
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Natalia A. Shnayder | -- | 1880 | 2023-02-03 09:41:38 | | | |
| 2 | Jessie Wu | Meta information modification | 1880 | 2023-02-03 09:57:49 | | | | |
| 3 | Jessie Wu | Meta information modification | 1880 | 2023-02-03 09:58:57 | | | | |
| 4 | Jessie Wu | + 2 word(s) | 1882 | 2023-02-03 09:59:50 | | |
Video Upload Options
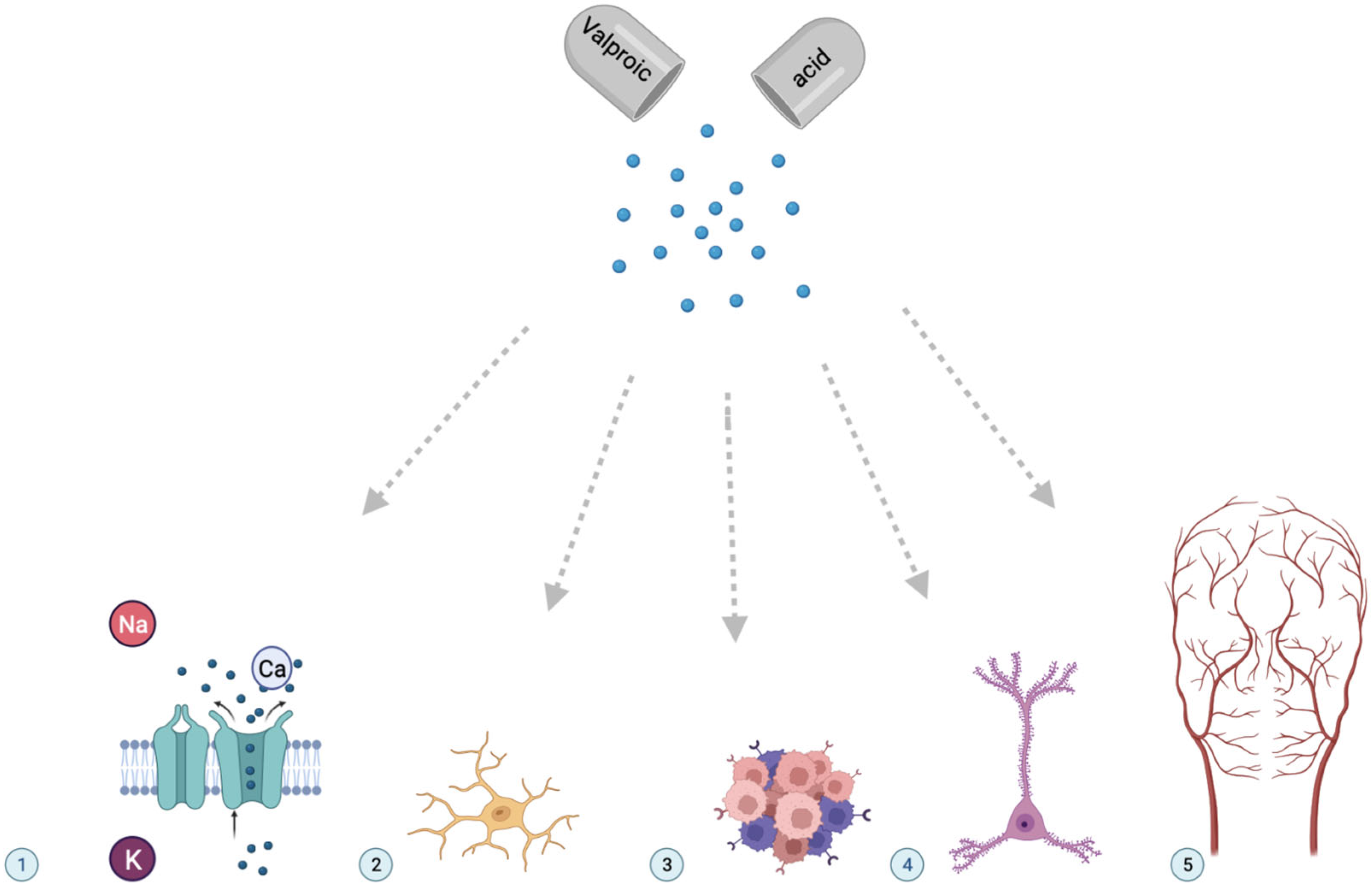
Valproic acid (CH3CH2CH2)2CHCOOH 2-propylvaleric acid, VPA) is a fatty acid derivative originally synthesized. Valproic acid (VPA) and its salts are psychotropic drugs that are widely used in neurological diseases (epilepsy, neuropathic pain, migraine, etc.) and psychiatric disorders (schizophrenia, bipolar affective disorder, addiction diseases, etc.). In addition, the indications for the appointment of valproate have been expanding in recent years in connection with the study of new mechanisms of action of therapeutic and toxic metabolites of VPA in the human body. Thus, VPA is considered a component of disease-modifying therapy for multiple tumors, neurodegenerative diseases (Huntington’s disease, Parkinson’s disease, Duchenne progressive dystrophy, etc.), and human immunodeficiency syndrome. The metabolism of VPA is complex and continues to be studied. Known pathways of VPA metabolism include: β-oxidation in the tricarboxylic acid cycle (acetylation); oxidation with the participation of cytochrome P-450 isoenzymes (P-oxidation); and glucuronidation. The complex metabolism of VPA explains the diversity of its active and inactive metabolites, which have therapeutic, neutral, or toxic effects.
1. Therapeutic Metabolites of Valproic Acid
| Metabolite | HMDB Number | Clinical Effect |
References |
|---|---|---|---|
| VPA-glucuronide | 0000901 | Therapeutic Neutral |
[5][6] |
| 2-n-propyl-2-pentenoic acid | 0013902 | Therapeutic | [7] |
