Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Antonio Scarano | -- | 1552 | 2023-05-24 10:31:07 | | | |
| 2 | Lindsay Dong | Meta information modification | 1552 | 2023-05-25 02:37:42 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Scarano, A.; Khater, A.G.A.; Gehrke, S.A.; Serra, P.; Francesco, I.; Di Carmine, M.; Tari, S.R.; Leo, L.; Lorusso, F. Peri-Implant Diseases. Encyclopedia. Available online: https://encyclopedia.pub/entry/44757 (accessed on 07 February 2026).
Scarano A, Khater AGA, Gehrke SA, Serra P, Francesco I, Di Carmine M, et al. Peri-Implant Diseases. Encyclopedia. Available at: https://encyclopedia.pub/entry/44757. Accessed February 07, 2026.
Scarano, Antonio, Ahmad G. A. Khater, Sergio Alexandre Gehrke, Paola Serra, Inchingolo Francesco, Mariastella Di Carmine, Sergio Rexhep Tari, Lucia Leo, Felice Lorusso. "Peri-Implant Diseases" Encyclopedia, https://encyclopedia.pub/entry/44757 (accessed February 07, 2026).
Scarano, A., Khater, A.G.A., Gehrke, S.A., Serra, P., Francesco, I., Di Carmine, M., Tari, S.R., Leo, L., & Lorusso, F. (2023, May 24). Peri-Implant Diseases. In Encyclopedia. https://encyclopedia.pub/entry/44757
Scarano, Antonio, et al. "Peri-Implant Diseases." Encyclopedia. Web. 24 May, 2023.
Copy Citation
Dental implant-supported prostheses are a well-established rehabilitation treatment for partially or completely edentulous patients that restore function and esthetics while having long-term survival rates. The tissues surrounding osseointegrated dental implants are referred to as peri-implant tissues, consisting of soft and hard tissue parts. The soft tissue part forms following the placement of implant/abutment during the wound healing and is known as “peri-implant mucosa,” while the hard tissue part makes contact with the implant surface to ensure implant stability.
dental implant
evidence-based practice
mucositis
peri-implant disease
1. Peri-Implant Diseases and Conditions
1.1. Peri-Implant Health
Healthy peri-implant tissues is a more objective definition of implant success that focuses on the biological and esthetic health of surrounding tissues in addition to the implant function rather than just implant survival. This is clinically assessed by:
-
Absence of clinical inflammatory signs;
-
No bleeding and suppuration on mild probing (0.25 N);
-
Stable probing depth compared to previous visits;
-
Absence of radiographic bone loss (excluding physiological crestal bone loss one year after the prosthetic load of 0.5–2 mm) [1].
The physiological probing depth around implants cannot be determined since the absence of the periodontal ligament provides less resistance to probe insertion. Consequently, excessive force on probing can disrupt the integrity of the mucosa-abutment attachment and produce bleeding on healthy implants. As such, we could have peri-implant health on implants with reduced bone support, successfully treated implants, or implants positioned in a diminished alveolar crest [2].
The peri-implant mucosa section facing the implant consists of two compartments, a “coronal” compartment lined with the sulcular epithelium and a thin epithelial attachment, whereas the “apical” compartment contacts the connective tissue implant surface. Histologically, this mucosa contains a connective tissue core, often covered by orthokeratinized epithelium on its outer surface [1]. Therefore, after abutment placement, the mucosal height gradually stabilizes to 3–4 mm, with a 2 mm epithelium [3] (Figure 1).
