Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Thifhelimbilu Emmanuel (E) Luvhengo | -- | 5108 | 2023-05-04 02:18:50 | | | |
| 2 | Conner Chen | Meta information modification | 5108 | 2023-05-05 02:44:12 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Luvhengo, T.E.; Bombil, I.; Mokhtari, A.; Moeng, M.S.; Demetriou, D.; Sanders, C.; Dlamini, Z. Diagnosis and Management of Follicular Carcinoma. Encyclopedia. Available online: https://encyclopedia.pub/entry/43723 (accessed on 07 February 2026).
Luvhengo TE, Bombil I, Mokhtari A, Moeng MS, Demetriou D, Sanders C, et al. Diagnosis and Management of Follicular Carcinoma. Encyclopedia. Available at: https://encyclopedia.pub/entry/43723. Accessed February 07, 2026.
Luvhengo, Thifhelimbilu Emmanuel, Ifongo Bombil, Arian Mokhtari, Maeyane Stephens Moeng, Demetra Demetriou, Claire Sanders, Zodwa Dlamini. "Diagnosis and Management of Follicular Carcinoma" Encyclopedia, https://encyclopedia.pub/entry/43723 (accessed February 07, 2026).
Luvhengo, T.E., Bombil, I., Mokhtari, A., Moeng, M.S., Demetriou, D., Sanders, C., & Dlamini, Z. (2023, May 04). Diagnosis and Management of Follicular Carcinoma. In Encyclopedia. https://encyclopedia.pub/entry/43723
Luvhengo, Thifhelimbilu Emmanuel, et al. "Diagnosis and Management of Follicular Carcinoma." Encyclopedia. Web. 04 May, 2023.
Copy Citation
Follicular thyroid carcinoma (FTC) is the second most common cancer of the thyroid gland, accounting for up to 20% of all primary malignant tumors in iodine-replete areas. The diagnostic work-up, staging, risk stratification, management, and follow-up strategies in patients who have FTC are modeled after those of papillary thyroid carcinoma (PTC), even though FTC is more aggressive. FTC has a greater propensity for haematogenous metastasis than PTC. Furthermore, FTC is a phenotypically and genotypically heterogeneous disease. The diagnosis and identification of markers of an aggressive FTC depend on the expertise and thoroughness of pathologists during histopathological analysis.
follicular carcinoma
genomics
multi-omics
1. Introduction
Primary thyroid carcinoma (TC) can originate from the follicular cells, para-follicular cells, or lymphoid tissues. Thyroid cancers constitute 1–5% of malignancies in adults [1][2]. Cancers of the thyroid of follicular cell origin are divided into well-differentiated thyroid carcinoma (WDTC), poorly differentiated and undifferentiated/anaplastic carcinoma thyroid carcinoma (ATC) [1][2][3][4][5][6][7]. The WDTCs include papillary thyroid carcinoma (PTC), follicular thyroid carcinoma (FTC), and oncocytic cell carcinoma (OC) [8][9]. Papillary carcinoma and FTC consist of several subtypes. The diagnosis of PTC and FTC together with their subtypes is based on the presence of classical nuclear features and the architecture of the tumor [10][11][12].
Over 90% of WDTCs are sporadic. The major risk factors for WDTCs include previous exposure to ionizing radiation, a persistently abnormal level of iodine, and Hashimoto’s thyroiditis [13][14][15][16][17]. Around 85–90% of thyroid cancers in an iodine-replete environment are classical and other subtypes of PTC [18][19]. The prevalence of FTC is influenced by the iodine status of that region [20][21][22][23][24]. The experience of the histopathologists also influences the rate of diagnosis, as other benign and malignant lesions of the thyroid may be mistaken for FTC [25]. Although FTC can occur in children, it is predominantly a disease of females over the age of 40 [26][27].
The majority of patients who have TC present with euthyroid goiter, and a few present due to metastasis to cervical lymph nodes or distant sites from an occult primary tumor [28][29]. Sometimes a WDTC is detected incidentally during the histological analysis of a specimen following a thyroidectomy for supposedly benign goiter [30]. Sometimes, a patient who has a localized or metastatic FTC may present with hyperthyroidism [31][32]. The diagnostic work-up of a patient who is suspected to have TC includes thyroid function testing (TFT), ultrasound, and fine needle aspiration cytology (FNAC) [33][34]. The diagnosis of PTC following FNAC is based on the existence of typical nuclear features and/or architectural changes [35]. Supplementary imaging investigations, immunohistochemistry, mutational analysis, and diagnostic thyroid lobectomy are added if FNAC is not diagnostic, which is likely in the case of FTC [36][37][38][39].
The definitive management of WDTC is either lobectomy or total thyroidectomy. Lymph node dissection, thyroid stimulating hormone (TSH) suppression, I-131 treatment, tyrosine kinase inhibitors, and external beam radiotherapy are added based on clinicopathological findings [1][8][40]. The risk level of the disease influences the choice of the management strategy for WDTC [8][41]. Well-differentiated thyroid cancers are heterogeneous tumors with divergent clinical behavior, response to treatment, and overall outcome [42][43]. Risk stratification of FTC includes the age of a patient, tumour size, evidence and extent of extra-thyroidal extension. The other factors that are important in the risk stratification of a patient who has FTC are the existence lymph node or systemic metastasis, pre-operative level of thyroglobulin (Tg) and completeness of surgical excision. The histological subtype, tumour differentiation of the tumour, immunohistochemistry, genomics, epigenomics, metabolomics and the changes in the micro-environment of the tumour also have an influence on the prognosis of WDTC and therefore guide of appropriate treatment [26][27][28][41][44][45][46][47][48][49][50][51]. Additional markers that have been found to be useful in the risk stratification of patients with TC include serum Vitamin D and the neutrophil-to-lymphocyte ratio (NLR) [52][53].
Although observation alone or lobectomy with lifelong follow-up may be appropriate for low-risk WDTC, patients whose tumors have a high risk of local recurrence or mortality should have total thyroidectomy with or without lymph node dissection, adjuvant or therapeutic I-131, aggressive TSH suppression, and intense monitoring during follow-up [1]. Although the 10-year survival of 90% of patients who are diagnosed with WDTC is over 95%, around 10% of the WDTCs are however unexpectedly aggressive and have a markedly reduced disease-free survival [2][3][8]. Patients who have been diagnosed with WDTC need a lifelong follow-up, which should be more intense in the first year following the initiation of treatment [1][54][55][56][57]. The follow-up program for patients who have WDTC includes clinical evaluation, neck ultrasound, monitoring of serum Tg, and radioisotope scanning, based on the patient’s risk level [1].
Thyroid cancer is a heterogeneous disease clinically and genotypically among patients and within itself and its metastases [58][59]. There is also high inter- and intra-observer variability during the interpretation of the results of imaging and FNAC or histopathological specimens of follicular-patterned neoplasms of the thyroid gland [60]. The current diagnostic and staging modalities used in WDTC are not able to accurately quantify the burden of the disease, and recurrence or progression of WDTC is sometimes detected late. Untreated WDTC has a propensity towards de-differentiating and becoming more aggressive as it progresses, and a previously low-risk and well-differentiated cancer may acquire new mutations, de-differentiate, and become aggressive and resistant to I-131 [8][9][61][62].
Follicular thyroid carcinoma cannot be diagnosed pre-operatively on FNAC because it can be confused with a follicular adenoma, rarely spread to lymph nodes, and has a different mutational landscape from that of PTC [9][25][47][63]. Additionally, FTC has a higher tendency, when compared with PTC and other thyroid malignancies, to present with systemic metastases from an occult primary tumor [57][64][65]. Additionally, patients who have FTC may present with hyperthyroidism [31][32][66]. The prognosis of patients with FTC is worse than that of classical PTC [56]. Table 1 contains a summary of the comparison of FTC with PTC.
Table 1. Comparison of demography and clinicopathological features of follicular and papillary carcinomas.
| Parameter | FTC | PTC |
|---|---|---|
| Gender predilection | Females | Females |
| Age [45][67] | >50 years | <50 years |
| Risk factors | Iodine deficiency, colloid goiter. | Radiation, iodine excess and thyroiditis. |
| Genetic predisposition | <3% | <5% |
| Tumour size at presentation [60] | Large | Small |
| Multifocality [68] | Rare | Common |
| FNAC diagnosis | No | Yes |
| Tumour capsule | Yes | No |
| Capsular and vascular invasion | Common | Rare |
| Main subtypes [69][70] | 3 | >12 |
| Prevalent mutations or re-arrangements [71] | RAS, PAX8, PPARƴ, VEGFR. | BRAF, RET, VEGFR. |
| Lymph node metastasis [68][72] | Rare (<10%) | Common (20–90%) |
| Haematogenous metastasis [45][68] | Frequent (29%) | Rare (9%) |
| Standard surgical treatment | Lobectomy or total thyroidectomy | Lobectomy or total thyroidectomy with or without lymph node dissection. |
| 10-Year disease free survival [60][68] | 72% | 92% |
2. Diagnosis and Management of Follicular Carcinoma
Follicular carcinoma is the second most common malignant tumor of the thyroid gland and makes up around 10–15% of TCs [2][73]. There are two subtypes of FTC: minimally invasive follicular thyroid carcinoma (mi-FTC) and widely invasive follicular thyroid carcinoma (wi-FTC) carcinoma [9][11][35][62][74] (Figure 1).
