Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Prattana Punnakitikashem | -- | 1833 | 2023-02-24 10:35:04 | | | |
| 2 | Dean Liu | -4 word(s) | 1829 | 2023-02-27 03:13:40 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Lwin, H.N.N.; Punnakitikashem, P.; Thananusak, T. E-Health in Southeast Asia. Encyclopedia. Available online: https://encyclopedia.pub/entry/41630 (accessed on 07 February 2026).
Lwin HNN, Punnakitikashem P, Thananusak T. E-Health in Southeast Asia. Encyclopedia. Available at: https://encyclopedia.pub/entry/41630. Accessed February 07, 2026.
Lwin, Hnin Nu Nu, Prattana Punnakitikashem, Trin Thananusak. "E-Health in Southeast Asia" Encyclopedia, https://encyclopedia.pub/entry/41630 (accessed February 07, 2026).
Lwin, H.N.N., Punnakitikashem, P., & Thananusak, T. (2023, February 24). E-Health in Southeast Asia. In Encyclopedia. https://encyclopedia.pub/entry/41630
Lwin, Hnin Nu Nu, et al. "E-Health in Southeast Asia." Encyclopedia. Web. 24 February, 2023.
Copy Citation
eHealth or digital health innovations expanded tremendously during the COVID-19 pandemic. Innovation and digitalization offer creative solutions to build up a healthy society. The eHealth technologies are quickly taken up by Southeast Asia countries and continue to flourish to alleviate the burden of healthcare challenges.
e-health
bibliometric review
electronic health
1. Introduction
In the contemporary era, the world has been disrupted by digital technologies. With no exception in the healthcare industry, innovation and digitalization deliver promising solutions to build up a healthy society by fostering equitable, affordable, and universally accessible healthcare [1][2]. Since 2005, the World Health Organization has encouraged nations to use digital health strategies in their health system [3]. With the proper implementation, digital health technologies can escalate the progress toward Universal Health Coverage and health-related Sustainable Development Goals [2][4].
The term “eHealth” denotes the digital health technologies or the use of emerging information and communication technologies (e.g., Internet, artificial intelligence, big data, mobile device) to improve health and the healthcare system [5][6][7]. There are several subdomains under its broad scope, including telehealth, telemedicine, mHealth, wearable healthcare devices, health information technologies, and robotic and personalized medicine [8][9]. These technologies have significantly dominated the health system by connecting patients, families, and healthcare providers and enhancing patient-centered care delivery. The world is also receiving help from eHealth to solve the increasing healthcare demand by the aging global population.
Moreover, the recent COVID-19 pandemic highlighted the benefits of telemedicine and other forms of e-medical care [10][11]. Given the rapid spread of the coronavirus from person to person during the COVID-19 pandemic, hospitals are overwhelmed with virus-infected patients. Governments imposed large-scale lockdowns across the countries to reduce social contact and further spread the virus. However, the news reported that these extensive lockdown measures inflicted the health system as patients cannot easily and timely access the healthcare providers. Thereby, eHealth technologies are mushrooming as they can alleviate the tremendous burden on medical resources and minimize the amount of person-to-person contact required for treatment [12][13][14].
In Southeast Asia, the enhancement of the eHealth strategy was designated as one of the significant public service priorities by the ASEAN Digital Master Plan 2025 [15]. Southeast Asian countries are increasingly taking up eHealth services. Furthermore, eHealth’s implementation fulfills consumers’ rising demand for better healthcare services, especially amid the COVID-19 pandemic [16][17][18][19].
2. Intellectual Structure of the eHealth Literature in Southeast Asia
Co-citation analysis measures the similarity between authors, documents, or journals in the field of study. It refers to the frequency with which two units are cited together. The fundamental assumption underlying this analysis is that the more two items are co-cited, the more likely their content is related [20][21]. By using VOSviewer software, this bibliometric review conducted author co-citation analysis (ACA) to identify the intellectual structure of eHealth in Southeast Asia.
