Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Marianna Trebuňová | -- | 1695 | 2023-06-09 08:01:03 | | | |
| 2 | Rita Xu | Meta information modification | 1695 | 2023-06-09 08:20:34 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Modrák, M.; Trebuňová, M.; Balogová, A.F.; Hudák, R.; Živčák, J. Biodegradable Materials for Tissue Engineering. Encyclopedia. Available online: https://encyclopedia.pub/entry/45375 (accessed on 11 March 2026).
Modrák M, Trebuňová M, Balogová AF, Hudák R, Živčák J. Biodegradable Materials for Tissue Engineering. Encyclopedia. Available at: https://encyclopedia.pub/entry/45375. Accessed March 11, 2026.
Modrák, Marcel, Marianna Trebuňová, Alena Findrik Balogová, Radovan Hudák, Jozef Živčák. "Biodegradable Materials for Tissue Engineering" Encyclopedia, https://encyclopedia.pub/entry/45375 (accessed March 11, 2026).
Modrák, M., Trebuňová, M., Balogová, A.F., Hudák, R., & Živčák, J. (2023, June 09). Biodegradable Materials for Tissue Engineering. In Encyclopedia. https://encyclopedia.pub/entry/45375
Modrák, Marcel, et al. "Biodegradable Materials for Tissue Engineering." Encyclopedia. Web. 09 June, 2023.
Copy Citation
The growing importance of regenerative medicine and tissue engineering (TE) reflects the fact that bone metabolic and related diseases represent approximately 50% of all chronic diseases for people above the age of fifty. In addition, mechanical damage of bone often occurs because of an accident, required surgery and so forth. Bone defects or bone injuries caused by aging, traffic accidents, fractures, or bone tumor resection are among the serious problems in orthopedics because they cause major damage to health and lower the quality of life.
biodegradability
scaffold
implant
1. Introduction
Internal fixation is required for reconstructive surgery on fractured bone to maintain the anatomic reduction in the fragments and provide stability during the healing process. In the past, bone fractures were fixed by the methods of applying metal implants. To substitute the metal implants for internal fracture fixation, numerous biodegradable materials (BMs) were developed. Biodegradable implants are increasingly used in regenerative medicine and sports medicine [1]. To be used successfully for fracture fixation, BMs must have sufficient strength and not degrade too rapidly. In an ideal scenario, these implants would break down as the wound healed, transferring load gradually to the healing tissue.
Today’s regenerative medicine and tissue engineering are using a large portfolio of BMs, which are used largely as substitutes for damaged or missing hard tissue. Natural and synthetic biodegradable polymers and hydrolysable metals make the main components for the creation of temporary medical implants [2]. Recently, much attention has been paid to materials based on extracellular matrix (ECM) [3][4], which consist of proteins, glycosaminoglycans and glycoproteins [5]. There is no doubt that the development and application research of BMs has significantly intensified in the last decade, as evidenced by the growing number of publications in this area.
2. Indications and Materials for Biodegradable Implants in Orthopedics
There are several typical clinical indications for the use of biodegradable implants in orthopedics, which are mostly used for fractures stabilization, osteotomy procedures, bone grafts and fusions [6][7]. Furthermore, they can be used in re-attachment of tendons, ligaments, meniscal cracks, and other tissue structures [8]. The most common indications for biodegradable implants in orthopedics include anterior cruciate ligament reconstruction, meniscus repair, and ankle fracture treatment [9]. The occurrence of clinical indications for biodegradable implants is comprehensively demonstrated in Figure 1.
