Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Andrea Vianello and Version 2 by Rita Xu.
Asthma is a heterogeneous inflammatory disease characterized by abnormalities in immune response. Due to the inherent complexity of the disease and the presence of comorbidities, asthma control is often difficult to obtain. In asthmatic patients, an increased prevalence of irregular menstrual cycles, infertility, obesity, and insulin resistance has been reported.
- asthma
- polycystic ovary syndrome
- premenstrual asthma
1. Introduction
With an estimate of over 43 million new cases worldwide each year [1], asthma is one of the most common chronic diseases in the world. Globally, over 260 million people have poorly controlled asthma [2], making this condition the second leading cause of death among chronic respiratory diseases, with 450,000 deaths in 2017 [3]. Indeed, approximately 5% of asthmatics do not respond to standard therapy and are classified as “difficult to control”. Failure to achieve adequate control can be attributed to several factors, including comorbidities, which may impair the response to therapy and complicate patients’ clinical course. Pathophysiological mechanisms of asthma involve immune system cells (mast cells, eosinophils, neutrophils, and innate lymphoid cells), cytokines, and genetic factors [4].
In asthmatic patients, the most common symptoms include recurrent or episodic wheezing, shortness of breath, chest tightness, and cough, mainly occurring during night time or early in the morning, after exercise or as a result of exposure to allergens/cold air, or after intake of medications such as acetylsalicylic acid or β-blockers. Clinical suspicion of asthma is confirmed by the results of pulmonary function tests, which may detect a partially or fully reversible airflow limitation. Given that baseline pulmonary function evaluation may result in the normal range during intercritical periods, a more detailed assessment, including methacholine challenge test, serial peak flow monitoring, and measurement of airway inflammation may become essential to make a correct diagnosis [5][6][5,6].
Sputum eosinophil count is important for assessing asthma phenotype and predicting the response to biologic therapies. In the patient workup, it is also critical to evaluate risk factors such as allergic diathesis or occupational exposure. In-depth questionnaires may aid in the diagnostic path of bronchial asthma [7].
Most asthmatic patients have multiple comorbidities including rhinitis, sinusitis with or without nasal polyps, airway infections, gastro-esophageal reflux disease, obesity, sleep-related breathing disorders, anxiety and depression, and polycystic ovary syndrome (PCOS). Adequate treatment of comorbidities is essential to achieve satisfactory asthma control [8].
Gender differences should be taken into consideration when deciding therapeutic strategies in asthma patients [9][10][11][12][9,10,11,12]. Indeed, the risk of hospitalization for asthma exacerbation in adult women of childbearing age is higher than men, whereas levels are similar when considering the postmenopausal period [13][14][13,14].
Asthma Endotypes
In an effort to optimize the approach to the diagnosis and management of asthma patients, a classification of the disease based on different endotypes has been adopted in recent years. Endotypes can be distinguished according to the predominant inflammatory pathway and related biomarkers. They can be categorized as type 2-high (T2-high) endotypes, presenting with eosinophilic airway infiltrate and TH2-dependent cytokine overexpression (IL-4, IL-5, and IL-13) and type 2-low (T2-low) endotypes, showing neutrophilic and pauci-granulocytic airway infiltrates promoted by IL-6, IL-8, IL-17, IL-22, and epithelial cell-derived cytokines belonging to type 1 and 3 immunity [15][27]. Most patients with T2-high endotype report early disease onset, although a clear age-related cut-off has not yet been identified. In patients with T2-high asthma, biomarkers have been identified (i.e., sputum and blood eosinophils, exhaled nitric oxide, and blood IgE levels) that can be used to predict the response to biologic treatment [16][28]. Unlike this, T2-low endotype patients commonly report later disease onset and symptoms that are usually absent during childhood. Moreover, the prevalence of both female gender and obesity is unexpectedly high. Of importance, patients with T2-low asthma do not respond effectively to corticosteroid therapy [16][17][28,29]. Both asthma and PCOS are multifactorial, chronic, and very complex diseases. For this reason, identifying common pathways could allow reusearchers to optimize the therapeutic approach to both conditions. The aim is of this review is to identify pathophysiological and clinical similarities between asthma and PCOS (Figure 1) and evaluate whether myo-inositol (myo-Ins), a treatment currently utilized in patients with PCOS, may also have benefits in subjects with asthma.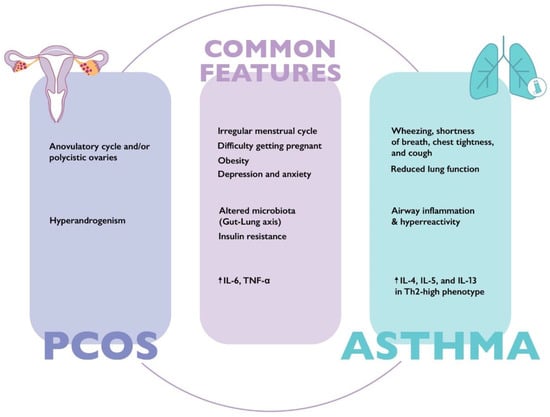
Figure 1. Main clinical and laboratory characteristics of asthma and polycystic ovary syndrome. IL-4: interleukin 4; IL-5: interleukin 5; IL-6: interleukin 6; IL-13: interleukin 13; TNF-α: tumor necrosis factor alpha; Th2: T helper 2.
