
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Cristian Arriaga-Canon | -- | 3073 | 2023-04-27 17:18:47 | | | |
| 2 | Beatrix Zheng | -1 word(s) | 3072 | 2023-05-04 03:40:19 | | |
Video Upload Options
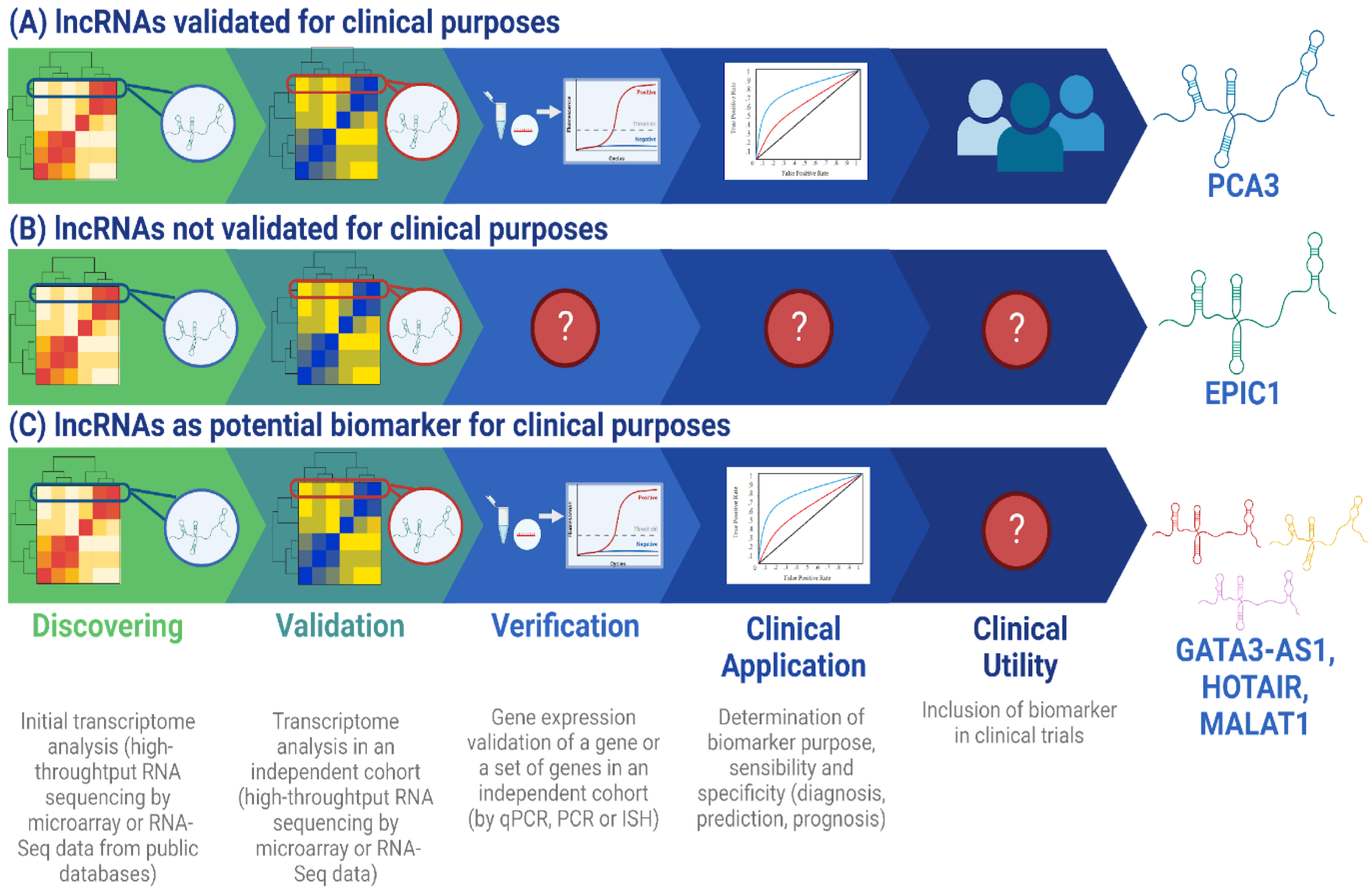
Given their tumor-specific and stage-specific gene expression, long non-coding RNAs (lncRNAs) have demonstrated to be potential molecular biomarkers for diagnosis, prognosis, and treatment response. Particularly, the lncRNAs DSCAM-AS1 and GATA3-AS1 serve as examples of this because of their high subtype-specific expression profile in luminal B-like breast cancer. This makes them candidates to use as molecular biomarkers in clinical practice. However, lncRNA studies in breast cancer are limited in sample size and are restricted to the determination of their biological function, which represents an obstacle for its inclusion as molecular biomarkers of clinical utility. Nevertheless, due to their expression specificity among diseases, such as cancer, and their stability in body fluids, lncRNAs are promising molecular biomarkers that could improve the reliability, sensitivity, and specificity of molecular techniques used in clinical diagnosis. The development of lncRNA-based diagnostics will be useful in routine medical practice to improve patient clinical management and quality of life.
