Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Nermin Morgan | -- | 1961 | 2023-05-25 23:52:16 | | | |
| 2 | Rita Xu | -1 word(s) | 1960 | 2023-05-26 04:09:05 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Morgan, N.; Meeus, J.; Shujaat, S.; Cortellini, S.; Bornstein, M.M.; Jacobs, R. CBCT for Sinus Floor Elevation Procedures. Encyclopedia. Available online: https://encyclopedia.pub/entry/44865 (accessed on 01 March 2026).
Morgan N, Meeus J, Shujaat S, Cortellini S, Bornstein MM, Jacobs R. CBCT for Sinus Floor Elevation Procedures. Encyclopedia. Available at: https://encyclopedia.pub/entry/44865. Accessed March 01, 2026.
Morgan, Nermin, Jan Meeus, Sohaib Shujaat, Simone Cortellini, Michael M. Bornstein, Reinhilde Jacobs. "CBCT for Sinus Floor Elevation Procedures" Encyclopedia, https://encyclopedia.pub/entry/44865 (accessed March 01, 2026).
Morgan, N., Meeus, J., Shujaat, S., Cortellini, S., Bornstein, M.M., & Jacobs, R. (2023, May 25). CBCT for Sinus Floor Elevation Procedures. In Encyclopedia. https://encyclopedia.pub/entry/44865
Morgan, Nermin, et al. "CBCT for Sinus Floor Elevation Procedures." Encyclopedia. Web. 25 May, 2023.
Copy Citation
Sinus floor elevation (SFE) is a standard surgical technique used to compensate for alveolar bone resorption in the posterior maxilla. Such a surgical procedure requires radiographic imaging pre- and postoperatively for diagnosis, treatment planning, and outcome assessment. Cone beam computed tomography (CBCT) has become a well-established imaging modality in the dentomaxillofacial region. The research is aimed to provide clinicians with an overview of the role of three-dimensional (3D) CBCT imaging for diagnostics, treatment planning, and postoperative monitoring of SFE procedures.
CBCT
maxillary sinus
sinus floor elevation
1. Introduction
Alveolar bone atrophy in the maxillary posterior region is inevitable following tooth extraction, resulting in horizontal and vertical ridge resorption [1][2]. If a dental implant is inserted in bone having inadequate volume, there is a high risk of compromised implant stability and poor prognosis [3][4]. In order to compensate for reduced bone height and volume of the maxillary posterior region, sinus floor elevation (SFE) is performed for bone reconstruction. It involves lifting up of the Schneiderian membrane, which is usually followed by the placement of a bone graft [5][6][7][8][9].
The two main techniques for SFE are either a direct approach using a lateral window or indirect with the transalveolar technique. In the lateral window approach, an osteotomy is performed in the buccal wall of the maxilla, creating access through the lateral bone wall of the sinus cavity [10][11][12]. The transalveolar technique is a less invasive technique that was modified by Summers [13], where a transcrestal osteotome is applied to elevate the sinus floor, pushing bone substitutes beyond the level of the original sinus floor [14]. This technique has been recommended in areas with sufficient alveolar crest width and where a residual vertical bone height of ≥5 mm is available [15]. In cases where the alveolar bone height is less than 5 mm, the lateral window approach is recommended [16].
To date, various graft materials have been successfully used for SFE solely or in combination with each other [17], such as autograft [18][19][20][21] (intraoral: chin, retromolar region, mandibular ramus, maxillary tuberosity [22][23]; extraoral: iliac crest, fibula, tibia [24][25][26]), allograft [27][28][29] (fresh, frozen, freeze-dried bone [30][31]), xenograft [32][33][34][35][36] (deproteinized bovine bone [37][38][39]), and phytogenic material [39][40][41] (Gusuibu, coral-based bone substitutes, and marine algae).
Along with patient history and clinical examination, radiographic examination is an essential component of preliminary diagnostics, treatment planning, and outcome assessment in patients requiring SFE. Previously, two-dimensional (2D) panoramic radiography acted as a clinical standard. However, it suffers from certain inherent limitations, which can negatively impact the task at hand, such as magnification, distortion, and superimposition [16][42].
Three-dimensional (3D) preoperative imaging of the specific site of augmentation becomes a prerequisite in order to provide needed information about the morphologic characteristics and/or pathological conditions of the sinus and residual ridge [43][44][45]. Some studies have used computed tomography (CT) for the planning of sinus grafting [46] and precalculated the augmented bone volume needed [47][48][49][50]. However, the use of CT imaging is limited for most dental practitioners due to the high costs, large size of the device, and high radiation dose. To overcome these general limitations, 3D imaging in the form of cone beam CT (CBCT) has become a standard [43][44] for patients requiring maxillary sinus procedures. Recently, various CBCT imaging systems with low-dose protocols have also been made commercially available, which are not only affordable and compact to be used in a private dental practice but also provide 3D imaging with a lower radiation dose exposure to the patient [51][52].
2. Digital Workflow for SFE Procedures
In recent years, digital technologies and workflows have been introduced in the majority of dental medicine fields, including restorative dentistry, orthodontics, dental implantology, and maxillofacial reconstructive surgery [53]. Digital treatment planning workflow refers to the incorporation of computer-controlled components and dental technologies for assisting a clinician with the planning process. This digitization of workflows in clinical dentistry has overcome the limitations associated with traditional methods by offering improved precision of dental procedures, time-efficiency, and a higher standard of patient care [54][55][56].
