropathogenic Escherichia coli (UPEC) [9][10]. The latter is also the most common causative agent of cUTI [10]. Antibiotic-resistant Gram-negative bacteria are more prevalent in hospitals than in community samples (e.g., carbapenemase-resistant Enterobacteriaceae) [11]. UTIs are mainly caused by bacteria, while the involvement of other microorganisms, such as fungi and viruses, is quite rare. Candida albicans is the most common type of fungus that causes UTIs. Common causes of viral UTI are cytomegalovirus, type 1 human Polyomavirus, and herpes simplex virus [12][13].
2. Pathogenesis of UTI
Urinary tract infections (UTIs) begin when gut-resident uropathogens colonize the urethra and subsequently the bladder through the action of specific adhesins. If the host’s inflammatory response fails to eliminate all bacteria, they begin to multiply, producing toxins and enzymes that promote their survival. Subsequent colonization of the kidneys can evolve into bacteremia if the pathogen crosses the kidney epithelial barrier (Figure 1). In complicated UTIs, infection by uropathogens is followed by bladder compromise, which occurs with catheterization. A very common situation is the accumulation of fibrinogen on the catheter as a result of the strong immune response induced by catheterization. Uropathogens, through the expression of fibrinogen-binding proteins, bind to the catheter. Bacteria also multiply as a result of biofilm protection, and if the infection is left untreated, it can progress to pyelonephritis and bacteremia (Figure 1). UTIs are the most common bacterial infection in humans worldwide and the most common hospital-acquired infection [14][15]. The spread of UTIs is closely linked to the effectiveness of a number of strategies that uropathogens have developed to adhere to and invade host tissues [16][17]. Often, the infection does not seem particularly severe, especially in the early stages, but it can worsen significantly in the presence of complicating factors [18][19]. Complicating factors that are involved in the progression of UTI are biofilms, urinary stasis due to obstruction, and catheters. UTIs comprise a heterogeneous group of clinical disorders that vary in terms of the etiology and severity of conditions. The risk of UTI is influenced by a wide range of intrinsic and acquired factors, such as urinary retention, vesicoureteral reflux, frequent sexual intercourse, prostate gland enlargement, vulvovaginal atrophy, and family history. The use of spermicides may also increase