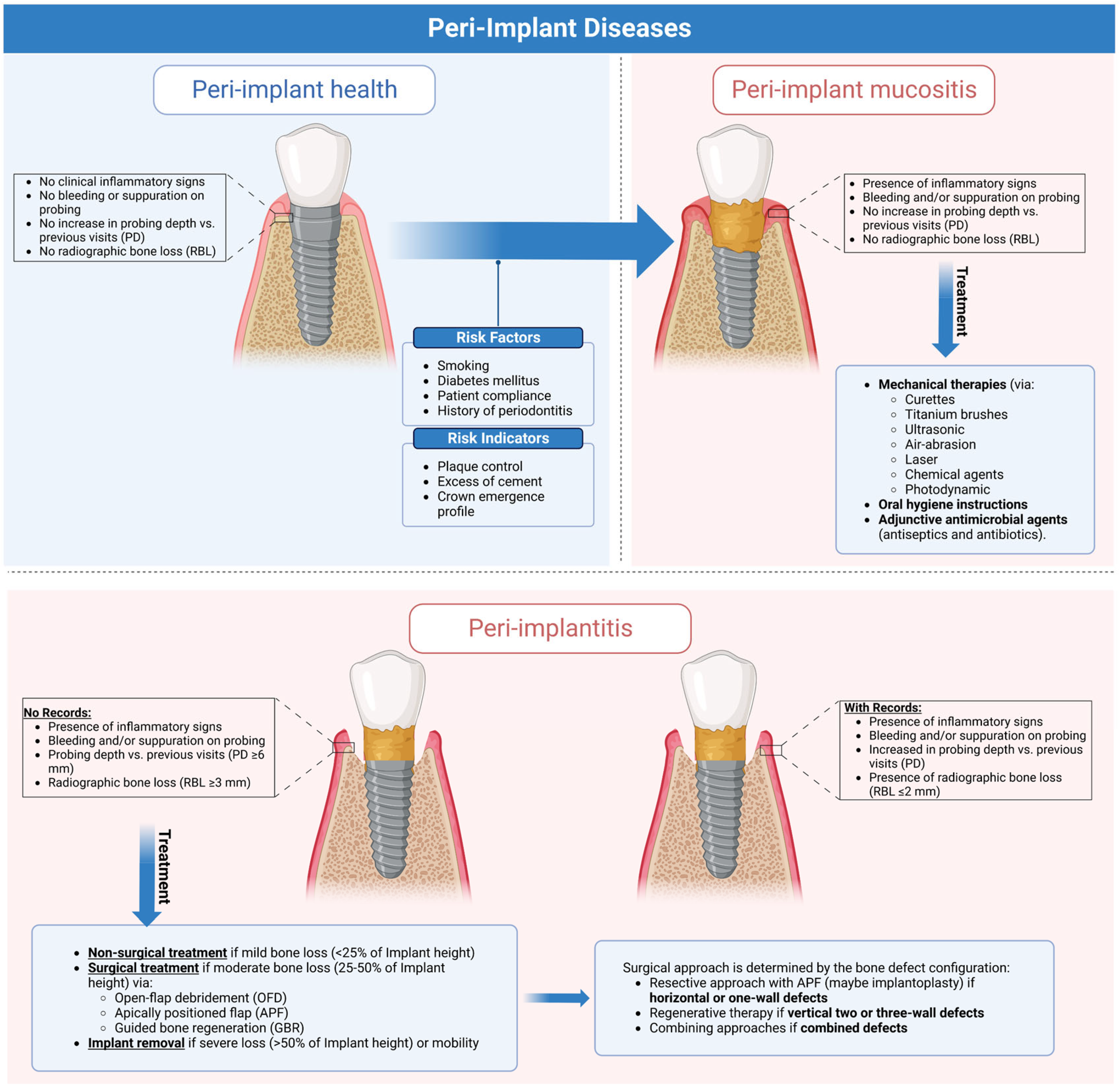
Figure 1. Graphical abstract illustrating the clinical characteristics of peri-implant health and diseases and current evidence-based approaches for managing peri-implant diseases. This figure was created using Biorender.com (https://app.biorender.com).
1.2. Peri-Implant Mucositis
Peri-implant mucositis (Figure 2) is an inflammation in the peri-implant tissue that is clinically identified by bleeding and/or suppuration on probing without radiographic bone loss [4].

Figure 2. Peri-implant mucositis; there is gingival inflammation around the implant unit.
Although a recognized cause–effect relationship exists between mucositis and plaque accumulation [5], reestablishing good oral hygiene could restore the clinical parameters and biochemical markers in the peri-implant crevicular fluid to normal. Even if implants have less plaque accumulation, they often show more inflammation and bleeding sites than teeth [6]. Histologically, the inflammatory lesion is found in the connective tissue, lateral to the epithelial barrier, and it is more extensive for advanced lesions (0.36 mm2) than in the early lesion (three weeks 0.14 mm2) (Figure 3).