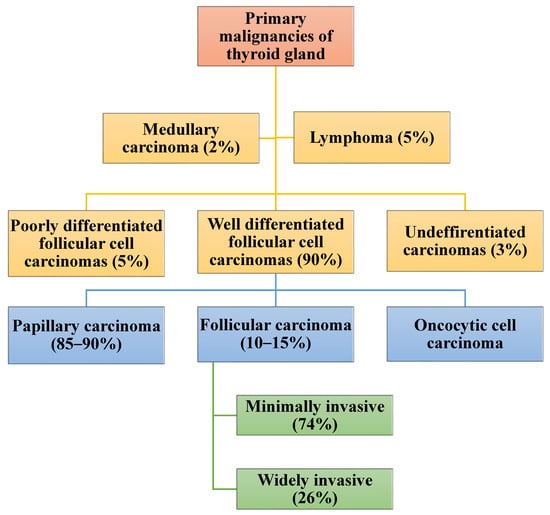
Figure 1. Classification and proportional rate of occurrence of follicular carcinoma and other thyroid malignancies.
The majority (86%) of FTC is diagnosed in women above the age of 40 years [5][75]. Less than 5% of FTC is heritable and related to syndromes such as FAP, Cowden’s disease, ataxia telangiectasia, and Li-Fraumeni syndrome [76][77]. Follicular carcinoma can develop from a pre-existing follicular adenoma (FA) [9][78][79]. Unlike with PTC, ionizing radiation and Hashimoto’s thyroiditis are not risk factors for follicular carcinoma [17]. The incidence of follicular carcinoma is decreasing globally [16][18][24][30][80][81]. Much of the decline in the prevalence of FTC is due to the iodine supplementation program, increasing expertise among pathologists, advances in immunohistochemistry, and the ability to perform mutational analysis [10][30][82]. However, around 72% of other types of thyroid cancer, including the follicular variant of PTC (FVPTC), are still mistakenly diagnosed as FTC [25][34][83][84][85][86][87]. Additionally, the OC was in the past erroneously considered a sub-type of FTC [88].
Follicular carcinoma of the thyroid usually presents as a nodular goiter, and rarely, patients who have FTC may present with hyperthyroidism or distant metastases from an occult primary tumor [57][64][89]. The common sites of distant metastases from FTC include bone, lung, and brain [57][90][91]. Lymph node metastasis occurs in less than 10% of FTC. The presence of lymph node metastases in a patient who has FTC should necessitate a review of the histopathology slides to rule out a missed FVPTC or other malignancies of the thyroid gland [92]. Because of its relative rarity, the diagnostic workup, staging, risk stratification, treatment, and follow-up of FTC are according to the guidelines developed for the management of PTC [1]. Follicular carcinoma is, however, clinically and genotypically different from PTC. Follicular carcinoma is more aggressive, has a greater propensity for haematogenous metastasis, and is associated with a shorter disease-free survival compared to PTC [28][83][92]. A longstanding FTC may de-differentiate and become a poorly differentiated (PDTC) or an undifferentiated/anaplastic thyroid carcinoma (ATC) [3][7][61][93][94][95][96][97]. Follicular thyroid carcinoma can also co-exist with other malignant tumors of the thyroid gland, which include medullary thyroid carcinoma (MTC) [98][99].
2.1. Diagnostic Work-Up of Suspected Follicular Carcinoma
Follicular carcinoma of the thyroid is rarely suspected pre-operatively except in patients who present with systemic metastasis [100][101]. The diagnostic work-up of a suspected FTC is like what is done for any patient presenting with a euthyroid nodular goiter and should include TFT, ultrasound, and FNAC [1]. None of the pre-operative investigations can confirm the diagnosis of FTC [87][100][101]. The majority of patients who have FTC are euthyroid, and the ultrasound examination is likely to show the same worrisome malignancy that is seen in PTC [102][103][104][105][106]. Among the worrisome features for malignancy on ultrasound of FTC is a solid hypoechoic lesion that is taller than wide and has increased intra-nodal vascularity, micro-calcifications, and an irregular border [102][103][104][105][107][108]. Follicular carcinoma is less likely to be multi-centric or multi-focal or be associated with regional lymph node involvement when compared with PTC [40][109]. Ultrasound also helps to pick up cervical lymph node metastasis and is complemented by a CT scan.
The Bethesda System of Reporting and Interpreting Thyroid FNAC (Bethesda System) is the most commonly used system to guide decision making regarding observation, repeat testing, additional pre-operative investigations, diagnostic lobectomy, or definitive surgical procedure for cancer [33][110][111]. The categories of the Bethesda system are non-diagnostic, benign, atypical, indeterminate, suspicious of malignancy, and malignant [33]. Result of FNAC of FTC is likely to yield a Bethesda III or IV lesion, which is an atypical or follicular neoplasm, respectively [33][112]. Follicular carcinoma is differentiated from FA by evidence of vascular and/or capsular invasion, which cannot be shown on FNAC, and FNAC is therefore not able to distinguish FTC from FA [87][100][113]. Follicular adenoma and FTC cannot be distinguished even after immunohistochemistry and mutational analysis [113]. The other thyroid conditions that may be mistaken for FTC following FNAC are adenomatous lesions of colloid goiter, FVPTC, OC, and the follicular variant of medullary carcinoma [87][114]. The diagnosis of FTC is only made after a lobectomy or total thyroidectomy. Diagnostic lobectomy is however unnecessary in up to 70% of the patients whose FNAC yielded a Bethesda System III or IV lesion, as the histology is likely to show a benign disease [33].
2.2. Staging of Follicular Carcinoma
The AJCC/TNM staging is used to stage WDTCs, including FTC, and parameters that are considered during the staging are the age of the patient, size of the tumor, evidence of extrathyroidal extension, presence of lymph node metastasis, and/or distant metastases [115]. Patients who are older than 55 years are at high risk of tumor progression or recurrence [2][116]. The categories that are used for tumor size are <2 cm, 2–4 cm, and >4 cm, whereas the nodal involvement is divided into involvement of the central nervous system, including level VII, or lateral cervical lymph nodes [115].
2.3. Risk Stratification and Associated Challenges in Follicular Carcinoma
The risk stratification of WDTCs considers gender and age of the patient, family history, type of tumor and histological subtype. The other parameters for risk stratification are tumor differentiation, degree of tumor necrosis, mitotic count, Ki67 index, mutational status and molecular subtypes. Lymph node status, thyroglobulin level, radio-iodine uptake, and PET/CT scan uptake are also important for risk assessment [26][35][51][92][117][118][119][120][121]. Follicular carcinoma is usually more aggressive than PTC, and the WI-FTC is likely to have distant metastases at presentation and lower disease-free survival [122][123]. The same risk scoring systems that are used in PTC are relied on for categorization of FTC, and among them are TNM staging; metastasis, age, completeness of resection, invasion, and size (MACIS); age, gender, extra-thyroidal extension, and size (AGES) and age, metastasis, extra-thyroidal extension and size (AMES) [117][119][123]. Low-risk FTC is a tumor that is less than 4 cm in maximum diameter and has no extra-thyroidal extension, lymph node, or distant metastasis, whereas an intermediate- or high-risk tumor is larger than 4 cm. A patient who has an FTC that is not completely excised, has extensive extrathyroidal extension, or has metastasized to lymph nodes or distant organs has a high-risk tumor [41][124]. Markers that have been used for risk-stratification of WDTC, including FTC, include vitamin D level and neutrophil-lymphocyte ratio (NLR) [52][53].
Patients who have FTC and are older than 55 years old are at increased risk of tumor recurrence or metastasis [2][116]. The organ involved influence the prognosis of patients who have systemic metastases. Patients who have pulmonary metastases from FTC generally do better than those who have metastases to bone, brain, liver, and other organs [91][125]. The prognosis depends on the volume of metastasis in an organ [91][125]. All the risk scoring systems, including the AJCC/TNM systems, are however not able to accurately quantify the burden of the disease, especially in patients with FTC [126]. The pathological diagnosis of FTC and its subtypes is dependent on the availability of expertise to perform the histopathological analysis [85]. Like other cancers, FTC is heterogenous, the aggressive component of the tumor may be overlooked during histopathological assessment, and a patient who has supposedly had mi-FTC and has had an appropriate lobectomy or total thyroidectomy may present years later with distant metastases [45]. The metastases are likely to have been there and were missed during the pre-operative assessment.
2.4. Management of Follicular Carcinoma and Related Challenges
The management of FTC follows that of PTC, and the selection of the package of care depends on the risk of recurrence and mortality [13][109]. Lobectomy or total thyroidectomy is the primary curative management of FTC. The other treatment strategies of FTC are added depending on the level of risk [51][56][59][124][127]. Lymph node metastasis occurs in less than 10% of FTCs, and lymphadenectomy is only performed if the involvement is confirmed clinically and/or following imaging investigation [40][109]. Additional treatment that may be required during the treatment of FTC includes radioactive iodine, TSH suppression, metastectomy, tyrosine kinase inhibitors (TKIs), multi-kinase inhibitors (MKIs), and de-differentiation therapy [8][9][61][62][128]. Evidence of de-differentiation of the tumor, which is likely if the tumor is locally advanced with extensive extra-thyroidal extension or is metastatic, may also influence the decision regarding further management of FTC [3][8][61][96][129][130][131].
2.4.1. Lobectomy versus Total Thyroidectomy in FTC
The diagnosis of FTC is not possible on pre-operative FNAC and is usually made following a diagnostic lobectomy, and the need for a complete thyroidectomy is only considered thereafter based on the size of the tumor and whether a patient is at high risk for recurrence or metastasis [124]. Lobectomy alone is appropriate for a tumor that is 1–4 cm in maximum diameter without high-risk features based on clinical, histological, immunohistochemical, or mutational analysis [56][59]. Total thyroidectomy should be the standard of care for FTC if the primary lesion is more than 4 cm in diameter. Mi-FCT usually has a benign course and does not require a complete thyroidectomy or radioactive iodine ablation. However, areas of major invasion may be missed during histopathological analysis, leading to the erroneous labeling of a wi-FTC as a mi-FTC [11]. The ability to perform mutational analysis is also not universally available.
