Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Andrea Vianello | -- | 2013 | 2023-06-21 09:37:28 | | | |
| 2 | Rita Xu | -3 word(s) | 2010 | 2023-06-21 09:59:02 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Guarnieri, G.; Iervolino, M.; Cavallone, S.; Unfer, V.; Vianello, A. Asthma-Polycystic Ovary Overlap Syndrome. Encyclopedia. Available online: https://encyclopedia.pub/entry/45907 (accessed on 13 January 2026).
Guarnieri G, Iervolino M, Cavallone S, Unfer V, Vianello A. Asthma-Polycystic Ovary Overlap Syndrome. Encyclopedia. Available at: https://encyclopedia.pub/entry/45907. Accessed January 13, 2026.
Guarnieri, Gabriella, Matteo Iervolino, Sara Cavallone, Vittorio Unfer, Andrea Vianello. "Asthma-Polycystic Ovary Overlap Syndrome" Encyclopedia, https://encyclopedia.pub/entry/45907 (accessed January 13, 2026).
Guarnieri, G., Iervolino, M., Cavallone, S., Unfer, V., & Vianello, A. (2023, June 21). Asthma-Polycystic Ovary Overlap Syndrome. In Encyclopedia. https://encyclopedia.pub/entry/45907
Guarnieri, Gabriella, et al. "Asthma-Polycystic Ovary Overlap Syndrome." Encyclopedia. Web. 21 June, 2023.
Copy Citation
Asthma is a heterogeneous inflammatory disease characterized by abnormalities in immune response. Due to the inherent complexity of the disease and the presence of comorbidities, asthma control is often difficult to obtain. In asthmatic patients, an increased prevalence of irregular menstrual cycles, infertility, obesity, and insulin resistance has been reported.
asthma
polycystic ovary syndrome
premenstrual asthma
1. Introduction
With an estimate of over 43 million new cases worldwide each year [1], asthma is one of the most common chronic diseases in the world. Globally, over 260 million people have poorly controlled asthma [2], making this condition the second leading cause of death among chronic respiratory diseases, with 450,000 deaths in 2017 [3]. Indeed, approximately 5% of asthmatics do not respond to standard therapy and are classified as “difficult to control”. Failure to achieve adequate control can be attributed to several factors, including comorbidities, which may impair the response to therapy and complicate patients’ clinical course. Pathophysiological mechanisms of asthma involve immune system cells (mast cells, eosinophils, neutrophils, and innate lymphoid cells), cytokines, and genetic factors [4].
In asthmatic patients, the most common symptoms include recurrent or episodic wheezing, shortness of breath, chest tightness, and cough, mainly occurring during night time or early in the morning, after exercise or as a result of exposure to allergens/cold air, or after intake of medications such as acetylsalicylic acid or β-blockers. Clinical suspicion of asthma is confirmed by the results of pulmonary function tests, which may detect a partially or fully reversible airflow limitation. Given that baseline pulmonary function evaluation may result in the normal range during intercritical periods, a more detailed assessment, including methacholine challenge test, serial peak flow monitoring, and measurement of airway inflammation may become essential to make a correct diagnosis [5][6].
Sputum eosinophil count is important for assessing asthma phenotype and predicting the response to biologic therapies. In the patient workup, it is also critical to evaluate risk factors such as allergic diathesis or occupational exposure. In-depth questionnaires may aid in the diagnostic path of bronchial asthma [7].
Most asthmatic patients have multiple comorbidities including rhinitis, sinusitis with or without nasal polyps, airway infections, gastro-esophageal reflux disease, obesity, sleep-related breathing disorders, anxiety and depression, and polycystic ovary syndrome (PCOS). Adequate treatment of comorbidities is essential to achieve satisfactory asthma control [8].
Gender differences should be taken into consideration when deciding therapeutic strategies in asthma patients [9][10][11][12]. Indeed, the risk of hospitalization for asthma exacerbation in adult women of childbearing age is higher than men, whereas levels are similar when considering the postmenopausal period [13][14].
Asthma Endotypes
In an effort to optimize the approach to the diagnosis and management of asthma patients, a classification of the disease based on different endotypes has been adopted in recent years. Endotypes can be distinguished according to the predominant inflammatory pathway and related biomarkers. They can be categorized as type 2-high (T2-high) endotypes, presenting with eosinophilic airway infiltrate and TH2-dependent cytokine overexpression (IL-4, IL-5, and IL-13) and type 2-low (T2-low) endotypes, showing neutrophilic and pauci-granulocytic airway infiltrates promoted by IL-6, IL-8, IL-17, IL-22, and epithelial cell-derived cytokines belonging to type 1 and 3 immunity [15]. Most patients with T2-high endotype report early disease onset, although a clear age-related cut-off has not yet been identified. In patients with T2-high asthma, biomarkers have been identified (i.e., sputum and blood eosinophils, exhaled nitric oxide, and blood IgE levels) that can be used to predict the response to biologic treatment [16].
