Valproic acid (CH3CH2CH2)2CHCOOH 2-propylvaleric acid, VPA) is a fatty acid derivative originally synthesized. Valproic acid (VPA) and its salts are psychotropic drugs that are widely used in neurological diseases (epilepsy, neuropathic pain, migraine, etc.) and psychiatric disorders (schizophrenia, bipolar affective disorder, addiction diseases, etc.). In addition, the indications for the appointment of valproate have been expanding in recent years in connection with the study of new mechanisms of action of therapeutic and toxic metabolites of VPA in the human body. Thus, VPA is considered a component of disease-modifying therapy for multiple tumors, neurodegenerative diseases (Huntington’s disease, Parkinson’s disease, Duchenne progressive dystrophy, etc.), and human immunodeficiency syndrome. The metabolism of VPA is complex and continues to be studied. Known pathways of VPA metabolism include: β-oxidation in the tricarboxylic acid cycle (acetylation); oxidation with the participation of cytochrome P-450 isoenzymes (P-oxidation); and glucuronidation. The complex metabolism of VPA explains the diversity of its active and inactive metabolites, which have therapeutic, neutral, or toxic effects.
1. Therapeutic Metabolites of Valproic Acid
A metabolite is any substance formed during metabolism (digestion or other chemical processes in the body)
[1][94]. In addition, the term “metabolite” refers to substances that remain (circulate in the blood, accumulate in organs and tissues, excreted in the urine) after the drug is broken down (metabolized) by the body
[2][95]. Research into therapeutic metabolites of
valproic acid (VPA
) has been ongoing for many years. Such studies have intensified over the past decade due to the rapid development of a new direction in personalized medicine—pharmacometabolomics
[3][96]. The number of studied VPA metabolites is close to fifty
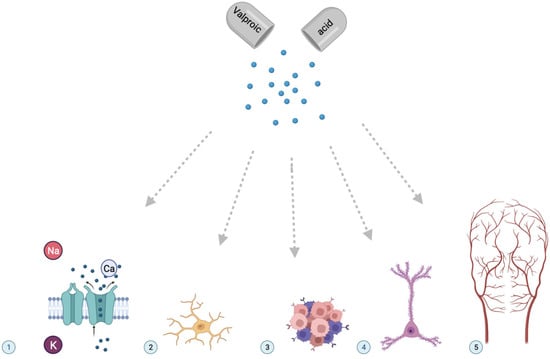
[4][97], but their clinical role (
Figure 1) in the expected therapeutic response to valproate has not yet been sufficiently studied for many of them.
The most studied therapeutic metabolites of VPA in the blood and urine are presented in Table 1 and Table 2.
1.1. Valproate Acid Glucuronide
Valproate acid glucuronide (VPAG) is a glucuronidation product of VPA. It is known that VPAG is the main metabolite of VPA excreted in the urine (30–50% of the dose). With the age of the patient, the level of this metabolite in the blood does not change, despite the known decrease in liver weight
[4][97].
1.2. 2-N-Propyl-2-Pentenoic Acid
2-n-propyl-2-pentenoic acid is also known as 2,4-diene VPA. This VPA metabolite is formed in the body by glucuronidation. This therapeutic metabolite of VPA exhibits a high antiepileptic potential similar to VPA, but it has a low teratogenic potential
[10][102], which is of undoubted clinical interest.
1.3. Valproyl-CoA
Valproyl-CoA is a therapeutic metabolite of VPA, which is formed by the metabolism of VPA as a result of β-oxidation (acetylation) in the Krebs cycle
[8][100]. Previously, this metabolite was found in liver cells (hepatocytes), but recent work has shown that valproyl-CoA can accumulate in brain neurons as a result of normal fatty acid turnover processes. Valproil-CoA is a therapeutic metabolite and increases the antiepileptic activity of VPA by stimulating the activity of Na+, K+-ATPase at low concentrations of adenosine triphosphate in the brain
[8][100].