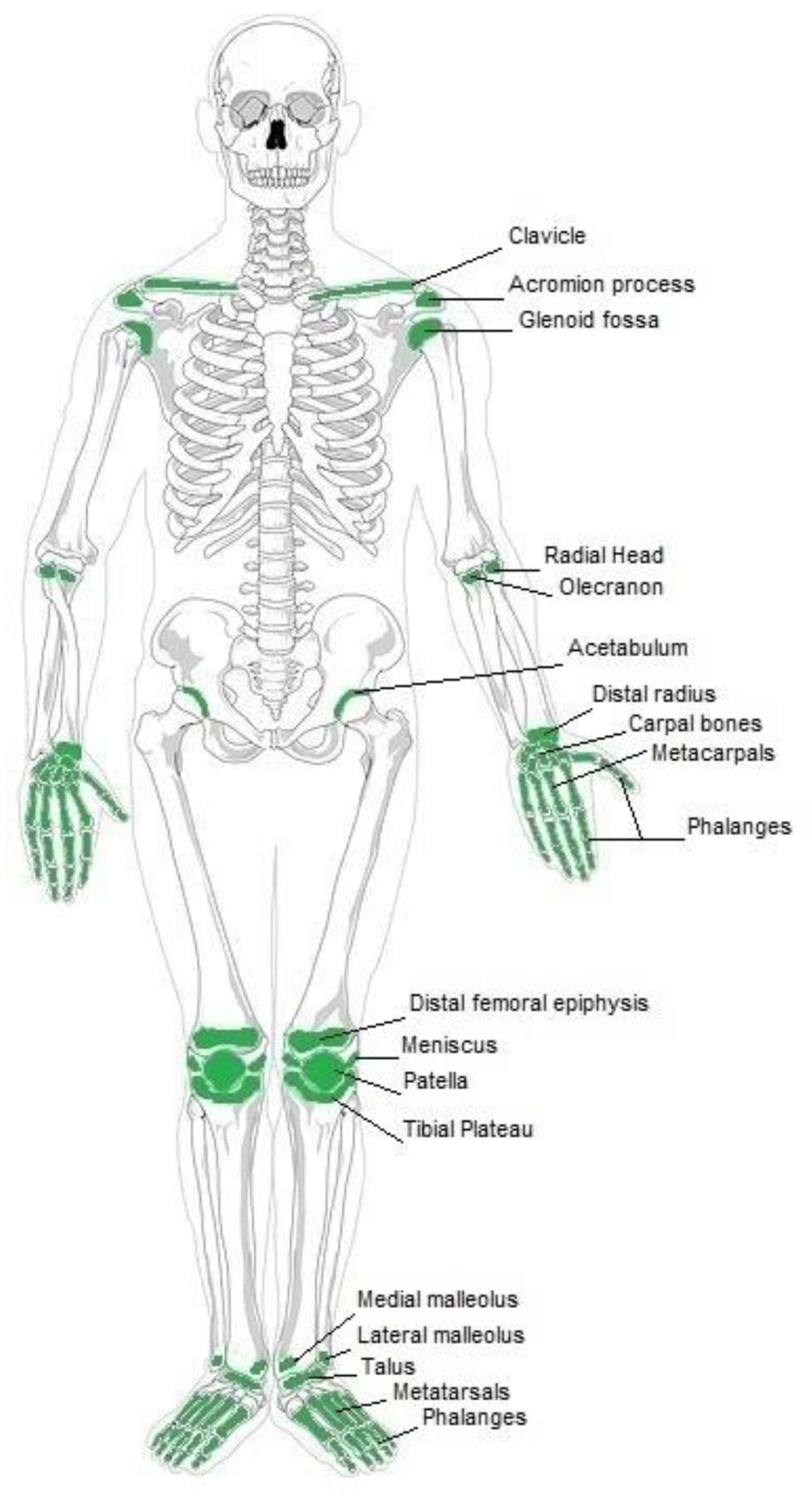
Figure 1. Current clinical applications of biodegradable implants.
As demonstrated in Figure 1, there are several clinical indications on the upper limb. In the shoulder area, biodegradable implants are applied in fracture fixation of the glenoid fossa and in shoulder lesions repair [10]. Other shoulder indications include reconstruction of various intra-articular and extra-articular abnormalities. Clinical indications for the arm include osteochondral fractures of head and epicondyles of the humerus [11]. Biodegradable implants are also used for fracture fixation of the radial head and radial neck [12][13][14]. Furthermore, these implants are used to treat fractures of metacarpals and phalanges, fixation of tendons and collateral ligaments, lunate and scaphoid fractures [15][16][17].
Further clinical indications include those which are related to the lower limb. In the knee region, anterior cruciate ligament reconstructions are treated with the use of biodegradable implants [10]. Biodegradable pins are appropriate for osteochondral fractures. In addition, meniscal tacks and biodegradable suture anchors allow for new ways to perform reconstruction after complicated knee injuries. Patella fractures can also be treated with these implants. The foot and ankle region also benefits from these innovative implants. Here implants made from BM are used for treatment of isolated fractures of the internal malleolus [18][19][20]. Further indications include fractures of metatarsals and phalanges, flake fracture of the talus and calcaneus [21][22][23]. In addition, Lisfranc’s dislocation, syndesmotic disruptions and osteotomies for hallux valgus are among the health conditions that can be treated with biodegradable implants.