1. Overview
2. Challenges and Perspectives for lncRNA Clinical Application as Predictive Biomarkers for Breast Cancer Management
3.The Use of lncRNAs as Molecular Biomarkers in the RNA-Based Therapeutics Era
4. The Current Challenges for lncRNA Research and for Their Implementation as Molecular Biomarkers in Routine Clinical Practice
References
- Jin, H.; Du, W.; Huang, W.; Yan, J.; Tang, Q.; Chen, Y.; Zou, Z. LncRNA and Breast Cancer: Progress from Identifying Mechanisms to Challenges and Opportunities of Clinical Treatment. Mol. Ther. Nucleic Acids 2021, 25, 613–637.
- Xi, X.; Li, T.; Huang, Y.; Sun, J.; Zhu, Y.; Yang, Y.; Lu, Z.J. RNA Biomarkers: Frontier of Precision Medicine for Cancer. Non-Coding RNA 2017, 3, 9.
- Jiang, S.; Cheng, S.-J.; Ren, L.-C.; Wang, Q.; Kang, Y.-J.; Ding, Y.; Hou, M.; Yang, X.-X.; Lin, Y.; Liang, N.; et al. An Expanded Landscape of Human Long Noncoding RNA. Nucleic Acids Res. 2019, 47, 7842–7856.
- Mehra, R.; Udager, A.M.; Ahearn, T.U.; Cao, X.; Feng, F.Y.; Loda, M.; Petimar, J.S.; Kantoff, P.; Mucci, L.A.; Chinnaiyan, A.M. Overexpression of the Long Non-Coding RNA SChLAP1 Independently Predicts Lethal Prostate Cancer. Eur. Urol. 2016, 70, 549–552.
- Işın, M.; Uysaler, E.; Özgür, E.; Köseoğlu, H.; Şanlı, Ö.; Yücel, Ö.B.; Gezer, U.; Dalay, N. Exosomal LncRNA-P21 Levels May Help to Distinguish Prostate Cancer from Benign Disease. Front. Genet. 2015, 6, 168.
- Lemos, A.E.G.; Matos, A.D.R.; Ferreira, L.B.; Gimba, E.R.P. The Long Non-Coding RNA PCA3: An Update of Its Functions and Clinical Applications as a Biomarker in Prostate Cancer. Oncotarget 2019, 10, 6589–6603.
- Prensner, J.R.; Iyer, M.K.; Sahu, A.; Asangani, I.A.; Cao, Q.; Patel, L.; Vergara, I.A.; Davicioni, E.; Erho, N.; Ghadessi, M.; et al. The Long Noncoding RNA SChLAP1 Promotes Aggressive Prostate Cancer and Antagonizes the SWI/SNF Complex. Nat. Genet. 2013, 45, 1392–1398.
- Mehra, R.; Shi, Y.; Udager, A.M.; Prensner, J.R.; Sahu, A.; Iyer, M.K.; Siddiqui, J.; Cao, X.; Wei, J.; Jiang, H.; et al. A Novel RNA in Situ Hybridization Assay for the Long Noncoding RNA SChLAP1 Predicts Poor Clinical Outcome after Radical Prostatectomy in Clinically Localized Prostate Cancer. Neoplasia 2014, 16, 1121–1127.
- Luo, J.; Wang, K.; Yeh, S.; Sun, Y.; Liang, L.; Xiao, Y.; Xu, W.; Niu, Y.; Cheng, L.; Maity, S.N.; et al. LncRNA-P21 Alters the Antiandrogen Enzalutamide-Induced Prostate Cancer Neuroendocrine Differentiation via Modulating the EZH2/STAT3 Signaling. Nat. Commun. 2019, 10, 2571.
