
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Kushal Chakraborty | -- | 3716 | 2023-04-29 09:10:51 | | | |
| 2 | Lindsay Dong | Meta information modification | 3716 | 2023-05-03 04:30:24 | | |
Video Upload Options
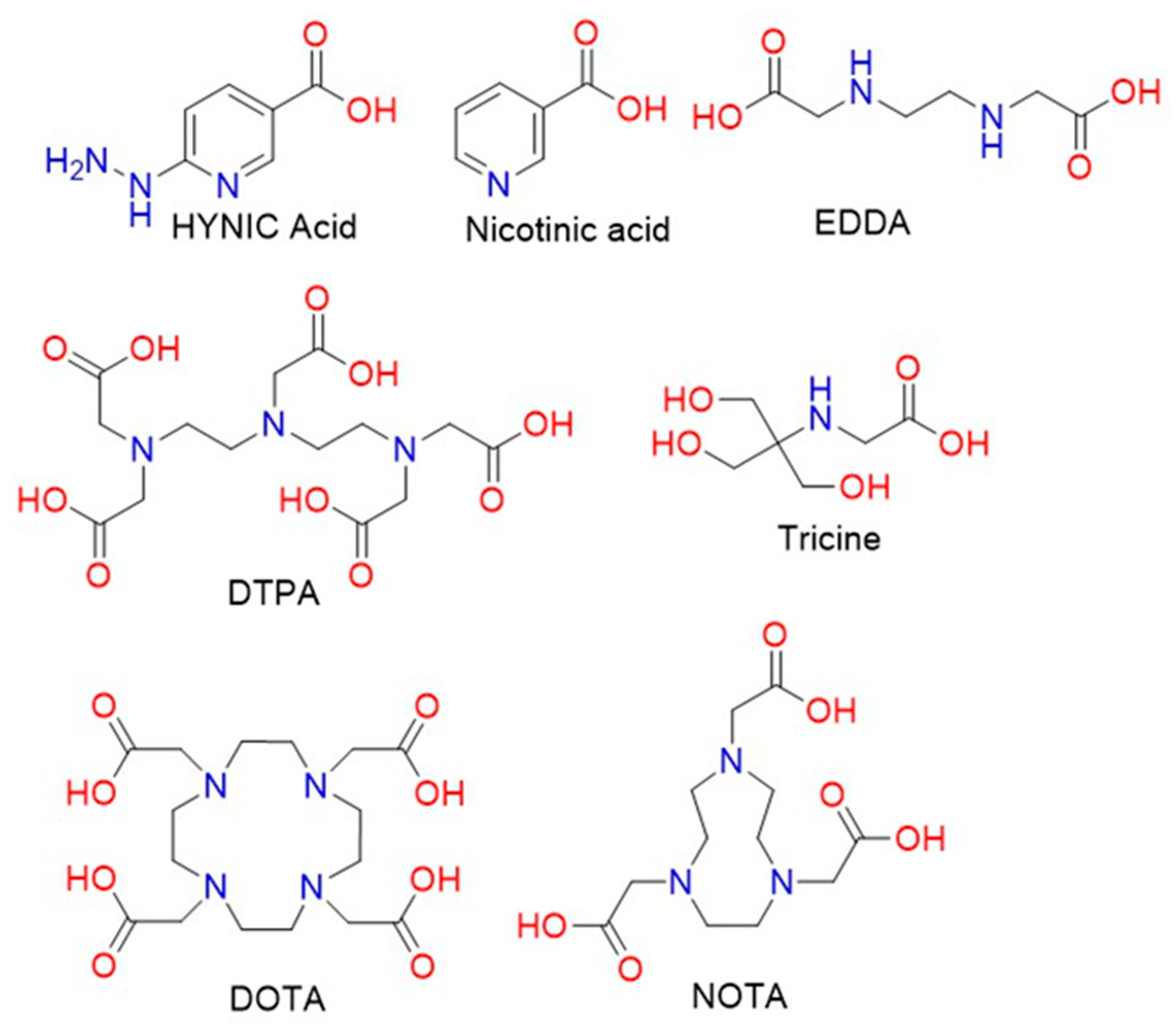
Radiopharmaceutical therapy, which can detect and treat tumours simultaneously, was introduced more than 80 years ago, and it has changed medical strategies with respect to cancer. Many radioactive radionuclides have been developed, and functional, molecularly modified radiolabelled peptides have been used to produce biomolecules and therapeutics that are vastly utilised in the field of radio medicine. Advanced technologies, such as conjugation of functional peptides or incorporation of radionuclides into chelating ligands, have been developed for advanced radiopharmaceutical cancer therapy. New radiolabelled conjugates for targeted radiotherapy have been designed to deliver radiation directly to cancer cells with improved specificity and minimal damage to the surrounding normal tissue. The development of new theragnostic radionuclides, which can be used for both imaging and therapy purposes, allows for more precise targeting and monitoring of the treatment response. The increased use of peptide receptor radionuclide therapy (PRRT) is also important in the targeting of specific receptors which are overexpressed in cancer cells.