Unlike this, T2-low endotype patients commonly report later disease onset and symptoms that are usually absent during childhood. Moreover, the prevalence of both female gender and obesity is unexpectedly high. Of importance, patients with T2-low asthma do not respond effectively to corticosteroid therapy [16][17].
Both asthma and PCOS are multifactorial, chronic, and very complex diseases. For this reason, identifying common pathways could allow researchers to optimize the therapeutic approach to both conditions. The aim is to identify pathophysiological and clinical similarities between asthma and PCOS (Figure 1) and evaluate whether myo-inositol (myo-Ins), a treatment currently utilized in patients with PCOS, may also have benefits in subjects with asthma.
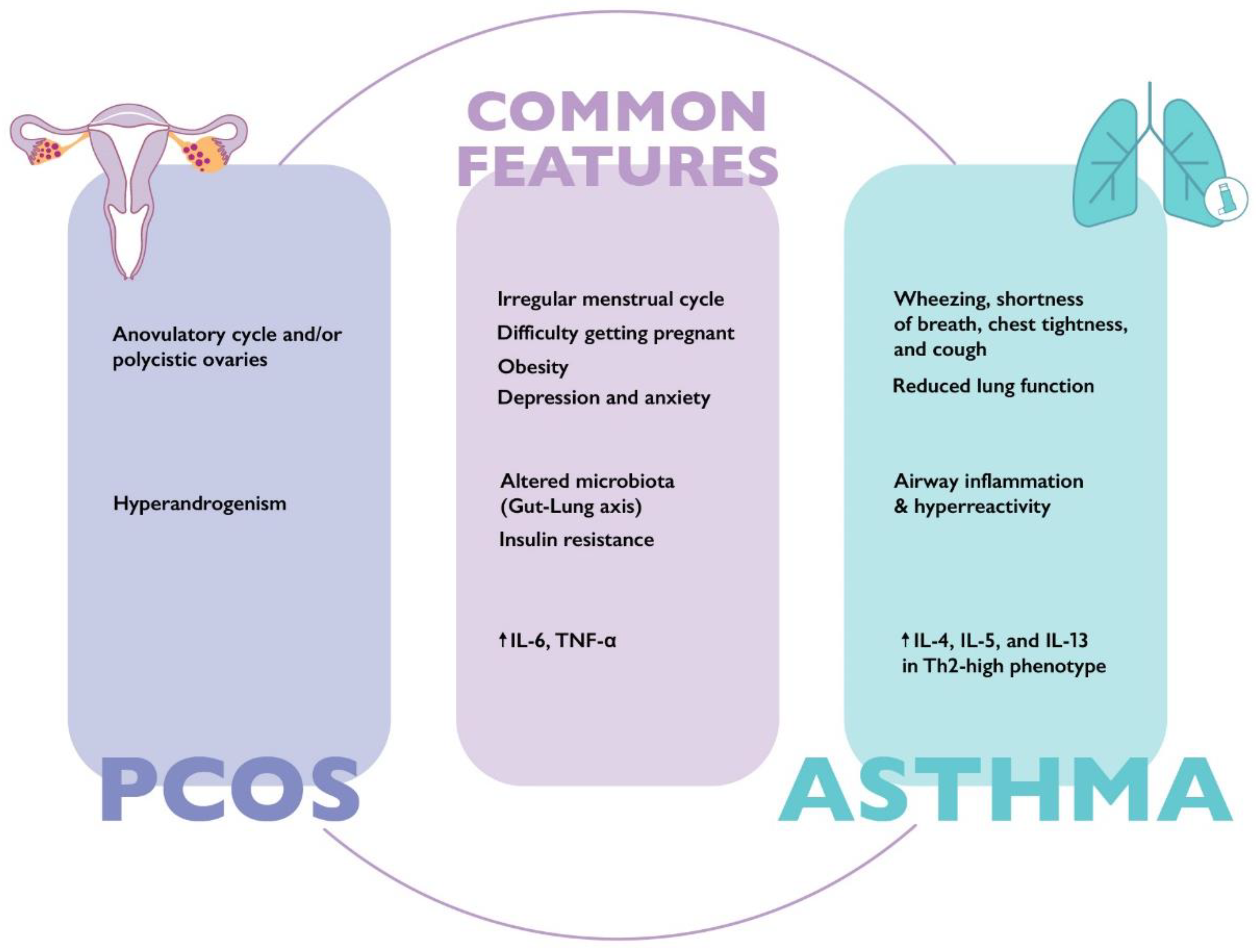
Figure 1. Main clinical and laboratory characteristics of asthma and polycystic ovary syndrome. IL-4: interleukin 4; IL-5: interleukin 5; IL-6: interleukin 6; IL-13: interleukin 13; TNF-α: tumor necrosis factor alpha; Th2: T helper 2.