Traditionally, non-degradable metals such as inert stainless steel, titanium and its alloys, and cobalt-chromium alloys were used for internal fixation of fractured bones and joints [24]. These materials used to lack bone ingrowth in the scaffold and cause that the scaffold did not respond to changes in bone topology [25]. However, this issue is solvable when scaffold surface has porous structure or coatings that promote bone cell attachment and growth. Biodegradable materials used in orthopedic applications include degradable synthetic polymers and degradable metals and alloys [2]. According to Hoffman [26] dozens of different polymeric BMs have been developed to substitute metal implants for internal fracture fixation, such as bone plates, screws, and intramedullary pins. He adds that their main limitation is the loss of mechanical strength within a short time interval. On the other hand, polymeric BMs have overcome metals in some important quality attributes, such as elasticity, flexibility, longevity, and bio-inertness [27]. Among them, polyglycolide (PGA), polylactide (PLA), and polycaprolactone (PCL) have been the most widely used for this purpose due to their good biocompatibility [28]. Polymers PLA, PGA and their co-polymer compositions are most often used in applications that include fracture-fixation pins and plates, interference screws, suture anchors and other fixation implants as they are highly resorbable [29]. Implants made from PLA are used, e.g., for the surgery and/or treatment of maxillofacial fractures, ankle fractures and syndesmosis injury [30][31]. The degradable polymer poly-l-d, l-lactide (PLDLA) is applicable for the treatment of mandibular fractures, since it has good mechanical properties. The screws made from this material provided the same fixation strength as titanium screws [32]. Another synthetic polymer Poly-l-lactic (PLLA) is notable for its gradual degradation and thanks to that is applicable in orthopedics for anterior cruciate ligament reconstruction, ankle fracture treatment or meniscus injury therapy [33][34]. Bio-absorbable screws made from copolymer PLLA/PGA are suitable, e.g., for fixation of osteochondritis dissecans lesions [35].
Biodegradable metals are seen as promising alternatives to non-biodegradable metals. Among the metals, magnesium (Mg), zinc (Zn), and iron (Fe) are considered as materials with the most biodegradable potential [36]. During the last decades, Mg-based alloys have been intensively explored by researchers in the context of orthopedic applications. The advantages of Mg-based biodegradable metals are that their bioactivity enhances osteogenesis and that their elastic modulus matches that of bone [37][38]. Magnesium’s good properties mean that it is often used to treat bone fractures, for example in the form of an implantable screw. Typically used magnesium alloys include high-purity magnesium alloy, MgCa0.8 alloy, MgYREZr alloy and Mg-Al-Zn alloys. For example, the MgYREZr screws were applied to treat hallux valgus with good therapeutic effect [39]. Currently, Zinc-based BMs are receiving considerable attention. A comprehensive review of related research progress on Zn-based BMs for orthopedic internal fixation is presented in a study by Liu et al. [40]. Its authors point out the important fact that there is a critical need for development of BMs for fixation of fractures at heavy load-bearing bone sites where fractures occur most frequently.
3. Smart Biodegradable Materials for Tissue Engineering
Traditionally, biodegradable materials were designed to interact with living tissue temporarily or permanently to provide functions, such as mechanical support. Smart BMs are defined as those that respond to external stimuli, such as light, magnetic fields, ultrasound, etc. Typical smart BMs include, e.g., photoresponsive and chemoresponsive polymers that combine sensing and actuation within the same material, without need for external devices [41][42][43]. Moreover, development of smart bioactive glasses for bone contact applications is becoming a hot research area in TE [44]. Recent research in this domain focuses on the molecular interaction of bioactive glass-based ionic dissolution products with their physiological surrounding environment [45]. Another example of smart biomaterial is decellularized extracellular matrix, which is the noncellular component of tissue that retains relevant biological cues for cells [46]. The related research is oriented towards directly using the component of the dECM to obtain scaffolds simulating native ECM [47].