1. Introduction
2. Various Radionuclides for Theragnosis
3. Radiopharmaceuticals with Radiolabelled Peptides towards Cancer Therapy: Mechanistic Pathway and Biological Paraphernalia
3.1. Radiation Dosimetry
3.2. Localization Pathways
4. Fabrication of Amino Chains for Radiopharmaceutical Applications
5. Radiolabelled Peptides Used in Cancer Theragnosis
5.1. Somatostatin Receptor-Targeted Anticancer Therapy
5.2. CD13-Targeted Anticancer Therapy
6. Radiolabelled Peptides Translated into Clinical Trials
Metastatic, castration-resistant prostate cancer is one of the most challenging curable diseases. Since castration-resistant prostate cancer does not respond to hormone therapy, there is an urgent need to develop a therapeutic agent that targets this type of cancer [87]. Recently, specific proteins, such as SWI/SNF, which are overexpressed in castration-resistant prostate cancer have been discovered [88]. Prostate-specific membrane antigen (PSMA) is also one of the proteins that is highly expressed in metastatic, castration-resistant prostate cancer [89]. In the clinical trial for the curing of this disease, 177Lu-PSMA-617 was investigated as a radioligand therapy that could deliver beta-particle radiation to PSMA-expressing cells and the surrounding microenvironment (NCT03511664) [89]. Oliver et al. evaluated the theragnostic efficacy of 177Lu-PSMA-617 through an international, open-label, phase 3 trial involving patients previously treated for metastatic, castration-resistant prostate cancer. The patients had undergone treatment of not only one androgen receptor pathway inhibitor, but also of one or two taxane regimens. Furthermore, PET-CT-scanned patients who used PSMA-positive gallium-68 (68Ga)-labelled PSMA-11 also participated. In the clinical trials, one group of patients additionally received 177Lu-PSMA-617 treatment (7.4 GBq every six weeks for four to six cycles) as they were provided with protocol-permitted standard care that excluded radium-223 (223Ra). The other group of patients only received standard care. The endpoints were determined based on bioimaging of the patients or the objective responses. The side effects that occurred during the clinical trial were limited to those that occurred within 30 days of the last administration of 177Lu-PSMA-617 and those that occurred before the subsequent anticancer treatment. According to the imaging-based results for progression-free survival and overall survival, 177Lu-PSMA-617 plus standard care led to significant improvement as compared with standard care alone (in the case of imaging-based progression-free survival, median was 8.7 vs. 3.4 months; hazard ratio for progression or death, 0.40; 99.2% confidence interval, 0.29 to 0.57; p < 0.001; in the case of survival, median was 15.3 vs. 11.3 months; hazard ratio for death, 0.62; 95% CI, 0.52 to 0.74; p < 0.001). However, the incidence of adverse events of grade 3 and above was higher with the administration of 177Lu-PSMA-617 (52.7%) than without (38.0%). Fortunately, the adverse events that occurred did not cause negative effects such as a reduction in the quality of life of the patients. Therefore, standard care plus radioligand therapy with 177Lu -PSMA-617 as a combination therapy significantly prolonged the imaging-based progression-free survival and overall survival of patients with PSMA-positive, metastatic, castration-resistant prostate cancer.
References
- Simón, M.; Jørgensen, J.T.; Khare, H.A.; Christensen, C.; Nielsen, C.H.; Kjaer, A. Combination of Lu-DOTA-TATE Targeted Radionuclide Therapy and Photothermal Therapy as a Promising Approach for Cancer Treatment: In Vivo Studies in a Human Xenograft Mouse Model. Pharmaceutics 2022, 14, 1284.
- Frantellizzi, V.; Verrina, V.; Raso, C.; Pontico, M.; Petronella, F.; Bertana, V.; Ballesio, A.; Marasso, S.L.; Miglietta, S.; Rosa, P.; et al. 99mTc-Labeled Keratin Gold-Nanoparticles in a Nephron-like Microfluidic Chip for Photo-Thermal Therapy Applications. Mater. Today Adv. 2022, 16, 100286.