2. The Therapeutic Role of Myo-Inositol in Patients with “Asthma-PCOS Overlap Syndrome”
2.1. Structural and Functional Characteristics of Myo-Inositol
A natural compound, myo-inositol (myo-Ins) raised considerable interest among clinicians, due to its safety profile and the growing evidence of its effectiveness in managing PCOS [18][19][20][21]. Myo-Ins is the most abundant inositol in the human body, showing different physiological functions. Indeed, it was found to be a G-protein coupled second messenger involved in hormone signaling, in particular insulin, follicle-stimulating hormone (FSH), thyroid stimulating hormone (TSH), serotonin, acetylcholine, and dopamine signaling [22][23][24][25][26].
As a second messenger of FSH, myo-Ins has been widely used for managing PCOS, in particular for facilitating ovulation. Moreover, myo-Ins can improve pregnancy outcomes in women undergoing ART [27][28][29], restore hormonal balance, reduce acne and hirsutism [30][31], and limit the probability of developing gestational diabetes (GDM) [32]. Importantly, it was found to be extremely safe, even at high doses [33]. Myo-Ins can increase insulin sensitivity and was proven to be as effective as metformin in improving metabolic control [34][35][36][37].
Myo-Ins is an essential component of lung surfactant, which in turn plays a fundamental role in reducing alveolar surface tension. The composition of lung surfactant includes surfactant protein A (SP-A) and D (SP-D), both of which act as a barrier to pathogens and modulate inflammatory response [38].
An alteration in surfactant synthesis was demonstrated in obese asthmatic patients, in particular a reduction in SP-A protein [39], which can be explained by increased secretory phospholipase A (2) [sPLA(2)] and eosinophil lysophospholipase activity [40]. It is important to note that myo-Ins is involved in the SP-A activation pathway via PI3K. Indeed, it can prevent SP-A-induced rise in macrophage mannose receptor (MR) expression through inhibition of PI3K function. PI3K plays a role in SP-A upregulation, and, in turn, SP-A induces a rise in IP3, activating the Ca2+/PLC/IP3 signal transduction pathway [41][42].
2.2. Therapeutic Role of Myo-Inositol in Lung Disorders
The efficacy and safety of myo-Ins in the treatment of lung diseases have been assessed by several trials. In a phase 1 study evaluating the safety, tolerability, and chemo-preventive effect of its oral administration, myo-Ins showed a protective effect on tracheo-bronchial mucosa, leading to a significant regression of bronchial dysplastic lesions. Moreover, it was proven to be safe even at high doses, causing mild side effects at gastrointestinal level [43].
In line with these results, myo-Ins showed a chemo-preventive effect on the development of bronchial dysplasia in smoking patients. A protective effect on lesion progression and the ability to reduce the serum level of inflammatory cytokines, in particular IL-6, were demonstrated [44]. Laganà et al. suggested that IL-6 reduction could be mediated by inositol-requiring enzyme 1 (IRE1), X-box-binding protein 1 (XBP1), and activation of transcription 3 (STAT3) pathways. Myo-Ins supplementation also increased surfactant concentration by stimulating PI3K [45]. A study conducted on premature infants with respiratory distress syndrome (RDS) showed that myo-Ins reduced the risk of lung damage and was associated with a lower mortality rate compared to the placebo group [46][47]. In this regard, a systematic review from the Cochrane library concluded that myo-Ins supplementation may significantly reduce short-term adverse neonatal outcomes and the incidence of bronchopulmonary dysplasia [48].
Several studies reported that myo-Ins has the potential to reduce inflammation and oxidative stress [49][50]. Of interest, myo-Ins was found to decrease the level of inflammation mediated by the NF-kB pathway in patients with severe asthma [50].
2.3. Routes of Drug Administration
When focusing on myo-Ins therapeutic effect on lung disease, inhalation route should be preferred. Indeed, inhalation route can be rapidly effective, reduce the risk of side effects, and avoid first-pass metabolism [51]. A pilot study demonstrated that nebulized myo-Ins was able to reduce symptoms and increase SpO2 levels in patients with various lung diseases, including asthma [52].
If orally administered, myo-Ins is absorbed at the intestinal level via sodium/myo-Ins transporters (SMIT1/2). A study by Orrù et al. found that a twice-dose 2 g oral myo-Ins in powder form could effectively cover 24 h. There are no sex differences in myo-Ins absorption [53]. Several factors can influence the absorption of myo-Ins, including the simultaneous intake of food or beverages containing sugar or sugar substitutes [54]. Coffee may also interfere with the absorption of myo-Ins [55].