the risk of UTI in women [19][20]. A urine culture with ≥105 colony-forming units/mL without any specific UTI symptoms is defined asymptomatic bacteriuria, as it usually resolves spontaneously and does not require treatment [21]. Asymptomatic UTIs should be treated only in selected cases, such as pregnant women, neutropenic patients, and those undergoing genitourinary surgery, as antibiotic treatment may contribute to the development of bacterial resistance [22][23]. In contrast, symptomatic UTIs are commonly treated with antibiotics that can alter the intestinal and vaginal microbiota, increasing the risk factors for the spread of multidrug-resistant microorganisms [4][23][24].
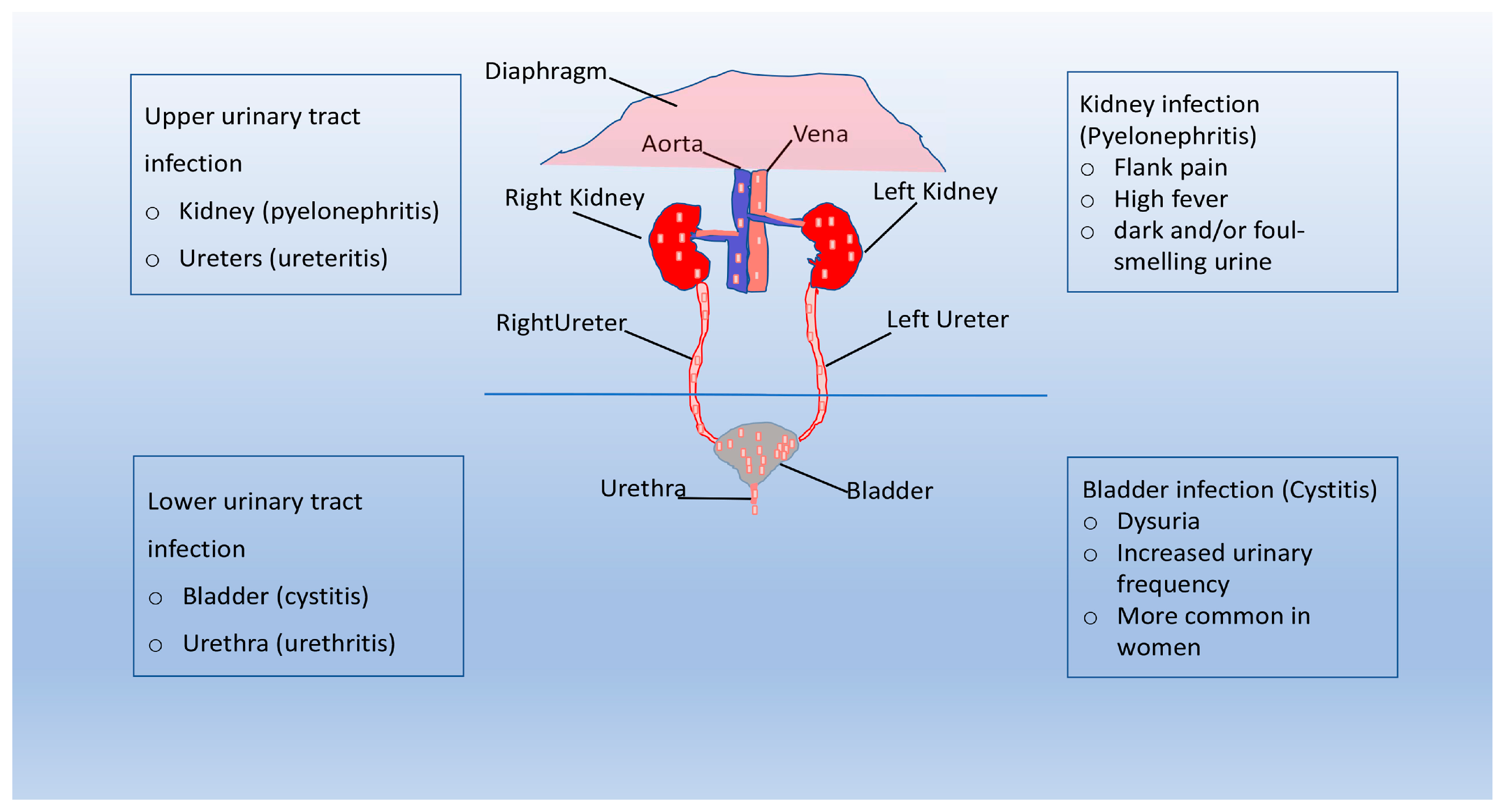
Figure 1. Pathogenesis of UTI. Urinary tract infections (UTIs) start when uropathogens colonize the urethra and subsequently the bladder through the action of specific adhesins. If the bacteria are able to evade the immune system, they begin to multiply and biofilms form. Bacteria can reach the kidney from the lower urinary tract, and UTI can evolve into bacteremia. In complicated UTI, uropathogens are usually able to bind to the catheter and multiply due to the protection of the biofilm. If left untreated, the infection can progress to pyelonephritis and bacteraemia.
3. Classification of UTI
In general, UTIs are named according to the site of infection: urethritis is inflammation of the urethra, ureteritis refers to inflammation of the ureter, and cystitis and pyelonephritis involve the bladder and kidney, respectively [25]. UTIs are further classified according to the presence of predisposing conditions for infection (uncomplicated or complicated) or the nature of the event (primary or recurrent) [25][26][27]. In most cases, uUTIs are caused by uropathogens that reside in the intestine and, after accidental contamination of the urethra, migrate, colonizing the bladder [28]. While sharing the same dynamics described for uncomplicated infections, cUTIs occur in the presence of predisposing factors, such as functional or structural abnormalities of the urinary tract [29]. Other typical features of complicated UTIs include a significantly higher rate of treatment failure and systemic or invasive tissue involvement [22][28]. Three or more uncomplicated UTIs within 12 months or two or more infections within six months define recurrent UTIs; usually, recurrences in this type of infection are due to the same microorganism responsible for the previous infections [30][31].