| Valproyl-CoA | 0013115 | Therapeutic | [8] |
| 4-ene-VPA | 0013897 | Therapeutic | [9] |
| 2-ene-VPA | 0013902 | Therapeutic | [9] |
| Metabolite | HMDB Number | Clinical Effect |
References |
|---|---|---|---|
| VPA-glucuronide | 0000901 | Therapeutic Neutral |
[5][6] |
| 2-n-propyl-2-pentenoic acid | 0013902 | Therapeutic | [7] |
| 4-ene-VPA | 0013897 | Therapeutic | [8] |
| 2-ene-VPA | 0013902 | Therapeutic | [9] |
1.1. Valproate Acid Glucuronide
1.2. 2-N-Propyl-2-Pentenoic Acid
1.3. Valproyl-CoA
1.4. 4-Ene-Valproic Acid
1.5. 2-Ene-Valproic Acid
2. Role of Therapeutic Metabolites of Valproic Acid
References
- Siemes, H.; Nau, H.; Schultze, K.; Wittfoht, W.; Drews, E.; Penzien, J.; Seidel, U. Valproate (VPA) metabolites in various clinical conditions of probable VPA-associated hepatotoxicity. Epilepsia 1993, 34, 332–346.
- Ghodke-Puranik, Y.; Thorn, C.F.; Lamba, J.K.; Leeder, J.S.; Song, W.; Birnbaum, A.K.; Altman, R.B.; Klein, T.E. Valproic acid pathway: Pharmacokinetics and pharmacodynamics. Pharm. Genom. 2013, 23, 236–241.
- Beger, R.D.; Schmidt, M.A.; Kaddurah-Daouk, R. Current Concepts in Pharmacometabolomics, Biomarker Discovery, and Precision Medicine. Metabolites 2020, 10, 129.
- Wishart, D.S.; Guo, A.; Oler, E.; Wang, F.; Anjum, A.; Peters, H.; Dizon, R.; Sayeeda, Z.; Tian, S.; Lee, B.L.; et al. HMDB 5.0: The Human Metabolome Database for 2022. Nucleic Acids Res. 2022, 50, D622–D631.
- Perucca, E. Pharmacological and therapeutic properties of valproate: A summary after 35 years of clinical experience. CNS Drugs. 2002, 16, 695–714.
- Suzuki, E.; Yamamura, N.; Ogura, Y.; Nakai, D.; Kubota, K.; Kobayashi, N.; Miura, S.; Okazaki, O. Identification of valproic acid glucuronide hydrolase as a key enzyme for the interaction of valproic acid with carbapenem antibiotics. Drug Metab. Dispos. 2010, 38, 1538–1544.