Of interest, several studies showed that overall restoration of ovulation in PCOS women treated with myo-Ins was between 60% and 70% [56][57][58]. High body mass index (BMI), obesity, insulin resistance, and dysbiosis were identified as possible causes of “inositol resistance”.
To increase the proportion of responders to treatment, optimizing myo-Ins absorption is essential [58]. Alpha-lactalbumin(α-LA), a small protein with a molecular weight of 14.2 kDa, and the major whey protein of breast milk may contribute to creating a healthy gut environment. α-LA also has anti-inflammatory, muco-protective, and trophic properties, improving the absorption of micronutrients. For this reason, the hypothesis was advanced that it may increase oral absorption of inositol [59][60].
A study by Monastra et al. demonstrated that α-LA improved the absorption of myo-Ins both in vitro and in vivo as measured by plasma levels compared to myo-Ins alone. The study also evaluated the improvement of myo-Ins absorption in human intestine Caco-2 cells, showing a 4.5 times greater trans-epithelial passage of myo-Ins in the intestinal human cells if it was combined with 10 mg/mL of α-LA [61]. Montanino et al. conducted a clinical study to evaluate whether myo-Ins efficacy could be improved when combined with α-LA. Initially, myo-inositol was administered to anovulatory PCOS patients as monotherapy at a dose of 2 g twice a day for 3 months. As a result, ovulation was not restored in 38% of cases, who were considered “inositol resistant”. Subsequently, the “inositol resistant” subgroup was supplemented with 2 g of myo-Ins plus 50 mg α-LA twice a day for further 3 months, resulting in the restoration of ovulation in 86% of cases [62].
Different mechanisms have been hypothesized to explain why α-LA may improve myo-Ins absorption. First, α-LA can modify intestinal tight junctions by stimulating the secretion of glucagon-like peptide-2 (GLP 2) [63]. Intestinal tight junctions create a dynamic barrier between epithelial and endothelial cells and regulate the diffusion of molecules, especially nutrients and micronutrients. On the other hand, glucagon-like peptide-2, promotes the absorption of nutrients by stimulating intestinal cell proliferation and regeneration [64][65]. Modulating tight junction function and stimulating GLP 2, α-LA can increase the uptake of various natural compounds [64][66].
Second, due to its probiotic activity, α-LA promotes the growth of bacteria that may improve gut health, such as Lactobacilli and Bifidobacteria, which are commonly reduced in the microbiota of PCOS women. Furthermore, α-LA may adhere to intestinal cells and prevent infection by enteropathogenic bacteria such as E. coli, S. typhiumurium and S. flexneri, and K. pneumonia [67].
Third, α-LA exerts an anti-inflammatory activity through the inhibition of cyclooxygenase (COX) and phospholipase A2 enzymes. Indeed, studies on animal models showed a reduction in inflammatory cytokines IL-6 and Prostaglandin E2 (PGE2) [60].
A study conducted by D’Anna et al. in pregnant women with gestational diabetes (GDM) confirmed the efficacy of combining 2 g of myo-Ins with 50 mg of α-LA twice a day. In fact, after two months of combined treatment, a statistically significant reduction in insulin resistance and improved fetal growth was reported in the treatment group versus placebo. Moreover, a decrease in the number of women who required insulin treatment and pre-term birth was evident [68].
Finally, Hernandez-Marin et al. showed that the combined treatment of myo-Ins and α-LA improved hormonal and metabolic parameters in PCOS patients. In particular, HOMA-index, LH, and androstenedione improved after 3 and 6 months of treatment in both Italian and Mexican populations [69]. To date, randomized control trials aimed at demonstrating whether oral administration of myo-Ins combined with α-LA may be effective in patients with airway/lung disease, including asthma are lacking.
In the event of asthma flare-up, rapid relief of symptoms is a fundamental need for patients. For this reason, nebulized myo-Ins pharmacokinetic studies analyzing its action speed and duration are essential to evaluate its therapeutic role in exacerbated patients.
In summary, even though evidence on pharmacokinetics is limited and study results on its therapeutic effect are scarce, preliminary data on the possible use of myo-Ins in patients with asthma are encouraging.
References
- Mattiuzzi, C.; Lippi, G. Worldwide asthma epidemiology: Insights from the Global Health Data Exchange database. Int. Forum. Allergy Rhinol. 2020, 10, 75–80.
- Song, P.; Adeloye, D.; Salim, H.; Dos Santos, J.P.; Campbell, H.; Sheikh, A.; Rudan, I. Global, regional, and national prevalence of asthma in 2019: A systematic analysis and modelling study. J. Glob. Health 2022, 12, 04052.