2.1. Virtual Modelling
Generally, CBCT images are saved in a Digital Imaging and Communications in Medicine (DICOM) format, which is then transferred to 3D software programs for further processing to plan the procedure. The most essential step in SFE planning workflows is segmentation, a process by which the region of interest is extracted from 3D images for generating 3D virtual models. These models are then used for fabricating guides or pre-surgically assessing the amount of required (bone) graft (Figure 1).
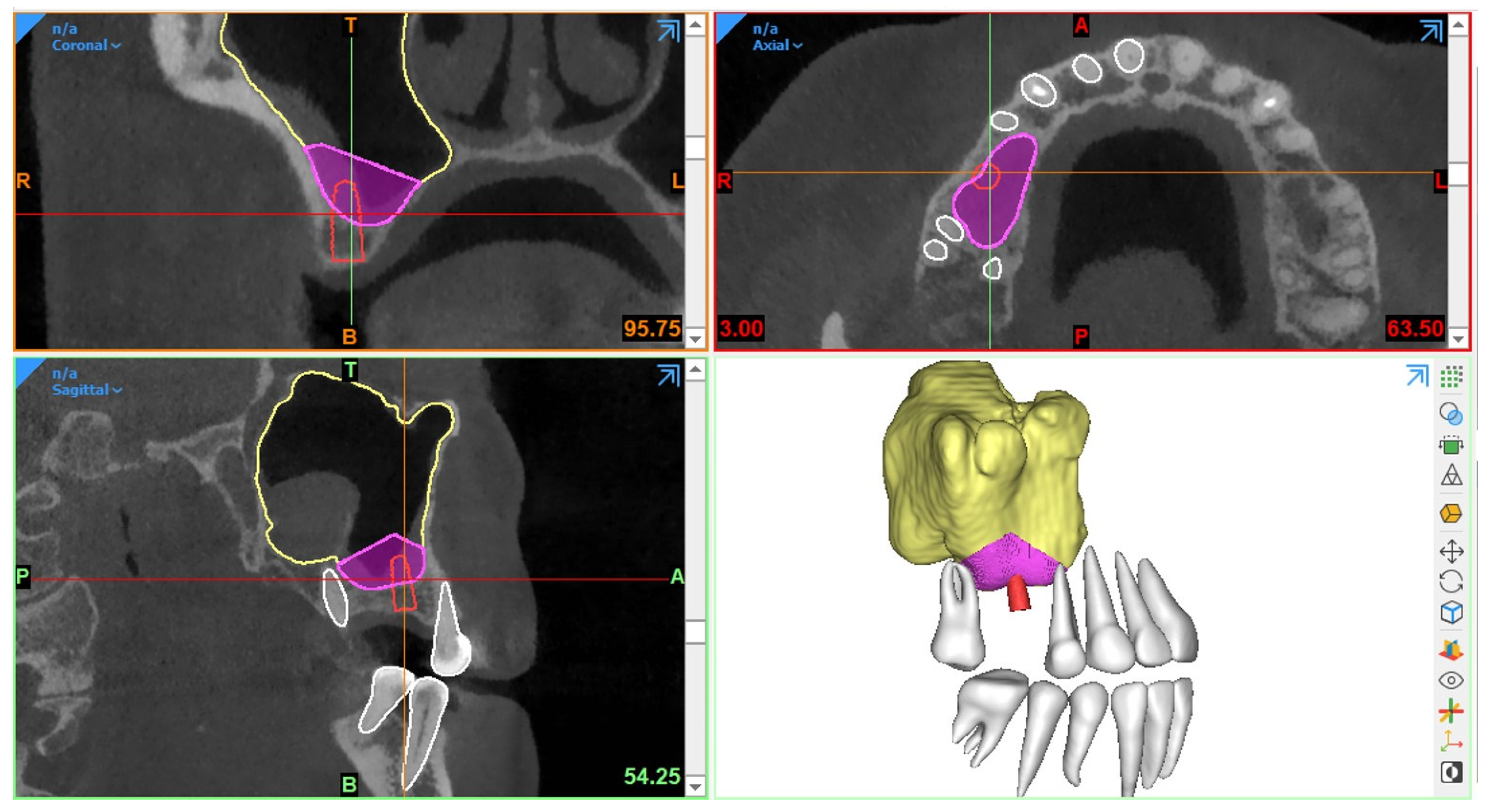
Figure 1. Example of graft volume estimation in Mimics (version 23.0, Materialise N.V., Leuven, Belgium) following automated sinus and teeth segmentation.
Traditionally, manual sinus segmentation, referred to as slice-by-slice delineation on 2D CBCT planes, performed by an expert is considered the gold standard. However, it is prone to certain limitations, such as labor-intensiveness, increased time consumption, and observer variability [57][58]. Based on the aforementioned limitations, semi-automated segmentation via thresholding-based approaches has been widely adopted for the segmentation of CBCT images to improve the efficiency of planning workflows [59][60]. Nevertheless, the final segmentation lacks optimal delineation due to the presence of different structural densities, and manual post-processing is often required. Recently, artificial intelligence (AI) in the form of deep learning has been employed for automated segmentation to overcome the limitations associated with both manual and semi-automated segmentation approaches. In deep learning, convolutional neural networks (CNNs) have demonstrated excellent performance with the employment of multi-layer neural computational connections for sinus segmentation on CBCT images [61][62][63]. The application of such deep learning-based approaches might enhance the quality and predictability of presurgical graft planning, enable a more precise treatment planning process and volumetric quantification of sinus/graft changes, and may further improve the standard of care. Yet, a lack of evidence exists related to the application of AI in the SFE treatment planning workflows.
