Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Landry Rali Hakiza | -- | 1103 | 2023-06-14 10:56:46 | | | |
| 2 | Jessie Wu | + 15 word(s) | 1118 | 2023-06-15 04:25:49 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Hakiza, L.; Sartoretto, A.; Burgmann, K.; Kumbhari, V.; Matter, C.; Seibold, F.; Staudenmann, D. Transoral Outlet Reduction for Roux-en-Y Gastric Bypass. Encyclopedia. Available online: https://encyclopedia.pub/entry/45560 (accessed on 07 February 2026).
Hakiza L, Sartoretto A, Burgmann K, Kumbhari V, Matter C, Seibold F, et al. Transoral Outlet Reduction for Roux-en-Y Gastric Bypass. Encyclopedia. Available at: https://encyclopedia.pub/entry/45560. Accessed February 07, 2026.
Hakiza, Landry, Adrian Sartoretto, Konstantin Burgmann, Vivek Kumbhari, Christoph Matter, Frank Seibold, Dominic Staudenmann. "Transoral Outlet Reduction for Roux-en-Y Gastric Bypass" Encyclopedia, https://encyclopedia.pub/entry/45560 (accessed February 07, 2026).
Hakiza, L., Sartoretto, A., Burgmann, K., Kumbhari, V., Matter, C., Seibold, F., & Staudenmann, D. (2023, June 14). Transoral Outlet Reduction for Roux-en-Y Gastric Bypass. In Encyclopedia. https://encyclopedia.pub/entry/45560
Hakiza, Landry, et al. "Transoral Outlet Reduction for Roux-en-Y Gastric Bypass." Encyclopedia. Web. 14 June, 2023.
Copy Citation
Obesity is a chronic relapsing disease of global pandemic proportions. In this context, an increasing number of patients are undergoing bariatric surgery, which is considered the most effective weight loss treatment for long-term improvement in obesity-related comorbidities. One of the most popular bariatric surgeries is the Roux-en-Y gastric bypass (RYGB).
endoscopic transoral outlet reduction
bariatric endoscopy
obesity
gastric bypass
dumping syndrome
weight
1. Transoral Outlet Reduction for Weight Regain after Roux-en-Y Gastric Bypass
Weight recidivism is a common complication following Roux-en-Y gastric bypass (RYGB) surgery. On average, patients regain between 20 and 30 % of lost weight, and moreover, excessive weight gain is experienced by over one third of patients [1][2]. Weight regain after gastric bypass is often multifactorial and can be attributed to eating patterns, and psychological and social factors. However, dilatation or enlargement of the gastrojejunal anastomosis of >30 mm is a significant predictor of weight regain following RYGB [3][4][5]. Due to the technical complexity of the anatomy, surgical re-intervention is accompanied by a high risk of complications and an increase in postoperative morbidity and mortality [6]. As an alternative, transoral outlet reduction (TORe) was developed in 2013 as an endoscopic procedure focusing on reducing the size of the gastrojejunal anastomosis (GJA) [7]. The first interventional study included 25 patients with an average weight regain of 24 kg after RYGB [7]. This research described endoscopically reducing the diameter of the anastomosis by an average of 77.3% which was associated with an average weight loss of 11.5 kg, 11.7 kg and 10.8 kg at 3, 6 and 12 months, respectively [7].
Vargas et al. demonstrated in a multicenter study that TORe is a safe, reproducible and effective approach to managing weight recidivism after RYGB [8]. The average weight loss at 6, 12 and 18 months was 9.31 ± 6.7 kg, 7.75 ± 8.4 kg and 8 ± 8.8 kg, respectively, and no serious adverse events were reported [8].
2. Transoral Outlet Reduction for Dumping Syndrome after Roux-en-Y Gastric Bypass
Dumping syndrome (DS) is a postprandial phenomenon in which patients present with a constellation of gastrointestinal and vasomotor symptoms, including tachycardia, fatigue, syncope, and occasionally, shock and seizures due to profound hypoglycemia [9]. Symptoms may occur early (within 1 h of a meal) or up to 3 h later, the latter being associated with postprandial hypoglycemia. As the name suggests, DS occurs, in part, due to rapid gastric emptying, leading to rapid passage of food into the small intestine [10][11]. The patient’s typical history and blood sugar determination inform the diagnosis. The Sigstad score (a score >7 is strongly suggestive of dumping) and questionnaires may also be helpful [10].