2. The Therapeutic Role of Myo-Inositol in Patients with “Asthma-PCOS Overlap Syndrome”
2.1. Structural and Functional Characteristics of Myo-Inositol
A natural compound, myo-inositol (myo-Ins) raised considerable interest among clinicians, due to its safety profile and the growing evidence of its effectiveness in managing PCOS [18][19][20][21][82,83,84,85]. Myo-Ins is the most abundant inositol in the human body, showing different physiological functions. Indeed, it was found to be a G-protein coupled second messenger involved in hormone signaling, in particular insulin, follicle-stimulating hormone (FSH), thyroid stimulating hormone (TSH), serotonin, acetylcholine, and dopamine signaling [22][23][24][25][26][86,87,88,89,90].
As a second messenger of FSH, myo-Ins has been widely used for managing PCOS, in particular for facilitating ovulation. Moreover, myo-Ins can improve pregnancy outcomes in women undergoing ART [27][28][29][91,92,93], restore hormonal balance, reduce acne and hirsutism [30][31][94,95], and limit the probability of developing gestational diabetes (GDM) [32][96]. Importantly, it was found to be extremely safe, even at high doses [33][97]. Myo-Ins can increase insulin sensitivity and was proven to be as effective as metformin in improving metabolic control [34][35][36][37][98,99,100,101].
Myo-Ins is an essential component of lung surfactant, which in turn plays a fundamental role in reducing alveolar surface tension. The composition of lung surfactant includes surfactant protein A (SP-A) and D (SP-D), both of which act as a barrier to pathogens and modulate inflammatory response [38][102].
An alteration in surfactant synthesis was demonstrated in obese asthmatic patients, in particular a reduction in SP-A protein [39][103], which can be explained by increased secretory phospholipase A (2) [sPLA(2)] and eosinophil lysophospholipase activity [40][104]. It is important to note that myo-Ins is involved in the SP-A activation pathway via PI3K. Indeed, it can prevent SP-A-induced rise in macrophage mannose receptor (MR) expression through inhibition of PI3K function. PI3K plays a role in SP-A upregulation, and, in turn, SP-A induces a rise in IP3, activating the Ca2+/PLC/IP3 signal transduction pathway [41][42][105,106].
2.2. Therapeutic Role of Myo-Inositol in Lung Disorders
The efficacy and safety of myo-Ins in the treatment of lung diseases have been assessed by several trials. In a phase 1 study evaluating the safety, tolerability, and chemo-preventive effect of its oral administration, myo-Ins showed a protective effect on tracheo-bronchial mucosa, leading to a significant regression of bronchial dysplastic lesions. Moreover, it was proven to be safe even at high doses, causing mild side effects at gastrointestinal level [43][107].
In line with these results, myo-Ins showed a chemo-preventive effect on the development of bronchial dysplasia in smoking patients. A protective effect on lesion progression and the ability to reduce the serum level of inflammatory cytokines, in particular IL-6, were demonstrated [44][108]. Laganà et al. suggested that IL-6 reduction could be mediated by inositol-requiring enzyme 1 (IRE1), X-box-binding protein 1 (XBP1), and activation of transcription 3 (STAT3) pathways. Myo-Ins supplementation also increased surfactant concentration by stimulating PI3K [45][109]. A study conducted on premature infants with respiratory distress syndrome (RDS) showed that myo-Ins reduced the risk of lung damage and was associated with a lower mortality rate compared to the placebo group [46][47][110,111]. In this regard, a systematic review from the Cochrane library concluded that myo-Ins supplementation may significantly reduce short-term adverse neonatal outcomes and the incidence of bronchopulmonary dysplasia [48][112].
Several studies reported that myo-Ins has the potential to reduce inflammation and oxidative stress [49][50][113,114]. Of interest, myo-Ins was found to decrease the level of inflammation mediated by the NF-kB pathway in patients with severe asthma [50][114].
2.3. Routes of Drug Administration
When focusing on myo-Ins therapeutic effect on lung disease, inhalation route should be preferred. Indeed, inhalation route can be rapidly effective, reduce the risk of side effects, and avoid first-pass metabolism [51][115]. A pilot study demonstrated that nebulized myo-Ins was able to reduce symptoms and increase SpO2 levels in patients with various lung diseases, including asthma [52][116].