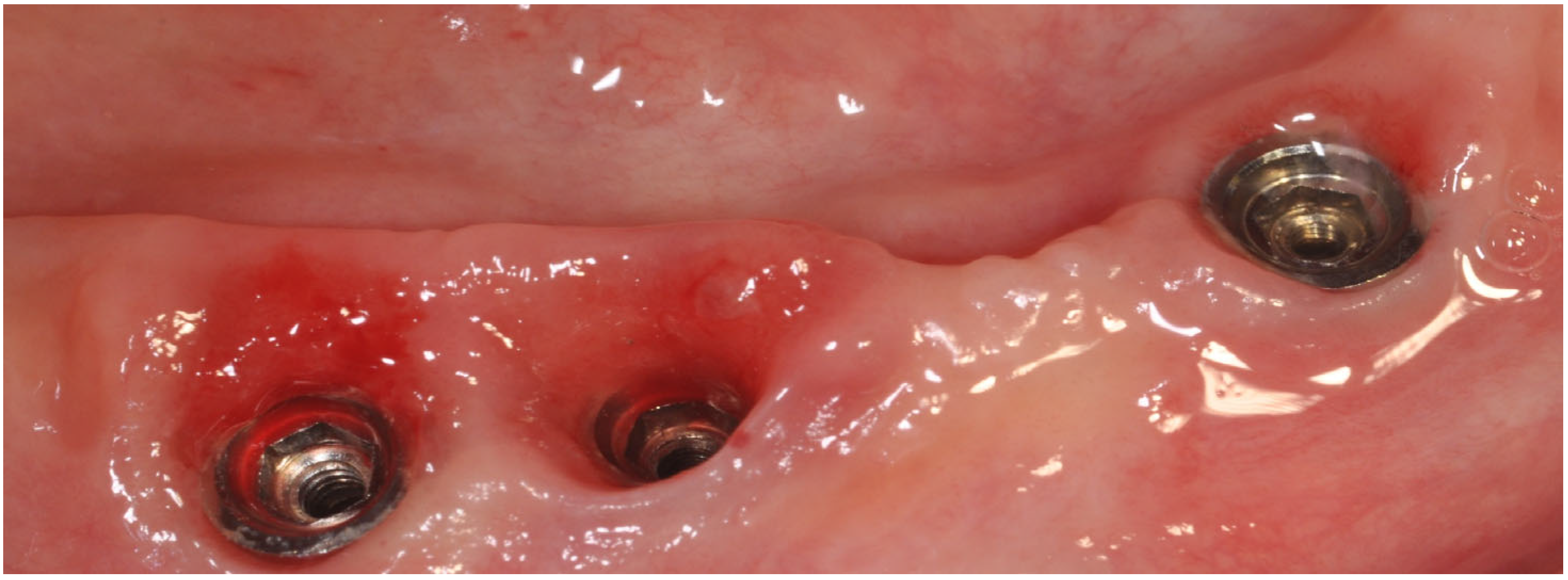
Figure 3. Peri-implant mucositis; inflammatory tissues induced by abutment loosening.
1.3. Peri-Implantitis
Peri-implant mucositis is an inflammation in the peri-implant soft tissues with a progressive loss in the supporting bone. It is clinically identified by bleeding and/or suppuration on probing, increased pocket depth compared to previous visits, and radiographic bone loss [7] (Figure 4).

Figure 4. Peri-implantitis; (A) Clinical signs. (B) Probing depth. (C) Peri-implant inflammatory tissue.
Standardized intraoral radiographs should be performed to monitor changes in bone levels around implants beginning with abutment placement, as crestal losses of more than 2 mm (physiological remodeling) from the baseline should be considered pathological [2]. When previous clinical or radiographic data are unavailable, the diagnosis should be confirmed by bleeding and/or suppuration on probing, a pocket depth greater than 6 mm, and more than 3 mm of radiographic bone loss (measured from the most coronal part of the marginal bone crest). Histologically, the inflammation becomes twice the size of the periodontal lesion (3.5 mm2 versus 1.5 mm2), extending to the bone crest and containing more neutrophils and lymphocytes B CD19+ than mucositis and more polymorphonuclear and macrophages than periodontitis [8][9] (Figure 5).