2.2. Surgical Guidance
In SFE procedures, CBCT-based guidance has played a vital role in improving the precision of the surgical procedure with a reduction in complications. The guidance can be static or dynamic in nature. The procedures performed via these guides are referred to as “guided sinus lift [64]” or “guided bone grafting [65]”.
2.2.1. Static Surgical Guides
Static guides are designed via 3D planning software programs following the integration of intraoral scanned images with CBCT datasets and later fabricated using 3D printers. Such surgical templates act as a support aid and offer the advantages of time-efficiency, better working ergonomics, less operator stress, and greater predictability of the procedure [64][66][67]. Moreover, this procedure can also be combined with concurrent implant placement planning.
In 2008, Manderales and Rosenfeld [65] pioneered computer-guided SFE. They proposed using CAD/CAM surgical cutting guides for exact lateral wall outlining to considerably improve the quality and outcomes of the SFE procedure. Cecchetti et al. [64] have recently introduced virtual planning of surgical guides for lateral wall sinus elevation, concluding that the surgical template should be seen as a support aid to minimize risk and complications of the surgical procedures, especially in “difficult” cases.
Following the same concept, Osman et al. [68] and Strbac et al. [67] performed computer-guided SFE through a lateral window approach in addition to simultaneous implant placement. They found that applying static guides resulted in better and more consistent results. Similarly, Pistilli et al. [66] also concluded that such a digital approach is highly efficient in the mid-term (follow-up of 10 years) to implant rehabilitation of severely resorbed maxilla simultaneously with sinus lift.
Considering transrectal sinus augmentation, Pozzi et al. [69] and An et al. [70] combined static guide-based flapless maxillary crestal sinus augmentation with an immediate nonfunctional loading of dental implants, reporting a 98.53% and 100% survival rate at 3 years and 37 months, respectively.
Another type of surgical guidance is dynamic navigation, which is based on computer-guided surgery planning. Here, a physical surgical guide is unnecessary [71].
2.2.2. Dynamic Surgical Guides
A dynamic navigation system combined with CBCT imaging has been proposed for improving the intraoperative precision of implant placement, where a static surgical guide is not required and the operator can place the implants with real-time navigation [72]. With regard to SFE, limited evidence exists related to the application of navigation-based approaches. Recently, dynamic navigation has been used for posterior maxilla implant surgery via transcrestal SFE using piezoelectric devices [73]. The proposed technique offered high precision with excellent clinical outcome. However, it is recommended to perform further clinical studies to assess the effectiveness of dynamic navigation for performing SFE.
Considering the intraoperative use of CBCT imaging, Blake et al. [74] performed one case trial of using a C-arm-based CBCT scanner during sinus augmentation surgery under general anesthesia with iliac crest grafting. The images were taken prior to wound closure to immediately verify the surgery result. However, there is no solid evidence regarding such procedures for surgeries performed under local anesthesia.
3. Use of CBCT for Monitoring and Follow-Up after SFE
Post-surgical radiographic examination is vital [19][49][75][76][77][78][79][80][81][82][83][84][85][86][87] for the evaluation of bony integration of the inserted graft, follow-up of its long term stability, and also assessment of implant success and/or osteointegration after sinus lift procedures.
Ideally, imaging guidelines for the follow-up of sinus augmentation with or without immediate implant placement should follow the same regulations as those for post-surgical implant placement. Based on the AAOMR recommendations [88] and the guidelines for the use of diagnostic imaging in implant dentistry published by the E.A.O. [89], intraoral periapical radiography should be performed for the postoperative assessment of implants in the absence of clinical signs or symptoms. Panoramic radiographs may be indicated for more extensive implant therapy cases.
Meanwhile, CBCT [75][78][81] has become the standard imaging technique for 3D visualization and improved assessment prior to implant placement in the case of staged sinus augmentation. CBCT imaging can help to assess bone healing by visualizing how the material has integrated with the surrounding bone as well as if any signs of early resorption exist. It is beneficial in providing information about the volume, extent, and density of the augmented region [89] and can also be used to monitor any complications, which are not visible to the naked eye, such as mucosal changes, infection, and/or inflammation.
Furthermore, bone graft materials undergo remodeling over time at varying rates depending on the material used (resorbable versus non-resorbable) [90], and positive pressure formed inside the sinus during respiration also accelerates graft resorption [91]. Certainly, this remodeling could have a significant impact on the success of SFE outcome and the respective implant treatment. Thereby, CBCT can aid in the quantification of the resorption rate of different grafting materials [92][93][94] and also to monitor sinus changes at follow-up stages by comparing pre-surgical and/or post-surgical scans acquired at different time points. Usually, the Schneiderian membrane exhibits significant post-surgical edema, which increases the mucosal thickness visible. In addition, the edema might cause ostium obstruction with the possibility of impaired drainage capacity of sinus mucus. The reduction in the patency and obstruction of the ostium and infundibulum can lead to an inflammatory reaction and/or infectious processes of the sinus cavity, causing acute or chronic sinusitis [95]. Hence, CBCT imaging could act as a useful follow-up assessment tool to measure the thickness of the membrane and monitor mucosal changes in an attempt to avoid both early and delayed postoperative complications [96]. Additionally, following up the mucosal thickness changes could help to study the possible effects of different graft materials on sinus mucosa for research purposes [97].