- Cheng, M.H.Y.; Overchuk, M.; Rajora, M.A.; Lou, J.W.H.; Chen, Y.; Pomper, M.G.; Chen, J.; Zheng, G. Targeted Theranostic 111 In/Lu-Nanotexaphyrin for SPECT Imaging and Photodynamic Therapy. Mol. Pharm. 2022, 19, 1803–1813.
- Kumar, D.S.; Girija, A.R. Bionanotechnology in Cancer; Jenny Stanford Publishing: New York, NY, USA, 2022; ISBN 9780429422911.
- Ferreira, C.A.; Heidari, P.; Ataeinia, B.; Sinevici, N.; Sise, M.E.; Colvin, R.B.; Wehrenberg-Klee, E.; Mahmood, U. Non-Invasive Detection of Immunotherapy-Induced Adverse Events. Clin. Cancer Res. 2021, 27, 5353–5364.
- Luo, Q.; Zhang, Y.; Wang, Z.; Sun, Y.; Shi, L.; Yu, Y.; Shi, J.; Hu, Z.; Wang, F. A Novel Peptide-Based Probe 99mTc-PEG6-RD-PDP2 for the Molecular Imaging of Tumor PD-L2 Expression. Chin. Chem. Lett. 2022, 33, 3497–3501.
- Wen, X.; Zeng, X.; Liu, J.; Zhang, Y.; Shi, C.; Wu, X.; Zhuang, R.; Chen, X.; Zhang, X.; Guo, Z. Synergism of 64 Cu-Labeled RGD with Anti-PD-L1 Immunotherapy for the Long-Acting Antitumor Effect. Bioconjug. Chem. 2022, 33, 2170–2179.
- He, Z.; Jia, H.; Zheng, M.; Wang, H.; Yang, W.; Gao, L.; Zhang, Z.; Xue, J.; Xu, B.; Yang, W.; et al. Trp2 Peptide-Assembled Nanoparticles with Intrinsically Self-Chelating 64 Cu Properties for PET Imaging Tracking and Dendritic Cell-Based Immunotherapy against Melanoma. ACS Appl. Bio Mater. 2021, 4, 5707–5716.
- Wang, C.; Tian, Y.; Wu, B.; Cheng, W. Recent Progress Toward Imaging Application of Multifunction Sonosensitizers in Sonodynamic Therapy. Int. J. Nanomed. 2022, 17, 3511–3529.
- Dhaini, B.; Kenzhebayeva, B.; Ben-Mihoub, A.; Gries, M.; Acherar, S.; Baros, F.; Thomas, N.; Daouk, J.; Schohn, H.; Hamieh, T.; et al. Peptide-Conjugated Nanoparticles for Targeted Photodynamic Therapy. Nanophotonics 2021, 10, 3089–3134.
- Wang, H.; Wang, Z.; Chen, W.; Wang, W.; Shi, W.; Chen, J.; Hang, Y.; Song, J.; Xiao, X.; Dai, Z. Self-Assembly of Photosensitive and Radiotherapeutic Peptide for Combined Photodynamic-Radio Cancer Therapy with Intracellular Delivery of MiRNA-139-5p. Bioorg. Med. Chem. 2021, 44, 116305.
- Ho, J.A.; Wang, L.-S.; Chuang, M.-C. Nanotheranostics—A Review of Recent Publications. Int. J. Nanomed. 2012, 7, 4679–4695.
- Pan, T.; Mawlawi, O. PET/CT in Radiation Oncology. Med. Phys. 2008, 35, 4955–4966.
- Guerra Liberal, F.D.C.; Tavares, A.A.S.; Tavares, J.M.R.S. Palliative Treatment of Metastatic Bone Pain with Radiopharmaceuticals: A Perspective beyond Strontium-89 and Samarium-153. Appl. Radiat. Isot. 2016, 110, 87–99.
- Manzzini Calegaro, J.U.; de Podestá Haje, D.; Machado, J.; Sayago, M.; de Landa, D.C. Synovectomy Using Samarium-153 Hydroxyapatite in the Elbows and Ankles of Patients with Hemophilic Arthropathy. World J. Nucl. Med. 2018, 17, 6–11.
- Kolesnikov-Gauthier, H.; Lemoine, N.; Tresch-Bruneel, E.; Olivier, A.; Oudoux, A.; Penel, N. Efficacy and Safety of 153Sm-EDTMP as Treatment of Painful Bone Metastasis: A Large Single-Center Study. Support. Care Cancer 2018, 26, 751–758.