- Amirinejad, R.; Rezaei, M.; Shirvani-Farsani, Z. An Update on Long Intergenic Noncoding RNA P21: A Regulatory Molecule with Various Significant Functions in Cancer. Cell Biosci. 2020, 10, 82.
- Bussemakers, M.J.; van Bokhoven, A.; Verhaegh, G.W.; Smit, F.P.; Karthaus, H.F.; Schalken, J.A.; Debruyne, F.M.; Ru, N.; Isaacs, W.B. DD3: A New Prostate-Specific Gene, Highly Overexpressed in Prostate Cancer. Cancer Res. 1999, 59, 5975–5979.
- Xue, W.-J.; Ying, X.-L.; Jiang, J.-H.; Xu, Y.-H. Prostate Cancer Antigen 3 as a Biomarker in the Urine for Prostate Cancer Diagnosis: A Meta-Analysis. J. Cancer Res. Ther. 2014, 10 (Suppl. S3), C218–C221.
- Jiang, G.; Su, Z.; Liang, X.; Huang, Y.; Lan, Z.; Jiang, X. Long Non-Coding RNAs in Prostate Tumorigenesis and Therapy (Review). Mol. Clin. Oncol. 2020, 13, 76.
- Reid, J.; Gen-Probe, Incorporated. Clinical Evaluation of the PROGENSA(R) PCA3 Assay in Men with a Previous Negative Biopsy Result; Clinical Trial ID: NCT01024959. 2012. Available online: https://beta.clinicaltrials.gov/study/NCT01024959?distance=50&term=NCT01024959&rank=1 (accessed on 22 February 2023).
- Durand, X.; Moutereau, S.; Xylinas, E.; de la Taille, A. ProgensaTM PCA3 Test for Prostate Cancer. Expert Rev. Mol. Diagn. 2011, 11, 137–144.
- Chaput, G.; Sumar, N. Endocrine Therapies for Breast and Prostate Cancers. Can. Fam. Physician 2022, 68, 271–276.
- Hou, P.; Zhao, Y.; Li, Z.; Yao, R.; Ma, M.; Gao, Y.; Zhao, L.; Zhang, Y.; Huang, B.; Lu, J. LincRNA-ROR Induces Epithelial-to-Mesenchymal Transition and Contributes to Breast Cancer Tumorigenesis and Metastasis. Cell Death Dis. 2014, 5, e1287.
- Udager, A.M.; Tomlins, S.A. Molecular Biomarkers in the Clinical Management of Prostate Cancer. Cold Spring Harb. Perspect. Med. 2018, 8, a030601.
- Alarcón-Zendejas, A.P.; Scavuzzo, A.; Jiménez-Ríos, M.A.; Álvarez-Gómez, R.M.; Montiel-Manríquez, R.; Castro-Hernández, C.; Jiménez-Dávila, M.A.; Pérez-Montiel, D.; González-Barrios, R.; Jiménez-Trejo, F.; et al. The Promising Role of New Molecular Biomarkers in Prostate Cancer: From Coding and Non-Coding Genes to Artificial Intelligence Approaches. Prostate Cancer Prostatic Dis. 2022, 25, 431–443.
- Ramos, C.G.; Valdevenito, R.; Vergara, I.; Anabalon, P.; Sanchez, C.; Fulla, J. PCA3 Sensitivity and Specificity for Prostate Cancer Detection in Patients with Abnormal PSA and/or Suspicious Digital Rectal Examination. First Latin American Experience. Urol. Oncol. 2013, 31, 1522–1526.
- van Gils, M.P.M.Q.; Hessels, D.; van Hooij, O.; Jannink, S.A.; Peelen, W.P.; Hanssen, S.L.J.; Witjes, J.A.; Cornel, E.B.; Karthaus, H.F.M.; Smits, G.A.H.J.; et al. The Time-Resolved Fluorescence-Based PCA3 Test on Urinary Sediments after Digital Rectal Examination; a Dutch Multicenter Validation of the Diagnostic Performance. Clin. Cancer Res. 2007, 13, 939–943.