4. Immune Response to Uropathogens
Although the urinary tract is often exposed to microorganisms from the gastrointestinal tract, infection by these microorganisms is a rather rare occurrence due to the innate immune defenses of the urinary tract [32]. Previous studies have shown that the immune response is carefully regulated so as not to compromise the structural integrity of the epithelial barrier. Macrophages and mast cells play a key role in immune regulation of the urinary tract, coordinating the recruitment and initiation of neutrophil responses that lead to the removal of bacteria in the bladder. In addition, these cells are critical in preventing an excessive neutrophil response from causing damage to bladder tissue and predisposing this organ to persistent infection [33].
5. Virulence Factors of the Main Uropathogens
The ability of different uropathogens to successfully adhere to and colonize the epithelium of the lower urinary tract is related to their ability to express specific virulence factors [34]. Uropathogenic E. coli (UPEC) is the most common causative agent of both uUTIs and cUTIs [34]. Most UTIs are caused by Gram-negative and Gram-positive bacteria residing in the colon, such as Escherichia coli, Enterococcus faecalis, Proteus mirabilis, and Klebsiella pneumoniae [4][34]. Other causative agents include Staphylococcus saprophyticus, Group B Streptococcus (GBS), and Pseudomonas aeruginosa [4]. Figure 2 shows the epidemiology of different uropathogens in uUTIs and cUTIs. On the cell surface of uropathogens are several adhesion proteins that play a crucial role in the initial interactions between the host and pathogen [34]. In addition, adhesins have recently been found to promote both the attachment of bacteria and invasion of host tissues in the urinary tract. Among the best-known adhesion factors are the pili of uropathogenic bacteria belonging to both Gram-positive and Gram-negative bacteria. Two distinct pathways are required for pili assembly in Gram-negative and Gram-positive bacteria, known as the chaperone/usher pathway and the sortase-assembled pili pathway, respectively [34]. These uropathogens use different types of adhesins that promote binding and biofilm formation on biotic and abiotic surfaces. In this context, it is important to note that most UTIs are biofilm-associated infections in which uropathogens colonize both the mucosa of the urinary tract and indwelling devices such as urinary catheters [35]. Biofilm formation by these pathogenic bacteria requires specific virulence factors that play a key role in inducing adhesion to host epithelial cells or catheter materials [35][36]. Bacterial biofilms play an important role in UTIs, being responsible for the persistence of infections that result in recurrence and relapse. Since eradication of biofilms often cannot be achieved by antibiotic treatment, new approaches for eradication of aggressive biofilms are being tested, such as phagotherapy, enzymatic degradation, antimicrobic peptides, and nanoparticles [37]. Table 1 shows the main types of adhesins that are crucial for biofilm formation. These structures promote the attachment of uropathogens to biotic/abiotic surfaces. Uropathogens are also producers of toxins, proteases (e.g., elastase and phospho-lipase) and iron-harvesting siderophores, all of which are involved in the onset and spread of UTIs [38].
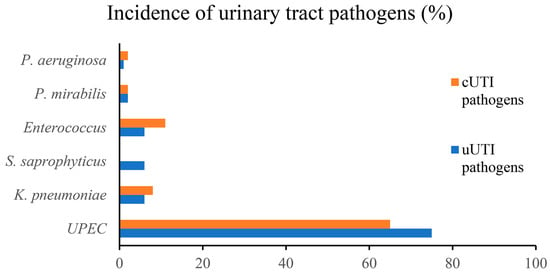
Figure 2. Epidemiology of uropathogens in uUTIs and cUTIs.
Table 1. Main types of adhesins expressed by Gram-negative and Gram-positive uropathogens.