It should be kept in mind that the use of CBCT should not be opted for regular follow-up assessment of normal SFE procedures without any evident or suspected complications to avoid exposure to unnecessary radiation doses. Postoperative CBCT could be indicated in cases with complications and contraindicated in patients where no direct benefit is to be expected. In instances of no clinical signs or symptoms of treatment failure or complications, periapical or panoramic images could be considered more than enough for postoperative follow-up. Moreover, CBCT imaging should also be justifiable for ethically approved clinical research projects, which might improve the standard of patient care. However, optimized strategies still need to be developed for SFE follow-up assessment, allowing good image quality and accurate 3D modeling with low-dose scanning protocols.
References
- Chen, S.T.; Darby, I. Alveolar ridge preservation and early implant placement at maxillary central incisor sites: A prospective case series study. Clin. Oral Implant. Res. 2020, 31, 803–813.
- Hansson, S.; Halldin, A. Alveolar ridge resorption after tooth extraction: A consequence of a fundamental principle of bone physiology. J. Dent. Biomech. 2012, 3, 1758736012456543.
- Farmer, M.; Darby, I. Ridge dimensional changes following single-tooth extraction in the aesthetic zone. Clin. Oral Implant. Res. 2014, 25, 272–277.
- Jemt, T.; Lekholm, U. Implant treatment in edentulous maxillae: A 5-year follow-up report on patients with different degrees of jaw resorption. Int. J. Oral Maxillofac. Implant. 1995, 10, 303–311.
- Bathla, S.C.; Fry, R.R.; Majumdar, K. Maxillary sinus augmentation. J. Indian Soc. Periodontol. 2018, 22, 468–473.
- Bornstein, M.M.; Chappuis, V.; Von Arx, T.; Buser, D. Performance of dental implants after staged sinus floor elevation procedures: 5-year results of a prospective study in partially edentulous patients. Clin. Oral Implant. Res. 2008, 19, 1034–1043.
- Del Fabbro, M.; Wallace, S.S.; Testori, T. Long-term implant survival in the grafted maxillary sinus: A systematic review. Int. J. Periodontics Restor. Dent. 2013, 33, 773–783.
- Esposito, M.; Felice, P.; Worthington, H.V. Interventions for replacing missing teeth: Augmentation procedures of the maxillary sinus. Cochrane Database Syst. Rev. 2014, Cd008397.
- Starch-Jensen, T.; Jensen, J.D. Maxillary Sinus Floor Augmentation: A Review of Selected Treatment Modalities. J. Oral Maxillofac. Res. 2017, 8, e3.
- Boyne, P.J.; James, R.A. Grafting of the maxillary sinus floor with autogenous marrow and bone. J. Oral Surg. 1980, 38, 613–616.
- Caudry, S.; Landzberg, M. Lateral window sinus elevation technique: Managing challenges and complications. J. Can. Dent. Assoc. 2013, 79, d101.
- Tatum, H., Jr. Maxillary and sinus implant reconstructions. Dent. Clin. N. Am. 1986, 30, 207–229.
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome technique. Compendium 1994, 15, 152, 154-6, 158 passim, quiz 162.
- Temmerman, A.; Van Dessel, J.; Cortellini, S.; Jacobs, R.; Teughels, W.; Quirynen, M. Volumetric changes of grafted volumes and the Schneiderian membrane after transcrestal and lateral sinus floor elevation procedures: A clinical, pilot study. J. Clin. Periodontol. 2017, 44, 660–671.
- Wang, H.L.; Katranji, A. ABC sinus augmentation classification. Int. J. Periodontics Restor. Dent. 2008, 28, 383–389.
- Mohan, N.; Wolf, J.; Dym, H. Maxillary sinus augmentation. Dent. Clin. N. Am. 2015, 59, 375–388.
- Zhao, R.; Yang, R.; Cooper, P.R.; Khurshid, Z.; Shavandi, A.; Ratnayake, J. Bone Grafts and Substitutes in Dentistry: A Review of Current Trends and Developments. Molecules 2021, 26, 3007.
- Johansson, L.A.; Isaksson, S.; Lindh, C.; Becktor, J.P.; Sennerby, L. Maxillary sinus floor augmentation and simultaneous implant placement using locally harvested autogenous bone chips and bone debris: A prospective clinical study. J. Oral Maxillofac. Surg. 2010, 68, 837–844.
- Klijn, R.J.; Meijer, G.J.; Bronkhorst, E.M.; Jansen, J.A. A meta-analysis of histomorphometric results and graft healing time of various biomaterials compared to autologous bone used as sinus floor augmentation material in humans. Tissue Eng. Part B Rev. 2010, 16, 493–507.
- Nkenke, E.; Stelzle, F. Clinical outcomes of sinus floor augmentation for implant placement using autogenous bone or bone substitutes: A systematic review. Clin. Oral Implant. Res. 2009, 20 (Suppl. S4), 124–133.
- Schmitt, C.M.; Doering, H.; Schmidt, T.; Lutz, R.; Neukam, F.W.; Schlegel, K.A. Histological results after maxillary sinus augmentation with Straumann® BoneCeramic, Bio-Oss®, Puros®, and autologous bone. A randomized controlled clinical trial. Clin. Oral Implant. Res. 2013, 24, 576–585.