Table 1 presents the highly co-cited authors in the eHealth in Southeast Asia literature. In addition, Figure 1 illustrates the ACA map by using the VOSviewer setting at a threshold of at least 23 author co-citations, which yielded a display of 86 scholars on the co-citation map. The size of the bubbles indicates the co-citation frequency. The larger the bubble means, the greater the scholars’ influence in the field of eHealth in Southeast Asia. The colored clusters represent schools of thought, which are the collection of items with similar theoretical perspectives and research interests. There are four distinct, coherent schools of thought in the literature on eHealth in Southeast Asia: “technology for healthcare and disease management” (red cluster with 39 items), “analysis and adoption of hospital information system/eHealth records” (green cluster with 22 items), “user intention and acceptance of information technology” (blue cluster with 15 items), and “m-Health” (yellow cluster with ten items).
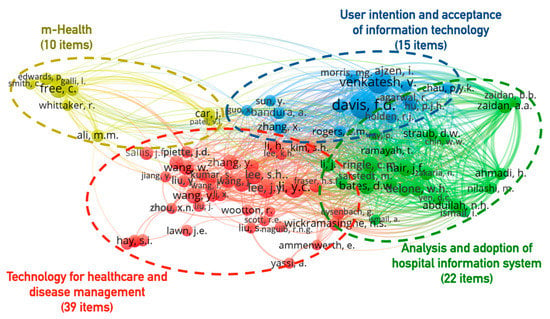
Figure 1. Four clusters representing the intellectual structure of eHealth in Southeast Asia (Threshold 23, Display 86 Authors).
Table 1. Highly co-cited authors in eHealth in Southeast Asia.
| Rank | Author | Nation | Co-Citation | Topical Focus |
|---|---|---|---|---|
| 1 | Davis, F.D. | United States | 112 | User intention and acceptance of IT |
| 2 | Venkatesh, V. | United States | 75 | User intention and acceptance of IT |
| 3 | Li, Y.C. | Taiwan | 70 | Technology for healthcare and disease management |
| 4 | Lee, J.Y. | United States | 58 | Technology for healthcare and disease management |
| 5 | Free, C. | United Kingdom | 53 | m-Health |
| 6 | Ajzen, I. | United States | 50 | User intention and acceptance of IT |
| 7 | Hair, J.F. | United States | 46 | Analysis and adoption of hospital information system |
| 8 | Ringle, C.M. | Germany | 45 | Analysis and adoption of hospital information system |
| 9 | Bates, D.W. | United States | 44 | Analysis and adoption of hospital information system |
| 10 | Lee, S.H. | United Kingdom | 44 | Technology for healthcare and disease management |
| 11 | Wang, Y. | Canada | 44 | Technology for healthcare and disease management |
| 12 | Wang, J. | United States | 42 | Technology for healthcare and disease management |
| 13 | Wang, W. | Singapore | 41 | Technology for healthcare and disease management |
| 14 | Zhang, Y. | China | 41 | Technology for healthcare and disease management |
| 15 | Delone, W.H. | United States | US | Analysis and adoption of hospital information system |
| 16 | Sarstedt, M. | Germany | 39 | Analysis and adoption of hospital information system |
| 17 | Zhang, J. | Singapore | 38 | Technology for healthcare and disease management |
| 18 | Li, H. | Finland | 36 | Technology for healthcare and disease management |
| 19 | Li, J. | Australia | 36 | Technology for healthcare and disease management |
| 20 | Zaidan, A.A. | Malaysia | 36 | Analysis and adoption of hospital information system |
The red cluster represents the technology for healthcare and disease management. Scholars associated with this school of thought investigated the factors related to the adoption and management of computer science and technology for health, physical activities, and disease management [22][23][24][25][26][27]. This is the biggest cluster, and many top co-cited authors (such as Li, Y.C., Lee, J.Y., Lee, S.H., Wang, Y., Wang, J., Wang, W., Zhang, Y., Zhang, J., Li, H., and Li, J.) are involved in this cluster. Studies of authors in this cluster highlighted that adopting eHealth technologies needs financial support and trust, organization structural support, leadership, and knowledge-sharing capacity [22][23][26][27]. These findings provide valuable implications for practitioners and researchers interested in adopting eHealth technologies.