- Silva, M.F.; Ruiter, J.P.; IJlst, L.; Jakobs, C.; Duran, M.; de Almeida, I.T.; Wanders, R.J. Differential effect of valproate and its Delta2- and Delta4-unsaturated metabolites, on the beta-oxidation rate of long-chain and medium-chain fatty acids. Chem. Biol. Interact. 2001, 137, 203–212.
- Friel, P. Valproyl CoA: An active metabolite of valproate? Med. Hypotheses 1990, 31, 31–32.
- Eyal, S.; Yagen, B.; Shimshoni, J.; Bialer, M. Histone deacetylases inhibition and tumor cells cytotoxicity by CNS-active VPA constitutional isomers and derivatives. Biochem. Pharmacol. 2005, 69, 1501–1508.
- Ehlers, K.; Stürje, H.; Merker, H.J.; Nau, H. The valproic acid metabolite E-2-n-propyl-2-pentenoic acid does not induce spina bifida in the mouse. Dev. Pharmacol. Ther. 1992, 19, 196–204.
- Kim, T.; Song, S.; Park, Y.; Kang, S.; Seo, H. HDAC Inhibition by Valproic Acid Induces Neuroprotection and Improvement of PD-like Behaviors in LRRK2 R1441G Transgenic Mice. Exp. Neurobiol. 2019, 28, 504–515.
- Chateauvieux, S.; Morceau, F.; Dicato, M.; Diederich, M. Molecular and therapeutic potential and toxicity of valproic acid. J. Biomed. Biotechnol. 2010, 2010, 479364.
- Zádori, D.; Geisz, A.; Vámos, E.; Vécsei, L.; Klivényi, P. Valproate ameliorates the survival and the motor performance in a transgenic mouse model of Huntington’s disease. Pharmacol. Biochem. Behav. 2009, 94, 148–153.
- Binvignat, O.; Olloquequi, J. Excitotoxicity as a Target Against Neurodegenerative Processes. Curr. Pharm. Des. 2020, 26, 1251–1262.
- Scheuing, L.; Chiu, C.T.; Liao, H.M.; Linares, G.R.; Chuang, D.M. Preclinical and clinical investigations of mood stabilizers for Huntington’s disease: What have we learned? Int. J. Biol. Sci. 2014, 10, 1024–1038.
- Soria-Castro, R.; Schcolnik-Cabrera, A.; Rodríguez-López, G.; Campillo-Navarro, M.; Puebla-Osorio, N.; Estrada-Parra, S.; Estrada-García, I.; Chacón-Salinas, R.; Chávez-Blanco, A.D. Exploring the Drug Repurposing Versatility of Valproic Acid as a Multifunctional Regulator of Innate and Adaptive Immune Cells. J. Immunol. Res. 2019, 2019, 9678098.
- Reis, K.P.; Sperling, L.E.; Teixeira, C.; Sommer, L.; Colombo, M.; Koester, L.S.; Pranke, P. VPA/PLGA microfibers produced by coaxial electrospinning for the treatment of central nervous system injury. Braz. J. Med. Biol. Res. 2020, 53, e8993.
- Chen, S.; Ye, J.; Chen, X.; Shi, J.; Wu, W.; Lin, W.; Lin, W.; Li, Y.; Fu, H.; Li, S. Valproic acid attenuates traumatic spinal cord injury-induced inflammation via STAT1 and NF-κB pathway dependent of HDAC3. J. Neuroinflammation. 2018, 15, 150.
- Heers, H.; Stanislaw, J.; Harrelson, J.; Lee, M.W. Valproic acid as an adjunctive therapeutic agent for the treatment of breast cancer. Eur. J. Pharmacol. 2018, 835, 61–74.
- Scholz, B.; Schulte, J.S.; Hamer, S.; Himmler, K.; Pluteanu, F.; Seidl, M.D.; Stein, J.; Wardelmann, E.; Hammer, E.; Völker, U.; et al. HDAC (Histone Deacetylase) Inhibitor Valproic Acid Attenuates Atrial Remodeling and Delays the Onset of Atrial Fibrillation in Mice. Circ. Arrhythm. Electrophysiol. 2019, 12, e007071.