Montoya et al. [48] suggested classifying smart biomaterials according to their degree of interaction with their external environment and the subsequent biological responses to clarify the concept of smartness in this context. The authors categorized smart materials into three kinds, namely, active, responsive, and autonomous. The inert biomaterial is just biocompatible or bioinert, while the active one can provide planned one-way interaction, e.g., bioactive therapy, with biological tissue. One of the first materials of this category was bioactive glass composed of four oxides, namely SiO2-CaO-Na2O-P2O5, introduced by Hench [49]. The main limitation of active biomaterials lies in the limited duration and efficacy of the therapy due to their degradation in a biological environment. Active biomaterials, namely polymer and lipid-based ones are often used for the controlled release of drugs like antibiotics, antiseptics, vitamins, and statins [50][51]. Responsive biomaterials can receive a stimulus and provide feedback to it through triggered reactions. Examples of such materials are artificial cells and hydrogels [52]. Especially, the need for biodegradable hydrogels in biomedical applications is significant since their physical properties can be designed to follow those of articular cartilage [53]. Recent developments in the design of responsive nanocomposite hydrogels increase their potential in biomedical applications including their utilization as therapeutic platforms for the delivery of precisely prescribed medications [54]. The responsive functionalities of biomaterials can be triggered from internal or external sources. The stimuli coming from inside an organism are internal, while external sources generate stimuli from outside of the body like heat, light, chemicals, or pressure. Both kinds of the signals can be categorized into three groups: biological, chemical, and physical [55]. For instance, PLLA-based biomaterials processed into piezoelectric structures can be engineered as scaffolds for promoting cellular growth during electrostimulation [56]. The low piezoelectric effect of PLLA is similar in magnitude to that of natural biomacromolecules like collagen [57] giving it the ability to interact with biological systems without being rejected [58]. The highest degree of smartness represents biomaterials capable of autonomously responding to the surrounding environment. Biomaterials with such properties can be considered as kind of dynamic biomaterials, which respond to stimuli by autonomous feedback loops [52]. The model of autonomous biomaterial is graphically illustrated in Figure 2.
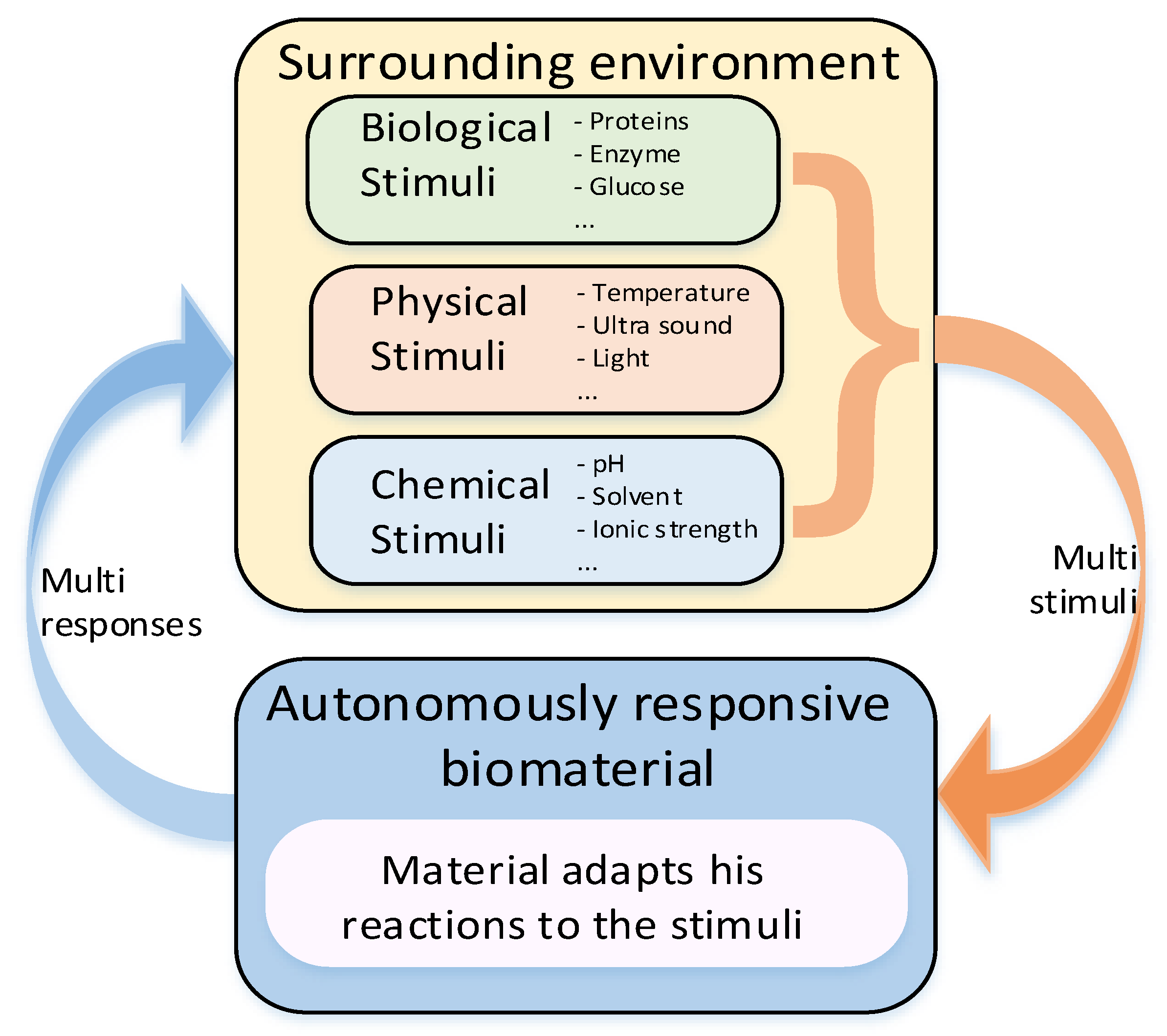
Figure 2. Model of stimuli-responsive biomaterial with closed loop.