- Ma, H.; Li, F.; Shen, G.; Cai, H.; Liu, W.; Lan, T.; Yang, Y.; Yang, J.; Liao, J.; Liu, N. Synthesis and Preliminary Evaluation of 131 I-Labeled FAPI Tracers for Cancer Theranostics. Mol. Pharm. 2021, 18, 4179–4187.
- Giannakenas, C.; Kalofonos, H.P.; Apostolopoulos, D.J.; Zarakovitis, J.; Kosmas, C.; Vassilakos, P.J. Preliminary Results of the Use of Re-186-HEDP for Palliation of Pain in Patients with Metastatic Bone Disease. Am. J. Clin. Oncol. Cancer Clin. Trials 2000, 23, 83–88.
- Klett, R.; Lange, U.; Haas, H.; Voth, M.; Pinkert, J. Radiosynoviorthesis of Medium-Sized Joints with Rhenium-186-Sulphide Colloid: A Review of the Literature. Rheumatology 2007, 46, 1531–1537.
- Hertz, S. Radioactive Iodine in the Study of Thyroid Physiology. J. Am. Med. Assoc. 1946, 131, 81.
- Herrero Álvarez, N.; Bauer, D.; Hernández-Gil, J.; Lewis, J.S. Recent Advances in Radiometals for Combined Imaging and Therapy in Cancer. ChemMedChem 2021, 16, 2909–2941.
- Roll, W.; Weckesser, M.; Seifert, R.; Bodei, L.; Rahbar, K. Imaging and Liquid Biopsy in the Prediction and Evaluation of Response to PRRT in Neuroendocrine Tumors: Implications for Patient Management. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 4016–4027.
- Ambrosini, V.; Kunikowska, J.; Baudin, E.; Bodei, L.; Bouvier, C.; Capdevila, J.; Cremonesi, M.; de Herder, W.W.; Dromain, C.; Falconi, M.; et al. Consensus on Molecular Imaging and Theranostics in Neuroendocrine Neoplasms. Eur. J. Cancer 2021, 146, 56–73.
- Werner, R.A.; Solnes, L.B.; Javadi, M.S.; Weich, A.; Gorin, M.A.; Pienta, K.J.; Higuchi, T.; Buck, A.K.; Pomper, M.G.; Rowe, S.P.; et al. SSTR-RADS Version 1.0 as a Reporting System for SSTR PET Imaging and Selection of Potential PRRT Candidates: A Proposed Standardization Framework. J. Nucl. Med. 2018, 59, 1085–1091.
- Parghane, R.; Mitra, A.; Bannore, T.; Rakshit, S.; Banerjee, S.; Basu, S. Initial Clinical Evaluation of Indigenous 90Y-DOTATATE in Sequential Duo-PRRT Approach (177Lu-DOTATATE and 90Y-DOTATATE) in Neuroendocrine Tumors with Large Bulky Disease: Observation on Tolerability,90Y-DOTATATE Post- PRRT Imaging Characteristics (bremsstrahlung and PETCT) and early adverse effects. World J. Nucl. Med. 2021, 20, 73–81.
- Ngam, P.I.; Tan, E.; Lim, G.; Yan, S.X. Improving Yittrium-90 PET Scan Image Quality through Optimized Reconstruction Algorithms. J. Nucl. Med. Technol. 2023, 51, 26–31.
- Konuparamban, A.; Nautiyal, A.; Jha, A.; Srichandan, T.; Mithun, S.; RANGARAJAN, V. Feasibility and Reliability Assessment of Single Imaging Time-Point for Organ and Tumour Dosimetry Following 177Lu-DOTATATE PRRT. J. Nucl. Med. 2022, 63, 2817.
- Veenstra, E.B.; Brouwers, A.H.; de Groot, D.J.A.; Hofland, J.; Walenkamp, A.M.E.; Brabander, T.; Zandee, W.T.; Noordzij, W. Comparison of DOPA and DOTA-TOC as a PET Imaging Tracer before Peptide Receptor Radionuclide Therapy. Eur. J. Hybrid Imaging 2022, 6, 12.
- Wright, C.L.; Zhang, J.; Tweedle, M.F.; Knopp, M.V.; Hall, N.C. Theranostic Imaging of Yttrium-90. BioMed Res. Int. 2015, 2015, 481279.