Another parameter to consider is multifocality. Although the FTC is less likely to be multifocal when compared with the PTC, lobectomy alone in patients who have multifocal disease may lead to recurrence of the tumor [15][68][85]. The tumor that was left in the other lobe may de-differentiate and become a PDTC or ATC [8][54][72][122][129]. The extent of the primary tumor is another predictor of a poorer outcome in patients with FTC. Patients with macroscopic extra-thyroidal spread are at high risk of local recurrence or metastasis and should therefore be offered total thyroidectomy [68][132]. A total thyroidectomy is mandatory if the FTC is metastatic, as post-operative radioactive iodine would be required.
2.4.2. Radioactive Iodine Therapy and Dosimetry in the Management of FTC
Radioactive iodine is indicated in the management of intermediate- and high-risk FTC for the ablation of a remnant or as adjuvant therapy or treatment of metastatic disease following total thyroidectomy [13]. The aim of ablation therapy is to prevent local recurrence and to facilitate the use of Tg as a tumor marker for monitoring during follow-up [2][3][13][133]. The standard dose of I-131 for ablation of the remnant of the thyroid is 30 mCi. The dose for ablation of the remnant is administered around 6 weeks after a near-total or total thyroidectomy, when the s-TSH level is expected to have risen to 30 mIU/mL or higher [134]. A high level of s-TSH is achieved after a period of deferral of thyroxine replacement or by using recombinant TSH [72][133]. Adjuvant I-131 is to target presumed micrometastases from an intermediate- or high-risk FTC, which were however not picked up during pre-operative evaluation [56]. A dose of up to 150 mCi is necessary for ablation of metastases from FTC and can be increased to around 200 mCi if the metastases are extensive [3][28][133][134].
The dose of I-131 is adjusted considering the age of the patient, co-morbidities, the organ involved, and the burden of the metastases [72][133]. Clinical dosimetry is, however, less accurate when compared with radioisotope-based dosimetry. Dosimetry using I-124, I-123, or I-131 is useful for guiding the most effective dose of I-131 while reducing the likelihood of side effects [13]. Radioisotope-based dosimetry may also assist in the early identification of dedifferentiated metastases from FTC that are not trapping the iodine to avoid futile treatment. Problems associated with the use of I-131 during the management of FTC include side-effects like bone marrow suppression, xerostomia, infertility, severe hypothyroidism during the suspension of thyroxine replacement, and the development of a second primary malignant tumor [125][132][135][136]. The additional concerns of the use of I-131 for treatment in patients who have extensive lungs or brain metastases are that they may develop pulmonary fibrosis that may lead to respiratory failure or brain oedema, respectively [90][125][136]. Other challenges linked to the management of FTC using I-131 include the heterogeneity of cancer. The FTC may not be I-131 avid and therefore resistant to radioactive treatment. Resistance to I-131 is likely in patients who have metastatic disease [3][47][93][97][130][133][134][137][138][139][140]. Around 10% of TC cancers are under-staged and deemed low-risk, not needing I-131 ablation or adjuvant therapy). Similarly, areas of WI-FTC may be missed during histopathological analysis [11][84].
2.4.3. Thyroid Stimulating Hormone Suppression during Management of FTC
Patients who have had a total thyroidectomy need thyroxine for replacement and suppression. All patients who have FTC require TSH suppression regardless of the risk level [13][115][124]. The intensity of TSH suppression depends on the age of the patient, the presence of co-morbidity, and the level of risk for tumor recurrence or mortality [124][141]. The TSH suppression may be severe, moderate, or minimal [142]. Severe TSH suppression is when the TSH level is below 0.01 mU/L, moderate suppression is 0.01–0.1 mU/L, and mild suppression is 0.1–0.5 mIU/L [142]. Severe and moderate TSH suppression increase the risk of cardiac and musculoskeletal side effects. Cardiac side effects of high doses of thyroxine include atrial fibrillation and an increased risk of ischemic heart disease [143][144]. Osteoporosis is among the most severe musculoskeletal complications of a suppressive dose of thyroxine [145]. Additional side effects of extreme TSH suppression include depression and weight loss [145]. Furthermore, some of the patients may be misclassified as having low-risk instead of high-risk FTC and be erroneously placed on a less intense TSH suppression program [146]. The other problem with TSH suppression in the management of FTC is in tumors that have acquired aggressive mutations, have de-differentiated, and are no longer responsive to treatment [9][81][140].
2.4.4. Management of FTC with Extensive Extra-Thyroidal Extension
Some of the patients who have FTC may present with a tumor that has invaded the aerodigestive tract [49][147]. Mortality in half of the patients who have TC is related to local invasion of the upper aerodigestive tract and major vessels in the neck by the tumor [148]. Despite the extensive local invasion, curative resection may still be feasible unless the tumor is invading the carotid vessels or prevertebral fascia [147][149]. The nature of surgical resection may be extensive en-block resection of the larynx or oesophagus or a shaved excision [147]. Other treatment options for FTC with extensive extra-thyroidal extension include external beam radiotherapy and radiofrequency ablation [94][150]. Extensive extra-thyroidal extension is a marker of a high-risk FTC that is likely in tumors that have de-differentiated and become PDTC or ATC [94][147]. The area of de-differentiation might have been missed during the sampling and analysis of the FNAC or post-thyroidectomy specimen [94]. In some cases, the cancer might have already spread systemically, making the sometimes-debilitating en-block resection a futile operation.
2.5. Management of Metastatic Follicular Carcinoma and Related Challenges
The incidence of systemic metastases in FTC has been reported at 5–23% [148][151]. Follicular cancer rather than papillary thyroid cancer is more likely to metastasize to distant organs. Common sites of metastases for WDTC are the lungs, bones, brain, skin, and liver [65][91]. Male sex, older age, tumor size greater than or equal to 4 cm, vascular invasion, and lymph node involvement are some of the risk factors for systemic metastasis from FTC [151]. Systemic metastases are likely in TC with evidence of extra-thyroidal extension [151]. Poor prognostic features in patients who have metastatic FTC include age over 55 years, size of metastasis above 10mm in the maximum diameter at detection, and a high neutrophil to lymphocyte ratio). Well-differentiated FTC, especially in children, and FVPTC are relatively more I-131 avid and are therefore likely to respond to ablation or treatment [121].
The choice of treatment for FTC considers the patient’s age, comorbid conditions, sites, and number of metastases [1][5][40][51][63][72]. The prognosis of metastatic FTC is better in children and young adults, patients who have isolated lung metastases, metastases less than 5 cm in maximum diameter, and oligometastatic disease [1][2][26][40][51][56][63][66][71][72]. Patients who have intermediate- or high-risk FTC are likely to have systemic metastasis and be given adjuvant I-131 [1]. Radioactive iodine treatment is for the management of patients whose metastases are overt, and a dose of up to 200 mCi is used [115]. Treatment with I-131 is added after a patient has had a total thyroidectomy with or without resection of metastases that are amenable to resection [72]. Some of the problems associated with I-131 treatment of metastatic disease include the side effects, which are sometimes severe, like bone marrow suppression, infertility, and the development of another cancer [72][125]. A higher dose of I-131 is to be avoided in patients who have extensive pulmonary metastases and borderline lung function, multiple brain metastases, or large metastases to the vertebra, as it may lead to complications like pulmonary fibrosis, brain oedema, or instability of the spine [115][125]. However, extensive metastases are less likely to be iodine-avid as they would most probably have mutated and de-differentiated.
Patients who have metastatic FTC are in the high-risk group for WDTC and should be placed on an intense or high TSH-suppression protocol, unless there are contraindications, or it is not tolerated. The other options in the management of metastatic FTC are surgical excision, external beam radiotherapy, local ablative therapy, and kinase inhibitors. Surgical excision is preferred for the treatment of isolated metastases from FTC to most organs, including the lung, bone, brain, and liver. The TKIs are useful alone or when combined with other multi-kinase inhibitors (MKIs), especially if the FTC has dedifferentiated and is no longer retaining I-131 [72]. Examples of TKIs include lapatinib and vemurafenib [152]. The MKIs that are useful against WDTC include cabozantinib, lenvatinib, and sorafenib [71][153][154].
2.5.1. Pulmonary Metastases
The lung is the commonest site of distant metastases from FTC. Patients who have pulmonary metastases from FTC have a reduced 5-year and 10-year survival of 68.5% and 54%, respectively [151]. Lung metastases in FTC are likely to be macronodular when compared with secondary tumors in PTC [151]. The success rate of I-131 in the management of pulmonary metastases from FTC is lower than the 58% that is achieved in cases of metastatic PTC [151]. Patients who have FTC are usually older than those who have PTC and are therefore more likely to have co-morbidities [68]. A tolerable dose of I-131 depends on the baseline lung function and the extent of the disease, as ablation of the extensive pulmonary metastasis and their replacement with fibrous tissue may push the patient to irreversible respiratory failure. The other options for the treatment of pulmonary metastasis from FTC include surgical excision, percutaneous ablation, stereotactic radiotherapy, and tyrosine kinase or multi-kinase inhibitors [151].
The 18F-FDG PET/CT is useful for the investigation of recurrent or metastatic FTC when it is no longer I-131 iodine-avid. De-differentiation of FTC is associated with an increase in the expression of glucose transporter receptor type 1 and therefore high uptake of 18F-FDG PET/CT [72]. The uptake of DOTA PET by some of the metastases from FTC that have lost the ability to trap iodine is even higher than that of 18F-FDGvPET/CT, which raises the possibility of utilizing 177Lu as a potential theranostic agent [151]. There are numerous society guidelines for the management of metastatic disease from differentiated thyroid cancers, and most of them address WDTCs as a group and not specifically FTC [45]. The guidelines are mainly for PTC. Ongoing research for markers predictive of poor prognosis includes the investigation of Telomerase Reverse Transcriptase (TERT) promoters and RNA H-19. Challenges associated with the management of metastatic FTC include delay in their detection, underestimation of the extent of the disease, and dealing with metastases that do not take I-131 [148]. Sometimes, metastases are missed, and FTC is erroneously labeled as low-risk and treated without total thyroidectomy, I-131 ablation, or adjuvant therapy and TSH suppression, only to present years later with systemic metastases.