A conservative stepwise approach is currently recommended, starting with dietary changes in the form of more frequent meals with increased protein content and lower overall carbohydrate content, favoring complex carbohydrates [12][13]. If dietary measures prove unsuccessful, drug therapy can be initiated with acarbose, calcium antagonists or GLP-1 analogues [14].
However, dietary restrictions and pharmacological treatments are often ineffective or poorly tolerated [10][11]. In these cases, TORe provides a solution by reducing the speed of gastric emptying, however there is no clear consensus in the literature regarding the place of surgical re-intervention in treating dumping syndrome [10][15][16][17].
A large study involving 115 patients from two large academic centers in the United States and Germany supported TORe as an effective and safe adjuvant therapy to lifestyle and pharmacologic treatment of refractory DS [18]. The Sigstad score reduced significantly after only 3 months post-TORe, with the mean sore changing from 17 ± 6.1 to 2.6 ± 1.9 [18]. Similarly, Brown et al. demonstrated a 90% rate of resolution of DS after only 3 months of revision [19].
3. Transoral Outlet Reduction Technique
TORe is currently the most frequently used technique for the reduction of a dilated GJA (Figure 1A). The intervention is usually performed under general anesthesia. A double-lumen gastroscope is passed through a proprietary overtube of 25 cm in length, and CO2 is used for insufflation. It can be carried out on an outpatient basis, and it is typically performed with argon plasma coagulation (APC) combined with full-thickness suturing achieved using the OverStitchTM device (Apollo Endosurgery, Austin, TX, USA) [5][20][21]. This combined technique allows for greater durability of anastomotic reduction by inducing fibrosis of the GJA [22][23]. The first step of the procedure is to ablate the gastric rim of the anastomosis via APC (forced APC, 0.8 L/min with 30–70 watts) (Figure 1B), followed by a circumferential, transmural endoscopic suture (Figure 1C). Suturing is mainly performed via the creation of a purse-string, or alternatively, by placing interrupted sutures at the GJA [18]. The purse-string technique is, however, generally favored, as it results in more significant weight loss at one year than interrupted suture patterns [24]. Ideally, a dilation balloon (CRE balloon dilator, Boston Scientific, Marlborough, MA, USA) is introduced through the second channel of the endoscope and inflated to a diameter of 8–10 mm (Figure 1D) to size the GJA before the suture is tightened and cinched over the balloon, allowing the GJA to be precisely sized (Figure 1E and Video S1).