| Uropathogens | Adhesin | Biotic/Abiotic Surface | References |
|---|---|---|---|
| E. coli (UPEC) | Type 1 fimbriae Type 2, P fimbriae Dr adhesion S fimbriae F1C |
binds to kidney cells and promotes the formation of a biofilm binds to Globosides, a sub-class of the lipid class glycosphingolipid. binds bladder and kidney epithelial cells binds to receptors containing sialic acid binds to glycolipid receptors present in the endothelial cells of bladder and kidney and promotes biofilm formation |
[39] [40] [41] [42] [43] |
| K. pneumoniae | Type 1 fimbriae Type 3 fimbriae |
Binds to the mannose-binding receptors and promote biofilm formation on abiotic surfaces promote biofilm formation on abiotic surfaces |
[44] [44] |
| P. aeruginosa | T4Pa | Binds to glycosphingolipid receptors present in host epithelial cells and promotes biofilm formation. | [34] |
| P. mirabilis | MRP fimbriae | binds mannosylated glycoproteins of bladder cells | [45] |
| NAF fimbriae Mrp/H |
binds with glycolipids promote the formation of biofilms in the urinary tract |
[45][46] | |
| S. saprophyticus | Aas adhesin SdrI adhesin Uaf adhesin |
binds to human ureters binds to collagens binds to bladder epithelial cells |
[34] |
| E. faecalis | Enterococcal Surface Protein | promote primary attachment and biofilm formation on biotic and abiotic surface | [47] |
UPEC: UroPathogenic Escherichia coli; F1C, type 1-like immunological group C pili; T4Pa, type IV pili; MRP, mannose-resistant Proteus fimbriae; NAF, Non-agglutinating fimbriae; Aas, autolysin/adhesin of Staphylococcus saprophyticus; SdrI, serine-aspartate repeat proteins; Uaf, Uro-adherence factor.
References
- Stamm, W.E.; Norrby, S.R. Urinary tract infections: Disease panorama and challenges. J. Infect. Dis. 2001, 183 (Suppl. S1), S1–S4.
- Wolfe, A.J.; Brubaker, L. “Sterile Urine” and the Presence of Bacteria. Eur. Urol. 2015, 68, 173–174.
- McCann, E.; Sung, A.H.; Ye, G.; Vankeepuram, L.; Tabak, Y.P. Contributing Factors to the Clinical and Economic Burden of Patients with Laboratory-Confirmed Carbapenem-Nonsusceptible Gram-Negative Urinary Tract Infections. Clin. Outcomes Res. CEOR 2020, 12, 191–200.
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015, 13, 269–284.
- Naber, K.G.; Tiran-Saucedo, J.; Wagenlehner, F.M.E. Psychosocial burden of recurrent uncomplicated urinary tract infections. GMS Infect. Dis. 2022, 10, Doc01.
- Grigoryan, L.; Mulgirigama, A.; Powell, M.; Schmiemann, G. The emotional impact of urinary tract infections in women: A qualitative analysis. BMC Women’s Health 2022, 22, 182.
- Johnson, J.R. Definitions of Complicated Urinary Tract Infection and Pyelonephritis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2017, 64, 390.
- Dason, S.; Dason, J.T.; Kapoor, A. Guidelines for the diagnosis and management of recurrent urinary tract infection in women. Can. Urol. Assoc. 2011, 5, 316–322.
- Bader, M.S.; Loeb, M.; Brooks, A.A. An update on the management of urinary tract infections in the era of antimicrobial resistance. Postgrad. Med. 2017, 129, 242–258.
- Bader, M.S.; Loeb, M.; Leto, D.; Brooks, A.A. Treatment of urinary tract infections in the era of antimicrobial resistance and new antimicrobial agents. Postgrad. Med. 2020, 132, 234–250.
- Mancini, A.; Pucciarelli, S.; Lombardi, F.E.; Barocci, S.; Pauri, P.; Lodolini, S. Differences between Community—And Hospital—Acquired urinary tract infections in a tertiary care hospital. New Microbiol. 2020, 43, 17–21.
- Olin, S.J.; Bartges, J.W. Urinary tract infections: Treatment/comparative therapeutics. Vet. Clin. N. Am. Small Anim. Pract. 2015, 45, 721–746.
- Paduch, D.A. Viral lower urinary tract infections. Curr. Urol. Rep. 2007, 8, 324–335.
- McLellan, L.K.; Hunstad, D.A. Urinary Tract Infection: Pathogenesis and Outlook. Trends Mol. Med. 2016, 22, 946–957.
- Saint, S.; Kowalski, C.P.; Kaufman, S.R.; Hofer, T.P.; Kauffman, C.A.; Olmsted, R.N.; Forman, J.; Banaszak-Holl, J.; Damschroder, L.; Krein, S.L. Preventing hospital-acquired urinary tract infection in the United States: A national study. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2008, 46, 243–250.