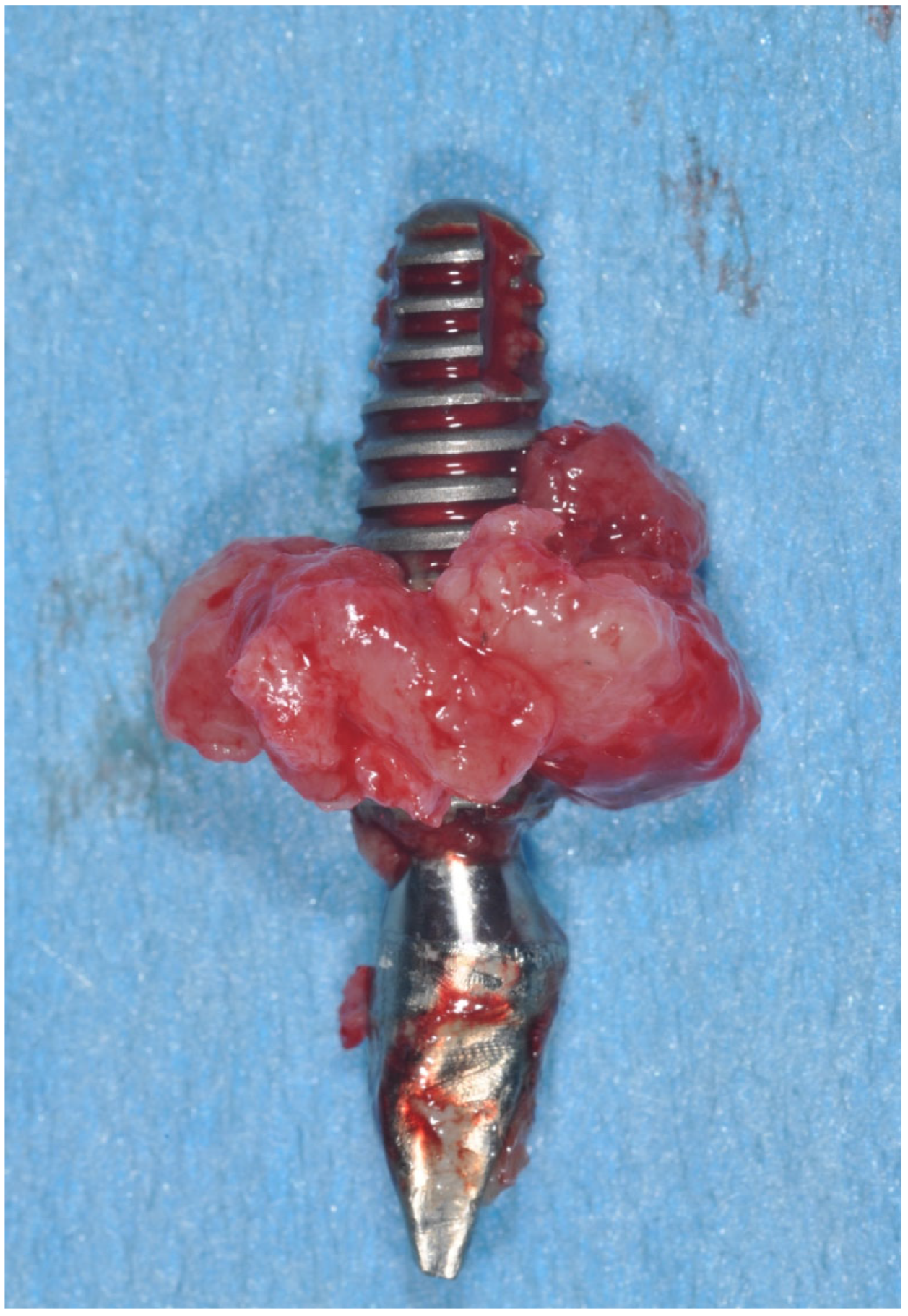
Figure 5. Clinical aspect of implant removed for peri-implantitis.
2. Epidemiology of Peri-Implant Diseases
Evaluation of the diseases’ epidemiological features aims to determine how frequently and why the disease arises. Such epidemiological data are used to assess and improve available disease-specific prevention approaches, which are often implemented to target the affected population [10]. As such, Derks et al. showed that the prevalence of peri-implant mucositis ranged from 19% to 65% and peri-implantitis from 1% to 47% [11]. However, Lee et al., in a meta-analysis, showed that the mean prevalence of peri-implant mucositis was 29.48% (implant-based) and 46.83% (subject-based), and the mean prevalence of peri-implantitis was 9.25% (implant-based) and 19.83% (subject-based) [12]. Moreover, Rakic et al. revealed in a meta-analysis that the peri-implantitis prevalence was 18.5% (implant-level) and 12.8% (patient-level) [13]; however, Dreyer et al. revealed in a meta-analysis that the peri-implantitis prevalence ranged from 1.1% to 85.0% (implant-level) and an incidence ranged from 0.4% (within three years) to 43.9% (within five years) [14].
Such variations in prevalence are due to methodological heterogeneity in reporting the peri-implant biological complications in studies, which limits attempts to estimate the true impact of peri-implant diseases globally; thus, that emphasizes the importance of fully adopting case definitions by the World Workshop on the Classification of Periodontal and Peri-implant Diseases (2017) for accurate prevalence estimation [15].
3. Risk Factors and Indicators
Risk factors are disease-causing agents usually established by longitudinal research, whereas risk indicators depend on cross-sectional investigations [16]. Several risk factors and risk indicators of peri-implant diseases are summarized in Figure 3. Smoking and diabetes are the most well-known systemic risk factors that have been reliably related to peri-implant disorders.