The green cluster researches the “analysis and adoption of hospital information system/eHealth records”. Scholars working within this school of thought have studied frameworks for decision-making and adopting the hospital information system (HIS) at the organizational level [28][29][30][31]. Popular theories by these authors are the DeLone and McLean Model of information systems success [30] and the Technology–Organization–Environment–Human framework [28]. These theories were foundations for adopting hospital information systems research in Southeast Asia. In addition, Hair et al., who introduced multivariate data analysis [32], are also included in this cluster. Due to the centrality of his node position in the cluster, it may be interpreted that scholars frequently adopt this quantitative method in empirical research of hospital information system adoption.
The blue cluster studies “the user intention and acceptance of information technology”, included scholars such as Davis, Venkatesh, Ajzen, Agarwal, and Fishbein [33][34][35][36][37]. These scholars were linked because their research examines individual users’ attitudes, perceptions, and acceptance of IT adoption. Davis and Venkatesh, located in this cluster, were the top two co-cited authors in Table 1. Davis is the pioneer in developing the user acceptance of technology theory [35]. Venkatech collaborated with Davis and colleagues to build the UTAUT model, which is very useful for scholars, policymakers, and technology developers to determine the user acceptance of IT [37]. The findings of the top-cited document also suggested that the UTAUT model could be applied to health technology in Thailand [38].
Finally, the yellow cluster can be termed “m-Health”. This group is the smallest of the four schools of thought. However, it has a distinct character because this group of scholars has investigated the use of mobile health technologies or text messaging to deliver health promotion or control public health problems [39][40][41]. Along with the exponential increase in the number of mobile phone users in both high- and low-income countries, mobile phones are widely used in health information and healthcare delivery [42]. In Southeast Asia, m-Health has been used via text messaging or smartphone applications to remind health service appointments, to deliver messages for medication adherence, to prevent unhealthy activities such as smoking cessation, to assist in monitoring and self-management of chronic disorders such as hypertension and diabetes [42][43][44][45][46].
To summarize, co-citation analysis revealed four major schools of thought involved in the literature on eHealth in Southeast Asia from 1975 to 2021. This result can be used to analyze the evolution of the academic field in future studies.
3. Topical Foci of the eHealth in Southeast Asia Knowledge Base
Keyword co-occurrence analysis, also called co-word analysis, identifies key themes and topics within the eHealth in Southeast Asia knowledge base. Co-word analysis frequently identifies co-occurring words in the titles, abstracts, and indexes of documents in the review database [20]. This analysis would offer insight into broad topical trends within the literature.
Figure 2 shows the density map of the most frequently occurring keywords in the literature: healthcare delivery (316), telemedicine (308), health information system (243), medical information system (164), m-health (162), electronic health record (141), geographical information system (135), public health (124), hospital (120), elderly (115), organization and management (105), and covid-19 (100). These frequently occurring keywords offer insight into the subjects of studies that describe the eHealth in Southeast Asia knowledge base since its emergence in the past four decades.
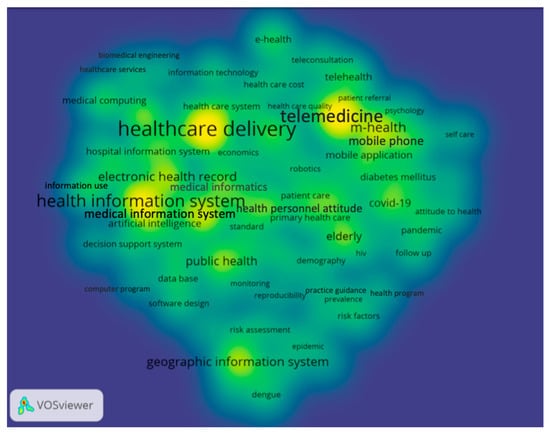
Figure 2. Keyword density heat map of the eHealth in Southeast Asia literature, 1975–2021 (Threshold 25 Occurrences, Display 94 Keywords).
In the next step, a temporal co-word map was generated in VOSviewer using a threshold of at least 25 occurrences (Figure 3). It synthesizes the time distribution of keywords based on the document publication date. The difference in colors indicates the different timeframe. Purple/darker bubbles are associated with topics popular in the earlier periods. In contrast, yellow/lighter-shaded bubbles are associated with the most recent topics in this research database.