- Tosoian, J.J.; Trock, B.J.; Morgan, T.M.; Salami, S.S.; Tomlins, S.A.; Spratt, D.E.; Siddiqui, J.; Kunju, L.P.; Botbyl, R.; Chopra, Z.; et al. Use of the MyProstateScore Test to Rule Out Clinically Significant Cancer: Validation of a Straightforward Clinical Testing Approach. J. Urol. 2021, 205, 732–739.
- Guo, W.; Wang, Q.; Zhan, Y.; Chen, X.; Yu, Q.; Zhang, J.; Wang, Y.; Xu, X.; Zhu, L. Transcriptome Sequencing Uncovers a Three–Long Noncoding RNA Signature in Predicting Breast Cancer Survival. Sci. Rep. 2016, 6, 27931.
- Yoosuf, N.; Navarro, J.F.; Salmén, F.; Ståhl, P.L.; Daub, C.O. Identification and Transfer of Spatial Transcriptomics Signatures for Cancer Diagnosis. Breast Cancer Res. 2020, 22, 6.
- Fan, C.-N.; Ma, L.; Liu, N. Systematic Analysis of LncRNA-MiRNA-MRNA Competing Endogenous RNA Network Identifies Four-LncRNA Signature as a Prognostic Biomarker for Breast Cancer. J. Transl. Med. 2018, 16, 264.
- Berger, A.C.; Korkut, A.; Kanchi, R.S.; Hegde, A.M.; Lenoir, W.; Liu, W.; Liu, Y.; Fan, H.; Shen, H.; Ravikumar, V.; et al. A Comprehensive Pan-Cancer Molecular Study of Gynecologic and Breast Cancers. Cancer Cell 2018, 33, 690–705.e9.
- Niknafs, Y.S.; Han, S.; Ma, T.; Speers, C.; Zhang, C.; Wilder-Romans, K.; Iyer, M.K.; Pitchiaya, S.; Malik, R.; Hosono, Y.; et al. The LncRNA Landscape of Breast Cancer Reveals a Role for DSCAM-AS1 in Breast Cancer Progression. Nat. Commun. 2016, 7, 12791.
- Contreras-Espinosa, L.; Alcaraz, N.; De La Rosa-Velázquez, I.A.; Díaz-Chávez, J.; Cabrera-Galeana, P.; Vega, R.R.; Reynoso-Noveron, N.; Maldonado-Martínez, H.A.; González-Barrios, R.; Montiel-Manríquez, R.; et al. Transcriptome Analysis Identifies GATA3-AS1 as a Long Noncoding RNA Associated with Resistance to Neoadjuvant Chemotherapy in Locally Advanced Breast Cancer Patients. J. Mol. Diagn. 2021, 23, 1306–1323.
- De Palma, F.D.E.; Del Monaco, V.; Pol, J.G.; Kremer, M.; D’Argenio, V.; Stoll, G.; Montanaro, D.; Uszczyńska-Ratajczak, B.; Klein, C.C.; Vlasova, A.; et al. The Abundance of the Long Intergenic Non-Coding RNA 01087 Differentiates between Luminal and Triple-Negative Breast Cancers and Predicts Patient Outcome. Pharmacol. Res. 2020, 161, 105249.
- Jézéquel, P.; Gouraud, W.; Ben Azzouz, F.; Guérin-Charbonnel, C.; Juin, P.P.; Lasla, H.; Campone, M. Bc-GenExMiner 4.5: New Mining Module Computes Breast Cancer Differential Gene Expression Analyses. Database 2021, 2021, baab007.
- Lu, R.; Zhang, J.; Zhang, W.; Huang, Y.; Wang, N.; Zhang, Q.; Qu, S. Circulating HOTAIR Expression Predicts the Clinical Response to Neoadjuvant Chemotherapy in Patients with Breast Cancer. Cancer Biomark. 2018, 22, 249–256.
- Pan, J.; Bian, Y.; Cao, Z.; Lei, L.; Pan, J.; Huang, J.; Cai, X.; Lan, X.; Zheng, H. Long Noncoding RNA MALAT1 as a Candidate Serological Biomarker for the Diagnosis of Non-small Cell Lung Cancer: A Meta-analysis. Thorac. Cancer 2020, 11, 329–335.
- Han, D.; Gao, X.; Wang, M.; Qiao, Y.; Xu, Y.; Yang, J.; Dong, N.; He, J.; Sun, Q.; Lv, G.; et al. Long Noncoding RNA H19 Indicates a Poor Prognosis of Colorectal Cancer and Promotes Tumor Growth by Recruiting and Binding to EIF4A3. Oncotarget 2016, 7, 22159–22173.