- Lewis, A.J.; Richards, A.C.; Mulvey, M.A. Invasion of Host Cells and Tissues by Uropathogenic Bacteria. Microbiol. Spectr. 2016, 4, 359–381.
- Wiles, T.J.; Kulesus, R.R.; Mulvey, M.A. Origins and virulence mechanisms of uropathogenic Escherichia coli. Exp. Mol. Pathol. 2008, 85, 11–19.
- Zagaglia, C.; Ammendolia, M.G.; Maurizi, L.; Nicoletti, M.; Longhi, C. Urinary Tract Infections Caused by Uropathogenic Escherichia coli Strains-New Strategies for an Old Pathogen. Microorganisms 2022, 10, 1425.
- Storme, O.; Tiran Saucedo, J.; Garcia-Mora, A.; Dehesa-Davila, M.; Naber, K.G. Risk factors and predisposing conditions for urinary tract infection. Ther. Adv. Urol. 2019, 11, 1756287218814382.
- Craven, B.C.; Alavinia, S.M.; Gajewski, J.B.; Parmar, R.; Disher, S.; Ethans, K.; Shepherd, J.; Omidvar, M.; Farahani, F.; Hassouna, M.; et al. Conception and development of Urinary Tract Infection indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J. Spinal Cord Med. 2019, 42, 205–214.
- Wiley, Z.; Jacob, J.T.; Burd, E.M. Targeting Asymptomatic Bacteriuria in Antimicrobial Stewardship: The Role of the Microbiology Laboratory. J. Clin. Microbiol. 2020, 58, e00518-18.
- Luu, T.; Albarillo, F.S. Asymptomatic Bacteriuria: Prevalence, Diagnosis, Management, and Current Antimicrobial Stewardship Implementations. Am. J. Med. 2022, 135, e236–e244.
- Ourani, M.; Honda, N.S.; MacDonald, W.; Roberts, J. Evaluation of evidence-based urinalysis reflex to culture criteria: Impact on reducing antimicrobial usage. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2021, 102, 40–44.
- Mestrovic, T.; Matijasic, M.; Peric, M.; Cipcic Paljetak, H.; Baresic, A.; Verbanac, D. The Role of Gut, Vaginal, and Urinary Microbiome in Urinary Tract Infections: From Bench to Bedside. Diagnostics 2020, 11, 7.
- Huang, L.; Huang, C.; Yan, Y.; Sun, L.; Li, H. Urinary Tract Infection Etiological Profiles and Antibiotic Resistance Patterns Varied Among Different Age Categories: A Retrospective Study From a Tertiary General Hospital During a 12-Year Period. Front. Microbiol. 2021, 12, 813145.
- Li, X.; Fan, H.; Zi, H.; Hu, H.; Li, B.; Huang, J.; Luo, P.; Zeng, X. Global and Regional Burden of Bacterial Antimicrobial Resistance in Urinary Tract Infections in 2019. J. Clin. Med. 2022, 11, 2817.
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655.
- Klein, R.D.; Hultgren, S.J. Urinary tract infections: Microbial pathogenesis, host-pathogen interactions and new treatment strategies. Nat. Rev. Microbiol. 2020, 18, 211–226.
- Gomila, A.; Shaw, E.; Carratala, J.; Leibovici, L.; Tebe, C.; Wiegand, I.; Vallejo-Torres, L.; Vigo, J.M.; Morris, S.; Stoddart, M.; et al. Predictive factors for multidrug-resistant gram-negative bacteria among hospitalised patients with complicated urinary tract infections. Antimicrob. Resist. Infect. Control 2018, 7, 111.
- Nicolle, L.E. Complicated urinary tract infection in adults. Can. J. Infect. Dis. Med. Microbiol. 2005, 16, 349–360.
- Rando, E.; Giovannenze, F.; Murri, R.; Sacco, E. A review of recent advances in the treatment of adults with complicated urinary tract infection. Expert Rev. Clin. Pharmacol. 2022, 15, 1053–1066.
- Abraham, S.N.; Miao, Y. The nature of immune responses to urinary tract infections. Nat. Rev. Immunol. 2015, 15, 655–663.