- Maiorana, C.; Ferrario, S.; Poli, P.P.; Manfredini, M. Autogenous Chin Block Grafts in the Aesthetic Zone: A 20-Year Follow-Up Case Report. Case Rep. Dent. 2020, 2020, 6525797.
- Reininger, D.; Cobo-Vázquez, C.; Rosenberg, B.; López-Quiles, J. Alternative intraoral donor sites to the chin and mandibular body-ramus. J. Clin. Exp. Dent. 2017, 9, e1474–e1481.
- Sakkas, A.; Wilde, F.; Heufelder, M.; Winter, K.; Schramm, A. Autogenous bone grafts in oral implantology—Is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures. Int. J. Implant. Dent. 2017, 3, 23.
- Titsinides, S.; Agrogiannis, G.; Karatzas, T. Bone grafting materials in dentoalveolar reconstruction: A comprehensive review. Jpn. Dent. Sci. Rev. 2019, 55, 26–32.
- Wortmann, D.E.; Klein-Nulend, J.; van Ruijven, L.J.; Schortinghuis, J.; Vissink, A.; Raghoebar, G.M. Incorporation of anterior iliac crest or calvarial bone grafts in reconstructed atrophied maxillae: A randomized clinical trial with histomorphometric and micro-CT analyses. Clin. Implant. Dent. Relat. Res. 2021, 23, 492–502.
- Annibali, S.; Cristalli, M.P.; La Monaca, G.; Bignozzi, I.; Scarano, A.; Corrado, R.; Muzio, L.L. Human maxillary sinuses augmented with mineralized, solvent-dehydrated bone allograft: A longitudinal case series. Implant. Dent. 2011, 20, 445–454.
- Bavetta, G. The use of human allogenic graft (HBA) for maxillary bone regeneration: Review of literature and case reports. Curr. Pharm. Des. 2012, 18, 5559–5568.
- Irinakis, T. Efficacy of injectable demineralized bone matrix as graft material during sinus elevation surgery with simultaneous implant placement in the posterior maxilla: Clinical evaluation of 49 sinuses. J. Oral Maxillofac. Surg. 2011, 69, 134–141.
- Chaushu, L.; Silva, E.R.; Balan, V.F.; Chaushu, G.; Xavier, S.P. Sinus augmentation-autograft vs. fresh frozen allograft: Bone density dynamics and implant stability. J. Stomatol. Oral Maxillofac. Surg. 2021, 122, 467–471.
- Roberts, T.T.; Rosenbaum, A.J. Bone grafts, bone substitutes and orthobiologics. Organogenesis 2012, 8, 114–124.
- Özkan, Y.; Akoğlu, B.; Kulak-Özkan, Y. Maxillary sinus floor augmentation using bovine bone grafts with simultaneous implant placement: A 5-year prospective follow-up study. Implant. Dent. 2011, 20, 455–459.
- Scarano, A.; Piattelli, A.; Perrotti, V.; Manzon, L.; Iezzi, G. Maxillary sinus augmentation in humans using cortical porcine bone: A histological and histomorphometrical evaluation after 4 and 6 months. Clin. Implant. Dent. Relat. Res. 2011, 13, 13–18.
- Sivolella, S.; Bressan, E.; Gnocco, E.; Berengo, M.; Favero, G.A. Maxillary sinus augmentation with bovine bone and simultaneous dental implant placement in conditions of severe alveolar atrophy: A retrospective analysis of a consecutively treated case series. Quintessence Int. 2011, 42, 851–862.
- Temmerman, A.; Cortellini, S.; Van Dessel, J.; De Greef, A.; Jacobs, R.; Dhondt, R.; Teughels, W.; Quirynen, M. Bovine-derived xenograft in combination with autogenous bone chips versus xenograft alone for the augmentation of bony dehiscences around oral implants: A randomized, controlled, split-mouth clinical trial. J. Clin. Periodontol. 2020, 47, 110–119.
- Testori, T.; Iezzi, G.; Manzon, L.; Fratto, G.; Piattelli, A.; Weinstein, R.L. High temperature-treated bovine porous hydroxyapatite in sinus augmentation procedures: A case report. Int. J. Periodontics Restor. Dent. 2012, 32, 295–301.
- Kuchler, U.; Dos Santos, G.M.; Heimel, P.; Stähli, A.; Strauss, F.J.; Tangl, S.; Gruber, R. DBBM shows no signs of resorption under inflammatory conditions. An experimental study in the mouse calvaria. Clin. Oral Implant. Res. 2020, 31, 10–17.
- Kuchler, U.; Heimel, P.; Stähli, A.; Strauss, F.J.; Luza, B.; Gruber, R. Impact of DBBM Fragments on the Porosity of the Calvarial Bone: A Pilot Study on Mice. Materials 2020, 13, 4748.
- Sheikh, Z.; Hamdan, N.; Abdallah, M.-N.; Glogauer, M.; Grynpas, M. Natural and synthetic bone replacement graft materials for dental and maxillofacial applications. In Advanced Dental Biomaterials; Khurshid, Z., Najeeb, S., Zafar, M.S., Sefat, F., Eds.; Woodhead Publishing: Sawston, UK, 2019; pp. 347–376.