- Yong, K.; Milenic, D.; Baidoo, K.; Brechbiel, M. Mechanisms of Cell Killing Response from Low Linear Energy Transfer (LET) Radiation Originating from 177Lu Radioimmunotherapy Targeting Disseminated Intraperitoneal Tumor Xenografts. Int. J. Mol. Sci. 2016, 17, 736.
- Kassis, A.I. Therapeutic Radionuclides: Biophysical and Radiobiologic Principles. Semin. Nucl. Med. 2008, 38, 358–366.
- Graves, S.A.; Hernandez, R.; Fonslet, J.; England, C.G.; Valdovinos, H.F.; Ellison, P.A.; Barnhart, T.E.; Elema, D.R.; Theuer, C.P.; Cai, W.; et al. Novel Preparation Methods of 52 Mn for ImmunoPET Imaging. Bioconjug. Chem. 2015, 26, 2118–2124.
- McDevitt, M.R.; Sgouros, G.; Finn, R.D.; Humm, J.L.; Jurcic, J.G.; Larson, S.M.; Scheinberg, D.A. Radioimmunotherapy with Alpha-Emitting Nuclides. Eur. J. Nucl. Med. Mol. Imaging 1998, 25, 1341–1351.
- McDevitt, M.R.; Ma, D.; Lai, L.T.; Simon, J.; Borchardt, P.; Frank, R.K.; Wu, K.; Pellegrini, V.; Curcio, M.J.; Miederer, M.; et al. Tumor Therapy with Targeted Atomic Nanogenerators. Science 2001, 294, 1537–1540.
- Müller, C.; van der Meulen, N.P.; Benešová, M.; Schibli, R. Therapeutic Radiometals Beyond 177 Lu and 90 Y: Production and Application of Promising α-Particle, β-Particle, and Auger Electron Emitters. J. Nucl. Med. 2017, 58, 91S–96S.
- Ling, S.W.; de Blois, E.; Hooijman, E.; van der Veldt, A.; Brabander, T. Advances in 177Lu-PSMA and 225Ac-PSMA Radionuclide Therapy for Metastatic Castration-Resistant Prostate Cancer. Pharmaceutics 2022, 14, 2166.
- Filippi, L.; Chiaravalloti, A.; Schillaci, O.; Bagni, O. The Potential of PSMA-Targeted Alpha Therapy in the Management of Prostate Cancer. Expert Rev. Anticancer Ther. 2020, 20, 823–829.
- Ku, A.; Facca, V.J.; Cai, Z.; Reilly, R.M. Auger Electrons for Cancer Therapy—A Review. EJNMMI Radiopharm. Chem. 2019, 4, 27.
- Stella, M.; Braat, A.J.A.T.; Lam, M.G.E.H.; de Jong, H.W.A.M.; van Rooij, R. Gamma Camera Characterization at High Holmium-166 Activity in Liver Radioembolization. EJNMMI Phys. 2021, 8, 22.
- Klaassen, N.J.M.; Arntz, M.J.; Gil Arranja, A.; Roosen, J.; Nijsen, J.F.W. The Various Therapeutic Applications of the Medical Isotope Holmium-166: A Narrative Review. EJNMMI Radiopharm. Chem. 2019, 4, 19.
- Ha, E.J.; Gwak, H.-S.; Rhee, C.H.; Youn, S.M.; Choi, C.-W.; Cheon, G.J. Intracavitary Radiation Therapy for Recurrent Cystic Brain Tumors with Holmium-166-Chico: A Pilot Study. J. Korean Neurosurg. Soc. 2013, 54, 175.
- Bhusari, P.; Vatsa, R.; Singh, G.; Parmar, M.; Bal, A.; Dhawan, D.K.; Mittal, B.R.; Shukla, J. Development of Lu-177-Trastuzumab for Radioimmunotherapy of HER2 Expressing Breast Cancer and Its Feasibility Assessment in Breast Cancer Patients. Int. J. Cancer 2017, 140, 938–947.
- Emmett, L.; Willowson, K.; Violet, J.; Shin, J.; Blanksby, A.; Lee, J. Lutetium 177 PSMA Radionuclide Therapy for Men with Prostate Cancer: A Review of the Current Literature and Discussion of Practical Aspects of Therapy. J. Med. Radiat. Sci. 2017, 64, 52–60.
- Dash, A.; Knapp, F.F.; Pillai, M. Targeted Radionuclide Therapy—An Overview. Curr. Radiopharm. 2013, 6, 152–180.
- Yeong, C.-H.; Cheng, M.; Ng, K.-H. Therapeutic Radionuclides in Nuclear Medicine: Current and Future Prospects. J. Zhejiang Univ. Sci. B 2014, 15, 845–863.