Smart biomaterials can be applied, e.g., for the regulation of stem cell activity, as well as to understand complex cellular processes [59]. The control of dynamic biomaterials after implantation in the body becomes challenging research in this field. For this purpose, Badeau et al. [60] employed a logic-based peptide hydrogel as a miniature computer system taking inputs from the surrounding microenvironment to decide when to release therapeutic agents for drug delivery. Research devoted to smart biomaterials in biomedical engineering is widely published, and its development is comprehensively summarized in recent works [61][62][63].
References
- Kroczek, K.; Turek, P.; Mazur, D.; Szczygielski, J.; Filip, D.; Brodowski, R.; Balawender, K.; Przeszłowski, Ł.; Lewandowski, B.; Orkisz, S.; et al. Characterisation of selected materials in medical applications. Polymers 2022, 14, 1526.
- Li, C.; Guo, C.; Fitzpatrick, V.; Ibrahim, A.; Zwierstra, M.J.; Hanna, P.; Lechtig, A.; Nazarian, A.; Lin, S.J.; Kaplan, D.L. Design of biodegradable, implantable devices towards clinical translation. Nat. Rev. Mater. 2020, 5, 61–81.
- Kim, Y.; Ko, H.; Kwon, I.K.; Shin, K. Extracellular matrix revisited: Roles in tissue engineering. Int. Neurourol. J. 2016, 20, 23–29.
- Yao, Q.; Zheng, Y.W.; Lan, Q.H.; Kou, L.; Xu, H.L.; Zhao, Y.Z. Recent development and biomedical applications of decellularized extracellular matrix biomaterials. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 104, 109942.
- Theocharis, A.D.; Skandalis, S.S.; Gialeli, C.; Karamanos, N.K. Extracellular matrix structure. Adv. Drug Deliv. Rev. 2016, 97, 4–27.
- Pisecky, L.; Luger, M.; Klasan, A.; Gotterbarm, T.; Klotz, M.C.; Hochgatterer, R. Bioabsorbable implants in forefoot surgery: A review of materials, possibilities and disadvantages. EFORT Open Rev. 2021, 6, 1132–1139.
- Santic, V.; Tudor, A.; Sestan, B.; Legovic, D.; Sirola, L.; Rakovac, I. Bone allograft provides bone healing in the medial opening high tibial osteotomy. Int. Orthop. 2010, 34, 225–229.
- Vadodaria, K.; Kulkarni, A.; Santhini, E.; Vasudevan, P. Materials and structures used in meniscus repair and regeneration: A review. Biomedicine 2019, 9, 2.
- Li, J.W.; Du, C.F.; Yuchi, C.X.; Zhang, C.Q. Application of biodegradable materials in orthopedics. J. Med. Biol. Eng. 2019, 39, 633–645.
- Vatchha, S.P.; Kohli, A.; Tripathi, S.K.; Nanda, S.N.; Pradhan, P.; Shiraz, S.M. Biodegradable Implants in Orthopaedics. Ann. Int. Med. Dent. Res. 2015, 1, 3–8.
- Claes, L.; Burri, C.; Kiefer, H.; Rübenacker, S. The refixation of osteochondral and bony fragments with various resorbable implants. In Proceedings of the 8th European Conference on Biomaterials (ESB), Heidelberg, Germany, 7–9 September 1989.