2.5.2. Bone Metastases
Patients with FTC are more likely to develop bony metastases than those who have PTC. The bone is the second most common site of metastases from FTC. The prognosis of patients who have bone metastases is poorer when it is compared with that of patients in whom the FTC has spread to the lungs. Additionally, bone metastasis from FTC is less sensitive to I-131. The bone metastases may be symptomatic or detected on CT, MRI, 18 FDG PET CT, SPECT/CT, or WBS using I-123, I-124, or I-131. Patients who have metastatic FTC are treated with I-131 together with TSH suppression unless the metastases are no longer iodine-avid, but FTC tends to acquire aggressive mutations as it progresses and metastases. Radioisotope-based dosimetry, although not uniformly practiced, can provide guidance on the safety and efficacy of I-131 treatment and help avoid unnecessary toxicity and treatments in patients in whom the metastases are not responding to the treatment [151]. Usually, close to 30% of patients who have metastatic FTC do not respond to I-131 [151].
2.5.3. Brain Metastasis
Brain metastases from FTC are rare and occur in less than 1% of the patients, and over 70% of the patients who have brain metastases from FTC are likely to have synchronous pulmonary metastases [28][155]. The prognosis of patients who have FTC with metastasis to the brain is poor, and the overall survival is less than 3 years even with treatment [156]. Resection for an isolated brain metastasis from FTC is preferred if it can be excised [155][157]. Severe TSH suppression should be part of the treatment of brain metastases from FTC. Treatment with I-131ne is effective if the metastases are iodine-avid and not extensive. The other options for the treatment of brain metastases from FTC include stereotactic radiosurgery, external beam radiotherapy, and multi-kinase inhibitors [28][155].
2.6. Management of De-Differentiated FTC
De-differentiation of FTC is a process that happens during tumor progression, and a de-differentiated cancer is likely to have new mutations and become aggressive and resistant to conventional therapy, such as I-131. De-differentiated FTC and PTC, PDTC, and ATC account for most of the deaths due to TC. The more prevalent mutations in de-differentiated TCs, including FTC, are BRAF, RAS, TP53, TERT promoter, and P13K/AKT/mTOR pathway effectors [96][158]. Both SPEC/CT and PET/CT are useful for evaluating the burden of metastases in cases where the tumor is no longer iodine-avid. The treatment of de-differentiated FTC is like that of PDTC and ATC and includes the use of TKIs or MTIs. Some of the de-differentiated FTCs may overexpress somatostatin receptor type 2 (SSTR2) and could be evaluated with 68Ga-DOTANOC PET/CT. Patients whose metastases demonstrate high uptake of 68Ga-DOTANOC may respond to treatment with 177Lu-Dotatate [159].
2.7. Follow-Up of Patients Who Have Follicular Carcinoma and Associated Challenges
Guidelines relating to the follow-up of FTC are often inferred from those of PTC, even though FTC forms a unique subgroup of DTC (differentiated thyroid cancer) and, therefore, requires specific considerations. A multidisciplinary approach with well-established communication channels between clinical endocrinologists and surgeons, pathologists, oncologists, radiologists, and nuclear physicians should form the backbone of the care of a patient who has FTC. Placing the patient in the center goes a long way towards improving the quality of care and eventually securing a good outcome. An important tool in achieving this is risk stratification, which consists of both. Patients who have been treated for FTC require lifelong follow-up, regardless of the initial risk level of the tumor [119]. The follow-up is intense in the first year following definitive treatment. Dynamic risk stratification, clinical evaluation, serum basal and stimulated Tg levels, and neck ultrasound are used during follow-up monitoring. Concurrent testing for the existence of Tg antibodies must be done to reduce the likelihood of falsely low levels of Tg.
The success of the management of the FTC should be determined within the first 3–6 months. Patients can be categorized as possibly cured both biochemically and anatomically, biochemically incomplete, or anatomically residual. The primary purpose of the stringent follow-up of cases of FTC is for the timeous diagnosis of persistence or local recurrence of the tumor or the appearance of new metastases. It is also critical that the de-differentiation of FTC is detected and managed early, using agents such as TKI or de-differentiation therapy to improve the chance of long-term survival [8][72][129]. The follow-up of patients on TKIs or MKIs must be regular and stringent to watch for side-effects. The most dreadful complication is bleeding, which, although rare, may be fatal [70].
It is not usual for metastases from FTC to lie dormant and unsuspected, even for tumors that are deemed low-risk clinically, pathologically, and radiologically [54][57][146][160]. Follicular thyroid carcinoma may acquire aggressive mutations as it progresses. Some of the aggressive mutations that the FTC can acquire include TP53, TERT, and PI3K/AKT/mTOR mutations [3][6][9][47][61][96][97][130][161][162].
2.8. Outcome of Treatment of Follicular Carcinoma
The outcome of patients who have FTC depends on the stage of the disease at presentation. The available staging systems for WDTC are not able to accurately predict disease-specific mortality [35]. The AJCC is the most commonly used staging system. Unfortunately, the AJCC/TNM staging on its own is not enough to direct and monitor a specific therapy. Other risk stratification systems are considered to improve the care of patients with DTC. The inclusion of intra-operative findings, histopathological changes, and genomics improves the prognostication of FTC.
References
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016, 26, 1–133.
- Lamartina, L.; Grani, G.; Durante, C.; Filetti, S. Recent advances in managing differentiated thyroid cancer. F1000Research 2018, 7.
- Bolin, J. Thyroid follicular epithelial cell–derived cancer: New approaches and treatment strategies. J. Nucl. Med. Technol. 2021, 49, 199–208.
- Katoh, H.; Yamashita, K.; Enomoto, T.; Watanabe, M. Classification and general considerations of thyroid cancer. Ann. Clin. Pathol. 2015, 3, 1045.
- Pulcrano, M.; Boukheris, H.; Talbot, M.; Caillou, B.; Dupuy, C.; Virion, A.; De Vathaire, F.; Schlumberger, M. Poorly differentiated follicular thyroid carcinoma: Prognostic factors and relevance of histological classification. Thyroid 2007, 17, 639–646.
- Romano, C.; Martorana, F.; Pennisi, M.S.; Stella, S.; Massimino, M.; Tirrò, E.; Vitale, S.R.; Di Gregorio, S.; Puma, A.; Tomarchio, C. Opportunities and challenges of liquid biopsy in thyroid cancer. Int. J. Mol. Sci. 2021, 22, 7707.
- Pozdeyev, N.; Gay, L.M.; Sokol, E.S.; Hartmaier, R.; Deaver, K.E.; Davis, S.; French, J.D.; Borre, P.V.; LaBarbera, D.V.; Tan, A.-C. Genetic analysis of 779 advanced differentiated and anaplastic thyroid cancers. Clin. Cancer Res. 2018, 24, 3059–3068.
- Ferrari, S.M.; Fallahi, P.; Politti, U.; Materazzi, G.; Baldini, E.; Ulisse, S.; Miccoli, P.; Antonelli, A. Molecular targeted therapies of aggressive thyroid cancer. Front. Endocrinol. 2015, 6, 176.
- Singh, A.; Ham, J.; Po, J.W.; Niles, N.; Roberts, T.; Lee, C.S. The genomic landscape of thyroid cancer tumourigenesis and implications for immunotherapy. Cells 2021, 10, 1082.
- Kakudo, K.; Bai, Y.; Liu, Z.; Ozaki, T. Encapsulated papillary thyroid carcinoma, follicular variant: A misnomer. Pathol. Int. 2012, 62, 155–160.
- Podda, M.; Saba, A.; Porru, F.; Reccia, I.; Pisanu, A. Follicular thyroid carcinoma: Differences in clinical relevance between minimally invasive and widely invasive tumors. World J. Surg. Oncol. 2015, 13, 1–7.
- Tallini, G.; Tuttle, R.M.; Ghossein, R.A. The History of the Follicular Variant of Papillary Thyroid Carcinoma. J. Clin. Endocrinol. Metab. 2017, 102, 15–22.
- Araque, K.A.; Gubbi, S.; Klubo-Gwiezdzinska, J. Updates on the management of thyroid cancer. Horm. Metab. Res. 2020, 52, 562–577.
- Huszno, B.; Szybiński, Z.; Przybylik-Mazurek, E.; Stachura, J.; Trofimiuk, M.; Buziak-Bereza, M.; Gołkowski, F.; Pantoflinski, J. Influence of iodine deficiency and iodine prophylaxis on thyroid cancer histotypes and incidence in endemic goiter area. J. Endocrinol. Investig. 2003, 26, 71–76.
- Nicol, F.; McLaren, K.M.; Toft, A.D. Multifocal follicular carcinoma of thyroid following radiotherapy for Hodgkin’s disease. Postgrad. Med. J. 1982, 58, 180–181.
- Ogbera, A.O.; Kuku, S.F. Epidemiology of thyroid diseases in Africa. Indian J. Endocrinol. Metab. 2011, 15, S82.
- Sáez, J.M.G. Hashimoto’s Thyroiditis and thyroid cancer. J. Hum. Endocrinol. 2016, 1.
- Deivanathan, N.; Rathinam, S.; Gopal, K.A.; Anandan, H. Incidence of Types of Thyroid Carcinoma in an Iodine-rich Area: Thoothukudi Southern Coastal City. Int. J. Sci. Study 2016, 4, 137–139.