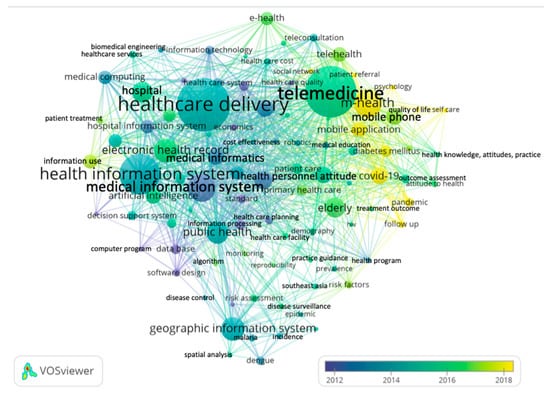
Figure 3. The temporal co-word map of the eHealth in Southeast Asia literature, 1975–2021 (Threshold 25 Occurrences, Display 94 Keywords).
The biggest bubbles, such as “healthcare delivery”, “telemedicine”, “health information system”, have darker colors, meaning that they were popular keywords in the earlier periods. However, this temporal co-word map also presents recent topics in the eHealth literature. The term “m-Health” is shown in the lighter bubble, and it is a relatively new topic emerging after the year 2018. Recent topics of interest among scholars are keywords such as “mobile application”, “social network”, “covid-19”, “pandemic”, “patient referral”, “follow up”, “self-care”, “quality of life”, “psychology”, “diabetes mellitus”, and “hypertension”. These findings, thus, confirm that the recent public health outbreak, the COVID-19 pandemic, accelerated the usage and application of new health technology in Southeast Asia, especially mobile health technology.
After the World Health Organization announced COVID-19 as a global pandemic in 2020, the world was alarmed by its rapid spread. Governments imposed large-scale lockdowns across the countries to reduce social contact and further spread the virus. The effect of this extensive lockdown is the acceleration of death by other diseases such as diabetes mellitus, hypertension, heart attack, and stroke because patients cannot easily and timely access healthcare providers. This issue highlighted the benefits of m-Health, telemedicine, and other forms of e-medical care to support and treat patients [10][11]. m-Health is defined as medical or public health practice supported by mobile devices [47]. m-Health is widely used to ensure patients connect with their healthcare providers virtually. They are integrated into medical treatment, such as daily monitoring of chronic diseases, psychological support for mental health, health promotion, enabling home care, and consequently enhancing the quality of life of people.
References
- Awad, A.; Trenfield, S.J.; Pollard, T.D.; Ong, J.J.; Elbadawi, M.; McCoubrey, L.E.; Goyanes, A.; Gaisford, S.; Basit, A.W. Connected healthcare: Improving patient care using digital health technologies. Adv. Drug Deliv. Rev. 2021, 178, 113958.
- Punnakitikashem, P.; Hallinger, P. Bibliometric Review of the Knowledge Base on Healthcare Management for Sustainability, 1994–2018. Sustainability 2019, 12, 205.
- World Health Organization. Global Strategy on Digital Health 2020–2025. 2020. Available online: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf (accessed on 2 January 2021).
- Novillo-Ortiz, D.; Marin, H.D.F.; Saigí-Rubió, F. The role of digital health in supporting the achievement of the Sustainable Development Goals (SDGs). Int. J. Med. Inform. 2018, 114, 106–107.
- Alvarez, R.C. The promise of e-Health–A Canadian perspective. eHealth Int. 2002, 1, 4.
- Black, A.D.; Car, J.; Pagliari, C.; Anandan, C.; Cresswell, K.; Bokun, T.; McKinstry, B.; Procter, R.; Majeed, A.; Sheikh, A. The Impact of eHealth on the Quality and Safety of Health Care: A Systematic Overview. PLoS Med. 2011, 8, e1000387.
- Oh, H.; Jadad, A.; Rizo, C.; Enkin, M.; Powell, J.; Pagliari, C. What Is eHealth (3): A Systematic Review of Published Definitions. J. Med Internet Res. 2005, 7, e110.
- Luk, C.Y. The impact of digital health on traditional healthcare systems and doctor-patient relationships: The case study of Singapore. In Innovative Perspectives on Public Administration in the Digital Age; IGI Global: Hershey, PA, USA, 2018; pp. 143–167.
- Penedo, F.J.; Oswald, L.B.; Kronenfeld, J.P.; Garcia, S.F.; Cella, D.; Yanez, B. The increasing value of eHealth in the delivery of patient-centred cancer care. Lancet Oncol. 2020, 21, e240–e251.
