Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Robert T. Mallet | -- | 1618 | 2023-05-15 16:18:13 | | | |
| 2 | Sirius Huang | Meta information modification | 1618 | 2023-05-16 10:47:57 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Mallet, R.T.; Burtscher, J.; Pialoux, V.; Pasha, Q.; Ahmad, Y.; Millet, G.P.; Burtscher, M. Pathophysiology of High Altitude Illnesses. Encyclopedia. Available online: https://encyclopedia.pub/entry/44321 (accessed on 08 February 2026).
Mallet RT, Burtscher J, Pialoux V, Pasha Q, Ahmad Y, Millet GP, et al. Pathophysiology of High Altitude Illnesses. Encyclopedia. Available at: https://encyclopedia.pub/entry/44321. Accessed February 08, 2026.
Mallet, Robert T., Johannes Burtscher, Vincent Pialoux, Qadar Pasha, Yasmin Ahmad, Grégoire P. Millet, Martin Burtscher. "Pathophysiology of High Altitude Illnesses" Encyclopedia, https://encyclopedia.pub/entry/44321 (accessed February 08, 2026).
Mallet, R.T., Burtscher, J., Pialoux, V., Pasha, Q., Ahmad, Y., Millet, G.P., & Burtscher, M. (2023, May 15). Pathophysiology of High Altitude Illnesses. In Encyclopedia. https://encyclopedia.pub/entry/44321
Mallet, Robert T., et al. "Pathophysiology of High Altitude Illnesses." Encyclopedia. Web. 15 May, 2023.
Copy Citation
High-altitude illnesses (HAIs) result from acute exposure to high altitude/hypoxia. Numerous molecular mechanisms effect appropriate acclimatization to hypobaric and/or normobaric hypoxia and curtail the development of HAIs.
altitude
hypoxia
acclimatization
oxidative stress
redox homeostasis
mitochondria
genes
1. Introduction
Acute exposure to high altitude imposes hypobaric hypoxia, raising the risk of high-altitude illnesses (HAIs) in inadequately acclimatized individuals [1][2][3]. Such illnesses include acute mountain sickness (AMS), the most frequently observed but usually benign and self-limited form of HAI, and the rare but life-threatening high-altitude cerebral edema (HACE) and high-altitude pulmonary edema (HAPE) [1][2]. Although hypobaria per se may contribute to HAI symptoms [4][5], the central pathogenetic factor is hypoxia [1][6][7][8]. Appropriate acclimatization to hypoxia, whether hypobaric or normobaric, can minimize or even prevent those illnesses [2][9][10].
Although systemic physiological responses to acute hypoxia and systemic physiological changes occurring during acclimatization are well established after decades of extensive research [11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][28][29], the molecular mechanisms driving these physiological adjustments are not fully understood [30][31][32][33][34][35]. The discovery and characterization of hypoxia-inducible factors (HIFs), key transcription factors regulating gene expression when cellular oxygen availability declines, and other molecular pathways mediating hypoxia responses [36] have paved the way to a better understanding of molecular processes underlying acclimatization to high altitude/hypoxia [37]. For their contributions to deciphering the molecular mechanisms of oxygen sensing in cells and tissues, William G. Kaelin Jr., Sir Peter J. Ratcliffe, and Gregg L. Semenza were awarded the 2019 Nobel Prize in Physiology or Medicine [38]. Nevertheless, our understanding of the complex cell- and tissue-specific signaling and signal integration leading to high-altitude acclimatization on a systemic level is still in its infancy, in particular when considering differences among individuals and additional environmental factors, such as temperature, humidity or radiation.
2. Systemic Physiological Responses to Acute High-Altitude Exposure and Acclimatization
The most important physiological responses to acute high altitude/hypoxia exposure comprise hyperventilation triggered by the hypoxic ventilatory response (HVR) [39], hemoconcentration due to enhanced diuresis, and an increase in heart rate and cardiac output as a result of sympathetic activation in hypoxia/at altitude [6][40]. In contrast to peripheral vasodilation, acute hypoxia exposure causes pulmonary vasoconstriction (HPV) and elevated pulmonary arterial pressure [17].