- Xie, H.; Ma, H.; Zhou, D. Plasma HULC as a Promising Novel Biomarker for the Detection of Hepatocellular Carcinoma. Biomed. Res. Int. 2013, 2013, 136106.
- Fan, Y.; Shen, B.; Tan, M.; Mu, X.; Qin, Y.; Zhang, F.; Liu, Y. Long Non-Coding RNA UCA1 Increases Chemoresistance of Bladder Cancer Cells by Regulating Wnt Signaling. FEBS J. 2014, 281, 1750–1758.
- Shan, L.; Zhao, T.; Wang, Y. Upregulation of Serum LncRNA DLEU1 Predicts Progression of Premalignant Endometrial Lesion and Unfavorable Clinical Outcome of Endometrial Cancer. Technol. Cancer Res. Treat 2020, 19, 1533033820965589.
- Bhan, A.; Soleimani, M.; Mandal, S.S. Long Noncoding RNA and Cancer: A New Paradigm. Cancer Res. 2017, 77, 3965–3981.
- Selleck, M.J.; Senthil, M.; Wall, N.R. Making Meaningful Clinical Use of Biomarkers. Biomark. Insights 2017, 12, 1177271917715236.
- Matkovich, S.J.; Edwards, J.R.; Grossenheider, T.C.; Strong, C.D.G.; Dorn, G.W. Epigenetic Coordination of Embryonic Heart Transcription by Dynamically Regulated Long Noncoding RNAs. Proc. Natl. Acad. Sci. USA 2014, 111, 12264–12269.
- Sathishkumar, C.; Prabu, P.; Mohan, V.; Balasubramanyam, M. Linking a Role of LncRNAs (Long Non-Coding RNAs) with Insulin Resistance, Accelerated Senescence, and Inflammation in Patients with Type 2 Diabetes. Hum. Genom. 2018, 12, 41.
- World Health Organization. World Health Statistics 2021: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2021.
- Harbeck, N.; Penault-Llorca, F.; Cortes, J.; Gnant, M.; Houssami, N.; Poortmans, P.; Ruddy, K.; Tsang, J.; Cardoso, F. Breast Cancer. Nat. Rev. Dis. Prim. 2019, 5, 66.
- Galamb, O.; Barták, B.K.; Kalmár, A.; Nagy, Z.B.; Szigeti, K.A.; Tulassay, Z.; Igaz, P.; Molnár, B. Diagnostic and Prognostic Potential of Tissue and Circulating Long Non-Coding RNAs in Colorectal Tumors. World J. Gastroenterol. 2019, 25, 5026–5048.
- Shi, T.; Gao, G.; Cao, Y. Long Noncoding RNAs as Novel Biomarkers Have a Promising Future in Cancer Diagnostics. Dis. Markers 2016, 2016, e9085195.
- Yang, E.; van Nimwegen, E.; Zavolan, M.; Rajewsky, N.; Schroeder, M.; Magnasco, M.; Darnell, J.E. Decay Rates of Human MRNAs: Correlation with Functional Characteristics and Sequence Attributes. Genome Res. 2003, 13, 1863–1872.
- Özgür, E.; Ferhatoğlu, F.; Şen, F.; Saip, P.; Gezer, U. Circulating LncRNA H19 May Be a Useful Marker of Response to Neoadjuvant Chemotherapy in Breast Cancer. Cancer Biomark. 2020, 27, 11–17.
- Zidan, H.E.; Karam, R.A.; El-Seifi, O.S.; Abd Elrahman, T.M. Circulating Long Non-Coding RNA MALAT1 Expression as Molecular Biomarker in Egyptian Patients with Breast Cancer. Cancer Genet. 2018, 220, 32–37.
- Tang, H.; Wu, Z.; Zhang, J.; Su, B. Salivary LncRNA as a Potential Marker for Oral Squamous Cell Carcinoma Diagnosis. Mol. Med. Rep. 2013, 7, 761–766.
- Alba, J.; Gutierrez, J.; Coupe, V.M.; Fernández, B.; Vázquez-Boquete, Á.; Alba, J.; Forteza, J.; García-Caballero, T. HER2 Status Determination Using RNA-ISH--a Rapid and Simple Technique Showing High Correlation with FISH and IHC in 141 Cases of Breast Cancer. Histol. Histopathol. 2012, 27, 1021–1027.