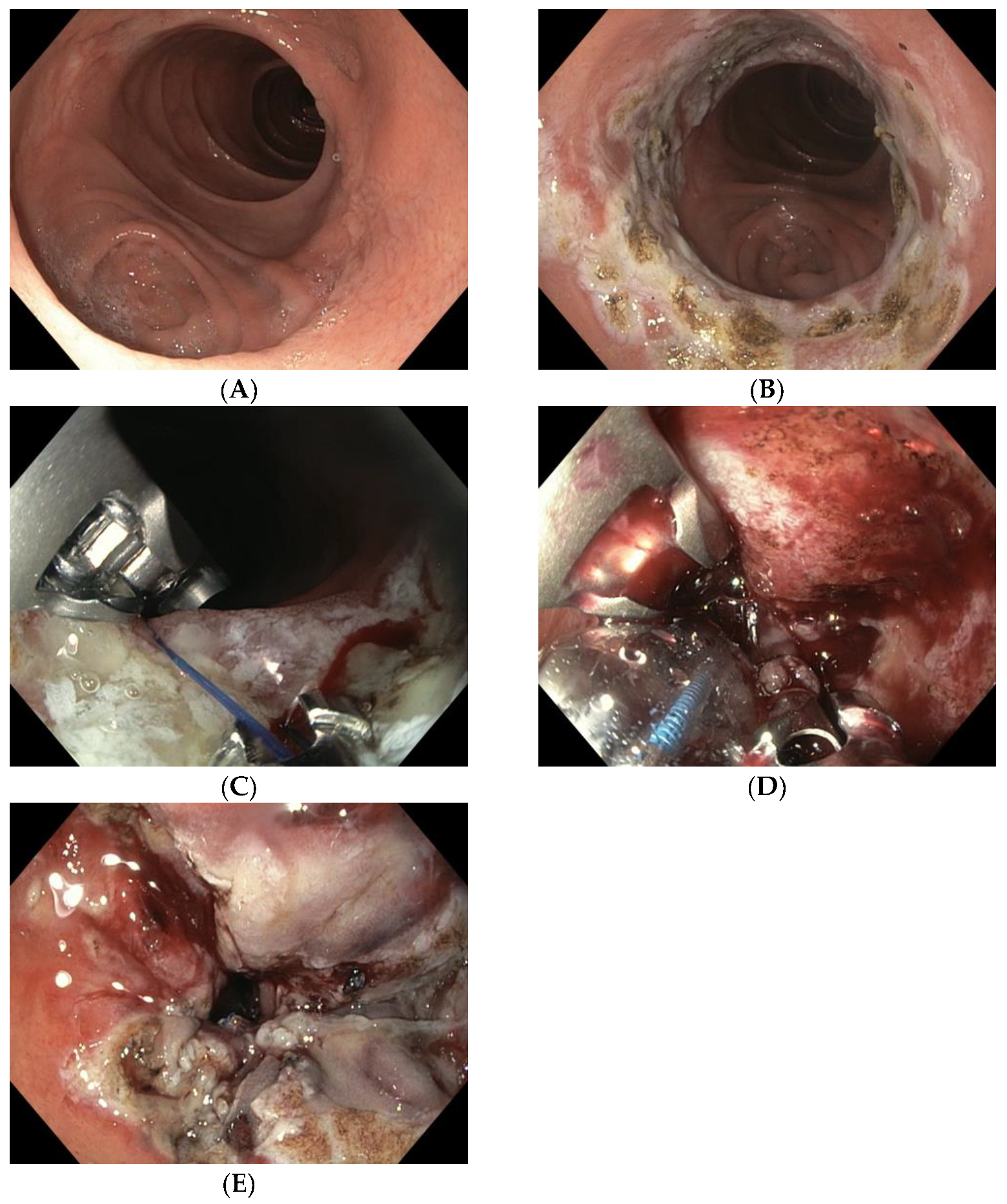
Figure 1. (A) Dilated GJA; (B) ablation of the gastric rim via APC; (C) suturing the anastomosis with the Apollo Overstitch system; (D) suture size control using an 8 mm CRE balloon; (E) narrowed GJA after TORe.
There are several other TORe techniques described in the literature [23][25][26][27][28]. Initially, some studies demonstrated efficacy using APC alone in the GJA, which was relatively simple to perform, and even feasible with patients under conscious sedation [29][30][31][32]. Jaruvongvanich et al. reported a meta-analysis showing that both full-thickness suturing plus APC (ft-TORe) and argon plasma mucosal coagulation alone (APMC-TORe) offer comparable weight loss outcomes and safety profiles, but the AMPC-TORe technique usually requires multiple endoscopic sessions [23].
Barola et al. performed a two-fold running suture TORe technique with a significant reduction in BMI (5.5 + 5.0%, p < 0.001 at mean follow-up of 113.2 ± 75.7 days (15.4%)); however, 15.4% of the patients developed a gastric stenosis that was treated with balloon dilation [27].
A new approach combining the restriction component of TORe followed by type 1 surgical distalization of the Roux limb may be another alternative for managing weight regain in high-BMI patients after RYGB; however, this could result in greater malabsorption, leading to greater deficiency syndrome [28].
More recently, researchers have seen the emergence of a novel, modified technique: first performing an endoscopic submucosal dissection (ESD) before applying endoscopic sutures. This is known as ESD-TORe [25][26]. A retrospective study compared patients who underwent modified ESD-TORe vs. APC -TORe. At 12 months, the ESD-TORe group experienced greater weight loss compared with the traditional TORe group (12.1% ± 9.3% vs. 7.5% ± 3.3% TBWL) [26]. However, this technique resulted in a higher rate of major complications (21.1% for ESD-TORe vs. 8.77% for APC-TORe) which, combined with the technical difficulty of ESD, limits its widespread adoption [22][26].