If orally administered, myo-Ins is absorbed at the intestinal level via sodium/myo-Ins transporters (SMIT1/2). A study by Orrù et al. found that a twice-dose 2 g oral myo-Ins in powder form could effectively cover 24 h. There are no sex differences in myo-Ins absorption [53][117]. Several factors can influence the absorption of myo-Ins, including the simultaneous intake of food or beverages containing sugar or sugar substitutes [54][118]. Coffee may also interfere with the absorption of myo-Ins [55][119].
Of interest, several studies showed that overall restoration of ovulation in PCOS women treated with myo-Ins was between 60% and 70% [56][57][58][120,121,122]. High body mass index (BMI), obesity, insulin resistance, and dysbiosis were identified as possible causes of “inositol resistance”.
To increase the proportion of responders to treatment, optimizing myo-Ins absorption is essential [58][122]. Alpha-lactalbumin(α-LA), a small protein with a molecular weight of 14.2 kDa, and the major whey protein of breast milk may contribute to creating a healthy gut environment. α-LA also has anti-inflammatory, muco-protective, and trophic properties, improving the absorption of micronutrients. For this reason, the hypothesis was advanced that it may increase oral absorption of inositol [59][60][123,124].
A study by Monastra et al. demonstrated that α-LA improved the absorption of myo-Ins both in vitro and in vivo as measured by plasma levels compared to myo-Ins alone. The study also evaluated the improvement of myo-Ins absorption in human intestine Caco-2 cells, showing a 4.5 times greater trans-epithelial passage of myo-Ins in the intestinal human cells if it was combined with 10 mg/mL of α-LA [61][125]. Montanino et al. conducted a clinical study to evaluate whether myo-Ins efficacy could be improved when combined with α-LA. Initially, myo-inositol was administered to anovulatory PCOS patients as monotherapy at a dose of 2 g twice a day for 3 months. As a result, ovulation was not restored in 38% of cases, who were considered “inositol resistant”. Subsequently, the “inositol resistant” subgroup was supplemented with 2 g of myo-Ins plus 50 mg α-LA twice a day for further 3 months, resulting in the restoration of ovulation in 86% of cases [62][126].
Different mechanisms have been hypothesized to explain why α-LA may improve myo-Ins absorption. First, α-LA can modify intestinal tight junctions by stimulating the secretion of glucagon-like peptide-2 (GLP 2) [63][127]. Intestinal tight junctions create a dynamic barrier between epithelial and endothelial cells and regulate the diffusion of molecules, especially nutrients and micronutrients. On the other hand, glucagon-like peptide-2, promotes the absorption of nutrients by stimulating intestinal cell proliferation and regeneration [64][65][128,129]. Modulating tight junction function and stimulating GLP 2, α-LA can increase the uptake of various natural compounds [64][66][128,130].
Second, due to its probiotic activity, α-LA promotes the growth of bacteria that may improve gut health, such as Lactobacilli and Bifidobacteria, which are commonly reduced in the microbiota of PCOS women. Furthermore, α-LA may adhere to intestinal cells and prevent infection by enteropathogenic bacteria such as E. coli, S. typhiumurium and S. flexneri, and K. pneumonia [67][131].
Third, α-LA exerts an anti-inflammatory activity through the inhibition of cyclooxygenase (COX) and phospholipase A2 enzymes. Indeed, studies on animal models showed a reduction in inflammatory cytokines IL-6 and Prostaglandin E2 (PGE2) [60][124].
A study conducted by D’Anna et al. in pregnant women with gestational diabetes (GDM) confirmed the efficacy of combining 2 g of myo-Ins with 50 mg of α-LA twice a day. In fact, after two months of combined treatment, a statistically significant reduction in insulin resistance and improved fetal growth was reported in the treatment group versus placebo. Moreover, a decrease in the number of women who required insulin treatment and pre-term birth was evident [68][132].
Finally, Hernandez-Marin et al. showed that the combined treatment of myo-Ins and α-LA improved hormonal and metabolic parameters in PCOS patients. In particular, HOMA-index, LH, and androstenedione improved after 3 and 6 months of treatment in both Italian and Mexican populations [69][133]. To date, randomized control trials aimed at demonstrating whether oral administration of myo-Ins combined with α-LA may be effective in patients with airway/lung disease, including asthma are lacking.
In the event of asthma flare-up, rapid relief of symptoms is a fundamental need for patients. For this reason, nebulized myo-Ins pharmacokinetic studies analyzing its action speed and duration are essential to evaluate its therapeutic role in exacerbated patients.
In summary, even though evidence on pharmacokinetics is limited and study results on its therapeutic effect are scarce, preliminary data on the possible use of myo-Ins in patients with asthma are encouraging.