- Arnould, L.; Roger, P.; MacGrogan, G.; Chenard, M.-P.; Balaton, A.; Beauclair, S.; Penault-Llorca, F. Accuracy of HER2 Status Determination on Breast Core-Needle Biopsies (Immunohistochemistry, FISH, CISH and SISH vs. FISH). Mod. Pathol. 2012, 25, 675–682.
- Jiang, H.; Li, X.; Wang, W.; Dong, H. Long Non-Coding RNA SNHG3 Promotes Breast Cancer Cell Proliferation and Metastasis by Binding to MicroRNA-154-3p and Activating the Notch Signaling Pathway. BMC Cancer 2020, 20, 838.
- Yan, X.; Hu, Z.; Feng, Y.; Hu, X.; Yuan, J.; Zhao, S.D.; Zhang, Y.; Yang, L.; Shan, W.; He, Q.; et al. Comprehensive Genomic Characterization of Long Non-Coding RNAs across Human Cancers. Cancer Cell 2015, 28, 529–540.
- Ginsburg, G.S.; Phillips, K.A. Precision Medicine: From Science to Value. Health Aff. (Millwood) 2018, 37, 694–701.
- Hu, Q.; Ma, H.; Chen, H.; Zhang, Z.; Xue, Q. LncRNA in Tumorigenesis of Non-Small-Cell Lung Cancer: From Bench to Bedside. Cell Death Discov. 2022, 8, 359.
- Dey Ghosh, R.; Guha Majumder, S. Circulating Long Non-Coding RNAs Could Be the Potential Prognostic Biomarker for Liquid Biopsy for the Clinical Management of Oral Squamous Cell Carcinoma. Cancers 2022, 14, 5590.
- Hessels, D.; Klein Gunnewiek, J.M.T.; van Oort, I.; Karthaus, H.F.M.; van Leenders, G.J.L.; van Balken, B.; Kiemeney, L.A.; Witjes, J.A.; Schalken, J.A. DD3(PCA3)-Based Molecular Urine Analysis for the Diagnosis of Prostate Cancer. Eur. Urol. 2003, 44, 8–15; discussion 15–16.
- Li, J.; Guan, X.; Fan, Z.; Ching, L.-M.; Li, Y.; Wang, X.; Cao, W.-M.; Liu, D.-X. Non-Invasive Biomarkers for Early Detection of Breast Cancer. Cancers 2020, 12, 2767.
- Rogers-Broadway, K.-R.; Karteris, E. Amplification Efficiency and Thermal Stability of QPCR Instrumentation: Current Landscape and Future Perspectives. Exp. Ther. Med. 2015, 10, 1261–1264.
- Reasons for Delays in Getting Your Biopsy and Cytology Test Results. Available online: https://www.cancer.org/treatment/understanding-your-diagnosis/tests/testing-biopsy-and-cytology-specimens-for-cancer/how-long-does-testing-take.html (accessed on 10 December 2021).
- Zhang, Y.; XIA, K.; LI, C.; WEI, B.; Zhang, B. Review of Breast Cancer Pathologigcal Image Processing. Biomed. Res. Int. 2021, 2021, 1994764.
- Gamble, P.; Jaroensri, R.; Wang, H.; Tan, F.; Moran, M.; Brown, T.; Flament-Auvigne, I.; Rakha, E.A.; Toss, M.; Dabbs, D.J.; et al. Determining Breast Cancer Biomarker Status and Associated Morphological Features Using Deep Learning. Commun. Med. 2021, 1, 14.
- Lobato-Delgado, B.; Priego-Torres, B.; Sanchez-Morillo, D. Combining Molecular, Imaging, and Clinical Data Analysis for Predicting Cancer Prognosis. Cancers 2022, 14, 3215.
- Li, Y.; Wu, F.-X.; Ngom, A. A Review on Machine Learning Principles for Multi-View Biological Data Integration. Brief. Bioinform. 2016, 19, 325–340.
- Ektefaie, Y.; Yuan, W.; Dillon, D.A.; Lin, N.U.; Golden, J.A.; Kohane, I.S.; Yu, K.-H. Integrative Multiomics-Histopathology Analysis for Breast Cancer Classification. Npj Breast Cancer 2021, 7, 147.