On the other hand, the TORe procedure has demonstrated a high degree of safety, with only minor intraprocedural adverse effects (AE) such as superficial lacerations of the esophageal mucosa due to the use of the overtube [2][7][8][18][19][20][21][33][34][35][36][37]. Additional postprocedural serious AEs include bleeding from marginal ulceration and GJA stenosis [9][10][11][14][19][20][21][22][28][29][30][34]. In general, AEs can be successfully managed endoscopically without the need for surgery.
References
- Cooper, T.C.; Simmons, E.B.; Webb, K.; Burns, J.L.; Kushner, R.F. Trends in Weight Regain Following Roux-en-Y Gastric Bypass (RYGB) Bariatric Surgery. Obes. Surg. 2015, 25, 1474–1481.
- Jirapinyo, P.; Kumar, N.; AlSamman, M.A.; Thompson, C.C. Five-year outcomes of transoral outlet reduction for the treatment of weight regain after Roux-en-Y gastric bypass. Gastrointest. Endosc. 2020, 91, 1067–1073.
- Ramadan, M.; Loureiro, M.; Laughlan, K.; Caiazzo, R.; Iannelli, A.; Brunaud, L.; Czernichow, S.; Nedelcu, M.; Nocca, D. Risk of Dumping Syndrome after Sleeve Gastrectomy and Roux-en-Y Gastric Bypass: Early Results of a Multicentre Prospective Study. Gastroenterol. Res. Pract. 2016, 2016, 2570237.
- Abu Dayyeh, B.K.; Lautz, D.B.; Thompson, C.C. Gastrojejunal Stoma Diameter Predicts Weight Regain after Roux-en-Y Gastric Bypass. Clin. Gastroenterol. Hepatol. 2011, 9, 228–233.
- Kumar, N.; Thompson, C.C. Transoral outlet reduction for weight regain after gastric bypass: Long-term follow-up. Gastrointest. Endosc. 2016, 83, 776–779.
- Mann, J.P.; Jakes, A.D.; Hayden, J.D.; Barth, J.H. Systematic Review of Definitions of Failure in Revisional Bariatric Surgery. Obes. Surg. 2015, 25, 571–574.
- Jirapinyo, P.; Slattery, J.; Ryan, M.B.; Abu Dayyeh, B.K.; Lautz, D.B.; Thompson, C.C. Evaluation of an endoscopic suturing device for transoral outlet reduction in patients with weight regain following Roux-en-Y gastric bypass. Endoscopy 2013, 45, 532–536.
- Vargas, E.J.; Bazerbachi, F.; Rizk, M.; Rustagi, T.; Acosta, A.; Wilson, E.B.; Wilson, T.; Neto, M.G.; Zundel, N.; Mundi, M.S.; et al. Transoral outlet reduction with full thickness endoscopic suturing for weight regain after gastric bypass: A large multicenter international experience and meta-analysis. Surg. Endosc. 2018, 32, 252–259.
- Van Beek, A.P.; Emous, M.; Laville, M.; Tack, J. Dumping syndrome after esophageal, gastric or bariatric surgery: Pathophysiology, diagnosis, and management. Obes. Rev. 2017, 18, 68–85.
- Scarpellini, E.; Arts, J.; Karamanolis, G.; Laurenius, A.; Siquini, W.; Suzuki, H.; Ukleja, A.; Van Beek, A.; Vanuytsel, T.; Bor, S.; et al. International consensus on the diagnosis and management of dumping syndrome. Nat. Rev. Endocrinol. 2020, 16, 448–466.
- Tack, J.; Arts, J.; Caenepeel, P.; De Wulf, D.; Bisschops, R. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat. Rev. Gastroenterol. Hepatol. 2009, 6, 583–590.
- Ukleja, A. Dumping Syndrome: Pathophysiology and Treatment. Nutr. Clin. Pract. 2005, 20, 517–525.
- Banerjee, A.; Ding, Y.; Mikami, D.J.; Needleman, B.J. The role of dumping syndrome in weight loss after gastric bypass surgery. Surg. Endosc. 2013, 27, 1573–1578.