- Zhang, W.; Ruan, X.; Li, Y.; Zhi, J.; Hu, L.; Hou, X.; Shi, X.; Wang, X.; Wang, J.; Ma, W. KDM1A promotes thyroid cancer progression and maintains stemness through the Wnt/β-catenin signaling pathway. Theranostics 2022, 12, 1500.
- Ivanova, L.B.; Vukov, M.I.; Vassileva-Valerianova, Z.G. Thyroid Cancer Incidence in Bulgaria before and after the Introduction of Universal Salt Iodization: An Analysis of the National Cancer Registry Data. Balk. Med. J. 2020, 37, 330.
- Mulaudzi, T.V.; Ramdial, P.K.; Madiba, T.E.; Callaghan, R.A. Thyroid carcinoma at King Edward VIII Hospital, Durban, South Africa. East Afr. Med. J. 2001, 78, 242–245.
- Mitro, S.D.; Rozek, L.S.; Vatanasapt, P.; Suwanrungruang, K.; Chitapanarux, I.; Srisukho, S.; Sriplung, H.; Meza, R. Iodine deficiency and thyroid cancer trends in three regions of Thailand, 1990–2009. Cancer Epidemiol. 2016, 43, 92–99.
- Shin, D.Y.; Jo, Y.S. Clinical implications of follicular and Hurthle cell carcinoma in an iodine-sufficient area. Korean J. Intern. Med. 2014, 29, 305–306.
- Zimmermann, M.B.; Galetti, V. Iodine intake as a risk factor for thyroid cancer: A comprehensive review of animal and human studies. Thyroid Res. 2015, 8, 1–21.
- Widder, S.; Guggisberg, K.; Khalil, M.; Pasieka, J.L. A pathologic re-review of follicular thyroid neoplasms: The impact of changing the threshold for the diagnosis of the follicular variant of papillary thyroid carcinoma. Surgery 2008, 144, 80–85.
- Grigsby, P.W.; Gal-or, A.; Michalski, J.M.; Doherty, G.M. Childhood and adolescent thyroid carcinoma. Cancer Interdiscip. Int. J. Am. Cancer Soc. 2002, 95, 724–729.
- Oka, K.; Shien, T.; Otsuka, F. Thyroid follicular carcinoma in a teenager: A case report. J. Gen. Fam. Med. 2018, 19, 170–172.
- Lin, J.-D.; Lin, S.-F.; Chen, S.-T.; Hsueh, C.; Li, C.-L.; Chao, T.-C. Long-term follow-up of papillary and follicular thyroid carcinomas with bone metastasis. PLoS ONE 2017, 12, e0173354.
- Parameswaran, R.; Shulin Hu, J.; Min En, N.; Tan, W.B.; Yuan, N.K. Patterns of metastasis in follicular thyroid carcinoma and the difference between early and delayed presentation. Ann. R. Coll. Surg. Engl. 2017, 99, 151–154.
- Bombil, I.; Bentley, A.; Kruger, D.; Luvhengo, T.E. Incidental cancer in multinodular goitre post thyroidectomy. South Afr. J. Surg. 2014, 52, 5–9.
- Karimifar, M. A case of functional metastatic follicular thyroid carcinoma that presented with hip fracture and hypercalcemia. Adv. Biomed. Res. 2018, 7.
- Liu, J.; Wang, Y.; Da, D.; Zheng, M. Hyperfunctioning thyroid carcinoma: A systematic review. Mol. Clin. Oncol. 2019, 11, 535–550.
- Cibas, E.S.; Ali, S.Z. The 2017 Bethesda system for reporting thyroid cytopathology. Thyroid 2017, 27, 1341–1346.
- Ustun, B.; Chhieng, D.; Prasad, M.L.; Holt, E.; Hammers, L.; Carling, T.; Udelsman, R.; Adeniran, A.J. Follicular variant of papillary thyroid carcinoma: Accuracy of FNA diagnosis and implications for patient management. Endocr. Pathol. 2014, 25, 257–264.
- Baloch, Z.W.; Asa, S.L.; Barletta, J.A.; Ghossein, R.A.; Juhlin, C.C.; Jung, C.K.; LiVolsi, V.A.; Papotti, M.G.; Sobrinho-Simoes, M.; Tallini, G. Overview of the 2022 WHO classification of thyroid neoplasms. Endocr. Pathol. 2022, 33, 27–63.
- Armanious, H.; Adam, B.; Meunier, D.; Formenti, K.; Izevbaye, I. Digital gene expression analysis might aid in the diagnosis of thyroid cancer. Curr. Oncol. 2020, 27, 93–99.
- Endo, M.; Sipos, J.A.; Ringel, M.D.; Porter, K.; Nagaraja, H.N.; Phay, J.E.; Shirley, L.A.; Long, C.; Wright, C.L.; Roll, K. Prevalence of cancer and the benign call rate of afirma gene classifier in 18F-Fluorodeoxyglucose positron emission tomography positive cytologically indeterminate thyroid nodules. Cancer Med. 2021, 10, 1084–1090.
- Kim, K.; Jung, C.K.; Lim, D.-J.; Bae, J.S.; Kim, J.S. Clinical and pathologic features for predicting malignancy in thyroid follicular neoplasms. Gland Surg. 2021, 10, 50.
- Zhao, L.; Zhu, X.-Y.; Jiang, R.; Xu, M.; Wang, N.; Chen, G.G.; Liu, Z.-M. Role of GPER1, EGFR and CXCR1 in differentiating between malignant follicular thyroid carcinoma and benign follicular thyroid adenoma. Int. J. Clin. Exp. Pathol. 2015, 8, 11236.
- Zaydfudim, V.; Feurer, I.D.; Griffin, M.R.; Phay, J.E. The impact of lymph node involvement on survival in patients with papillary and follicular thyroid carcinoma. Surgery 2008, 144, 1070–1078.
- Matsuura, D.; Yuan, A.; Harris, V.; Shaha, A.R.; Tuttle, R.M.; Patel, S.G.; Shah, J.P.; Ganly, I. Surgical management of low-/intermediate-risk node negative thyroid cancer: A single-institution study using propensity matching analysis to compare thyroid lobectomy and total thyroidectomy. Thyroid 2022, 32, 28–36.
- Schneider, D.F.; Elfenbein, D.; Lloyd, R.V.; Chen, H.; Sippel, R.S. Lymph node metastases do not impact survival in follicular variant papillary thyroid cancer. Ann. Surg. Oncol. 2015, 22, 158–163.
- Xu, B.; Farhat, N.; Barletta, J.A.; Hung, Y.P.; Biase, D.d.; Casadei, G.P.; Onenerk, A.M.; Tuttle, R.M.; Roman, B.R.; Katabi, N. Should subcentimeter non-invasive encapsulated, follicular variant of papillary thyroid carcinoma be included in the noninvasive follicular thyroid neoplasm with papillary-like nuclear features category? Endocrine 2018, 59, 143–150.
- Brecelj, E.; Grazio, S.F.; Auersperg, M.; Bračko, M. Prognostic value of E-cadherin expression in thyroid follicular carcinoma. Eur. J. Surg. Oncol. 2005, 31, 544–548.
- Dai, Y.; Miao, Y.; Zhu, Q.; Gao, M.; Hao, F. Expression of long non-coding RNA H19 predicts distant metastasis in minimally invasive follicular thyroid carcinoma. Bioengineered 2019, 10, 383–389.
- Gupta, A.; Jain, S.; Khurana, N.; Kakar, A.K. Expression of p63 and Bcl-2 in malignant thyroid tumors and their correlation with other diagnostic immunocytochemical markers. J. Clin. Diagn. Res. 2016, 10, EC04.
- Heriyanto, D.S.; Laiman, V.; Limantara, N.V.; Anantawikrama, W.P.; Yuliani, F.S.; Cempaka, R.; Anwar, S.L. High frequency of KRAS and EGFR mutation profiles in BRAF-negative thyroid carcinomas in Indonesia. BMC Res. Notes 2022, 15, 369.
- Indrasena, B.S.H. Use of thyroglobulin as a tumour marker. World J. Biol. Chem. 2017, 8, 81.
- McCaffrey, J.C. Aerodigestive tract invasion by well-differentiated thyroid carcinoma: Diagnosis, management, prognosis, and biology. Laryngoscope 2006, 116, 1–11.
- Mahmoudian-Sani, M.-R.; Jalali, A.; Jamshidi, M.; Moridi, H.; Alghasi, A.; Shojaeian, A.; Mobini, G.-R. Long non-coding RNAs in thyroid cancer: Implications for pathogenesis, diagnosis, and therapy. Oncol. Res. Treat. 2019, 42, 136–142.
- Wang, X.; Zheng, X.; Zhu, J.; Li, Z.; Wei, T. Impact of Extent of Surgery on Long-Term Prognosis of Follicular Thyroid Carcinoma Without Extrathyroidal Extension and Distant Metastasis. World J. Surg. 2022, 46, 104–111.
- Bains, A.; Mur, T.; Wallace, N.; Noordzij, J.P. The role of vitamin D as a prognostic marker in papillary thyroid cancer. Cancers 2021, 13, 3516.
- Riguetto, C.M.; Barreto, I.S.; Maia, F.F.R.; Assumpção, L.V.M.d.; Zantut-Wittmann, D.E. Usefulness of pre-thyroidectomy neutrophil–lymphocyte, platelet–lymphocyte, and monocyte–lymphocyte ratios for discriminating lymph node and distant metastases in differentiated thyroid cancer. Clinics 2021, 76.
- Fakhar, Y.; Khooei, A.; Aghaee, A.; Mohammadzadeh Kosari, H.; Wartofsky, L.; Zakavi, S.R. Bone metastasis from noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP); a case report. BMC Endocr. Disord. 2021, 21, 1–5.