- Kolk, A.; Handschel, J.; Drescher, W.; Rothamel, D.; Kloss, F.; Blessmann, M.; Heiland, M.; Wolff, K.-D.; Smeets, R. Current trends and future perspectives of bone substitute materials–from space holders to innovative biomaterials. J. Cranio-Maxillofac. Surg. 2012, 40, 706–718.
- Wang, W.; Yeung, K.W.K. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact. Mater. 2017, 2, 224–247.
- Temmerman, A.; Hertelé, S.; Teughels, W.; Dekeyser, C.; Jacobs, R.; Quirynen, M. Are panoramic images reliable in planning sinus augmentation procedures? Clin. Oral Implant. Res. 2011, 22, 189–194.
- Bornstein, M.M.; Horner, K.; Jacobs, R. Use of cone beam computed tomography in implant dentistry: Current concepts, indications and limitations for clinical practice and research. Periodontology 2000 2017, 73, 51–72.
- Bornstein, M.M.; Scarfe, W.C.; Vaughn, V.M.; Jacobs, R. Cone beam computed tomography in implant dentistry: A systematic review focusing on guidelines, indications, and radiation dose risks. Int. J. Oral Maxillofac. Implant. 2014, 29, 55–77.
- Jacobs, R.; Salmon, B.; Codari, M.; Hassan, B.; Bornstein, M.M. Cone beam computed tomography in implant dentistry: Recommendations for clinical use. BMC Oral Health 2018, 18, 88.
- Reddy, M.S.; Mayfield-Donahoo, T.; Vanderven, F.J.; Jeffcoat, M.K. A comparison of the diagnostic advantages of panoramic radiography and computed tomography scanning for placement of root form dental implants. Clin. Oral Implant. Res. 1994, 5, 229–238.
- Arias-Irimia, Ó.; Barona Dorado, C.; Gómez Moreno, G.; Brinkmann, J.C.; Martínez-González, J.M. Pre-operative measurement of the volume of bone graft in sinus lifts using CompuDent. Clin. Oral Implant. Res. 2012, 23, 1070–1074.
- Buyukkurt, M.C.; Tozoglu, S.; Yavuz, M.S.; Aras, M.H. Simulation of sinus floor augmentation with symphysis bone graft using three-dimensional computerized tomography. Int. J. Oral Maxillofac. Surg. 2010, 39, 788–792.
- Krennmair, G.; Krainhöfner, M.; Maier, H.; Weinländer, M.; Piehslinger, E. Computerized tomography-assisted calculation of sinus augmentation volume. Int. J. Oral Maxillofac. Implant. 2006, 21, 907–913.
- Uchida, Y.; Goto, M.; Katsuki, T.; Soejima, Y. Measurement of maxillary sinus volume using computerized tomographic images. Int. J. Oral Maxillofac. Implant. 1998, 13, 811–818.
- Scarfe, W.C.; Farman, A.G. What is cone-beam CT and how does it work? Dent. Clin. N. Am. 2008, 52, 707–730.
- Scarfe, W.C.; Farman, A.G.; Sukovic, P. Clinical applications of cone-beam computed tomography in dental practice. J. Can. Dent. Assoc. 2006, 72, 75–80.
- Vandenberghe, B. The digital patient–Imaging science in dentistry. J. Dent. 2018, 74 (Suppl. S1), S21–S26.
- Lin, Y.-M. Digitalisation in Dentistry: Development and Practices. In The Digitization of Business in China: Exploring the Transformation from Manufacturing to a Digital Service Hub; Kim, Y.-C., Chen, P.-C., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 199–217.
- Shujaat, S.; Bornstein, M.M.; Price, J.B.; Jacobs, R. Integration of imaging modalities in digital dental workflows-possibilities, limitations, and potential future developments. Dentomaxillofacial Radiol. 2021, 50, 20210268.
- Shujaat, S.; Riaz, M.; Jacobs, R. Synergy between artificial intelligence and precision medicine for computer-assisted oral and maxillofacial surgical planning. Clin. Oral Investig. 2023, 27, 897–906.
- Heye, T.; Merkle, E.M.; Reiner, C.S.; Davenport, M.S.; Horvath, J.J.; Feuerlein, S.; Breault, S.R.; Gall, P.; Bashir, M.R.; Dale, B.M.; et al. Reproducibility of dynamic contrast-enhanced MR imaging. Part II. Comparison of intra- and interobserver variability with manual region of interest placement versus semiautomatic lesion segmentation and histogram analysis. Radiology 2013, 266, 812–821.
- Parmar, C.; Velazquez, E.R.; Leijenaar, R.; Jermoumi, M.; Carvalho, S.; Mak, R.H.; Mitra, S.; Shankar, B.U.; Kikinis, R.; Haibe-Kains, B.; et al. Robust Radiomics feature quantification using semiautomatic volumetric segmentation. PLoS ONE 2014, 9, e102107.
- Renard, F.; Guedria, S.; De Palma, N.; Vuillerme, N. Variability and reproducibility in deep learning for medical image segmentation. Sci. Rep. 2020, 10, 13724.
- Withey, D.; Koles, Z. Medical Image Segmentation: Methods and Software. In Proceedings of the 2007 Joint Meeting of the 6th International Symposium on Noninvasive Functional Source Imaging of the Brain and Heart and the International Conference on Functional Biomedical Imaging, Hangzhou, China, 12–14 October 2007; pp. 140–143.