- Sartor, O. Overview of Samarium Sm 153 Lexidronam in the Treatment of Painful Metastatic Bone Disease. Rev. Urol. 2004, 6 (Suppl. 10), S3–S12.
- Eary, J.F.; Collins, C.; Stabin, M.; Vernon, C.; Petersdorf, S.; Baker, M.; Hartnett, S.; Ferency, S.; Addison, S.J.; Appelbaum, F. Samarium-153-EDTMP Biodistribution and Dosimetry Estimation. J. Nucl. Med. 1993, 34, 1031–1036.
- D’Arienzo, M. Emission of Β+ Particles Via Internal Pair Production in the 0+–0+ Transition of 90Zr: Historical Background and Current Applications in Nuclear Medicine Imaging. Atoms 2013, 1, 2–12.
- Kim, Y.-C.; Kim, Y.-H.; Uhm, S.-H.; Seo, Y.S.; Park, E.-K.; Oh, S.-Y.; Jeong, E.; Lee, S.; Choe, J.-G. Radiation Safety Issues in Y-90 Microsphere Selective Hepatic Radioembolization Therapy: Possible Radiation Exposure from the Patients. Nucl. Med. Mol. Imaging 2010, 44, 252–260.
- Tong, A.K.T.; Kao, Y.H.; Too, C.W.; Chin, K.F.W.; Ng, D.C.E.; Chow, P.K.H. Yttrium-90 Hepatic Radioembolization: Clinical Review and Current Techniques in Interventional Radiology and Personalized Dosimetry. Br. J. Radiol. 2016, 89, 20150943.
- Kong, G.; Hicks, R.J. PRRT for Higher-Grade Neuroendocrine Neoplasms: What Is Still Acceptable? Curr. Opin. Pharmacol. 2022, 67, 102293.
- Desai, P.; Rimal, R.; Sahnoun, S.E.M.; Mottaghy, F.M.; Möller, M.; Morgenroth, A.; Singh, S. Radiolabeled Nanocarriers as Theranostics—Advancement from Peptides to Nanocarriers. Small 2022, 18, 2200673.
- Gudkov, S.; Shilyagina, N.; Vodeneev, V.; Zvyagin, A. Targeted Radionuclide Therapy of Human Tumors. Int. J. Mol. Sci. 2015, 17, 33.
- Lee, S.J.; Park, H.J. Single Photon Emission Computed Tomography (SPECT) or Positron Emission Tomography (PET) Imaging for Radiotherapy Planning in Patients with Lung Cancer: A Meta-Analysis. Sci. Rep. 2020, 10, 14864.
- Park, M.; Kim, M.; Yoo, J.; Jo, M. Validation of the Whole-Body Counting Measurement in a Radiation Emergency. Appl. Radiat. Isot. 2021, 168, 109476.
- Tashima, H.; Yamaya, T. Compton Imaging for Medical Applications. Radiol. Phys. Technol. 2022, 15, 187–205.
- Andreo, P. Monte Carlo Simulations in Radiotherapy Dosimetry. Radiat. Oncol. 2018, 13, 121.
- Lee, C.; Park, B.; Lee, S.-S.; Kim, J.-E.; Han, S.-S.; Huh, K.-H.; Yi, W.-J.; Heo, M.-S.; Choi, S.-C. Efficacy of the Monte Carlo Method and Dose Reduction Strategies in Paediatric Panoramic Radiography. Sci. Rep. 2019, 9, 9691.
- Muraro, S.; Battistoni, G.; Kraan, A.C. Challenges in Monte Carlo Simulations as Clinical and Research Tool in Particle Therapy: A Review. Front. Phys. 2020, 8, 567800.
- Snyder, W.S.; Fisher, H.L.; Ford, M.R.; Warner, G.G. Estimates of Absorbed Fractions for Monoenergetic Photon Sources Uniformly Distributed in Various Organs of a Heterogeneous Phantom. J. Nucl. Med. 1969, 10 (Suppl. S3), 7–52.
- Dieudonné, A.; Hobbs, R.F.; Bolch, W.E.; Sgouros, G.; Gardin, I. Fine-Resolution Voxel S Values for Constructing Absorbed Dose Distributions at Variable Voxel Size. J. Nucl. Med. 2010, 51, 1600–1607.