Ventilatory acclimatization to hypoxia (VAH), the progressive increase in ventilation during acclimatization, supports recovery of the initially reduced alveolar (PAO2) and arterial (PaO2) oxygen partial pressures and arterial oxygen saturation (SaO2) [12]. Increased ventilation lowers alveolar (PACO2) and arterial (PaCO2) partial pressures of carbon dioxide, producing respiratory alkalosis and compensatory renal bicarbonate excretion [41]. Paralleling the increased PaO2 and SaO2, both hemoconcentration and increased cardiac output (at rest and during exercise) help to maintain tissue oxygen delivery in the hypoxic high-altitude environment [42]. However, the acclimatization process, whether occurring at high altitude or in artificial environments (hypobaric or normobaric chambers, tents or face masks with reduced inspired oxygen), encompasses—in addition to ventilatory acclimatization—a broad spectrum of physiological changes, e.g., cardiovascular, cerebrovascular, metabolic, hematological, neurophysiological, and hormonal adjustments [2][10][43][44][45]. Figure 1 depicts the time courses of selected physiological responses to moderate or high altitude/hypoxia.
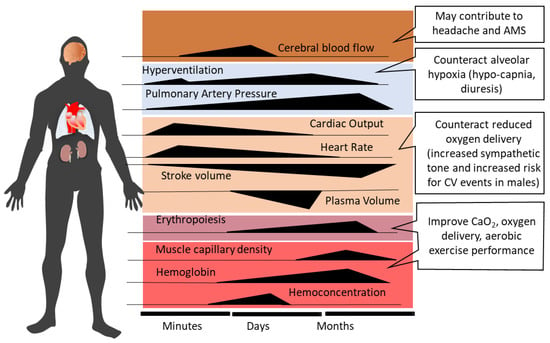
Figure 1. Time-dependent changes and related consequences of physiological responses during acclimatization to high altitude (modified from Burtscher et al., 2022 [10]). AMS, acute mountain sickness; CV, cardiovascular; CaO2, arterial oxygen content.
Alveolar minute ventilation progressively increases over the first 8–10 days at altitude and then plateaus [12][46]. Sympathetic activation at the onset of acute altitude/hypoxia exposure acutely increases heart rate and systemic blood pressure [47][48]. Over the following 10 days at altitude, heart rate tends to decrease [48][49], while elevated systemic blood pressure persists [47]. Increased PAO2 with acclimatization may produce some dampening of HPV [50][51]. As the initial hemoconcentration subsides, HIF-1 related upregulation of erythropoietin (EPO) sustains the increases in hemoglobin (Hb) concentration and arterial oxygen content (CaO2 = Hb x SaO2) after the first 1–2 weeks of high-altitude exposure [52]. The increase in muscle capillarity due to vascular endothelial growth factor (VEGF) up-regulation [53] represents another HIF-1-initiated response to altitude/hypoxia exposure.
3. High Altitude Illnesses: Epidemiology and Pathophysiology
This section provides a brief overview of the heterogeneous pathophysiologic processes involved in the development of HAIs, which are largely determined by the diverse responses and susceptibility to hypoxia-associated injury among individuals. A comprehensive understanding of the pathophysiology of HAI is essential for the development of new treatment options, for example, to facilitate successful acclimatization by targeting adaptive or maladaptive signaling pathways and molecular processes.
3.1. Acute Mountain Sickness and High-Altitude Cerebral Edema
Acute mountain sickness (AMS) frequently develops in high-altitude visitors and typically follows a benign disease course, with symptoms that often resolve over a few days of acclimatization [2][54]. AMS incidence steeply increases with an ascent in altitude or hypoxia intensity (from about 7% at 2200 m to over 50% at 4559 m) in susceptible individuals not acclimatized to high altitude/hypoxia [55][56]. The incidences of severe AMS and HACE are about 24% and 1%, respectively, at 4000 m altitude [57].
Unacclimatized individuals typically develop AMS symptoms within the first 6 to 12 h of acute high-altitude exposure [1][2]. While headache represents the cardinal symptom, subjects most susceptible to AMS typically develop nausea first [58]. In persons suffering from HACE, altered mental status and ataxia are the most prevalent symptoms and are often accompanied by headache, anorexia, nausea, vomiting, and retinal hemorrhages [59][60]. AMS development in unacclimatized persons may be ascribable to acute cellular and/or systemic responses that are delayed and/or insufficient to maintain oxygen delivery to tissues at high altitudes [2][12][39].