- Choi, H.; Jeon, K.J.; Kim, Y.H.; Ha, E.-G.; Lee, C.; Han, S.-S. Deep learning-based fully automatic segmentation of the maxillary sinus on cone-beam computed tomographic images. Sci. Rep. 2022, 12, 14009.
- Hung, K.F.; Ai, Q.Y.H.; King, A.D.; Bornstein, M.M.; Wong, L.M.; Leung, Y.Y. Automatic detection and segmentation of morphological changes of the maxillary sinus mucosa on cone-beam computed tomography images using a three-dimensional convolutional neural network. Clin. Oral Investig. 2022, 26, 3987–3998.
- Jung, S.-K.; Lim, H.-K.; Lee, S.; Cho, Y.; Song, I.-S. Deep Active Learning for Automatic Segmentation of Maxillary Sinus Lesions Using a Convolutional Neural Network. Diagnostics 2021, 11, 688.
- Cecchetti, F.; Spuntarelli, M.; Mazza, D.; Di Girolamo, M.; Baggi, L. Guided sinus lift: Virtual planning of surgical templates for lateral access. J. Biol. Regul. Homeost. Agents 2021, 35, 139–145.
- Mandelaris, G.A.; Rosenfeld, A.L. A novel approach to the antral sinus bone graft technique: The use of a prototype cutting guide for precise outlining of the lateral wall. A case report. Int. J. Periodontics Restor. Dent. 2008, 28, 569–575.
- Pistilli, R.; Canullo, L.; Pesce, P.; Pistilli, V.; Caponio, V.C.A.; Sbricoli, L. Guided implant surgery and sinus lift in severely resorbed maxillae: A retrospective clinical study with up to 10 years of follow-up. J. Dent. 2022, 121, 104137.
- Strbac, G.D.; Giannis, K.; Schnappauf, A.; Bertl, K.; Stavropoulos, A.; Ulm, C. Guided Lateral Sinus Lift Procedure Using 3-Dimensionally Printed Templates for a Safe Surgical Approach: A Proof-of-Concept Case Report. J. Oral Maxillofac. Surg. 2020, 78, 1529–1537.
- Osman, A.H.; Mansour, H.; Atef, M.; Hakam, M. Computer guided sinus floor elevation through lateral window approach with simultaneous implant placement. Clin. Implant. Dent. Relat. Res. 2017, 20, 137–143.
- Pozzi, A.; Moy, P.K. Minimally Invasive Transcrestal Guided Sinus Lift (TGSL): A Clinical Prospective Proof-of-Concept Cohort Study up to 52 Months. Clin. Implant. Dent. Relat. Res. 2013, 16, 582–593.
- An, X.; Lee, C.; Fang, Y.; Choi, B. Immediate nonfunctional loading of implants placed simultaneously using computer-guided flapless maxillary crestal sinus augmentation with bone morphogenetic protein-2/collagen matrix. Clin. Implant. Dent. Relat. Res. 2019, 21, 1054–1061.
- Mauer, R.G.; Shadrav, A.; Dashti, M. Static Surgical Guides and Dynamic Navigation in Implant Surgery. In Navigation in Oral and Maxillofacial Surgery: Applications, Advances, and Limitations; Parhiz, S.A., James, J.N., Ghasemi, S., Amirzade-Iranaq, M.H., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 135–150.
- Block, M.S.; Emery, R.W.; Cullum, D.R.; Sheikh, A. Implant Placement Is More Accurate Using Dynamic Navigation. J. Oral Maxillofac. Surg. 2017, 75, 1377–1386.
- Wu, B.-Z.; Ma, F.-F.; Sun, F. Analysis of the accuracy of a dynamic navigation system when performing dental implant surgery with transcrestal sinus floor elevation: A pilot study. J. Dent. Sci. 2023.
- Blake, F.; Blessmann, M.; Pohlenz, P.; Heiland, M. A new imaging modality for intraoperative evaluation of sinus floor augmentation. Int. J. Oral Maxillofac. Surg. 2008, 37, 183–185.
- Dellavia, C.; Speroni, S.; Pellegrini, G.; Gatto, A.; Maiorana, C. A New Method to Evaluate Volumetric Changes in Sinus Augmentation Procedure. Clin. Implant. Dent. Relat. Res. 2013, 16, 684–690.
- Diserens, V.; Mericske, E.; Mericske-Stern, R. Radiographic Analysis of the Transcrestal Sinus Floor Elevation: Short-Term Observations. Clin. Implant. Dent. Relat. Res. 2005, 7, 70–78.
- Gray, C.F.; Redpath, T.W.; Bainton, R.; Smith, F.W. Magnetic resonance imaging assessment of a sinus lift operation using reoxidised cellulose (SurgicelR) as graft material. Clin. Oral Implant. Res. 2001, 12, 526–530.
- Hallman, M.; Hedin, M.; Sennerby, L.; Lundgren, S. A prospective 1-year clinical and radiographic study of implants placed after maxillary sinus floor augmentation with bovine hydroxyapatite and autogenous bone. J. Oral Maxillofac. Surg. 2002, 60, 277–284.
- Johansson, B.; Grepe, A.; Wannfors, K.; Aberg, P.; Hirsch, J.M. Volumetry of simulated bone grafts in the edentulous maxilla by computed tomography: An experimental study. Dentomaxillofacial Radiol. 2001, 30, 153–156.
- Kirmeier, R.; Arnetzl, C.; Robl, T.; Payer, M.; Lorenzoni, M.; Jakse, N. Reproducibility of volumetric measurements on maxillary sinuses. Int. J. Oral Maxillofac. Surg. 2011, 40, 195–199.