- Chen, H.; Wu, D.; Pan, T.; Pan, J.; Zhang, R.; Shi, X. Comparison of three different fixation constructs for radial neck fractures: A biomechanical study. J. Orthop. Surg. Res. 2017, 12, 175.
- Jahn, R.; Diederichs, D.; Friedrich, B. Resorbable implants and their use exemplified by fracture of the head of the radius. Aktuelle Traumatol. 1989, 19, 281–286.
- Adm, F.F.; Mohammedin, A.; Mostafa, K.; Mohamed, M.A. Open Reduction and Internal Fixation of Radial-Head Fractures Mason Type II. Egypt. J. Hosp. Med. 2022, 89, 8058–8064.
- Tarallo, L.; Mugnai, R.; Rocchi, M.; Capra, F.; Catani, F. Comparison between absorbable pins and mini-screw fixations for the treatment of radial head fractures Mason type II-III. BMC Musculoskelet. Disord. 2018, 19, 94.
- Simón, F.P.; Medrano, B.G.; Serrano, P.J.D. Diagnostic and Therapeutic Approach to Acute Scaphoid Fractures. Rev. Iberoam. Cirugía De La Mano 2020, 48, 109–118.
- Vihtonen, K. Preliminary results of reinsertion of ruptured ulnar collateral ligament of the first metacarpophalangeal joint with totally biodegradable polylactide (PLLA) pin. Acta Orthop. Scand 1990, 61, 44.
- Bostman, O.; Vainionpaa, S.; Hirvensalo, E.; Makela, A.; Vihtonen, K.; Tormala, P.; Rokkanen, P. Biodegradable internal fixation for malleolar fractures: A prospective randomised trial. J. Bone Jt. Surg. 1987, 69, 615–619.
- Böstman, O.; Hirensalo, E.; Vainionpää, S.; Mäkelä, A.; Vihtonen, K.; Törmälä, P.; Rokkanen, P. Ankle fractures treated using biodegradable internal fixation. Clin. Orthop. Relat. Res. 1989, 238, 195–203.
- Böstman, O.; Hirvensalo, E.; Vainionpää, S.; Vihtonen, K.; Törmälä, P.; Rokkanen, P. Degradable polyglycolide rods for the internal fixation of displaced bimalleolar fractures. Int. Orthop. 1990, 14, 1–8.
- Hirvensalo, E.; Böstman, O.; Rokkanen, P. Absorbable polyglycolide pins in fixation of displaced fractures of the radial head. Arch. Orthop. Trauma Surg. 1990, 109, 258–261.
- Hofmann, G.O. Biodegradable implants in traumatology: A review on the state-of-the-art. Arch. Orthop. Trauma Surg. 1995, 114, 123–132.
- Hoffmann, R.; Weiler, A.; Helling, H.J.; Krettek, C.; Rehm, K.E. Local foreign-body reactions to biodegradable implants A classification system: A classification system. Der. Unf. 1997, 100, 658–666.
- Manam, N.S.; Harun, W.S.W.; Shri, D.N.A.; Ghani, S.A.C.; Kurniawan, T.; Ismail, M.H.; Ibrahim, M.H.I. Study of corrosion in biocompatible metals for implants: A review. J. Alloys Compd. 2017, 701, 698–715.
- Saini, M.; Singh, Y.; Arora, P.; Arora, V.; Jain, K. Implant biomaterials: A comprehensive review. World J. Clin. Cases WJCC 2015, 3, 52–57.
- Hofmann, G.O. Biodegradable implants in orthopaedic surgery—A review on the state-of-the-art. Clin. Mater. 1992, 10, 75–80.
- Teo, A.J.; Mishra, A.; Park, I.; Kim, Y.-J.; Park, W.-T.; Yoon, Y.-J. Polymeric biomaterials for medical implants and devices. ACS Biomater. Sci. Eng. 2016, 2, 454–472.
- Adeosun, S.O.; Lawal, G.I.; Gbenebor, O.P. Characteristics of biodegradable implants. J. Miner. Mater. Charact. Eng. 2014, 2, 88–106.
- De Jong, W.H.; Bersgma, J.E.; Robinson, J.E.; Bos, R.R. Tissue response to partially in vitro predegraded poly(L-lactide) implants. Biomaterials 2005, 26, 1781–1791.