Diagnosis of AMS is usually based on the Lake Louise Scoring system (LLS) or less frequently on the abridged (11-item) version (ESQ-C) of the 67-item Environmental Symptoms Questionnaire (ESQ-III) [2]. The original LLS [61] is a self-assessment questionnaire, rating the severity (no discomfort = 0; mild symptoms = 1; moderate symptoms = 2; severe symptoms = 3) of five main criteria, i.e., headache, nausea, dizziness, fatigue, and difficulty sleeping, but has recently been revised by deleting the “difficulty sleeping” criterion [62].
Increased intracranial pressure, brain swelling and edema formation may constitute AMS pathophysiology and explain the symptoms [63][64][65]. Sequential magnetic resonance imaging (MRI) scans during a 22-h exposure to normobaric hypoxia (FiO2: 0.12) demonstrated total brain parenchymal expansion, but only the extent of white matter edema (indicating vasogenic edema) correlated with AMS severity [63]. These authors suggested that veno-compression of the small and deep cerebral veins likely contributes to elevated intracranial pressure and brain swelling [63]. Major AMS symptoms, i.e., headache, may result from activation and sensitization of the trigemino-vascular system via mechanical (e.g., elevated cranial and/or intravascular pressure) and/or biochemical (e.g., reactive oxygen species (ROS), nitric oxide (NO), prostaglandins, inflammatory molecules) factors [19][66][67][68].
Why and when severe AMS progresses to HACE remains unclear. Although AMS and HACE are often considered manifestations on a continuum of cerebral HAIs [69], with mild AMS likely progressing to severe AMS and, in rare cases, even to HACE [69], whether HACE really is a severe form of AMS [1] or rather an independent entity remains to be established. The occurrence of white matter edema in HACE indicates dysfunction or disruption of the blood-brain barrier (BBB), which may be caused by ROS-related membrane destabilization and inflammation and/or local HIF and VEGF activation [70].
Pharmacological treatment options for AMS primarily aim to improve oxygen delivery (e.g., hyperoxic breathing or augmenting hyperventilation by the use of acetazolamide), reduce AMS symptoms (e.g., headache) and/or prevent cerebral edema formation by administration of dexamethasone and/or nonsteroidal anti-inflammatory drugs [1][2][71]. However, prevention of AMS in particular, and HAIs in general, through appropriate acclimatization strategies is the most effective countermeasure.
3.2. High-Altitude Pulmonary Edema
Both HACE and HAPE represent life-threatening diseases with ~50% mortality when untreated [71]. Like AMS and HACE, the incidence of HAPE primarily depends on the rate of ascent, the absolute altitude attained and the individual’s susceptibility to HAPE. For instance, in mountaineers with unknown HAPE history who ascended over 4 days to an altitude of 4500 m, the HAPE incidence was 0.2%, but the incidence increased to 6% when ascending in only 1–2 days [71], underscoring the importance of acclimatization to prevent HAPE.
HAPE is a non-cardiogenic pulmonary edema caused by pronounced hypoxic pulmonary vasoconstriction and related elevations of pulmonary-artery and capillary pressures, resulting in a noninflammatory and hemorrhagic alveolar capillary leak [72]. Genetic predisposition has been implicated as a cause of the remarkably robust pulmonary vascular responses to hypoxia in some individuals, which may be attributed to insufficient formation and bioavailability of NO likely associated with high ROS levels in hypoxia/at altitude [73][74].
While in high-altitude pulmonary hypertension (HAPH), inflammatory pathways may importantly contribute to the proliferation of pulmonary artery smooth muscle cells and pulmonary hypertension [75], this may not be the case for HAPE. Although inflammation in HAPE could contribute to increased alveolar-capillary permeability, studies in humans rather indicate that inflammation constitutes a secondary response to the pulmonary edema and/or disruption of the alveolar-capillary barrier, not a primary factor in HAPE pathogenesis [72].