- Klijn, R.J.; Meijer, G.J.; Bronkhorst, E.M.; Jansen, J.A. Sinus Floor Augmentation Surgery Using Autologous Bone Grafts from Various Donor Sites: A Meta-Analysis of the Total Bone Volume. Tissue Eng. Part B Rev. 2010, 16, 295–303.
- Ozyuvaci, H.; Bilgiç, B.; Firatli, E. Radiologic and Histomorphometric Evaluation of Maxillary Sinus Grafting with Alloplastic Graft Materials. J. Periodontol. 2003, 74, 909–915.
- Reinert, S.; König, S.; Bremerich, A.; Eufinger, H.; Krimmel, M. Stability of bone grafting and placement of implants in the severely atrophic maxilla. Br. J. Oral Maxillofac. Surg. 2003, 41, 249–255.
- Riachi, F.; Naaman, N.; Tabarani, C.; Aboelsaad, N.; Aboushelib, M.N.; Berberi, A.; Salameh, Z. Influence of Material Properties on Rate of Resorption of Two Bone Graft Materials after Sinus Lift Using Radiographic Assessment. Int. J. Dent. 2012, 2012, 737262.
- Szabó, G.; Huys, L.; Coulthard, P.; Maiorana, C.; Garagiola, U.; Barabás, J.; Németh, Z.; Hrabák, K.; Suba, Z. A prospective multicenter randomized clinical trial of autogenous bone versus beta-tricalcium phosphate graft alone for bilateral sinus elevation: Histologic and histomorphometric evaluation. Int. J. Oral Maxillofac. Implant. 2005, 20, 371–381.
- Wanschitz, F.; Figl, M.; Wagner, A.; Rolf, E. Measurement of volume changes after sinus floor augmentation with a phycogenic hydroxyapatite. Int. J. Oral Maxillofac. Implant. 2006, 21, 433–438.
- Zijderveld, S.A.; Schulten, E.A.J.M.; Aartman, I.H.A.; ten Bruggenkate, C.M. Long-term changes in graft height after maxillary sinus floor elevation with different grafting materials: Radiographic evaluation with a minimum follow-up of 4.5 years. Clin. Oral Implant. Res. 2009, 20, 691–700.
- Tyndall, D.A.; Price, J.B.; Tetradis, S.; Ganz, S.D.; Hildebolt, C.; Scarfe, W.C. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, 817–826.
- Harris, D.; Horner, K.; Gröndahl, K.; Jacobs, R.; Helmrot, E.; Benic, G.I.; Bornstein, M.M.; Dawood, A.; Quirynen, M.E.A.O. guidelines for the use of diagnostic imaging in implant dentistry 2011. A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin. Oral Implant. Res. 2012, 23, 1243–1253.
- Hatano, N.; Shimizu, Y.; Ooya, K. A clinical long-term radiographic evaluation of graft height changes after maxillary sinus floor augmentation with a 2: 1 autogenous bone/xenograft mixture and simultaneous placement of dental implants. Clin. Oral Implant. Res. 2004, 15, 339–345.
- Hürzeler, M.B.; Kirsch, A.; Ackermann, K.L.; Quiñones, C.R. Reconstruction of the severely resorbed maxilla with dental implants in the augmented maxillary sinus: A 5-year clinical investigation. Int. J. Oral Maxillofac. Implant. 1996, 11, 466–475.
- Galindo-Moreno, P.; Hernández-Cortés, P.; Mesa, F.; Carranza, N.; Juodžbalys, G.; Aguilar, M.; Dds, P.G.; Hernández-Cortés, P. Slow Resorption of Anorganic Bovine Bone by Osteoclasts in Maxillary Sinus Augmentation. Clin. Implant. Dent. Relat. Res. 2012, 15, 858–866.
- Kirmeier, R.; Payer, M.; Wehrschuetz, M.; Jakse, N.; Platzer, S.; Lorenzoni, M. Evaluation of three-dimensional changes after sinus floor augmentation with different grafting materials. Clin. Oral Implant. Res. 2008, 19, 366–372.
- Mazzocco, F.; Lops, D.; Gobbato, L.; Lolato, A.; Romeo, E.; Del Fabbro, M. Three-Dimensional Volume Change of Grafted Bone in the Maxillary Sinus. Int. J. Oral Maxillofac. Implant. 2014, 29, 178–184.
- Molina, A.; Sanz-Sánchez, I.; Sanz-Martín, I.; Ortiz-Vigón, A.; Sanz, M. Complications in sinus lifting procedures: Classification and management. Periodontology 2000 2022, 88, 103–115.
- Zhou, C.; Sun, S.-Z.; Lin, M.-N.; He, F.-M. Responses of Sinus Membrane and Antral Pseudocyst Following Lateral Window Sinus Augmentation with Bone Grafting: A Retrospective Study. Int. J. Oral Maxillofac. Implant. 2021, 36, 885–893.
- Jiang, X.; He, S.; Bornstein, M.M.; Wu, Y.; Ye, L.; Wang, F. Effects of different grafting materials on volumetric changes in the Schneiderian membrane following lateral maxillary sinus floor elevation: A preliminary study. BMC Oral Health 2023, 23, 102.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.4K
Revisions:
2 times
(View History)
Update Date:
26 May 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