- Nwaeze, O.; Obidike, S.; Mullen, D.; Aftab, F. Follicular variant papillary thyroid carcinoma with a twist. Int. J. Surg. Case Rep. 2015, 8, 107–110.
- Kammori, M.; Fukumori, T.; Sugishita, Y.; Hoshi, M.; Yamada, T. Therapeutic strategy for low-risk thyroid cancer in Kanaji Thyroid Hospital. Endocr. J. 2014, 61, 1–12.
- Omar, B.; Yassir, H.; Youssef, O.; Sami, R.; Larbi, A.R.; Mohamed, R.; Mohamed, M. A rare case of follicular thyroid carcinoma metastasis to the sacral region: A case report with literature review. Int. J. Surg. Case Rep. 2022, 94, 107001.
- Swierniak, M.; Pfeifer, A.; Stokowy, T.; Rusinek, D.; Chekan, M.; Lange, D.; Krajewska, J.; Oczko-Wojciechowska, M.; Czarniecka, A.; Jarzab, M. Somatic mutation profiling of follicular thyroid cancer by next generation sequencing. Mol. Cell. Endocrinol. 2016, 433, 130–137.
- Vaisman, F.; Momesso, D.; Bulzico, D.A.; Pessoa, C.H.C.N.; Cruz, M.D.G.d.; Dias, F.; Corbo, R.; Vaisman, M.; Tuttle, R.M. Thyroid lobectomy is associated with excellent clinical outcomes in properly selected differentiated thyroid cancer patients with primary tumors greater than 1 cm. J. Thyroid Res. 2013, 2013.
- Pignatti, E.; Vighi, E.; Magnani, E.; Kara, E.; Roncati, L.; Maiorana, A.; Santi, D.; Madeo, B.; Cioni, K.; Carani, C. Expression and clinicopathological role of miR146a in thyroid follicular carcinoma. Endocrine 2019, 64, 575–583.
- Capdevila, J.; Awada, A.; Führer-Sakel, D.; Leboulleux, S.; Pauwels, P. Molecular diagnosis and targeted treatment of advanced follicular cell-derived thyroid cancer in the precision medicine era. Cancer Treat. Rev. 2022, 102380.
- Fallahi, P.; Ferrari, S.M.; Galdiero, M.R.; Varricchi, G.; Elia, G.; Ragusa, F.; Paparo, S.R.; Benvenga, S.; Antonelli, A. Molecular targets of tyrosine kinase inhibitors in thyroid cancer. Semin. Cancer Biol. 2022, 79, 180–196.
- Aboelnaga, E.M.; Ahmed, R.A. Difference between papillary and follicular thyroid carcinoma outcomes: An experince from Egyptian institution. Cancer Biol. Med. 2015, 12, 53–59.
- Vuong, H.G.; Kondo, T.; Oishi, N.; Nakazawa, T.; Mochizuki, K.; Inoue, T.; Tahara, I.; Kasai, K.; Hirokawa, M.; Tran, T.M. Genetic alterations of differentiated thyroid carcinoma in iodine-rich and iodine-deficient countries. Cancer Med. 2016, 5, 1883–1889.
- Battoo, A.J.; Rasool, Z.; Sheikh, Z.A.; Haji, A.G. Follicular thyroid carcinoma presenting as solitary liver metastasis: A case report. J. Med. Case Rep. 2016, 10, 1–7.
- Kato, S.; Demura, S.; Shinmura, K.; Yokogawa, N.; Shimizu, T.; Tsuchiya, H. Current management of bone metastases from differentiated thyroid cancer. Cancers 2021, 13, 4429.
- Sharma, P.; Kumar, N.; Gupta, R.; Jain, S. Follicular Carcinoma of the Thyroid with Hyperthyroidism. Acta Cytol. 2004, 48, 219–222.
- Oyer, S.L.; Fritsch, V.A.; Lentsch, E.J. Comparison of survival rates between papillary and follicular thyroid carcinomas among 36,725 patients. Ann. Otol. Rhinol. Laryngol. 2014, 123, 94–100.
- Chow, S.M.; Law, S.C.K.; Au, S.K.; Leung, T.W.; Chan, P.T.M.; Mendenhall, W.M.; Lau, W.H. Differentiated thyroid carcinoma: Comparison between papillary and follicular carcinoma in a single institute. J. Sci. Spec. Head Neck 2002, 24, 670–677.
- Nicolson, N.G.; Paulsson, J.O.; Juhlin, C.C.; Carling, T.; Korah, R. Transcription factor profiling identifies spatially heterogenous mediators of follicular thyroid cancer invasion. Endocr. Pathol. 2020, 31, 367–376.
- Schmidbauer, B.; Menhart, K.; Hellwig, D.; Grosse, J. Differentiated thyroid cancer—Treatment: State of the art. Int. J. Mol. Sci. 2017, 18, 1292.
- Puliafito, I.; Esposito, F.; Prestifilippo, A.; Marchisotta, S.; Sciacca, D.; Vitale, M.P.; Giuffrida, D. Target therapy in thyroid cancer: Current challenge in clinical use of tyrosine kinase inhibitors and management of side effects. Front. Endocrinol. 2022, 13.
- Madabhushi, A.; Lee, G. Image analysis and machine learning in digital pathology: Challenges and opportunities. Med. Image Anal. 2016, 33, 170–175.
- Rudzińska, M.; Czarnocka, B. The impact of transcription factor prospero homeobox 1 on the regulation of thyroid cancer malignancy. Int. J. Mol. Sci. 2020, 21, 3220.
- Liang, P.; Wang, S.; Chen, K.B.; Li, M.; Liu, Y.; Li, S.; Pan, Y.W.; Zhang, Y.X.; Jiang, Y. The diagnosis and treatment of primary thyroid lymphoma. Chin. J. Otorhinolaryngol. Head Neck Surg. 2016, 51, 313–316.
- Badulescu, C.I.; Piciu, D.; Apostu, D.; Badan, M.; Piciu, A. Follicular thyroid carcinoma-clinical and diagnostic findings in a 20-year follow up study. Acta Endocrinol. 2020, 16, 170.
- Miasaki, F.Y.; Saito, K.C.; Yamamoto, G.L.; Boguszewski, C.L.; de Carvalho, G.A.; Kimura, E.T.; Kopp, P.A. Thyroid and Breast Cancer in 2 Sisters With Monoallelic Mutations in the Ataxia Telangiectasia Mutated (ATM) Gene. J. Endocr. Soc. 2022, 6, bvac026.
- Nosé, V. Thyroid cancer of follicular cell origin in inherited tumor syndromes. Adv. Anat. Pathol. 2010, 17, 428–436.
- Howell, G.M.; Hodak, S.P.; Yip, L. RAS mutations in thyroid cancer. Oncology 2013, 18, 926–932.
- Motoi, N.; Sakamoto, A.; Yamochi, T.; Horiuchi, H.; Motoi, T.; Machinami, R. Role of ras mutation in the progression of thyroid carcinoma of follicular epithelial origin. Pathol. Res. Pract. 2000, 196, 1–7.
- Bhuiyan, M.; Machowski, A. Nodular thyroid disease and thyroid malignancy: Experience at Polokwane Mankweng Hospital Complex, Limpopo Province, South Africa. South Afr. Med. J. 2015, 105, 570–572.
- Trovato, M.; Campennì, A.; Giovinazzo, S.; Siracusa, M.; Ruggeri, R.M. Hepatocyte growth factor/C-met axis in thyroid cancer: From diagnostic biomarker to therapeutic target. Biomark. Insights 2017, 12, 1177271917701126.
- Livolsi, V.A.; Asa, S.L. The demise of follicular carcinoma of the thyroid gland. Thyroid 1994, 4, 233–236.
- Cipriani, N.A.; Nagar, S.; Kaplan, S.P.; White, M.G.; Antic, T.; Sadow, P.M.; Aschebrook-Kilfoy, B.; Angelos, P.; Kaplan, E.L.; Grogan, R.H. Follicular thyroid carcinoma: How have histologic diagnoses changed in the last half-century and what are the prognostic implications? Thyroid 2015, 25, 1209–1216.
- De Crea, C.; Raffaelli, M.; Sessa, L.; Ronti, S.; Fadda, G.; Bellantone, C.; Lombardi, C.P. Actual incidence and clinical behaviour of follicular thyroid carcinoma: An institutional experience. Sci. World J. 2014, 2014.
- DeMay, R.M. Follicular Lesions of the Thyroid: W(h)ither Follicular Carcinoma? Am. J. Clin. Pathol. 2000, 114, 681–683.
- Lee, S.R.; Jung, C.K.; Kim, T.E.; Bae, J.S.; Jung, S.L.; Choi, Y.J.; Kang, C.S. Molecular genotyping of follicular variant of papillary thyroid carcinoma correlates with diagnostic category of fine-needle aspiration cytology: Values of RAS mutation testing. Thyroid 2013, 23, 1416–1422.
- Kapur, U.; Wojcik, E.M. Follicular neoplasm of the thyroid—Vanishing cytologic diagnosis? Diagn. Cytopathol. 2007, 35, 525–528.
- Ahmadi, S.; Stang, M.; Jiang, X.S.; Sosa, J.A. Hürthle cell carcinoma: Current perspectives. OncoTargets Ther. 2016, 6873–6884.
- Lau, L.W.; Ghaznavi, S.; Frolkis, A.D.; Stephenson, A.; Robertson, H.L.; Rabi, D.M.; Paschke, R. Malignancy risk of hyperfunctioning thyroid nodules compared with non-toxic nodules: Systematic review and a meta-analysis. Thyroid Res. 2021, 14, 1–16.
- Saito, F.; Uruno, T.; Shibuya, H.; Kitagawa, W.; Nagahama, M.; Sugino, K.; Ito, K. Prognosis After Brain Metastasis from Differentiated Thyroid Carcinoma. World J. Surg. 2016, 40, 574–581.