- Siegel, J.A.; Thomas, S.R.; Stubbs, J.B.; Stabin, M.G.; Hays, M.T.; Koral, K.F.; Robertson, J.S.; Howell, R.W.; Wessels, B.W.; Fisher, D.R.; et al. MIRD Pamphlet No. 16: Techniques for Quantitative Radiopharmaceutical Biodistribution Data Acquisition and Analysis for Use in Human Radiation Dose Estimates. J. Nucl. Med. 1999, 40, 37S–61S.
- Amaya, H. Diffusion Processes in Tumors: A Nuclear Medicine Approach. In AIP Conference Proceedings; AIP Publishing LLC: Melville, NY, USA, 2016; p. 080015.
- Rani, N.; Singh, B.; Kumar, N.; Singh, P.; Hazari, P.P.; Vyas, S.; Hooda, M.; Chitkara, A.; Shekhawat, A.S.; Gupta, S.K.; et al. -Bis-Methionine-DTPA Single-Photon Emission Computed Tomography Impacting Glioma Management: A Sensitive Indicator for Postsurgical/Chemoradiotherapy Response Assessment. Cancer Biother. Radiopharm. 2021, 36, 568–578.
- Verma, A.; Hesterman, J.Y.; Chazen, J.L.; Holt, R.; Connolly, P.; Horky, L.; Vallabhajosula, S.; Mozley, P.D. Intrathecal 99m Tc-DTPA Imaging of Molecular Passage from Lumbar Cerebrospinal Fluid to Brain and Periphery in Humans. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2020, 12, e12030.
- Santra, A.; Sharma, P.; Kumar, R. Use of 99m-Technetium-Glucoheptonate as a Tracer for Brain Tumor Imaging: An Overview of Its Strengths and Pitfalls. Indian J. Nucl. Med. 2015, 30, 1–8.
- Kung, H.F. New Technetium 99m-Labeled Brain Perfusion Imaging Agents. Semin. Nucl. Med. 1990, 20, 150–158.
- Porubcin, S.; Rovnakova, A.; Zahornacky, O.; Jarcuska, P. Diagnostic Value of Radioisotope Cisternography Using 111In-DTPA in a Patient with Rhinorrhea and Purulent Meningitis. Medicina 2022, 58, 714.
- Wangler, B.; Schirrmacher, R.; Bartenstein, P.; Wangler, C. Chelating Agents and Their Use in Radiopharmaceutical Sciences. Mini-Rev. Med. Chem. 2011, 11, 968–983.
- Okarvi, S.M. Recent Developments in 99Tcm-Labelled Peptide-Based Radiopharmaceuticals. Nucl. Med. Commun. 1999, 20, 1093–1112.
- Dijkgraaf, I.; Agten, S.M.; Bauwens, M.; Hackeng, T.M. Strategies for Site-Specific Radiolabeling of Peptides and Proteins. In Radiopharmaceuticals—Current Research for Better Diagnosis and Therapy; IntechOpen: London, UK, 2022.
- Bronstein, M.D. Acromegaly: Molecular Expression of Somatostatin Receptor Subtypes and Treatment Outcome. In Pituitary Today: Molecular, Physiological and Clinical Aspects; KARGER: Basel, Switzerland, 2006; pp. 129–134.
- de Herder, W.W.; Rehfeld, J.F.; Kidd, M.; Modlin, I.M. A Short History of Neuroendocrine Tumours and Their Peptide Hormones. Best Pract. Res. Clin. Endocrinol. Metab. 2016, 30, 3–17.
- Bauer, W.; Briner, U.; Doepfner, W.; Haller, R.; Huguenin, R.; Marbach, P.; Petcher, T.J.; Pless, J. SMS 201–995: A Very Potent and Selective Octapeptide Analogue of Somatostatin with Prolonged Action. Life Sci. 1982, 31, 1133–1140.
- Reubi, J.C.; Maurer, R. Autoradiographic Mapping of Somatostatin Receptors in the Rat Central Nervous System and Pituitary. Neuroscience 1985, 15, 1183–1193.
- Lamberts, S.W.; Reubi, J.C.; Bakker, W.H.; Krenning, E.P. Somatostatin Receptor Imaging with 123I-Tyr3-Octreotide. Z. Gastroenterol. 1990, 28 (Suppl. S2), 20–21.
- Bakker, W.H.; Albert, R.; Bruns, C.; Breeman, W.A.P.; Hofland, L.J.; Marbach, P.; Pless, J.; Pralet, D.; Stolz, B.; Koper, J.W.; et al. -Octreotide, a Potential Radiopharmaceutical for Imaging of Somatostatin Receptor-Positive Tumors: Synthesis, Radiolabeling and in Vitro Validation. Life Sci. 1991, 49, 1583–1591.