- Brørs, G.; Norman, C.D.; Norekvål, T.M. Accelerated importance of eHealth literacy in the COVID-19 outbreak and beyond. Eur. J. Cardiovasc. Nurs. 2020, 19, 458–461.
- Watson, A.R.; Wah, R.; Thamman, R. The Value of Remote Monitoring for the COVID-19 Pandemic. Telemed. e-Health 2020, 26, 1110–1112.
- Koonin, L.M.; Hoots, B.; Tsang, C.A.; Leroy, Z.; Farris, K.; Jolly, B.; Antall, P.; McCabe, B.; Zelis, C.B.; Tong, I. Trends in the Use of Telehealth during the Emergence of the COVID-19 Pandemic—United States, January–March 2020. Morb. Mortal. Wkly. Rep. Cent. Dis. Control. Prev. 2020, 69, 1595–1599. Available online: https://www.cdc.gov/mmwr/volumes/69/wr/mm6943a3.htm (accessed on 8 July 2022).
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193.
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962.
- The ASEAN Secretariat. Master Plan on ASEAN Connectivity 2025; The ASEAN Secretariat: Jakarta, Indonesia, 2016.
- Ang, I.Y.H.; Tan, K.X.Q.; Tan, C.; Tan, C.H.; Kwek, J.W.M.; Tay, J.; Toh, S.A. A Personalized Mobile Health Program for Type 2 Diabetes During the COVID-19 Pandemic: Single-Group Pre–Post Study. JMIR Diabetes 2021, 6, e25820.
- Le, H.T.; Nguyen, D.N.; Beydoun, A.S.; Le, X.T.T.; Nguyen, T.T.; Pham, Q.T.; Ta, N.T.K.; Nguyen, Q.T.; Nguyen, A.N.; Hoang, M.T.; et al. Demand for Health Information on COVID-19 among Vietnamese. Int. J. Environ. Res. Public Health 2020, 17, 4377.
- Lim, H.M.; Teo, C.H.; Ng, C.J.; Chiew, T.K.; Ng, W.L.; Abdullah, A.; Hadi, H.A.; Liew, C.S.; Chan, C.S. An Automated Patient Self-Monitoring System to Reduce Health Care System Burden During the COVID-19 Pandemic in Malaysia: Development and Implementation Study. JMIR Public Health Surveill. 2021, 9, e23427.
- Teh, H.L.; Suan, M.A.M.; Mohammed, N.S. Geriatric Telemedicine: Ensuring continuity of healthcare services to the older patients in Kedah, Malaysia during the COVID-19 pandemic. Med J. Malays. 2021, 76, 562–564.
- Zupic, I.; Čater, T. Bibliometric methods in management and organization. Organ. Res. Methods 2015, 18, 429–472.
- Small, H. Co-citation in the scientific literature: A new measure of the relationship between two documents. J. Am. Soc. Inf. Sci. 1973, 24, 265–269.
- Li, Y.-C.; Hung, M.-C.; Hsiao, S.-J.; Tsai, K.-D.; Chang, M.-M. An Assessment of Patient Safety in Acupuncture Process Under EMR Support. J. Med. Syst. 2010, 35, 1447–1453.
- Li, Y.-C.; Chang, I.-C.; Hung, W.-F.; Fu, H.-K. The Critical Factors Affecting Hospital Adoption of Mobile Nursing Technologies in Taiwan. In Proceedings of the 38th Annual Hawaii International Conference on System Sciences, Big Island, HI, USA, 6 January 2005; p. 157b.
- Jaana, M.; Sicotte, C.; Paré, G. Exploring Health Information Technology Innovativeness and its Antecedents in Canadian Hospitals. Methods Inf. Med. 2010, 49, 28–36.
- Wang, Y.; Liu, Z. Automatic detecting indicators for quality of health information on the Web. Int. J. Med. Inform. 2007, 76, 575–582.
- Wickramasinghe, N. IS/IT as a tool to achieve goal alignment. Int. J. Health Technol. Manag. 2000, 2, 163.
- Wickramasinghe, N.; Misra, S.K. A wireless trust model for healthcare. Int. J. Electron. Health 2004, 1, 60–77.