- Lee, H.B.; Oh, J.S.; Kim, S.G.; Kim, H.K.; Moon, S.Y.; Kim, Y.K.; Yun, P.Y.; Son, J.S. Comparison of titanium and biodegradable miniplates for fixation of mandibular fractures. J. Oral Maxillofac. Surg. 2010, 68, 2065–2069.
- Findrik Balogová, A.; Trebuňová, M.; Ižaríková, G.; Kaščák, Ľ.; Mitrík, L.; Klímová, J.; Feranc, J.; Modrák, M.; Hudák, R.; Živčák, J. In vitro degradation of specimens produced from PLA/PHB by additive manufacturing in simulated conditions. Polymers 2021, 13, 1542.
- Yerit, K.C.; Hainich, S.; Enislidis, G.; Turhani, D.; Klug, C.; Wittwer, G.; Öckher, M.; Undt, G.; Kermer, C.; Watzinger, F.; et al. Biodegradable fixation of mandibular fractures in children: Stability and early results. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2005, 100, 17–24.
- Ramos, D.M.; Dhandapani, R.; Subramanian, A.; Sethuraman, S.; Kumbar, S.G. Clinical complications of biodegradable screws for ligament injuries. Mater. Sci. Eng. 2020, 109, 110423.
- Lee, D.W.; Lee, J.W.; Kim, S.B.; Park, J.H.; Chung, K.S.; Ha, J.K.; Kim, J.G.; Kim, W.J. Comparison of poly-L-lactic acid and poly-L-lactic acid/hydroxyapatite bioabsorbable screws for tibial fixation in ACL reconstruction: Clinical and magnetic resonance imaging results. Clin. Orthop. Surg. 2017, 9, 270–279.
- Larsen, M.W.; Pietrzak, W.S.; DeLee, J.C. Fixation of osteochondritis dissecans lesions using poly (l-lactic acid)/poly (glycolic acid) copolymer bioabsorbable screws. Am. J. Sport. Med. 2005, 33, 68–76.
- Cheng, J.; Liu, B.; Wu, Y.H.; Zheng, Y.F. Comparative in vitro study on pure metals (Fe, Mn, Mg, Zn and W) as biodegradable metals. J. Mater. Sci. Technol. 2013, 29, 619–627.
- Lee, J.W.; Han, H.S.; Han, K.J.; Park, J.; Jeon, H.; Ok, M.R.; Seok, H.K.; Ahn, J.P.; Lee, K.E.; Lee, D.H.; et al. Long-term clinical study and multiscale analysis of in vivo biodegradation mechanism of Mg alloy. Proc. Natl Acad. Sci. USA 2016, 113, 716–721.
- Zhang, Y.; Xu, J.; Ruan, Y.C.; Yu, M.K.; O’Laughlin, M.; Wise, H.; Chen, D.; Tian, L.; Shi, D.; Wang, J.; et al. Implant-derived magnesium induces local neuronal production of CGRP to improve bone-fracture healing in rats. Nat. Med. 2016, 22, 1160–1169.
- Brown, A.; Zaky, S.; Ray, H., Jr.; Sfeir, C. Porous magnesium/PLGA composite scaffolds for enhanced bone regeneration following tooth extraction. Acta Biomater. 2015, 11, 543–553.
- Liu, Y.; Du, T.; Qiao, A.; Mu, Y.; Yang, H. Zinc-Based Biodegradable Materials for Orthopaedic Internal Fixation. J. Funct. Biomater. 2022, 13, 164.
- Siskind, R.D.; Smith, R.C. Model development for shape memory polymers. In Proceedings of the Behavior and Mechanics of Multifunctional and Composite Materials, San Diego, CA, USA, 2 April 2008; pp. 313–322.
- Schneider, H.J. (Ed.) Chemoresponsive Materials: Smart Materials for Chemical and Biological Stimulation; Royal Society of Chemistry: London, UK, 2022; pp. 47–95.
- Du, W.; Liu, X.; Liu, L.; Lam, J.W.; Tang, B.Z. Photoresponsive polymers with aggregation-induced emission. ACS Appl. Polym. Mater. 2021, 3, 2290–2309.
- Cazzola, M.; Vernè, E.; Cochis, A.; Sorrentino, R.; Azzimonti, B.; Prenesti, E.; Rimondini, L.; Ferraris, S. Bioactive glasses functionalized with polyphenols: In vitro interactions with healthy and cancerous osteoblast cells. J. Mater. Sci. 2017, 52, 9211–9223.