Poor plaque control is a risk factor since it makes it difficult to reach the implant sites during oral hygiene, explaining the higher incidence of peri-implantitis in areas with limited access to oral hygiene (65%) compared to cleanable areas (18%) [17]. Excess cement retained around peri-implant soft tissues promotes plaque accumulation due to its rough surface [18], and its removal promotes the normalization of inflammation indices [19]. Thus, cemented prostheses without cement residues appear to have no increased risk of developing peri-implantitis compared to screw-retained prostheses (Figure 4). Adherence to oral hygiene instructions is also a risk factor, as Costa et al. [20] and Roccuzzo et al. [21] found that individuals who followed a regular maintenance program had a lower incidence of peri-implantitis (18% and 27%, respectively) than those who did not (43% and 47%). There is controversy about the minimum amount of keratinized mucosa around the implant; however, many observational studies indicated that keratinized mucosal deficiency (<2 mm) causes more discomfort in oral hygiene procedures, higher plaque levels, deeper pockets, and bleeding [22][23].
The presence of peri-implantitis has been associated with many gene polymorphisms (e.g., IL-1 gene) and osteoprotegerin (IL-6, and TNF7). In addition, Titanium and/or iron particles were identified in peri-implant tissue biopsies and inflammatory cells at peri-implantitis areas [24]. Titanium atoms may boost T-lymphocyte differentiation towards the osteoclastic pathway [25] and could alter microbial genetic expression via epigenetic DNA methylation [26] (Figure 6).
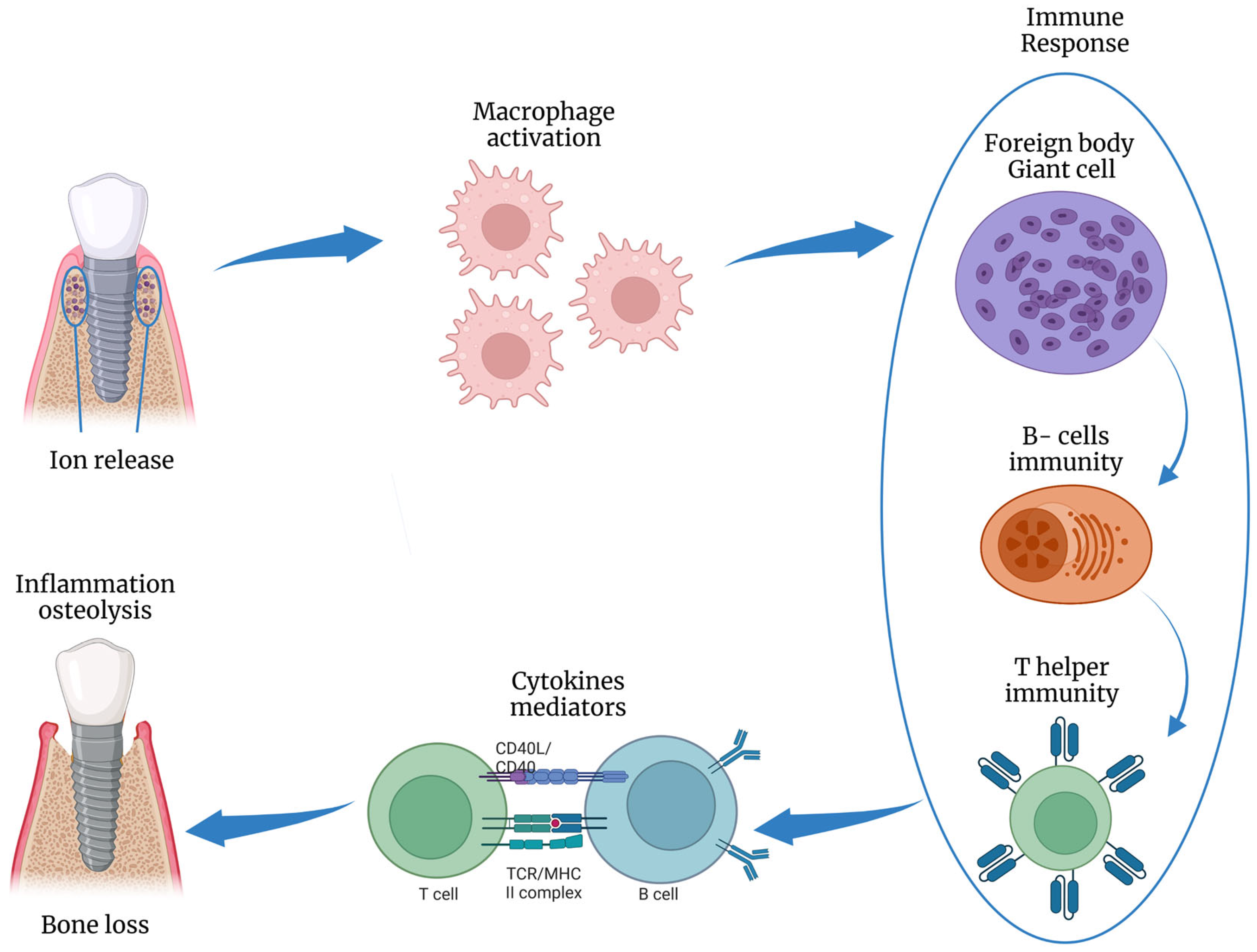
Figure 6. Schematic illustration of the inflammatory response to titanium ions release, inducing osteolysis. This figure was created using Biorender.com.