- Ou, F.-S.; Michiels, S.; Shyr, Y.; Adjei, A.A.; Oberg, A.L. Biomarker Discovery and Validation: Statistical Considerations. J. Thorac. Oncol. 2021, 16, 537–545.
- Pepe, M.S.; Li, C.I.; Feng, Z. Improving the Quality of Biomarker Discovery Research: The Right Samples and Enough of Them. Cancer Epidemiol. Biomark. Prev. 2015, 24, 944–950.
- Ren, S.; Peng, Z.; Mao, J.-H.; Yu, Y.; Yin, C.; Gao, X.; Cui, Z.; Zhang, J.; Yi, K.; Xu, W.; et al. RNA-Seq Analysis of Prostate Cancer in the Chinese Population Identifies Recurrent Gene Fusions, Cancer-Associated Long Noncoding RNAs and Aberrant Alternative Splicings. Cell Res. 2012, 22, 806–821.
- Wang, Z.; Yang, B.; Zhang, M.; Guo, W.; Wu, Z.; Wang, Y.; Jia, L.; Li, S.; Cancer Genome Atlas Research Network; Xie, W.; et al. lncRNA Epigenetic Landscape Analysis Identifies EPIC1 as an Oncogenic lncRNA that Interacts with MYC and Promotes Cell-Cycle Progression in Cancer. Cancer Cell 2018, 33, 706–720.e9.
- Zhang, Y.; Wagner, E.K.; Guo, X.; May, I.; Cai, Q.; Zheng, W.; He, C.; Long, J. Long Intergenic Non-Coding RNA Expression Signature in Human Breast Cancer. Sci. Rep. 2016, 6, 37821.
- Gupta, R.A.; Shah, N.; Wang, K.C.; Kim, J.; Horlings, H.M.; Wong, D.J.; Tsai, M.-C.; Hung, T.; Argani, P.; Rinn, J.L.; et al. Long Non-Coding RNA HOTAIR Reprograms Chromatin State to Promote Cancer Metastasis. Nature 2010, 464, 1071–1076.
- Huang, X.-J.; Xia, Y.; He, G.-F.; Zheng, L.-L.; Cai, Y.-P.; Yin, Y.; Wu, Q. MALAT1 Promotes Angiogenesis of Breast Cancer. Oncol. Rep. 2018, 40, 2683–2689.
- FDA-NIH Biomarker Working Group. BEST (Biomarkers, EndpointS, and Other Tools) Resource; National Institutes of Health:: Bethesda, MD, USA; Food and Drug Administration: Silver Spring, MD, USA, 2006.
- Ács, B.; Zámbó, V.; Vízkeleti, L.; Szász, A.M.; Madaras, L.; Szentmártoni, G.; Tőkés, T.; Molnár, B.Á.; Molnár, I.A.; Vári-Kakas, S.; et al. Ki-67 as a Controversial Predictive and Prognostic Marker in Breast Cancer Patients Treated with Neoadjuvant Chemotherapy. Diagn. Pathol. 2017, 12, 20.
- Gao, H.; Hao, G.; Sun, Y.; Li, L.; Wang, Y. Long Noncoding RNA H19 Mediated the Chemosensitivity of Breast Cancer Cells via Wnt Pathway and EMT Process. Onco. Targets Ther. 2018, 11, 8001–8012.
- Moradi, M.-T.; Fallahi, H.; Rahimi, Z. The Clinical Significance of Circulating DSCAM-AS1 in Patients with ER-Positive Breast Cancer and Construction of Its Competitive Endogenous RNA Network. Mol. Biol. Rep. 2020, 47, 7685–7697.
- Ferrando, L.; Cirmena, G.; Garuti, A.; Scabini, S.; Grillo, F.; Mastracci, L.; Isnaldi, E.; Marrone, C.; Gonella, R.; Murialdo, R.; et al. Development of a Long Non-Coding RNA Signature for Prediction of Response to Neoadjuvant Chemoradiotherapy in Locally Advanced Rectal Adenocarcinoma. PLoS ONE 2020, 15, e0226595.
- Wang, G.; Chen, X.; Liang, Y.; Wang, W.; Shen, K. A Long Noncoding RNA Signature That Predicts Pathological Complete Remission Rate Sensitively in Neoadjuvant Treatment of Breast Cancer. Transl. Oncol. 2017, 10, 988–997.