- Moreira, R.O.; Moreira, R.B.M.; Machado, N.A.M.; Gonçalves, T.B.; Coutinho, W.F. Post-prandial Hypoglycemia after Bariatric Surgery: Pharmacological Treatment with Verapamil and Acarbose. Obes. Surg. 2008, 18, 1618–1621.
- Lakdawala, M.; Limas, P.; Dhar, S.; Remedios, C.; Dhulla, N.; Sood, A.; Bhasker, A.G. Laparoscopic revision of Roux-en-Y gastric bypass to sleeve gastrectomy: A ray of hope for failed Roux-en-Y gastric bypass. Asian J. Endosc. Surg. 2016, 9, 122–127.
- Campos, G.M.; Ziemelis, M.; Paparodis, R.; Ahmed, M.; Davis, D.B. Laparoscopic reversal of Roux-en-Y gastric bypass: Technique and utility for treatment of endocrine complications. Surg. Obes. Relat. Dis. 2014, 10, 36–43.
- Tran, D.D.; Nwokeabia, I.D.; Purnell, S.; Zafar, S.N.; Ortega, G.; Hughes, K.; Fullum, T.M. Revision of Roux-En-Y Gastric Bypass for Weight Regain: A Systematic Review of Techniques and Outcomes. Obes. Surg. 2016, 26, 1627–1634.
- Vargas, E.J.; Dayyeh, B.K.; Storm, A.C.; Bazerbachi, F.; Matar, R.; Vella, A.; Kellogg, T.; Stier, C. Endoscopic management of dumping syndrome after Roux-en-Y gastric bypass: A large international series and proposed management strategy. Gastrointest. Endosc. 2020, 92, 91–96.
- Brown, M.; Zaman, J.; Arellano, J.; Binetti, B.; Singh, T.P. Sa2011 Endoscopic Gastrojejunostomy Revision Following Roux-En-Y Gastric Bypass: Outcomes at 2-Year Follow-Up. Gastrointest. Endosc. 2017, 85, AB275.
- Dhindsa, B.S.; Saghir, S.M.; Naga, Y.; Dhaliwal, A.; Ramai, D.; Cross, C.; Singh, S.; Bhat, I.; Adler, D.G. Efficacy of transoral outlet reduction in Roux-en-Y gastric bypass patients to promote weight loss: A systematic review and meta-analysis. Endosc. Int. Open 2020, 8, E1332–E1340.
- Brunaldi, V.O.; Jirapinyo, P.; de Moura, D.T.H.; Okazaki, O.; Bernardo, W.M.; Neto, M.G.; Campos, J.M.; Santo, M.A.; de Moura, E.G.H. Endoscopic Treatment of Weight Regain Following Roux-en-Y Gastric Bypass: A Systematic Review and Meta-analysis. Obes. Surg. 2018, 28, 266–276.
- Wong, S.K.H. Endoscopic full-thickness transoral outlet reduction with endoscopic submucosal dissection or argon plasma coagulation: Does it make a difference? Endoscopy 2019, 51, 617–618.
- Jaruvongvanich, V.; Vantanasiri, K.; Laoveeravat, P.; Matar, R.H.; Vargas, E.J.; Maselli, D.B.; Alkhatry, M.; Fayad, L.; Kumbhari, V.; Fittipaldi-Fernandez, R.J.; et al. Endoscopic full-thickness suturing plus argon plasma mucosal coagulation versus argon plasma mucosal coagulation alone for weight regain after gastric bypass: A systematic review and meta-analysis. Gastrointest. Endosc. 2020, 92, 1164–1175.e6.
- Schulman, A.R.; Kumar, N.; Thompson, C.C. Transoral outlet reduction: A comparison of purse-string with interrupted stitch technique. Gastrointest. Endosc. 2018, 87, 1222–1228.
- Hollenbach, M.; Selig, L.; Lellwitz, S.; Beer, S.; Feisthammel, J.; Rosendahl, J.; Schaumburg, T.; Mössner, J.; Hoffmeister, A. Endoscopic full-thickness transoral outlet reduction with semicircumferential endoscopic submucosal dissection. Endoscopy 2019, 51, 684–688.