- Sugino, K.; Kameyama, K.; Nagahama, M.; Kitagawa, W.; Shibuya, H.; Ohkuwa, K.; Uruno, T.; Akaishi, J.; Suzuki, A.; Masaki, C. Follicular thyroid carcinoma with distant metastasis: Outcome and prognostic factor. Endocr. J. 2014, 61, 273–279.
- Tang, J.; Kong, D.; Cui, Q.; Wang, K.; Zhang, D.; Liao, X.; Gong, Y.; Wu, G. Racial disparities of differentiated thyroid carcinoma: Clinical behavior, treatments, and long-term outcomes. World J. Surg. Oncol. 2018, 16, 1–9.
- Abe, I.; Lam, A.K. Anaplastic thyroid carcinoma: Updates on WHO classification, clinicopathological features and staging. Histol Histopathol 2021, 36, 239–248.
- Bible, K.C.; Kebebew, E.; Brierley, J.; Brito, J.P.; Cabanillas, M.E.; Clark Jr, T.J.; Di Cristofano, A.; Foote, R.; Giordano, T.; Kasperbauer, J. 2021 American thyroid association guidelines for management of patients with anaplastic thyroid cancer: American thyroid association anaplastic thyroid cancer guidelines task force. Thyroid 2021, 31, 337–386.
- Feldkamp, J. The role of genetic alterations in thyroid carcinoma. Front. Endocrinol. 2022, 13.
- Landa, I.; Ibrahimpasic, T.; Boucai, L.; Sinha, R.; Knauf, J.A.; Shah, R.H.; Dogan, S.; Ricarte-Filho, J.C.; Krishnamoorthy, G.P.; Xu, B. Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J. Clin. Investig. 2016, 126, 1052–1066.
- Penna, G.C.; Vaisman, F.; Vaisman, M.; Sobrinho-Simões, M.; Soares, P. Molecular markers involved in tumorigenesis of thyroid carcinoma: Focus on aggressive histotypes. Cytogenet. Genome Res. 2016, 150, 194–207.
- Kostoglou-Athanassiou, I.; Athanassiou, P.; Vecchini, G.; Gogou, L.; Kaldrymides, P. Mixed medullary-follicular thyroid carcinoma. Horm. Res. Paediatr. 2004, 61, 300–304.
- Tohidi, M.; Pourbehi, G.; Bahmanyar, M.; Eghbali, S.S.; Kalantar Hormozi, M.; Nabipour, I. Mixed medullary-follicular carcinoma of the thyroid. Case Rep. Endocrinol. 2013, 2013.
- Grani, G.; Lamartina, L.; Durante, C.; Filetti, S.; Cooper, D.S. Follicular thyroid cancer and Hürthle cell carcinoma: Challenges in diagnosis, treatment, and clinical management. Lancet Diabetes Endocrinol. 2018, 6, 500–514.
- Nabhan, F.; Ringel, M.D. Thyroid nodules and cancer management guidelines: Comparisons and controversies. Endocr. Relat. Cancer 2017, 24, R13.
- Ashamallah, G.A.; El-Adalany, M.A. Risk for malignancy of thyroid nodules: Comparative study between TIRADS and US based classification system. Egypt. J. Radiol. Nucl. Med. 2016, 47, 1373–1384.
- Kwak, J.Y.; Han, K.H.; Yoon, J.H.; Moon, H.J.; Son, E.J.; Park, S.H.; Jung, H.K.; Choi, J.S.; Kim, B.M.; Kim, E.-K. Thyroid imaging reporting and data system for US features of nodules: A step in establishing better stratification of cancer risk. Radiology 2011, 260, 892–899.
- Kuo, T.-C.; Wu, M.-H.; Chen, K.-Y.; Hsieh, M.-S.; Chen, A.; Chen, C.-N. Ultrasonographic features for differentiating follicular thyroid carcinoma and follicular adenoma. Asian J. Surg. 2020, 43, 339–346.
- Fernández Sánchez, J. TI-RADS classification of thyroid nodules based on a score modified regarding the ultrasound criteria for malignancy. Rev. Argent. De Radiol. 2014, 78, 138–148.
- Li, M.; Wei, L.; Li, F.; Kan, Y.; Liang, X.; Zhang, H.; Liu, J. High Risk Thyroid Nodule Discrimination and Management by Modified TI-RADS. Cancer Manag. Res. 2021, 225–234.
- Mistry, R.; Hillyar, C.R.; Nibber, A.; Sooriyamoorthy, T.; Kumar, N.; Hillyar, C. Ultrasound classification of thyroid nodules: A systematic review. Cureus J. Med. Sci. 2020, 12.
- Qiao, J.; Li, C.; Zhang, Y.; Wang, S.; Gao, S. HBME-1 expression in differentiated thyroid carcinoma and its correlation with the ultrasonic manifestation of thyroid. Oncol. Lett. 2017, 14, 6505–6510.
- Spinelli, C.; Rallo, L.; Morganti, R.; Mazzotti, V.; Inserra, A.; Cecchetto, G.; Massimino, M.; Collini, P.; Strambi, S. Surgical management of follicular thyroid carcinoma in children and adolescents: A study of 30 cases. J. Pediatr. Surg. 2019, 54, 521–526.
- Cibas, E.S.; Ali, S.Z. The Bethesda system for reporting thyroid cytopathology. Thyroid 2009, 19, 1159–1165.
- Misiakos, E.P.; Margari, N.; Meristoudis, C.; Machairas, N.; Schizas, D.; Petropoulos, K.; Spathis, A.; Karakitsos, P.; Machairas, A. Cytopathologic diagnosis of fine needle aspiration biopsies of thyroid nodules. World J. Clin. Cases 2016, 4, 38.
- Elsherbini, N.; Kim, D.H.; Payne, R.J.; Hudson, T.; Forest, V.-I.; Hier, M.P.; Payne, A.E.; Pusztaszeri, M.P. EIF1AX mutation in thyroid tumors: A retrospective analysis of cytology, histopathology and co-mutation profiles. J. Otolaryngol. Head Neck Surg. 2022, 51, 1–9.
- Dom, G.; Frank, S.; Floor, S.; Kehagias, P.; Libert, F.; Hoang, C.; Andry, G.; Spinette, A.; Craciun, L.; de Saint Aubin, N. Thyroid follicular adenomas and carcinomas: Molecular profiling provides evidence for a continuous evolution. Oncotarget 2018, 9, 10343.
- Sobrinho-Simoes, M.; Eloy, C.; Magalhaes, J.; Lobo, C.; Amaro, T. Follicular thyroid carcinoma. Mod. Pathol. 2011, 24, S10–S18.
- Filetti, S.; Durante, C.; Hartl, D.; Leboulleux, S.; Locati, L.D.; Newbold, K.; Papotti, M.G.; Berruti, A. Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2019, 30, 1856–1883.
- McLeod, D.S.; Jonklaas, J.; Brierley, J.D.; Ain, K.B.; Cooper, D.S.; Fein, H.G.; Haugen, B.R.; Ladenson, P.W.; Magner, J.; Ross, D.S.; et al. Reassessing the NTCTCS Staging Systems for Differentiated Thyroid Cancer, Including Age at Diagnosis. Thyroid 2015, 25, 1097–1105.
- Glikson, E.; Alon, E.; Bedrin, L.; Talmi, Y.P. Prognostic Factors in Differentiated Thyroid Cancer Revisited. Isr. Med. Assoc. J. 2017, 19, 114–118.
- Jung, C.K.; Bychkov, A.; Kakudo, K. Update from the 2022 world health organization classification of thyroid tumors: A standardized diagnostic approach. Endocrinol. Metab. 2022, 37, 703–718.
- Papaleontiou, M.; Haymart, M.R. New insights in risk stratification of differentiated thyroid cancer. Curr. Opin. Oncol. 2014, 26, 1.
- Shaha, A.R.; Tuttle, R.M. Thyroid cancer staging and genomics. Ann. Transl. Med. 2019, 7.
- Vaisman, F.; Corbo, R.; Vaisman, M. Thyroid carcinoma in children and adolescents—Systematic review of the literature. J. Thyroid Res. 2011, 2011.
- Naoum, G.E.; Morkos, M.; Kim, B.; Arafat, W. Novel targeted therapies and immunotherapy for advanced thyroid cancers. Mol. Cancer 2018, 17, 1–15.
- Teo, K.W.; Yuan, N.K.; Tan, W.B.; Parameswaran, R. Comparison of prognostic scoring systems in follicular thyroid cancer. Ann. R. Coll. Surg. Engl. 2017, 99, 479–484.
- Nabhan, F.; Dedhia, P.H.; Ringel, M.D. Thyroid cancer, recent advances in diagnosis and therapy. Int. J. Cancer 2021, 149, 984–992.
- Lee, S.L. Complications of radioactive iodine treatment of thyroid carcinoma. J. Natl. Compr. Cancer Netw. 2010, 8, 1277–1287.
- van Velsen, E.F.S.; Stegenga, M.T.; van Kemenade, F.J.; Kam, B.L.R.; van Ginhoven, T.M.; Visser, W.E.; Peeters, R.P. Comparing the prognostic value of the eighth edition of the American Joint Committee on cancer/tumor node metastasis staging system between papillary and follicular thyroid cancer. Thyroid 2018, 28, 976–981.
- Megwalu, U.C.; Green, R.W. Total Thyroidectomy Versus Lobectomy for the Treatment of Follicular Thyroid Microcarcinoma. Anticancer Res 2016, 36, 2899–2902.
- Coelho, S.M.; Vaisman, F.; Buescu, A.; Mello, R.C.R.; Carvalho, D.P.; Vaisman, M. Follow-up of patients treated with retinoic acid for the control of radioiodine non-responsive advanced thyroid carcinoma. Braz. J. Med. Biol. Res. 2011, 44, 73–77.