- Li, L.; Li, Y.; Yang, J.; Xie, X.; Chen, H. The immune responses to different Uropathogens call individual interventions for bladder infection. Front. Immunol. 2022, 13, 953354.
- Govindarajan, D.K.; Kandaswamy, K. Virulence factors of uropathogens and their role in host pathogen interactions. Cell Surf. 2022, 8, 100075.
- Shrestha, L.B.; Baral, R.; Khanal, B. Comparative study of antimicrobial resistance and biofilm formation among Gram-positive uropathogens isolated from community-acquired urinary tract infections and catheter-associated urinary tract infections. Infect. Drug Resist. 2019, 12, 957–963.
- Jacobsen, S.M.; Shirtliff, M.E. Proteus mirabilis biofilms and catheter-associated urinary tract infections. Virulence 2011, 2, 460–465.
- Amankwah, S.; Abdella, K.; Kassa, T. Bacterial Biofilm Destruction: A Focused Review On The Recent Use of Phage-Based Strategies With Other Antibiofilm Agents. Nanotechnol. Sci. Appl. 2021, 14, 161–177.
- van Buul, L.W.; Vreeken, H.L.; Bradley, S.F.; Crnich, C.J.; Drinka, P.J.; Geerlings, S.E.; Jump, R.L.P.; Mody, L.; Mylotte, J.J.; Loeb, M.; et al. The Development of a Decision Tool for the Empiric Treatment of Suspected Urinary Tract Infection in Frail Older Adults: A Delphi Consensus Procedure. J. Am. Med. Dir. Assoc. 2018, 19, 757–764.
- Staerk, K.; Khandige, S.; Kolmos, H.J.; Moller-Jensen, J.; Andersen, T.E. Uropathogenic Escherichia coli Express Type 1 Fimbriae Only in Surface Adherent Populations Under Physiological Growth Conditions. J. Infect. Dis. 2016, 213, 386–394.
- Shah, C.; Baral, R.; Bartaula, B.; Shrestha, L.B. Virulence factors of uropathogenic Escherichia coli (UPEC) and correlation with antimicrobial resistance. BMC Microbiol. 2019, 19, 204.
- Mulvey, M.A. Adhesion and entry of uropathogenic Escherichia coli. Cell. Microbiol. 2002, 4, 257–271.
- Miyazaki, J.; Ba-Thein, W.; Kumao, T.; Obata Yasuoka, M.; Akaza, H.; Hayshi, H. Type 1, P and S fimbriae, and afimbrial adhesin I are not essential for uropathogenic Escherichia coli to adhere to and invade bladder epithelial cells. FEMS Immunol. Med. Microbiol. 2002, 33, 23–26.
- Behzadi, P. Classical chaperone-usher (CU) adhesive fimbriome: Uropathogenic Escherichia coli (UPEC) and urinary tract infections (UTIs). Folia Microbiol. 2020, 65, 45–65.
- Schroll, C.; Barken, K.B.; Krogfelt, K.A.; Struve, C. Role of type 1 and type 3 fimbriae in Klebsiella pneumoniae biofilm formation. BMC Microbiol. 2010, 10, 179.
- Scavone, P.; Iribarnegaray, V.; Caetano, A.L.; Schlapp, G.; Hartel, S.; Zunino, P. Fimbriae have distinguishable roles in Proteus mirabilis biofilm formation. Pathog. Dis. 2016, 74, ftw03.
- Jiang, W.; Ubhayasekera, W.; Breed, M.C.; Norsworthy, A.N.; Serr, N.; Mobley, H.L.T.; Pearson, M.M.; Knight, S.D. MrpH, a new class of metal-binding adhesin, requires zinc to mediate biofilm formation. PLoS Pathog. 2020, 16, e1008707.
- Toledo-Arana, A.; Valle, J.; Solano, C.; Arrizubieta, M.J.; Cucarella, C.; Lamata, M.; Amorena, B.; Leiva, J.; Penades, J.R.; Lasa, I. The enterococcal surface protein, Esp, is involved in Enterococcus faecalis biofilm formation. Appl. Environ. Microbiol. 2001, 67, 4538–4545.
More
Information
Subjects:
Infectious Diseases
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
2.9K
Revisions:
2 times
(View History)
Update Date:
21 Jun 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