Besides rapid descent and oxygen supplementation, administration of the calcium channel blocker nifedipine has been shown to be effective for HAPE prophylaxis and treatment [17][76], but others have questioned nifedipine’s effectiveness [77].
It must be mentioned that apart from hypoxia, several other environmental and/or behavioral factors could contribute to the heightened risk of serious illnesses at high altitudes [78]. Although a comprehensive examination of these factors and their interactions with hypoxia are beyond the scope of this text, the potential contributions of hypothermia and dehydration to HAIs merit discussion. For example, exposure to cold at high altitudes may predispose mountaineers to dehydration due to elevated cold-diuresis and poor access to fluids [79]. These authors identified an association between the level of dehydration and the risk of AMS [79]. Moreover, exposure to cold and altitude may increase the risk of thrombosis and myocardial infarction [80]. Heavy exercise at altitude exacerbates dehydration, raising the risk of rhabdomyolysis and acute liver injury [81], and intensifying arterial hypoxemia, thereby triggering or accelerating the development of AMS [82]. Furthermore, both severe low ambient temperature and intense physical activity are also implicated as predisposing factors for HAPE development, primarily due to the increase in pulmonary artery pressure [83][84].
References
- Hackett, P.H.; Roach, R.C. High-altitude illness. N. Engl. J. Med. 2001, 345, 107–114.
- Burtscher, M.; Hefti, U.; Hefti, J.P. High-altitude illnesses: Old stories and new insights into the pathophysiology, treatment and prevention. Sport. Med. Health Sci. 2021, 3, 59–69.
- Burtscher, J.; Mallet, R.T.; Pialoux, V.; Millet, G.P.; Burtscher, M. Adaptive responses to hypoxia and/or hyperoxia in humans. Antioxid. Redox Signal. 2022, 37, 887–912.
- Millet, G.P.; Debevec, T. CrossTalk proposal: Barometric pressure, independent of PO2, is the forgotten parameter in altitude physiology and mountain medicine. J. Physiol. 2020, 598, 893–896.
- Loeppky, J.A.; Roach, R.C.; Maes, D.; Hinghofer-Szalkay, H.; Roessler, A.; Gates, L.; Fletcher, E.R.; Icenogle, M.V. Role of hypobaria in fluid balance response to hypoxia. High Alt. Med. Biol. 2005, 6, 60–71.
- Bärtsch, P.; Gibbs, J.S. Effect of altitude on the heart and the lungs. Circulation 2007, 116, 2191–2202.
- West, J.B.; Richalet, J.P. Denis Jourdanet (1815–1892) and the early recognition of the role of hypoxia at high altitude. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2013, 305, L333–L340.
- Luks, A.M.; Swenson, E.R.; Bartsch, P. Acute high-altitude sickness. Eur. Respir. Rev. 2017, 26, 160096.
- Tannheimer, M.; Lechner, R. Rapid ascents of Mt Everest: Normobaric hypoxic preacclimatization. J. Travel Med. 2020, 27, taaa099.
- Burtscher, M.; Millet, G.P.; Burtscher, J. Hypoxia conditioning for high-altitude pre-acclimatization. J. Sci. Sport Exerc. 2022, 4, 331–345.
- Houston, C.S. Acute pulmonary edema of high altitude. N. Engl. J. Med. 1960, 263, 478–480.
- Lenfant, C.; Sullivan, K. Adaptation to high altitude. N. Engl. J. Med. 1971, 284, 1298–1309.
- West, J.B.; Hackett, P.H.; Maret, K.H.; Milledge, J.S.; Peters, R.M.; Pizzo, C.J.; Winslow, R.M. Pulmonary gas exchange on the summit of Mount Everest. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 1983, 55, 678–687.
- Sutton, J.R.; Reeves, J.T.; Wagner, P.D.; Groves, B.M.; Cymerman, A.; Malconian, M.K.; Rock, P.B.; Young, P.M.; Walter, S.D.; Houston, C.S. Operation Everest II: Oxygen transport during exercise at extreme simulated altitude. J. Appl. Physiol. 1988, 64, 1309–1321.
- Hackett, P.H.; Roach, R.C.; Schoene, R.B.; Harrison, G.L.; Mills, W.J. Abnormal control of ventilation in high-altitude pulmonary edema. J. Appl. Physiol. 1988, 64, 1268–1272.