- Bushnell, D.L.; Menda, Y.; Madsen, M.T.; Link, B.K.; Kahn, D.; Truhlar, S.M.; Juweid, M.; Shannon, M.; Murguia, J.S. 99mTc-Depreotide Tumour Uptake in Patients with Non-Hodgkin’s Lymphoma. Nucl. Med. Commun. 2004, 25, 839–843.
- Liu, Q.; Cheng, Y.; Zang, J.; Sui, H.; Wang, H.; Jacobson, O.; Zhu, Z.; Chen, X. Dose Escalation of an Evans Blue–Modified Radiolabeled Somatostatin Analog 177Lu-DOTA-EB-TATE in the Treatment of Metastatic Neuroendocrine Tumors. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 947–957.
- Zhang, J.; Wang, H.; Jacobson, O.; Cheng, Y.; Niu, G.; Li, F.; Bai, C.; Zhu, Z.; Chen, X. Safety, Pharmacokinetics, and Dosimetry of a Long-Acting Radiolabeled Somatostatin Analog 177 Lu-DOTA-EB-TATE in Patients with Advanced Metastatic Neuroendocrine Tumors. J. Nucl. Med. 2018, 59, 1699–1705.
- Alessandrini, L.; Ferrari, M.; Taboni, S.; Sbaraglia, M.; Franz, L.; Saccardo, T.; Del Forno, B.M.; Agugiaro, F.; Frigo, A.C.; Dei Tos, A.P.; et al. Tumor-Stroma Ratio, Neoangiogenesis and Prognosis in Laryngeal Carcinoma. A Pilot Study on Preoperative Biopsies and Matched Surgical Specimens. Oral Oncol. 2022, 132, 105982.
- Mina-Osorio, P. The Moonlighting Enzyme CD13: Old and New Functions to Target. Trends Mol. Med. 2008, 14, 361–371.
- Kis, A.; Dénes, N.; Szabó, J.P.; Arató, V.; Beke, L.; Matolay, O.; Enyedi, K.N.; Méhes, G.; Mező, G.; Bai, P.; et al. In Vivo Molecular Imaging of the Efficacy of Aminopeptidase N (APN/CD13) Receptor Inhibitor Treatment on Experimental Tumors Using 68Ga-NODAGA-c(NGR) Peptide. Biomed Res. Int. 2021, 2021, 6642973.
- Surowiak, P.; Drąg, M.; Materna, V.; Suchocki, S.; Grzywa, R.; Spaczyński, M.; Dietel, M.; Oleksyszyn, J.; Zabel, M.; Lage, H. Expression of Aminopeptidase N/CD13 in Human Ovarian Cancers. Int. J. Gynecol. Cancer 2006, 16, 1783–1788.
- Meng, Y.; Zhang, Z.; Liu, K.; Ye, L.; Liang, Y.; Gu, W. Aminopeptidase N (CD13) Targeted MR and NIRF Dual-Modal Imaging of Ovarian Tumor Xenograft. Mater. Sci. Eng. C 2018, 93, 968–974.
- Yang, Y.; Zhang, J.; Zou, H.; Shen, Y.; Deng, S.; Wu, Y. Synthesis and Evaluation of 68 Ga-Labeled Dimeric CNGR Peptide for PET Imaging of CD13 Expression with Ovarian Cancer Xenograft. J. Cancer 2021, 12, 244–252.
- Crowley, F.; Sterpi, M.; Buckley, C.; Margetich, L.; Handa, S.; Dovey, Z. A Review of the Pathophysiological Mechanisms Underlying Castration-Resistant Prostate Cancer. Res. Rep. Urol. 2021, 13, 457–472.
- Cyrta, J.; Augspach, A.; De Filippo, M.R.; Prandi, D.; Thienger, P.; Benelli, M.; Cooley, V.; Bareja, R.; Wilkes, D.; Chae, S.-S.; et al. Role of Specialized Composition of SWI/SNF Complexes in Prostate Cancer Lineage Plasticity. Nat. Commun. 2020, 11, 5549.
- Sartor, O.; de Bono, J.; Chi, K.N.; Fizazi, K.; Herrmann, K.; Rahbar, K.; Tagawa, S.T.; Nordquist, L.T.; Vaishampayan, N.; El-Haddad, G.; et al. Lutetium-177–PSMA-617 for Metastatic Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2021, 385, 1091–1103.