4. Prevention of Peri-Implant Diseases
With the increasing prevalence of peri-implantitis, and its irreversible condition with limited and expensive treatments, preventing peri-implant diseases is becoming paramount to decreasing its incidence and boosting implant success rates [27][28]. As such, The European Federation of Periodontology (EFP) established some recommendations for managing the primary risk factors of peri-implant diseases throughout implant workflow [27]. Proper personalized risk assessment for the individual patient is the primary key to these preventive measures, which aim to address and modify any relevant risk factors (either local or systemic) [28].
Such preventive measures begin before implant placement (“Primordial prevention”) by addressing the underlying risk factors that may induce disease development (e.g., preventing noncommunicable diseases (diabetes type-II) by healthy behavior promotion such as not smoking, increasing physical activity, and healthy diets) [28]. Once implant placement occurs, preventive measures (“Primary prevention”) are implemented to maintain the peri-implant tissues healthy over time and address any risk factors that may trigger disease onset, such as regularly controlling biofilm accumulation around implants and practically educating and motivating patients on oral hygiene measures). Then, early management and control of peri-implant mucositis should be implemented to prevent peri-implantitis progression (“Secondary prevention”) [28].
5. Treatment Strategies
Nonsurgical Treatment
Nonsurgical therapy includes mechanical debridement, oral hygiene instructions, and possibly local antiseptics, which are indicated in managing mucositis and peri-implantitis with mild bone loss (<25% of implant height) [29]. Mechanical debridement of the implant surface aimed to reduce the adhered biofilm and restrict bacterial colonization to maintain peri-implant health. That debridement could be achieved by curettes ultrasonic instruments, titanium brushes, air power abrasion, laser, chemical agents, and photodynamic therapy [30][31].
Surgical Treatment
Surgical therapy is often recommended for treating peri-implantitis (with moderate loss, i.e., 25–50% of the implant height) since nonsurgical therapy, despite being conservative, has a high recurrence rate and typically does not resolve peri-implant disease [32][33][34][35]. The surgical treatment aims to decontaminate the implant surface, create a healthy hard and soft tissue peri-implant anatomy that allows easy cleaning, and regenerate the infrabony defect (if possible) [36][37]. Surgical approaches for treating peri-implantitis include open-flap debridement (OFD), apically positioned flap (APF), and guided bone regeneration (GBR). The surgical approach is often determined by the bone defect configuration, as the resective approach with APF (possibly with implantoplasty) is indicated for horizontal or one-wall defects, regenerative therapy is indicated for vertical two or three-wall defects, and combining approaches with combined defects.
Implant Removal
When there is osseointegration failure (severe loss, i.e., >50% of height), implant fractures, complicated implant designs (i.e., hollow-cylinder implant), or intricate infections affecting the surrounding anatomical structures (e.g., inferior alveolar nerve, maxillary sinus), the implant should be removed [38][39][40].
References
- Araujo, M.G.; Lindhe, J. Peri-Implant Health. J. Periodontol. 2018, 89 (Suppl. 1), S249–S256.
- Renvert, S.; Persson, G.R.; Pirih, F.Q.; Camargo, P.M. Peri-Implant Health, Peri-Implant Mucositis, and Peri-Implantitis: Case Definitions and Diagnostic Considerations. J. Clin. Periodontol. 2018, 45, S278–S285.
- Tomasi, C.; Tessarolo, F.; Caola, I.; Piccoli, F.; Wennström, J.L.; Nollo, G.; Berglundh, T. Early Healing of Peri-implant Mucosa in Man. J. Clin. Periodontol. 2016, 43, 816–824.
- Heitz-Mayfield, L.J.A.; Salvi, G.E. Peri-Implant Mucositis. J. Clin. Periodontol. 2018, 45, S237–S245.
- Pontoriero, R.; Tonelli, M.P.; Carnevale, G.; Mombelli, A.; Nyman, S.R.; Lang, N.P. Experimentally Induced Peri-Implant Mucositis. A Clinical Study in Humans: Experimental Peri-Implant Mucositis. Clin. Oral Implant. Res. 1994, 5, 254–259.