- Cao, Y.; Chen, S.; Chen, X.; Zou, W.; Liu, Z.; Wu, Y.; Hu, S. Global trends in the incidence and mortality of asthma from 1990 to 2019: An age-period-cohort analysis using the global burden of disease study 2019. Front. Public Health 2022, 10, 1036674.
- Holgate, S.T.; Wenzel, S.; Postma, D.S.; Weiss, S.T.; Renz, H.; Sly, P.D. Asthma. Nat. Rev. Dis. Prim. 2015, 10, 15025.
- Available online: www.ginasthma.org (accessed on 1 March 2023).
- Khatri, S.B.; Iaccarino, J.M.; Barochia, A.; Soghier, I.; Akuthota, P.; Brady, A.; Covar, R.A.; Debley, J.S.; Diamant, Z.; Fitzpatrick, A.M.; et al. American Thoracic Society Assembly on Allergy, Immunology, and Inflammation. Use of Fractional Exhaled Nitric Oxide to Guide the Treatment of Asthma: An Official American Thoracic Society Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2021, 204, 97–109.
- Kaplan, A.G.; Balter, M.S.; Bell, A.D.; Kim, H.; McIvor, R.A. Diagnosis of asthma in adults. CMAJ 2009, 181, E210–E220.
- Varkonyi-Sepp, J.; Freeman, A.; Ainsworth, B.; Kadalayil, L.P.; Haitchi, H.M.; Kurukulaaratchy, R.J. Multimorbidity in Difficult Asthma: The Need for Personalised and Non-Pharmacological Approaches to Address a Difficult Breathing Syndrome. J. Pers. Med. 2022, 12, 1435.
- Graziottin, A.; Serafini, A. Perimenstrual asthma: From pathophysiology to treatment strategies. Multidiscip. Respir. Med. 2016, 11, 30.
- Calcaterra, V.; Nappi, R.E.; Farolfi, A.; Tiranini, L.; Rossi, V.; Regalbuto, C.; Zuccotti, G. Perimenstrual Asthma in Adolescents: A Shared Condition in Pediatric and Gynecological Endocrinology. Children 2022, 9, 233.
- Zhang, G.Q.; Ermis, S.S.O.; Rådinger, M.; Bossios, A.; Kankaanranta, H.; Nwaru, B. Sex Disparities in Asthma Development and Clinical Outcomes: Implications for Treatment Strategies. J. Asthma Allergy 2022, 15, 231–247.
- Jenkins, C.R.; Boulet, L.P.; Lavoie, K.L.; Raherison-Semjen, C.; Singh, D. Personalized Treatment of Asthma: The Importance of Sex and Gender Differences. J. Allergy Clin. Immunol. Pract. 2022, 10, 963–971.e3.
- Chowdhury, N.U.; Guntur, V.P.; Newcomb, D.C.; Wechsler, M.E. Sex and gender in asthma. Eur. Respir. Rev. 2021, 30, 210067.
- Senna, G.; Latorre, M.; Bugiani, M.; Caminati, M.; Heffler, E.; Morrone, D.; Paoletti, G.; Parronchi, P.; Puggioni, F.; Blasi, F.; et al. Sex Differences in Severe Asthma: Results from Severe Asthma Network in Italy-SANI. Allergy Asthma. Immunol. Res. 2021, 13, 219–228.
- Ricciardolo, F.L.M.; Sprio, A.E.; Baroso, A.; Gallo, F.; Riccardi, E.; Bertolini, F.; Carriero, V.; Arrigo, E.; Ciprandi, G. Characterization of T2-Low and T2-High asthma phenotypes in real-life. Biomedicines 2021, 9, 1684.
- Wenzel, S.E. Asthma phenotypes: The evolution from clinical to molecular approaches. Nat. Med. 2012, 18, 716–725.
- Logotheti, M.; Agioutantis, P.; Katsaounou, P.; Loutrari, H. Microbiome Research and Multi-Omics Integration for Personalized Medicine in Asthma. J. Pers. Med. 2021, 11, 1299.
- Unfer, V.; Nestler, J.E.; Kamenov, Z.A.; Prapas, N.; Facchinetti, F. Effects of Inositol(s) in Women with PCOS: A Systematic Review of Randomized Controlled Trials. Int. J. Endocrinol. 2016, 2016, 1849162.
- Kamenov, Z.; Gateva, A. Inositols in PCOS. Molecules 2020, 27, 5566.
- Cantelmi, T.; Lambiase, E.; Unfer, V.R.; Gambioli, R.; Unfer, V. Inositol treatment for psychological symptoms in Polycystic Ovary Syndrome women. Eur. Rev. Med. Pharm. Sci. 2021, 25, 2383–2389.