- Deshmukh, K.; Kovářík, T.; Křenek, T.; Docheva, D.; Stich, T.; Pola, J. Recent advances and future perspectives of sol–gel derived porous bioactive glasses: A review. RSC Adv. 2020, 10, 33782–33835.
- Politi, S.; Carotenuto, F.; Rinaldi, A.; Di Nardo, P.; Manzari, V.; Albertini, M.C.; Araneo, R.; Ramakrishna, S.; Teodori, L. Smart ECM-based electrospun biomaterials for skeletal muscle regeneration. Nanomaterials 2020, 10, 1781.
- Heath, D.E. A review of decellularized extracellular matrix biomaterials for regenerative engineering applications. Regen. Eng. Transl. Med. 2019, 5, 155–166.
- Montoya, C.; Du, Y.; Gianforcaro, A.L.; Orrego, S.; Yang, M.; Lelkes, P.I. On the road to smart biomaterials for bone research: Definitions, concepts, advances, and outlook. Bone Res. 2021, 9, 12.
- Hench, L.L. Bioceramics: From concept to clinic. J. Am. Ceram. Soc. 1991, 74, 1487–1510.
- Fenton, O.S.; Olafson, K.N.; Pillai, P.S.; Mitchell, M.J.; Langer, R. Advances in biomaterials for drug delivery. Adv. Mater. 2018, 30, 1705328.
- Villalba-Rodriguez, A.M.; Parra-Saldivar, R.; Ahmed, I.; Karthik, K.; Malik, Y.S.; Dhama, K.; Iqbal, H. Bio-inspired biomaterials and their drug delivery perspectives—A review. Curr. Drug Metab. 2017, 18, 893–904.
- Morris, E.; Chavez, M.; Tan, C. Dynamic biomaterials: Toward engineering autonomous feedback. Curr. Opin. Biotechnol. 2016, 39, 97–104.
- Tan, H.; Marra, K.G. Injectable, biodegradable hydrogels for tissue engineering applications. Materials 2010, 3, 1746–1767.
- Lavrador, P.; Esteves, M.R.; Gaspar, V.M.; Mano, J.F. Stimuli-responsive nanocomposite hydrogels for biomedical applications. Adv. Funct. Mater. 2021, 31, 2005941.
- Pérez-Mitta, G.; Albesa, A.G.; Trautmann, C.; Toimil-Molares, M.E.; Azzaroni, O. Bioinspired integrated nanosystems based on solid-state nanopores: “Iontronic” transduction of biological, chemical and physical stimuli. Chem. Sci. 2017, 8, 890–913.
- Gazvoda, L.; Višić, B.; Spreitzer, M.; Vukomanović, M. Hydrophilicity Affecting the Enzyme-Driven Degradation of Piezoelectric Poly-l-Lactide Films. Polymers 2021, 13, 1719.
- Minary-Jolandan, M.; Yu, M.F. Nanoscale characterization of isolated individual type I collagen fibrils: Polarization and piezoelectricity. Nanotechnology 2009, 20, 85706.
- Murillo, G.; Blanquer, A.; Vargas-estevez, C.; Barrios, L.; Ibáñez, E.; Nogués, C.; Esteve, J. Electromechanical Nanogenerator-Cell Interaction Modulates Cell Activity. Adv. Mater. 2017, 29, 1605048.
- Khan, F.; Tanaka, M. Designing smart biomaterials for tissue engineering. Int. J. Mol. Sci. 2017, 19, 17.
- Badeau, B.A.; Comerford, M.P.; Arakawa, C.K.; Shadish, J.A.; DeForest, C.A. Engineered modular biomaterial logic gates for environmentally triggered therapeutic delivery. Nat. Chem. 2018, 10, 251–258.
- Amukarimi, S.; Ramakrishna, S.; Mozafari, M. Smart biomaterials—A proposed definition and overview of the field. Curr. Opin. Biomed. Eng. 2021, 19, 100311.
- Safavi, M.S.; Bordbar-Khiabani, A.; Walsh, F.C.; Mozafari, M.; Khalil-Allafi, J. Surface modified NiTi smart biomaterials: Surface engineering and biological compatibility. Curr. Opin. Biomed. Eng. 2023, 25, 100429.
- Zaszczyńska, A.; Gradys, A.; Sajkiewicz, P. Progress in the applications of smart piezoelectric materials for medical devices. Polymers 2020, 12, 2754.
More
Information
Subjects:
Engineering, Biomedical
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.0K
Revisions:
2 times
(View History)
Update Date:
09 Jun 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