- Oelz, O.; Maggiorini, M.; Ritter, M.; Waber, U.; Jenni, R.; Vock, P.; Bärtsch, P. Nifedipine for high altitude pulmonary oedema. Lancet 1989, 2, 1241–1244.
- Bärtsch, P.; Maggiorini, M.; Ritter, M.; Noti, C.; Vock, P.; Oelz, O. Prevention of high-altitude pulmonary edema by nifedipine. N. Engl. J. Med. 1991, 325, 1284–1289.
- Roach, R.C.; Greene, E.R.; Schoene, R.B.; Hackett, P.H. Arterial oxygen saturation for prediction of acute mountain sickness. Aviat. Space Environ. Med. 1998, 69, 1182–1185.
- Burtscher, M.; Likar, R.; Nachbauer, W.; Philadelphy, M. Aspirin for prophylaxis against headache at high altitudes: Randomised, double blind, placebo controlled trial. BMJ 1998, 316, 1057–1058.
- Hackett, P.H. High altitude cerebral edema and acute mountain sickness. A pathophysiology update. Adv. Exp. Med. Biol. 1999, 474, 23–45.
- Sartori, C.; Allemann, Y.; Trueb, L.; Delabays, A.; Nicod, P.; Scherrer, U. Augmented vasoreactivity in adult life associated with perinatal vascular insult. Lancet 1999, 353, 2205–2207.
- Scherrer, U.; Sartori, C.; Lepori, M.; Allemann, Y.; Duplain, H.; Trueb, L.; Nicod, P. High-altitude pulmonary edema: From exaggerated pulmonary hypertension to a defect in transepithelial sodium transport. Adv. Exp. Med. Biol. 1999, 474, 93–107.
- Maggiorini, M.; Melot, C.; Pierre, S.; Pfeiffer, F.; Greve, I.; Sartori, C.; Lepori, M.; Hauser, M.; Scherrer, U.; Naeije, R. High-altitude pulmonary edema is initially caused by an increase in capillary pressure. Circulation 2001, 103, 2078–2083.
- Calbet, J.A.; Rådegran, G.; Boushel, R.; Søndergaard, H.; Saltin, B.; Wagner, P.D. Effect of blood haemoglobin concentration on V(O2,max) and cardiovascular function in lowlanders acclimatised to 5260 m. J. Physiol. 2002, 545, 715–728.
- Swenson, E.R.; Maggiorini, M.; Mongovin, S.; Gibbs, J.S.; Greve, I.; Mairbäurl, H.; Bärtsch, P. Pathogenesis of high-altitude pulmonary edema: Inflammation is not an etiologic factor. JAMA 2002, 287, 2228–2235.
- Bernardi, L.; Schneider, A.; Pomidori, L.; Paolucci, E.; Cogo, A. Hypoxic ventilatory response in successful extreme altitude climbers. Eur. Respir. J. 2006, 27, 165–171.
- Bloch, J.; Duplain, H.; Rimoldi, S.F.; Stuber, T.; Kriemler, S.; Allemann, Y.; Sartori, C.; Scherrer, U. Prevalence and time course of acute mountain sickness in older children and adolescents after rapid ascent to 3450 meters. Pediatrics 2009, 123, 1–5.
- Naeije, R.; Huez, S.; Lamotte, M.; Retailleau, K.; Neupane, S.; Abramowicz, D.; Faoro, V. Pulmonary artery pressure limits exercise capacity at high altitude. Eur. Respir. J. 2010, 36, 1049–1055.
- Berger, M.M.; Sareban, M.; Bärtsch, P. Acute mountain sickness: Do different time courses point to different pathophysiological mechanisms? J. Appl. Physiol. 2020, 128, 952–959.
- Julian, C.G. Epigenomics and human adaptation to high altitude. J. Appl. Physiol. 2017, 123, 1362–1370.
- Gassmann, M.; Muckenthaler, M.U. Adaptation of iron requirement to hypoxic conditions at high altitude. J. Appl. Physiol. 2015, 119, 1432–1440.