- Jirapinyo, P.; de Moura, D.T.; Thompson, C.C. Endoscopic submucosal dissection with suturing for the treatment of weight regain after gastric bypass: Outcomes and comparison with traditional transoral outlet reduction (with video). Gastrointest. Endosc. 2020, 91, 1282–1288.
- Barola, S.; Agnihotri, A.; Hill, C.; Dunlap, M.K.; Ngamruengphong, S.; Chen, Y.-I.; Singh, V.; Khashab, M.A.; Kumbhari, V. Sa2017 Transoral Outlet Reduction Post Roux-En-Y Gastric Bypass: Evaluation of a Treatment Algorithm Using Two-Fold Running Sutures. Gastrointest. Endosc. 2017, 85, AB278–AB279.
- Abu Dayyeh, B.; Portela, R.; Mahmoud, T.; Ghazi, R.; Ghanem, O.M. A novel approach for weight regain after Roux-en-Y gastric bypass: Staged transoral outlet reduction (TORe) followed by surgical type 1 distalization. VideoGIE 2022, 7, 135–137.
- Jirapinyo, P.; Moura, D.; Dong, W.Y.; Farias, G.; Thompson, C.C. Dose response for argon plasma coagulation in the treatment of weight regain after Roux-en-Y gastric bypass. Gastrointest. Endosc. 2020, 91, 1078–1084.
- Jirapinyo, P.; Kroner, P.T.; Thompson, C.C. Argon Plasma Coagulation is Effective in Roux-En-Y Gastric Bypass Patients that do not Achieve Weight Loss Goals after Sutured Transoral Outlet Reduction (TORe). Gastroenterology 2017, 152, S635.
- Baretta, G.A.P.; Alhinho, H.C.A.W.; Matias, J.E.F.; Marchesini, J.B.; de Lima, J.H.F.; Empinotti, C.; Campos, J.M. Argon Plasma Coagulation of Gastrojejunal Anastomosis for Weight Regain After Gastric Bypass. Obes. Surg. 2015, 25, 72–79.
- Moon, R.C.; Teixeira, A.F.; Neto, M.G.; Zundel, N.; Sander, B.Q.; Ramos, F.M.; Matz, F.; Baretta, G.A.; de Quadros, L.G.; Grecco, E.; et al. Efficacy of Utilizing Argon Plasma Coagulation for Weight Regain in Roux-en-Y Gastric Bypass Patients: A Multi-center Study. Obes. Surg. 2018, 28, 2737–2744.
- Callahan, Z.M.; Su, B.; Kuchta, K.; Linn, J.; Carbray, J.; Ujiki, M. Five-year results of endoscopic gastrojejunostomy revision (transoral outlet reduction) for weight gain after gastric bypass. Surg. Endosc. 2020, 34, 2164–2171.
- Petchers, A.; Walker, A.; Bertram, C.; Feustel, P.; Singh, T.P.; Zaman, J. Evaluation of endoscopic gastrojejunostomy revision after Roux-en-Y gastric bypass for treatment of dumping syndrome. Gastrointest. Endosc. 2022, 96, 639–644.
- Relly, R.; Mati, S.; Aviv, C.N.; Fishman, S. Endoscopic trans-oral outlet reduction after bariatric surgery is safe and effective for dumping syndrome. Surg. Endosc. 2021, 35, 6846–6852.
- Tsai, C.; Steffen, R.; Kessler, U.; Merki, H.; Zehetner, J. Endoscopic Gastrojejunal Revisions Following Gastric Bypass: Lessons Learned in More Than 100 Consecutive Patients. J. Gastrointest. Surg. 2019, 23, 58–66.
- Stier, C.; Chiappetta, S. Endoluminal Revision (OverStitch TM, Apollo Endosurgery) of the Dilated Gastroenterostomy in Patients with Late Dumping Syndrome after Proximal Roux-en-Y Gastric Bypass. Obes. Surg. 2016, 26, 1978–1984.
More
Information
Subjects:
Gastroenterology & Hepatology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
651
Revisions:
2 times
(View History)
Update Date:
15 Jun 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