- Ahmadi, H.; Nilashi, M.; Shahmoradi, L.; Ibrahim, O. Hospital Information System adoption: Expert perspectives on an adoption framework for Malaysian public hospitals. Comput. Hum. Behav. 2017, 67, 161–189.
- Bates, D.W.; Gawande, A.A. Improving safety with information technology. N. Engl. J. Med. Mass Med. Soc. 2003, 348, 2526–2534.
- Delone, W.H.; McLean, E.R. The DeLone and McLean Model of Information Systems Success: A Ten-Year Update. J. Manag. Inf. Syst. 2003, 19, 9–30.
- Ismail, A.; Jamil, A.T.; Rahman, A.F.A.; Bakar, J.M.A.; Saad, N.M.; Saadi, H. The implementation of Hospital Information System (HIS) in tertiary hospitals in malaysia: A qualitative study. Malays. J. Public. Health Med. 2010, 10, 16–24.
- Hair, J.F. Multivariate Data Analysis: A Global Perspective, 7th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2009.
- Agarwal, R.; Prasad, J. The antecedents and consequents of user perceptions in information technology adoption. Decis. Support Syst. 1998, 22, 15–29.
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211.
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340.
- Fishbein, M.; Ajzen, I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Philos. Rhetor. 1977, 6, 244–245.
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478.
- Kijsanayotin, B.; Pannarunothai, S.; Speedie, S.M. Factors influencing health information technology adoption in Thailand’s community health centers: Applying the UTAUT model. Int. J. Med. Inform. 2009, 78, 404–416.
- Chib, A.; van Velthoven, M.H.; Car, J. mHealth Adoption in Low-Resource Environments: A Review of the Use of Mobile Healthcare in Developing Countries. J. Health Commun. 2014, 20, 4–34.
- Free, C.; Phillips, G.; Galli, L.; Watson, L.; Felix, L.; Edwards, P.; Patel, V.; Haines, A. The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review. PLoS Med. 2013, 10, e1001362.
- Whittaker, R.; McRobbie, H.; Bullen, C.; Rodgers, A.; Gu, Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2016, 4, CD006611.
- Van Do, V.; Spears, C.A.; Van Minh, H.; Huang, J.; Redmon, P.B.; Long, N.X.; Eriksen, M.P. Perceptions about mindfulness and text messaging for smoking cessation in Vietnam: Results from a qualitative study. JMIR mHealth uHealth 2020, 8, e17337.
- Bal, P.; Shamsir, S.; Warid, N.; Yahya, A.; Yunus, J.; Supriyanto, E.; Ngim, C.F. MHealth application: Mobile thalassemia patient management application. In Proceedings of the 2014 IEEE Conference on Biomedical Engineering and Sciences (IECBES), Kuala Lumpur, Malaysia, 8–10 December 2014; IEEE: Piscataway, NJ, USA, 2014; pp. 792–796.
- DeSilva, M.; Vu, C.N.; Bonawitz, R.; Hai, L.T.; Van Lam, N.; Yen, L.T.; Gifford, A.L.; Haberer, J.; Linh, D.T.; Sabin, L. The Supporting Adolescent Adherence in Vietnam (SAAV) study: Study protocol for a randomized controlled trial assessing an mHealth approach to improving adherence for adolescents living with HIV in Vietnam. Trials 2019, 20, 150.
- Liverani, M.; Ir, P.; Wiseman, V.; Perel, P. User experiences and perceptions of health wearables: An exploratory study in Cambodia. Glob. Health Res. Policy 2021, 6, 33.
- Suwanthara, J.; Noinongyao, A.; Vittayakorn, S. WiseMed: Medication reminder for seniors. In Proceedings of the 2019 23rd International Computer Science and Engineering Conference (ICSEC), Phuket, Thailand, 30 October–1 November 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 409–414.
- Becker, S.; Miron-Shatz, T.; Schumacher, N.; Krocza, J.; Diamantidis, C.; Albrecht, U.-V. mHealth 2.0: Experiences, possibilities, and perspectives. JMIR mHealth uHealth 2014, 2, e3328.
More
Information
Subjects:
Management
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
913
Revisions:
2 times
(View History)
Update Date:
27 Feb 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