- Lorusso, L.; Cappagli, V.; Valerio, L.; Giani, C.; Viola, D.; Puleo, L.; Gambale, C.; Minaldi, E.; Campopiano, M.C.; Matrone, A. Thyroid cancers: From surgery to current and future systemic therapies through their molecular identities. Int. J. Mol. Sci. 2021, 22, 3117.
- Poma, A.M.; Giannini, R.; Piaggi, P.; Ugolini, C.; Materazzi, G.; Miccoli, P.; Vitti, P.; Basolo, F. A six-gene panel to label follicular adenoma, low-and high-risk follicular thyroid carcinoma. Endocr. Connect. 2018, 7, 124.
- Tong, G.-X.; Mody, K.; Wang, Z.; Hamele-Bena, D.; Nikiforova, M.N.; Nikiforov, Y.E. Mutations of TSHR and TP53 genes in an aggressive clear cell follicular carcinoma of the thyroid. Endocr. Pathol. 2015, 26, 315–319.
- Iizuka, Y.; Katagiri, T.; Ogura, K.; Inoue, M.; Nakamura, K.; Mizowaki, T. Comparison of thyroid hormone withdrawal and recombinant human thyroid-stimulating hormone administration for adjuvant therapy in patients with intermediate-to high-risk differentiated thyroid cancer. Ann. Nucl. Med. 2020, 34, 736–741.
- Ciarallo, A.; Rivera, J. Radioactive iodine therapy in differentiated thyroid cancer: 2020 update. Am. J. Roentgenol. 2020, 215, 285–291.
- Silaghi, H.; Lozovanu, V.; Georgescu, C.E.; Pop, C.; Nasui, B.A.; Cătoi, A.F.; Silaghi, C.A. State of the art in the current management and future directions of targeted therapy for differentiated thyroid cancer. Int. J. Mol. Sci. 2022, 23, 3470.
- Corrêa, N.L.; de Sá, L.V.; de Mello, R.C.R. Estimation of second primary cancer risk after treatment with radioactive iodine for differentiated thyroid carcinoma. Thyroid 2017, 27, 261–270.
- Fard-Esfahani, A.; Emami-Ardekani, A.; Fallahi, B.; Fard-Esfahani, P.; Beiki, D.; Hassanzadeh-Rad, A.; Eftekhari, M. Adverse effects of radioactive iodine-131 treatment for differentiated thyroid carcinoma. Nucl. Med. Commun. 2014, 35, 808–817.
- Chmielik, E.; Rusinek, D.; Oczko-Wojciechowska, M.; Jarzab, M.; Krajewska, J.; Czarniecka, A.; Jarzab, B. Heterogeneity of thyroid cancer. Pathobiology 2018, 85, 117–129.
- Masui, T.; Uemura, H.; Ota, I.; Kimura, T.; Nishikawa, D.; Yamanaka, T.; Yane, K.; Kitahara, T. A study of 17 cases for the identification of prognostic factors for anaplastic thyroid carcinoma. Mol. Clin. Oncol. 2021, 14, 1.
- Saji, M.; Ringel, M.D. The PI3K-Akt-mTOR pathway in initiation and progression of thyroid tumors. Mol. Cell. Endocrinol. 2010, 321, 20–28.
- Zampella, E.; Klain, M.; Pace, L.; Cuocolo, A. PET/CT in the management of differentiated thyroid cancer. Diagn. Interv. Imaging 2021, 102, 515–523.
- Batrinos, M.L. The problem of exogenous subclinical hyperthyroidism. Horm. Athens 2006, 5, 119.
- Yavuz, D.G.; Yazan, C.D.; Hekimsoy, Z.; Aydin, K.; Gokkaya, N.; Ersoy, C.; Akalın, A.; Topaloglu, O.; Aydogan, B.I.; Dilekci, E.N.A. Assesment of attainment of recommended TSH levels and levothyroxine compliance in differentiated thyroid cancer patients. Clin. Endocrinol. 2022, 97, 833–840.
- Bartalena, L.; Pinchera, A. Effects of thyroxine excess on peripheral organs. Acta Med. Austriaca 1994, 21, 60–65.
- Yang, X.; Guo, N.; Gao, X.; Liang, J.; Fan, X.; Zhao, Y. Meta-analysis of TSH suppression therapy and the risk of cardiovascular events after thyroid cancer surgery. Front. Endocrinol. 2022, 13.
- Miccoli, P.; Materazzi, G.; Rossi, L. Levothyroxine therapy in thyrodectomized patients. Front. Endocrinol. 2021, 11, 626268.
- Rajan, N.; Khanal, T.; Ringel, M.D. Progression and dormancy in metastatic thyroid cancer: Concepts and clinical implications. Endocrine 2020, 70, 24–35.
- Brauckhoff, M. Classification of aerodigestive tract invasion from thyroid cancer. Langenbeck’s Arch. Surg. 2014, 399, 209–216.
- Wu, H.-S.; Young, M.T.; Ituarte, P.H.G.; D’Avanzo, A.; Duh, Q.-Y.; Greenspan, F.S.; Loh, K.C.; Clark, O.H. Death from thyroid cancer of follicular cell origin. J. Am. Coll. Surg. 2000, 191, 600–606.
- Allen, M.; Spillinger, A.; Arianpour, K.; Johnson, J.; Johnson, A.P.; Folbe, A.J.; Hotaling, J.; Svider, P.F. Tracheal Resection in the Management of Thyroid Cancer: An Evidence-Based Approach. Laryngoscope 2021, 131, 932–946.
- Chen, W.-C.; Chou, C.-K.; Chang, Y.-H.; Chiang, P.-L.; Lim, L.-S.; Chi, S.-Y.; Luo, S.-D.; Lin, W.-C. Efficacy of radiofrequency ablation for metastatic papillary thyroid cancer with and without initial biochemical complete status. Front. Endocrinol. 2022, 13.
- Ohkuwa, K.; Sugino, K.; Nagahama, M.; Kitagawa, W.; Matsuzu, K.; Suzuki, A.; Tomoda, C.; Hames, K.; Akaishi, J.; Masaki, C. Risk stratification in differentiated thyroid cancer with RAI-avid lung metastases. Endocr. Connect. 2021, 10, 825.
- Papanikolaou, V.; Kyrodimos, E.; Mastronikolis, N.; Asimakopoulos, A.D.; Papanastasiou, G.; Tsiambas, E.; Spyropoulou, D.; Katsinis, S.; Manoli, A.; Papouliakos, S. Anti-EGFR/BRAF-Tyrosine Kinase Inhibitors in Thyroid Carcinoma. Cancer Diagn. Progn. 2023, 3, 151.
- Broecker-Preuss, M.; Müller, S.; Britten, M.; Worm, K.; Schmid, K.W.; Mann, K.; Fuhrer, D. Sorafenib inhibits intracellular signaling pathways and induces cell cycle arrest and cell death in thyroid carcinoma cells irrespective of histological origin or BRAF mutational status. BMC Cancer 2015, 15, 1–13.
- Kiyota, N.; Robinson, B.; Shah, M.; Hoff, A.O.; Taylor, M.H.; Li, D.; Dutcus, C.E.; Lee, E.K.; Kim, S.-B.; Tahara, M. Defining radioiodine-refractory differentiated thyroid cancer: Efficacy and safety of lenvatinib by radioiodine-refractory criteria in the SELECT trial. Thyroid 2017, 27, 1135–1141.
- Hong, Y.-W.; Lin, J.-D.; Yu, M.-C.; Hsu, C.-C.; Lin, Y.-S. Outcomes and prognostic factors in thyroid cancer patients with cranial metastases: A retrospective cohort study of 4,683 patients. Int. J. Surg. 2018, 55, 182–187.
- Slutzky-Shraga, I.; Gorshtein, A.; Popovitzer, A.; Robenshtok, E.; Tsvetov, G.; Akirov, A.; Hirsch, D.; Benbassat, C. Clinical characteristics and disease outcome of patients with non-medullary thyroid cancer and brain metastases. Oncol. Lett. 2018, 15, 672–676.
- Choi, J.; Kim, J.W.; Keum, Y.S.; Lee, I.J. The largest known survival analysis of patients with brain metastasis from thyroid cancer based on prognostic groups. PLoS ONE 2016, 11, e0154739.
- Wong, K.; Di Cristofano, F.; Ranieri, M.; De Martino, D.; Di Cristofano, A. PI3K/mTOR inhibition potentiates and extends palbociclib activity in anaplastic thyroid cancer. Endocr. Relat. Cancer 2019, 26, 425.
- Thakur, S.; Daley, B.; Millo, C.; Cochran, C.; Jacobson, O.; Lu, H.; Wang, Z.; Kiesewetter, D.; Chen, X.; Vasko, V. 177Lu-DOTA-EB-TATE, a Radiolabeled Analogue of Somatostatin Receptor Type 2, for the Imaging and Treatment of Thyroid CancerRadiolabeled Somatostatin Analogues and Thyroid Cancer. Clin. Cancer Res. 2021, 27, 1399–1409.
- Panda, S.K.; Patro, B.; Samantaroy, M.R.; Mishra, J.; Mohapatra, K.C.; Meher, R.K. Unusual presentation of follicular carcinoma thyroid with special emphasis on their management. Int. J. Surg. Case Rep. 2014, 5, 408–411.
- Prete, A.; Borges de Souza, P.; Censi, S.; Muzza, N.N.; Sponziello, M. Update on fundamental mechanisms of thyroid cancer. Front. Endocrinol. 2020, 11, 102.
More
Information
Subjects:
Oncology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
880
Revisions:
2 times
(View History)
Update Date:
05 May 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