- Pkhaladze, L.; Russo, M.; Unfer, V.; Nordio, M.; Basciani, S.; Khomasuridze, A. Treatment of lean PCOS teenagers: A follow-up comparison between Myo-Inositol and oral contraceptives. Eur. Rev. Med. Pharm. Sci. 2021, 25, 7476–7485.
- Merviel, P.; James, P.; Bouée, S.; Le Guillou, M.; Rince, C.; Nachtergaele, C.; Kerlan, V. Impact of myo-inositol treatment in women with polycystic ovary syndrome in assisted reproductive technologies. Reprod. Health 2021, 19, 13.
- Elsaid, S.; Rubin-Kahana, D.S.; Kloiber, S.; Kennedy, S.H.; Chavez, S.; Le Foll, B. Neurochemical Alterations in Social Anxiety Disorder (SAD): A Systematic Review of Proton Magnetic Resonance Spectroscopic Studies. Int. J. Mol. Sci. 2022, 26, 4754.
- Taylor, C.W.; Tovey, S.C. IP(3) receptors: Toward understanding their activation. Cold Spring Harb. Perspect. Biol. 2010, 2, a004010.
- Cappelli, V.; Musacchio, M.C.; Bulfoni, A.; Morgante, G.; De Leo, V. Natural molecules for the therapy of hyperandrogenism and metabolic disorders in PCOS. Eur. Rev. Med. Pharm. Sci. 2017, 21 (Suppl. S2), 15–29.
- Benvenga, S.; Antonelli, A. Inositol(s) in thyroid function, growth, and autoimmunity. Rev. Endocr. Metab. Disord. 2016, 17, 471–484.
- Pundir, J.; Psaroudakis, D.; Savnur, P.; Bhide, P.; Sabatini, L.; Teede, H.; Coomarasamy, A.; Thangaratinam, S. Inositol treatment of anovulation in women with polycystic ovary syndrome: A meta-analysis of randomised trials. BJOG 2018, 125, 299–308.
- Vartanyan, E.V.; Tsaturova, K.A.; Devyatova, E.A.; Mikhaylyukova, A.S.; Levin, V.A.; Petuhova, N.L.; Markin, A.V.; Steptsova, E.M. Improvement in quality of oocytes in polycystic ovarian syndrome in programs of in vitro fertilization. Gynecol. Endocrinol. 2017, 33 (Suppl. S1), 8–11.
- Regidor, P.A.; Schindler, A.E. Myoinositol as a Safe and Alternative Approach in the Treatment of Infertile PCOS Women: A German Observational Study. Int. J. Endocrinol. 2016, 2016, 9537632.
- Zacchè, M.M.; Caputo, L.; Filippis, S.; Zacchè, G.; Dindelli, M.; Ferrari, A. Efficacy of myo-inositol in the treatment of cutaneous disorders in young women with polycystic ovary syndrome. Gynecol. Endocrinol. 2009, 25, 508–513.
- Minozzi, M.; D’Andrea, G.; Unfer, V. Treatment of hirsutism with myo-inositol: A prospective clinical study. Reprod. Biomed. Online 2008, 17, 579–582.
- Vitagliano, A.; Saccone, G.; Cosmi, E.; Visentin, S.; Dessole, F.; Ambrosini, G.; Berghella, V. Inositol for the prevention of gestational diabetes: A systematic review and meta-analysis of randomized controlled trials. Arch. Gynecol. Obs. 2019, 299, 55–68.
- Carlomagno, G.; Unfer, V. Inositol safety: Clinical evidences. Eur. Rev. Med. Pharm. Sci. 2011, 15, 931–936.
- Genazzani, A.D.; Santagni, S.; Ricchieri, F.; Campedelli, A.; Rattighieri, E.; Chierchia, E.; Marini, G.; Despini, G.; Prati, A.; Simoncini, T. Myo-inositol modulates insulin and luteinizing hormone secretion in normal weight patients with polycystic ovary syndrome. J. Obs. Gynaecol. Res. 2014, 40, 1353–1360.
- Unfer, V.; Facchinetti, F.; Orrù, B.; Giordani, B.; Nestler, J. Myo-inositol effects in women with PCOS: A meta-analysis of randomized controlled trials. Endocr. Connect. 2017, 6, 647–658.
- Zhang, J.Q.; Xing, C.; He, B. Short period-administration of myo-inositol and metformin on hormonal and glycolipid profiles in patients with polycystic ovary syndrome: A systematic review and updated meta-analysis of randomized controlled trials. Eur. Rev. Med. Pharm. Sci. 2022, 26, 1792–1802.