1.4. 4-Ene-Valproic Acid
It is known that 4-ene-valproic acid (4-ene-VPA) belongs to the class of organic compounds known as methyl-branched fatty acids. These are fatty acids with an acyl chain having a methyl branch. Usually, they are saturated and contain only one or several methyl groups
[9][101]. However, other branches than the methyl branch may also be present. In addition, 4-ene-VPA is a very hydrophobic molecule; it is practically insoluble (in water) but refers to relatively neutral VPA metabolites, although this opinion is debatable. Several studies have demonstrated that 4-ene-VPA has an antiepileptic effect and also inhibits HDACs, which is a promising direction in the treatment of cancer, autoimmune disease, and acquired immunodeficiency syndrome
[4][97]. 4-ene-VPA circulates in the blood and is excreted in the urine, which facilitates the study of its level in biological fluids of the human body.
1.5. 2-Ene-Valproic Acid
2-ene-valproic acid (2-ene-VPA) is a product of P-oxidation metabolism in hepatocytes. This therapeutic metabolite of VPA belongs to a class of organic compounds known as methyl-branched fatty acids. In addition, it inhibits HDACs, which is a promising direction in the treatment of cancer, autoimmune disease, and acquired immunodeficiency syndrome
[9][101].
2. Role of Therapeutic Metabolites of Valproic Acid
Thus, VPA is a derivative of fatty acids and HDACs of classes I and IIa
[11][103], which allows VPA and its active metabolites to regulate the expression of various genes
[11][103]. In addition, pathophysiological processes include both excitotoxicity of VPA metabolites and a decrease in gene transcription due to a decrease in the level of histone acetylation, which is accompanied by a loss of GABAergic (gamma-aminobutyric acid) neurons in the striatum as a pathological hallmark of Huntington’s disease
[12][13][13,104]. VPA is known to exert neuroprotective effects through these primary targets. Excitotoxicity is a mechanism of cell death caused by hyperactivation of excitatory amino acid receptors, which increases the ion permeability of the cell membrane and leads to an overload of intracellular calcium
[14][105]. Notably, VPA and its active metabolites also strongly induce 70 kilo dalton heat shock proteins through epigenetic mechanisms, reducing infarct volume and improving functional recovery in rodents subjected to cerebral ischemia
[15][106]. HDAC1 has been implicated in reducing the human immunodeficiency viruses’ activity in infected cells. The inhibitory effect of VPA metabolites on this protein makes it a good candidate for acquired immunodeficiency syndrome therapy
[16][107].
Neuroprotective effects of VPA therapeutic metabolites have been reported in a wide range of acute central nervous system injury models, including post-traumatic inflammation caused by spinal cord injury
[17][108]. The results of the studies demonstrated that VPA and its therapeutic metabolites promote the phenotypic shift of microglia from the M1 phenotype to the M2 phenotype and inhibited microglial activation, thereby reducing the level of pro-inflammatory factors caused by spinal cord injury. The increase in acetylation of signal transducer and activator of transcription 1/ nuclear factor-κB (STAT1/NF-κB pathway) during VPA treatment was probably caused by HDAC3 translocation to the nucleus and its activity. In addition, VPA and its therapeutic metabolites have been shown to downregulate HDAC3 expression and activity and increase acetylation of STAT1 as well as NF-κB p65 after spinal cord injury. The acetylation status of NF-kB p65 and the complex with nuclear factor kappa-light-chain-enhancer of activated B cells NF-κB (NF-κB) p65 and STAT1 suppressed the transcriptional activity of NF-kB p65 and attenuated the central inflammatory response mediated by microglia and led to the neuroprotective effect of VPA therapeutic metabolites
[18][109].