- Prabhakar, N.R.; Semenza, G.L. Adaptive and maladaptive cardiorespiratory responses to continuous and intermittent hypoxia mediated by hypoxia-inducible factors 1 and 2. Physiol. Rev. 2012, 92, 967–1003.
- Pham, K.; Frost, S.; Parikh, K.; Puvvula, N.; Oeung, B.; Heinrich, E.C. Inflammatory gene expression during acute high-altitude exposure. J. Physiol. 2022, 600, 4169–4186.
- Samaja, M.; Milano, G. Adaptation to Hypoxia: A Chimera? Int. J. Mol. Sci. 2020, 21, 1527.
- Samaja, M.; Milano, G. Hypoxia and reoxygenation: From basic science to bedside. Front. Pediatr. 2015, 3, 86.
- Lee, P.; Chandel, N.S.; Simon, M.C. Cellular adaptation to hypoxia through hypoxia inducible factors and beyond. Nat. Rev. Mol. Cell Biol. 2020, 21, 268–283.
- Semenza, G.L. Life with oxygen. Science 2007, 318, 62–64.
- Lee, C.C.; Wu, C.Y.; Yang, H.Y. Discoveries of how cells sense oxygen win the 2019 Nobel Prize in physiology or medicine. Biomed. J. 2020, 43, 434–437.
- Weil, J.V.; Byrne-Quinn, E.; Sodal, I.E.; Friesen, W.O.; Underhill, B.; Filley, G.F.; Grover, R.F. Hypoxic ventilatory drive in normal man. J. Clin. Investig. 1970, 49, 1061–1072.
- Reeves, J.T. Sympathetics and Hypoxia: A Brief Review; Burlington VT: Queen City, TX, USA, 1993; pp. 1–6.
- Zouboules, S.M.; Lafave, H.C.; O’Halloran, K.D.; Brutsaert, T.D.; Nysten, H.E.; Nysten, C.E.; Steinback, C.D.; Sherpa, M.T.; Day, T.A. Renal reactivity: Acid-base compensation during incremental ascent to high altitude. J. Physiol. 2018, 596, 6191–6203.
- Burtscher, M.; Faulhaber, M.; Flatz, M.; Likar, R.; Nachbauer, W. Effects of short-term acclimatization to altitude (3200 m) on aerobic and anaerobic exercise performance. Int. J. Sports Med. 2006, 27, 629–635.
- Savourey, G.; Garcia, N.; Besnard, Y.; Hanniquet, A.M.; Fine, M.O.; Bittel, J. Physiological changes induced by pre-adaptation to high altitude. Eur. J. Appl. Physiol. Occup. Physiol. 1994, 69, 221–227.
- Wolff, C.B.; Barry, P.; Collier, D.J. Cardiovascular and respiratory adjustments at altitude sustain cerebral oxygen delivery—Severinghaus revisited. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2002, 132, 221–229.
- Samaja, M.; di Prampero, P.E.; Cerretelli, P. The role of 2,3-DPG in the oxygen transport at altitude. Respir. Physiol. 1986, 64, 191–202.
- Sato, M.; Severinghaus, J.W.; Bickler, P. Time course of augmentation and depression of hypoxic ventilatory responses at altitude. J. Appl. Physiol. 1994, 77, 313–316.
- Bilo, G.; Caravita, S.; Torlasco, C.; Parati, G. Blood pressure at high altitude: Physiology and clinical implications. Kardiol. Pol. 2019, 77, 596–603.
- Dünnwald, T.; Kienast, R.; Niederseer, D.; Burtscher, M. The use of pulse oximetry in the assessment of acclimatization to high altitude. Sensors 2021, 21, 1263.
- Rimoldi, S.F.; Sartori, C.; Seiler, C.; Delacrétaz, E.; Mattle, H.P.; Scherrer, U.; Allemann, Y. High-altitude exposure in patients with cardiovascular disease: Risk assessment and practical recommendations. Prog. Cardiovasc. Dis. 2010, 52, 512–524.
- Swenson, E.R. Hypoxic pulmonary vasoconstriction. High Alt. Med. Biol. 2013, 14, 101–110.
- Naeije, R. Physiological adaptation of the cardiovascular system to high altitude. Prog. Cardiovasc. Dis. 2010, 52, 456–466.