- Unfer, V.; Porcaro, G. Updates on the myo-inositol plus D-chiro-inositol combined therapy in polycystic ovary syndrome. Expert Rev. Clin. Pharm. 2014, 7, 623–631.
- Crouch, E.; Wright, J.R. Surfactant proteins a and d and pulmonary host defense. Annu. Rev. Physiol. 2001, 63, 521–554.
- Lugogo, N.; Francisco, D.; Addison, K.J.; Manne, A.; Pederson, W.; Ingram, J.L.; Green, C.L.; Suratt, B.T.; Lee, J.J.; Sunday, M.E.; et al. Obese asthmatic patients have decreased surfactant protein A levels: Mechanisms and implications. J. Allergy Clin. Immunol. 2018, 141, 918–926.e3.
- Kwatia, M.A.; Doyle, C.B.; Cho, W.; Enhorning, G.; Ackerman, S.J. Combined activities of secretory phospholipases and eosinophil lysophospholipases induce pulmonary surfactant dysfunction by phospholipid hydrolysis. J. Allergy Clin. Immunol. 2007, 119, 838–847.
- Ogasawara, Y.; Kuroki, Y.; Akino, T. Pulmonary surfactant protein D specifically binds to phosphatidylinositol. J. Biol. Chem. 1992, 267, 21244–21249.
- Ogasawara, Y.; McCormack, F.X.; Mason, R.J.; Voelker, D.R. Chimeras of surfactant proteins A and D identify the carbohydrate recognition domains as essential for phospholipid interaction. J. Biol. Chem. 1994, 269, 29785–29792.
- Lam, S.; McWilliams, A.; LeRiche, J.; MacAulay, C.; Wattenberg, L.; Szabo, E. A phase I study of myo-inositol for lung cancer chemoprevention. Cancer Epidemiol. Biomark. Prev. 2006, 15, 1526–1531.
- Lam, S.; Mandrekar, S.J.; Gesthalter, Y.; Allen Ziegler, K.L.; Seisler, D.K.; Midthun, D.E.; Mao, J.T.; Aubry, M.C.; McWilliams, A.; Sin, D.D.; et al. Cancer Prevention Network. A Randomized Phase IIb Trial of myo-Inositol in Smokers with Bronchial Dysplasia. Cancer Prev. Res. 2016, 9, 906–914.
- Laganà, A.S.; Unfer, V.; Garzon, S.; Bizzarri, M. Role of inositol to improve surfactant functions and reduce IL-6 levels: A potential adjuvant strategy for SARS-CoV-2 pneumonia? Med. Hypotheses 2020, 144, 110262.
- Hallman, M.; Bry, K.; Hoppu, K.; Lappi, M.; Pohjavuori, M. Inositol supplementation in premature infants with respiratory distress syndrome. N. Engl. J. Med. 1992, 326, 1233–1239.
- Spengler, D.; Winoto-Morbach, S.; Kupsch, S.; Vock, C.; Blöchle, K.; Frank, S.; Rintz, N.; Diekötter, M.; Janga, H.; Weckmann, M.; et al. Novel therapeutic roles for surfactant-inositols and-phosphatidylglycerols in a neonatal piglet ARDS model: A translational study. Am. J. Physiol. Lung Cell. Mol. Physiol. 2018, 314, L32–L53.
- Howlett, A.; Ohlsson, A.; Plakkal, N. Inositol in preterm infants at risk for or having respiratory distress syndrome. Cochrane Database Syst. Rev. 2015, 2, CD000366.
- Baldassarre, M.P.A.; Di Tomo, P.; Centorame, G.; Pandolfi, A.; Di Pietro, N.; Consoli, A.; Formoso, G. Myoinositol Reduces Inflammation and Oxidative Stress in Human Endothelial Cells Exposed In Vivo to Chronic Hyperglycemia. Nutrients 2021, 13, 2210.
- Gagliardo, R.; Chanez, P.; Mathieu, M.; Bruno, A.; Costanzo, G.; Gougat, C.; Vachier, I.; Bousquet, J.; Bonsignore, G.; Vignola, A.M. Persistent activation of nuclear factor-kappaB signaling pathway in severe uncontrolled asthma. Am. J. Respir. Crit. Care Med. 2003, 168, 1190–1198.
- Alipour, S.; Mahmoudi, L.; Ahmadi, F. Pulmonary drug delivery: An effective and convenient delivery route to combat COVID-19. Drug Deliv. Transl. Res. 2022, 19, 1–11.
- Spiga, A. Nebulized myo-Inositol increases oxygen saturation and relieves symptoms in patients with airways diseases. IJMDAT 2021, 4, e356.