As mentioned earlier, VPA has been described as an HDAC, which makes it possible to consider not only the well-known therapeutic metabolites of VPA, but also the toxic metabolites of VPA, as promising potential therapeutic agents for the treatment of various forms of cancer and leukemia
[19][110]. Chromatin is formed from DNA packaged in nucleosome structures of 146 base pairs of DNA wound around a histone octamer (two copies of each histone: H2A, H2B, H3, and H4) held in place by histone H1. In terms of transcription, the condensed form of chromatin (heterochromatin) is inactive. In contrast, the decondensed form (euchromatin) corresponds to the active form. The transition between euchromatin and heterochromatin depends on two families of proteins: histone acetyltransferases and HDACs. It has been established that histone acetylation leads to relaxation of the nucleosome structure, releasing DNA and allowing activation of transcription. Inhibition of HDAC promotes the formation of decondensed chromatin, thereby promoting gene expression
[12][13]. The toxic metabolites of VPA are among the most promising molecules because, unlike other drugs that target the expression of a molecule or family of molecules, they target chromatin through associated proteins: HDAC; deoxyribonucleic acid methyltransferase; heterochromatin protein 1; and smooth muscle cells. Thus, toxic VPA metabolites affect the expression of many proteins and therefore can be considered as therapeutic and applicable to a wide range of neurodegenerative diseases and autoimmune diseases, as well as multiple tumors and leukemia, where these VPA metabolites repress many antioncogenes during carcinogenesis
[12][13].
Parkinson’s disease is caused by the degeneration of nigrostriatal dopaminergic neurons. No direct effect of VPA on Parkinson’s disease has been shown, but in vitro studies have shown a positive effect of active VPA metabolites in animal models that mimic Parkinson’s disease at various levels. VPA and its active metabolites prevent rotenone-induced apoptosis, protect neurons from the dopaminergic toxin 1-methyl-phenylpyridinium, stimulate the release of neutrophils from neuroglial cells, protect cultured dopaminergic neurons from degeneration caused by excessive microglial activation by stimulating microglial apoptosis, and protect neurons, increasing the expression of α-synuclein and preventing its monoubiquitination and nuclear translocation
[12][13]. Experiments on an animal model of Parkinson’s disease (rodents) have shown that selective changes in α-synuclein induced by rotenone (a decrease in native protein and an increase in monoubiquitination in substantia nigra and striatum) can be reduced with long-term administration of VPA
[13][104]. However, there is still no convincing answer to the question about which of the active metabolites of VPA are the most promising molecules for the treatment of Parkinson’s disease and other neurodegenerative diseases, including Huntington’s disease and Alzheimer’s disease.
The role of active VPA metabolites in the treatment of primary muscular dystrophy (eg., Duchenne muscular dystrophy) has been demonstrated in vitro and in vivo in
mdx/utrn-/- knockout mice. It has been shown that VPA therapeutic metabolites are able to induce the Akt/mTOR/p70S6K pathway through the induction of phosphatidylinositol-3-OH kinase, which leads to a decrease in collagen content and fibrosis in skeletal muscles, a decrease in hind limb contractures, an increase in the integrity of the myocyte sarcolemma, a decrease in the number CD8-positive inflammatory cells, and an increase in the level of activated Akt in the skeletal muscles of experimental animals
[12][13].
Additionally, therapeutic metabolites of VPA have the potential to delay the development of atrial remodeling in patients from the risk group. Therapeutic metabolites of VPA have been shown to attenuate many components of atrial remodeling that are present in transgenic mice, animal models, and humans. However, VPA therapeutic metabolites significantly reduced atrial dilatation, cardiomyocyte enlargement, atrial fibrosis, and myocyte ultrastructure disorganization. In addition, it was demonstrated that these metabolites significantly reduced the occurrence of atrial thrombi and reduced the severity of negative changes in the action potential of cardiomyocytes
[20][111]. An increase in H4 histone acetylation in the atria of VPA-treated transgenic mice confirmed the efficacy of HDAC inhibition in vivo. Cardiomyocyte-specific genetic inactivation of HDAC2 in transgenic mice attenuated ultrastructural myocyte disorganization comparable to VPA. Finally, in transgenic mice, VPA therapeutic metabolites restrain dysregulation of proteins that are involved in multiple pathways associated with atrial fibrillation, such as oxidative phosphorylation or RhoA (Ras homolog gene family, member A) signaling, and disease functions such as cardiac fibrosis and muscle cells apoptosis
[20][111].