- Garvican, L.; Martin, D.; Quod, M.; Stephens, B.; Sassi, A.; Gore, C. Time course of the hemoglobin mass response to natural altitude training in elite endurance cyclists. Scand. J. Med. Sci. Sports 2012, 22, 95–103.
- Breen, E.; Tang, K.; Olfert, M.; Knapp, A.; Wagner, P. Skeletal muscle capillarity during hypoxia: VEGF and its activation. High Alt. Med. Biol. 2008, 9, 158–166.
- Fulco, C.S.; Beidleman, B.A.; Muza, S.R. Effectiveness of preacclimatization strategies for high-altitude exposure. Exerc. Sport Sci. Rev. 2013, 41, 55–63.
- Maggiorini, M.; Bühler, B.; Walter, M.; Oelz, O. Prevalence of acute mountain sickness in the Swiss Alps. BMJ 1990, 301, 853–855.
- Mairer, K.; Wille, M.; Bucher, T.; Burtscher, M. Prevalence of acute mountain sickness in the Eastern Alps. High Alt. Med. Biol. 2009, 10, 239–245.
- Richalet, J.P.; Larmignat, P.; Poitrine, E.; Letournel, M.; Canouï-Poitrine, F. Physiological risk factors for severe high-altitude illness: A prospective cohort study. Am. J. Respir. Crit. Care Med. 2012, 185, 192–198.
- Burtscher, M.; Wille, M.; Menz, V.; Faulhaber, M.; Gatterer, H. Symptom progression in acute mountain sickness during a 12-hour exposure to normobaric hypoxia equivalent to 4500 m. High Alt. Med. Biol. 2014, 15, 446–451.
- Wu, T.; Ding, S.; Liu, J.; Jia, J.; Dai, R.; Liang, B.; Zhao, J.; Qi, D. Ataxia: An early indicator in high altitude cerebral edema. High Alt. Med. Biol. 2006, 7, 275–280.
- Davis, C.; Hackett, P. Advances in the prevention and treatment of high altitude illness. Emerg. Med. Clin. N. Am. 2017, 35, 241–260.
- Roach, R.C.; Bärtsch, P.; Hackett, P.H.; Oelz, O. The Lake Louise acute mountain sickness scoring system. In Hypoxia and Molecular Medicine, Sutton, J.R., Coates, G., Eds.; Queen City Press: Burlington, NJ, USA, 1993; pp. 272–274.
- Roach, R.C.; Hackett, P.H.; Oelz, O.; Bärtsch, P.; Luks, A.M.; MacInnis, M.J.; Baillie, J.K.; Committee, L.L.A.S.C. The 2018 Lake Louise acute mountain sickness score. High Alt. Med. Biol. 2018, 19, 4–6.
- Sagoo, R.S.; Hutchinson, C.E.; Wright, A.; Handford, C.; Parsons, H.; Sherwood, V.; Wayte, S.; Nagaraja, S.; Ng’Andwe, E.; Wilson, M.H.; et al. Magnetic Resonance investigation into the mechanisms involved in the development of high-altitude cerebral edema. J. Cereb. Blood Flow Metab. 2017, 37, 319–331.
- Kallenberg, K.; Bailey, D.M.; Christ, S.; Mohr, A.; Roukens, R.; Menold, E.; Steiner, T.; Bärtsch, P.; Knauth, M. Magnetic resonance imaging evidence of cytotoxic cerebral edema in acute mountain sickness. J. Cereb. Blood Flow Metab. 2007, 27, 1064–1071.
- Schoonman, G.G.; Sándor, P.S.; Nirkko, A.C.; Lange, T.; Jaermann, T.; Dydak, U.; Kremer, C.; Ferrari, M.D.; Boesiger, P.; Baumgartner, R.W. Hypoxia-induced acute mountain sickness is associated with intracellular cerebral edema: A 3 T magnetic resonance imaging study. J. Cereb. Blood Flow Metab. 2008, 28, 198–206.
- Sanchez del Rio, M.; Moskowitz, M.A. High altitude headache. Lessons from headaches at sea level. Adv. Exp. Med. Biol. 1999, 474, 145–153.