- Meyer, S.; Giannopoulou, C.; Courvoisier, D.; Schimmel, M.; Müller, F.; Mombelli, A. Experimental Mucositis and Experimental Gingivitis in Persons Aged 70 or over. Clinical and Biological Responses. Clin. Oral Implant. Res. 2017, 28, 1005–1012.
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.-L. Peri-Implantitis. J. Periodontol. 2018, 89, S267–S290.
- Berglundh, T.; Zitzmann, N.U.; Donati, M. Are Peri-Implantitis Lesions Different from Periodontitis Lesions?: Peri-Implantitis and Periodontitis Lesions. J. Clin. Periodontol. 2011, 38, 188–202.
- Berglundh, T.; Gislason, O.; Lekholm, U.; Sennerby, L.; Lindhe, J. Histopathological Observations of Human Periimplantitis Lesions. J. Clin. Periodontol. 2004, 31, 341–347.
- Fowkes, F.G.; Dobson, A.J.; Hensley, M.J.; Leeder, S.R. The Role of Clinical Epidemiology in Medical Practice. Eff. Health Care 1984, 1, 259–265.
- Derks, J.; Tomasi, C. Peri-Implant Health and Disease. A Systematic Review of Current Epidemiology. J. Clin. Periodontol. 2015, 42, S158–S171.
- Lee, C.-T.; Huang, Y.-W.; Zhu, L.; Weltman, R. Prevalences of Peri-Implantitis and Peri-Implant Mucositis: Systematic Review and Meta-Analysis. J. Dent. 2017, 62, 1–12.
- Rakic, M.; Galindo-Moreno, P.; Monje, A.; Radovanovic, S.; Wang, H.-L.; Cochran, D.; Sculean, A.; Canullo, L. How Frequent Does Peri-Implantitis Occur? A Systematic Review and Meta-Analysis. Clin. Oral Investig. 2018, 22, 1805–1816.
- Dreyer, H.; Grischke, J.; Tiede, C.; Eberhard, J.; Schweitzer, A.; Toikkanen, S.E.; Glöckner, S.; Krause, G.; Stiesch, M. Epidemiology and Risk Factors of Peri-Implantitis: A Systematic Review. J. Periodontal Res. 2018, 53, 657–681.
- Cosgarea, R.; Sculean, A.; Shibli, J.A.; Salvi, G.E. Prevalence of Peri-Implant Diseases—A Critical Review on the Current Evidence. Braz. Oral Res. 2019, 33, e063.
- Renvert, S.; Polyzois, I.; Claffey, N. Surgical Therapy for the Control of Peri-Implantitis. Clin. Oral Implant. Res. 2012, 23, 84–94.
- Serino, G.; Ström, C. Peri-Implantitis in Partially Edentulous Patients: Association with Inadequate Plaque Control. Clin. Oral Implant. Res. 2009, 20, 169–174.
- Staubli, N.; Walter, C.; Schmidt, J.C.; Weiger, R.; Zitzmann, N.U. Excess Cement and the Risk of Peri-Implant Disease—A Systematic Review. Clin. Oral Impl. Res. 2017, 28, 1278–1290.
- Scarano, A.; Inchingolo, F.; Scogna, S.; Leo, L.; Greco Lucchina, A.; Mavriqi, L. Peri-Implant Disease Caused by Residual Cement around Implant-Supported Restorations: A Clinical Report. J. Biol. Regul. Homeost. Agents 2021, 35, 211–216.
- Costa, F.O.; Takenaka-Martinez, S.; Cota, L.O.M.; Ferreira, S.D.; Silva, G.L.M.; Costa, J.E. Peri-Implant Disease in Subjects with and without Preventive Maintenance: A 5-Year Follow-Up. J. Clin. Periodontol. 2012, 39, 173–181.
- Roccuzzo, M.; De Angelis, N.; Bonino, L.; Aglietta, M. Ten-Year Results of a Three-Arm Prospective Cohort Study on Implants in Periodontally Compromised Patients. Part 1: Implant Loss and Radiographic Bone Loss. Clin. Oral Implant. Res. 2010, 21, 490–496.
- Lin, G.-H.; Chan, H.-L.; Wang, H.-L. The Significance of Keratinized Mucosa on Implant Health: A Systematic Review. J. Periodontol. 2013, 84, 1755–1767.
- Gobbato, L.; Avila-Ortiz, G.; Sohrabi, K.; Wang, C.-W.; Karimbux, N. The Effect of Keratinized Mucosa Width on Peri-Implant Health: A Systematic Review. Int. J. Oral Maxillofac. Implant. 2013, 28, 1536–1545.