- Orrù, B.; Circo, R.; Logoteta, P.; Petousis, S.; Carlomagno, G. Finding the best therapeutic approach for PCOS: The importance of inositol(s) bioavailability. Eur. Rev. Med. Pharm. Sci. 2017, 21 (Suppl. S2), 83–88.
- Dinicola, S.; Minini, M.; Unfer, V.; Verna, R.; Cucina, A.; Bizzarri, M. Nutritional and Acquired Deficiencies in Inositol Bioavailability. Correlations with Metabolic Disorders. Int. J. Mol. Sci. 2017, 18, 2187.
- De Grazia, S.; Carlomagno, G.; Unfer, V.; Cavalli, P. Myo-inositol soft gel capsules may prevent the risk of coffee-induced neural tube defects. Expert Opin. Drug Deliv. 2012, 9, 1033–1039.
- Kamenov, Z.; Kolarov, G.; Gateva, A.; Carlomagno, G.; Genazzani, A.D. Ovulation induction with myo-inositol alone and in combination with clomiphene citrate in polycystic ovarian syndrome patients with insulin resistance. Gynecol. Endocrinol. 2015, 31, 131–135.
- Raffone, E.; Rizzo, P.; Benedetto, V. Insulin sensitiser agents alone and in co-treatment with r-FSH for ovulation induction in PCOS women. Gynecol. Endocrinol. 2010, 26, 275–280.
- Gerli, S.; Papaleo, E.; Ferrari, A.; Di Renzo, G.C. Randomized, double blind placebo-controlled trial: Effects of myo-inositol on ovarian function and metabolic factors in women with PCOS. Eur. Rev. Med. Pharm. Sci. 2007, 11, 347–354.
- Grases, F.; Simonet, B.M.; Vucenik, I.; Prieto, R.M.; Costa-Bauzá, A.; March, J.G.; Shamsuddin, A.M. Absorption and excretion of orally administered inositol hexaphosphate (IP(6) or phytate) in humans. Biofactors 2001, 15, 53–61.
- Yamaguchi, M.; Yoshida, K.; Uchida, M. Novel functions of bovine milk-derived alpha-lactalbumin: Anti-nociceptive and anti-inflammatory activity caused by inhibiting cyclooxygenase-2 and phospholipase A2. Biol. Pharm. Bull. 2009, 32, 366–371.
- Monastra, G.; Sambuy, Y.; Ferruzza, S.; Ferrari, D.; Ranaldi, G. Alpha-lactalbumin Effect on Myo-inositol Intestinal Absorption: In vivo and In vitro. Curr. Drug Deliv. 2018, 15, 1305–1311.
- Montanino Oliva, M.; Buonomo, G.; Calcagno, M.; Unfer, V. Effects of myo-inositol plus alpha-lactalbumin in myo-inositol-resistant PCOS women. J. Ovarian Res. 2018, 10, 38.
- Manish, R.P.; Jignesh, S.; Varsha, N. The Role of Alpha-Lactalbumin with Myoinositol in the Treatment of PCOS: A Review. Asian Res. J. Gynaecol. Obs. 2022, 8, 5–11.
- Izumi, H.; Ishizuka, S.; Inafune, A.; Hira, T.; Ozawa, K.; Shimizu, T.; Takase, M.; Hara, H. Alpha-Lactalbumin hydrolysate stimulates glucagon-like peptide-2 secretion and small intestinal growth in suckling rats. J. Nutr. 2009, 139, 1322–1327.
- Förster, C. Tight junctions and the modulation of barrier function in disease. Histochem. Cell Biol. 2008, 130, 55–70.
- Lemmer, H.J.; Hamman, J.H. Paracellular drug absorption enhancement through tight junction modulation. Expert Opin. Drug Deliv. 2013, 10, 103–114.
- Cardinale, V.; Lepore, E.; Basciani, S.; Artale, S.; Nordio, M.; Bizzarri, M.; Unfer, V. Positive Effects of α-Lactalbumin in the Management of Symptoms of Polycystic Ovary Syndrome. Nutrients 2022, 14, 3220.
- D’Anna, R.; Corrado, F.; Loddo, S.; Gullo, G.; Giunta, L.; Di Benedetto, A. Myoinositol plus α-lactalbumin supplementation, insulin resistance and birth outcomes in women with gestational diabetes mellitus: A randomized, controlled study. Sci. Rep. 2021, 11, 8866.
- Hernandez Marin, I.; Picconi, O.; Laganà, A.S.; Costabile, L.; Unfer, V. A multicenter clinical study with myo-inositol and alpha-lactalbumin in Mexican and Italian PCOS patients. Eur. Rev. Med. Pharm. Sci. 2021, 25, 3316–3324.
More
Information
Subjects:
Pharmacology & Pharmacy
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
825
Revisions:
2 times
(View History)
Update Date:
21 Jun 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