- Serrano-Dueñas, M. High-altitude headache. Expert Rev. Neurother. 2007, 7, 245–248.
- Burtscher, M.; Mairer, K.; Wille, M.; Broessner, G. Risk factors for high-altitude headache in mountaineers. Cephalalgia 2011, 31, 706–711.
- Gallagher, S.A.; Hackett, P.H. High-altitude illness. Emerg. Med. Clin. N. Am. 2004, 22, 329–355.
- Lafuente, J.V.; Bermudez, G.; Camargo-Arce, L.; Bulnes, S. Blood-brain barrier changes in high altitude. CNS Neurol. Disord. Drug Targets 2016, 15, 1188–1197.
- Bärtsch, P.; Swenson, E.R. Clinical practice: Acute high-altitude illnesses. N. Engl. J. Med. 2013, 368, 2294–2302.
- Swenson, E.R.; Bärtsch, P. High-altitude pulmonary edema. Compr. Physiol. 2012, 2, 2753–2773.
- Eichstaedt, C.A.; Mairbäurl, H.; Song, J.; Benjamin, N.; Fischer, C.; Dehnert, C.; Schommer, K.; Berger, M.M.; Bärtsch, P.; Grünig, E.; et al. Genetic predisposition to high-altitude pulmonary edema. High Alt. Med. Biol. 2020, 21, 28–36.
- Scherrer, U.; Turini, P.; Thalmann, S.; Hutter, D.; Salmon, C.S.; Stuber, T.; Shaw, S.; Jayet, P.Y.; Sartori-Cucchial, C.; Villena, M.; et al. Pulmonary hypertension in high-altitude dwellers: Novel mechanisms, unsuspected predisposing factors. Adv. Exp. Med. Biol. 2006, 588, 277–291.
- El Alam, S.; Pena, E.; Aguilera, D.; Siques, P.; Brito, J. Inflammation in pulmonary hypertension and edema induced by hypobaric hypoxia exposure. Int. J. Mol. Sci. 2022, 23, 2656.
- Oelz, O.; Maggiorini, M.; Ritter, M.; Noti, C.; Waber, U.; Vock, P.; Bärtsch, P. Prevention and treatment of high altitude pulmonary edema by a calcium channel blocker. Int. J. Sports Med. 1992, 13 (Suppl. S1), S65–S68.
- Deshwal, R.; Iqbal, M.; Basnet, S. Nifedipine for the treatment of high altitude pulmonary edema. Wilderness Environ. Med. 2012, 23, 7–10.
- Boggild, A.K.; Costiniuk, C.; Kain, K.C.; Pandey, P. Environmental hazards in Nepal: Altitude illness, environmental exposures, injuries, and bites in travelers and expatriates. J. Travel Med. 2007, 14, 361–368.
- Nerín, M.A.; Palop, J.; Montaño, J.A.; Morandeira, J.R.; Vázquez, M. Acute mountain sickness: Influence of fluid intake. Wilderness Environ. Med. 2006, 17, 215–220.
- Whayne, T.F., Jr. Altitude and cold weather: Are they vascular risks? Curr. Opin. Cardiol. 2014, 29, 396–402.
- Yeh, Y.C.; Chen, C.C.; Lin, S.H. Case report: Severe rhabdomyolysis and acute liver injury in a high-altitude mountain climber. Front. Med. 2022, 9, 917355.
- Roach, R.C.; Maes, D.; Sandoval, D.; Robergs, R.A.; Icenogle, M.; Hinghofer-Szalkay, H.; Lium, D.; Loeppky, J.A. Exercise exacerbates acute mountain sickness at simulated high altitude. J. Appl. Physiol. 2000, 88, 581–585.
- Schoene, R.B.; Roach, R.C.; Hackett, P.H.; Harrison, G.; Mills, W.J. High altitude pulmonary edema and exercise at 4400 meters on mount McKinley. Effect of expiratory positive airway pressure. Chest 1985, 87, 330–333.
- Swenson, E.R. Early hours in the development of high-altitude pulmonary edema: Time course and mechanisms. J. Appl. Physiol. 2020, 128, 1539–1546.
More
Information
Subjects:
Physiology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
509
Revisions:
2 times
(View History)
Update Date:
16 May 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