- Wilson, T.G.; Valderrama, P.; Burbano, M.; Blansett, J.; Levine, R.; Kessler, H.; Rodrigues, D.C. Foreign Bodies Associated with Peri-Implantitis Human Biopsies. J. Periodontol. 2015, 86, 9–15.
- Noumbissi, S.; Scarano, A.; Gupta, S. A Literature Review Study on Atomic Ions Dissolution of Titanium and Its Alloys in Implant Dentistry. Materials 2019, 12, 368.
- Daubert, D.; Pozhitkov, A.; McLean, J.; Kotsakis, G. Titanium as a Modifier of the Peri-Implant Microbiome Structure. Clin. Implant Dent. Relat. Res. 2018, 20, 945–953.
- Jepsen, S.; Berglundh, T.; Genco, R.; Aass, A.M.; Demirel, K.; Derks, J.; Figuero, E.; Giovannoli, J.L.; Goldstein, M.; Lambert, F.; et al. Primary Prevention of Peri-Implantitis: Managing Peri-Implant Mucositis. J. Clin. Periodontol. 2015, 42, S152–S157.
- Tonetti, M.S.; Chapple, I.L.C.; Jepsen, S.; Sanz, M. Primary and Secondary Prevention of Periodontal and Peri-Implant Diseases: Introduction to, and Objectives of the 11 th European Workshop on Periodontology Consensus Conference. J. Clin. Periodontol. 2015, 42, S1–S4.
- Kormas, I.; Pedercini, C.; Pedercini, A.; Raptopoulos, M.; Alassy, H.; Wolff, L.F. Peri-Implant Diseases: Diagnosis, Clinical, Histological, Microbiological Characteristics and Treatment Strategies. A Narrative Review. Antibiotics 2020, 9, 835.
- Figuero, E.; Graziani, F.; Sanz, I.; Herrera, D.; Sanz, M. Management of Peri-Implant Mucositis and Peri-Implantitis. Periodontol. 2000 2014, 66, 255–273.
- Wilson, T.G.; Valderrama, P.; Rodrigues, D.B.C. Commentary: The Case for Routine Maintenance of Dental Implants. J. Periodontol. 2014, 85, 657–660.
- Subramani, K.; Wismeijer, D. Decontamination of Titanium Implant Surface and Re-Osseointegration to Treat Peri-Implantitis: A Literature Review. Int. J. Oral Maxillofac. Implant. 2012, 27, 1043–1054.
- Lindhe, J.; Meyle, J.; on behalf of Group D of the European Workshop on Periodontology. Peri-Implant Diseases: Consensus Report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35, 282–285.
- Ramanauskaite, A.; Fretwurst, T.; Schwarz, F. Efficacy of Alternative or Adjunctive Measures to Conventional Non-Surgical and Surgical Treatment of Peri-Implant Mucositis and Peri-Implantitis: A Systematic Review and Meta-Analysis. Int. J. Implant Dent. 2021, 7, 112.
- Suárez-López del Amo, F.; Yu, S.-H.; Wang, H.-L. Non-Surgical Therapy for Peri-Implant Diseases: A Systematic Review. J. Oral Maxillofac. Res. 2016, 7, e13.
- Renvert, S.; Polyzois, I.; Maguire, R. Re-Osseointegration on Previously Contaminated Surfaces: A Systematic Review. Clin. Oral Implant. Res. 2009, 20, 216–227.
- Heitz-Mayfield, L.J.A.; Salvi, G.E.; Mombelli, A.; Faddy, M.; Lang, N.P.; On behalf of the Implant Complication Research Group Anti-Infective Surgical Therapy of Peri-Implantitis. A 12-Month Prospective Clinical Study. Clin. Oral Implant. Res. 2012, 23, 205–210.
- Schwarz, F.; Ramanauskaite, A. It Is All about Peri-implant Tissue Health. Periodontol. 2000 2022, 88, 9–12.
- Scarano, A.; Barros, R.R.M.; Iezzi, G.; Piattelli, A.; Novaes, A.B. Acellular Dermal Matrix Graft for Gingival Augmentation: A Preliminary Clinical, Histologic, and Ultrastructural Evaluation. J. Periodontol. 2009, 80, 253–259.
- Scarano, A.; Piattelli, A.; Polimeni, A.; Di Iorio, D.; Carinci, F. Bacterial Adhesion on Commercially Pure Titanium and Anatase-Coated Titanium Healing Screws: An In Vivo Human Study. J. Periodontol. 2010, 81, 1466–1471.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
676
Revisions:
2 times
(View History)
Update Date:
25 May 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




