
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Mohd Imran | -- | 3237 | 2023-01-11 09:46:00 | | | |
| 2 | Peter Tang | Meta information modification | 3237 | 2023-01-11 10:05:49 | | |
Video Upload Options
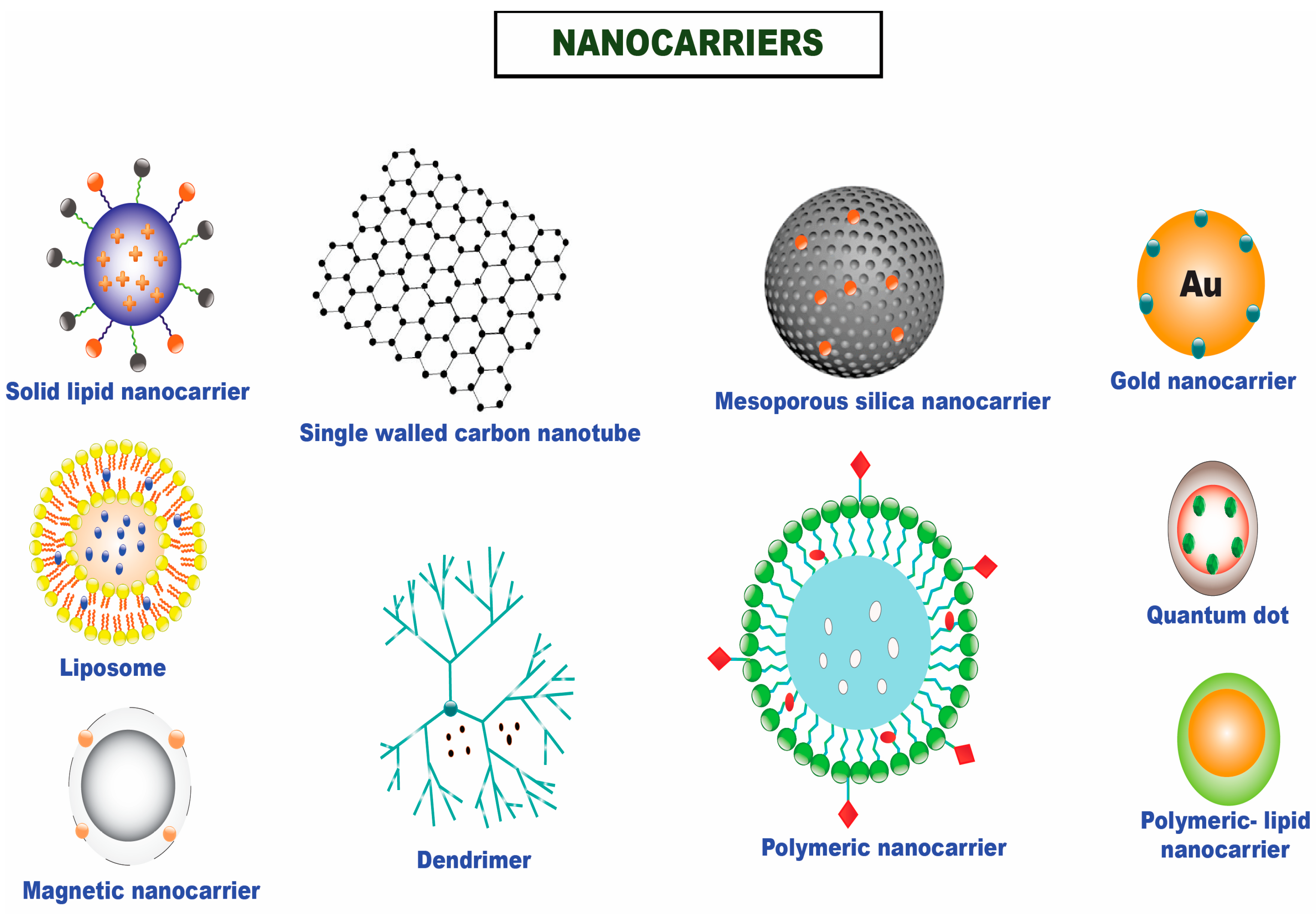
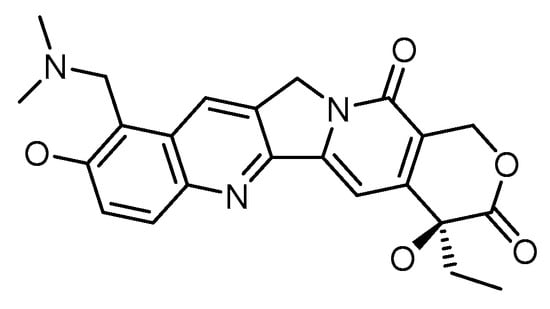
Chemotherapy has been the predominant treatment modality for cancer patients, but its overall performance is still modest. Difficulty in penetration of tumor tissues, a toxic profile in high doses, multidrug resistance in an array of tumor types, and the differential architecture of tumor cells as they grow are some of the bottlenecks associated with the clinical usage of chemotherapeutics. Advances in tumor biology understanding and the emergence of novel targeted drug delivery tools leveraging various nanosystems offer hope for developing effective cancer treatments. Topotecan is a topoisomerase I inhibitor that stabilizes the transient TOPO I-DNA cleavable complex, leading to single-stranded breaks in DNA. Due to its novel mechanism of action, TOPO is reported to be active against various carcinomas, namely small cell lung cancer, cervical cancer, breast cancer, and ovarian cancer. Issues of cross-resistance with numerous drugs, rapid conversion to its inactive form in biological systems, appended adverse effects, and higher water solubility limit its therapeutic efficacy in clinical settings. Topotecan nanoformulations offer several benefits for enhancing the therapeutic action of this significant class of chemotherapeutics. The likelihood that the target cancer cells will be exposed to the chemotherapeutic drug while in the drug-sensitive s-phase is increased due to the slow and sustained release of the chemotherapeutic, which could provide for a sustained duration of exposure of the target cancer cells to the bioavailable drug and result in the desired therapeutic outcome.
1. Introduction
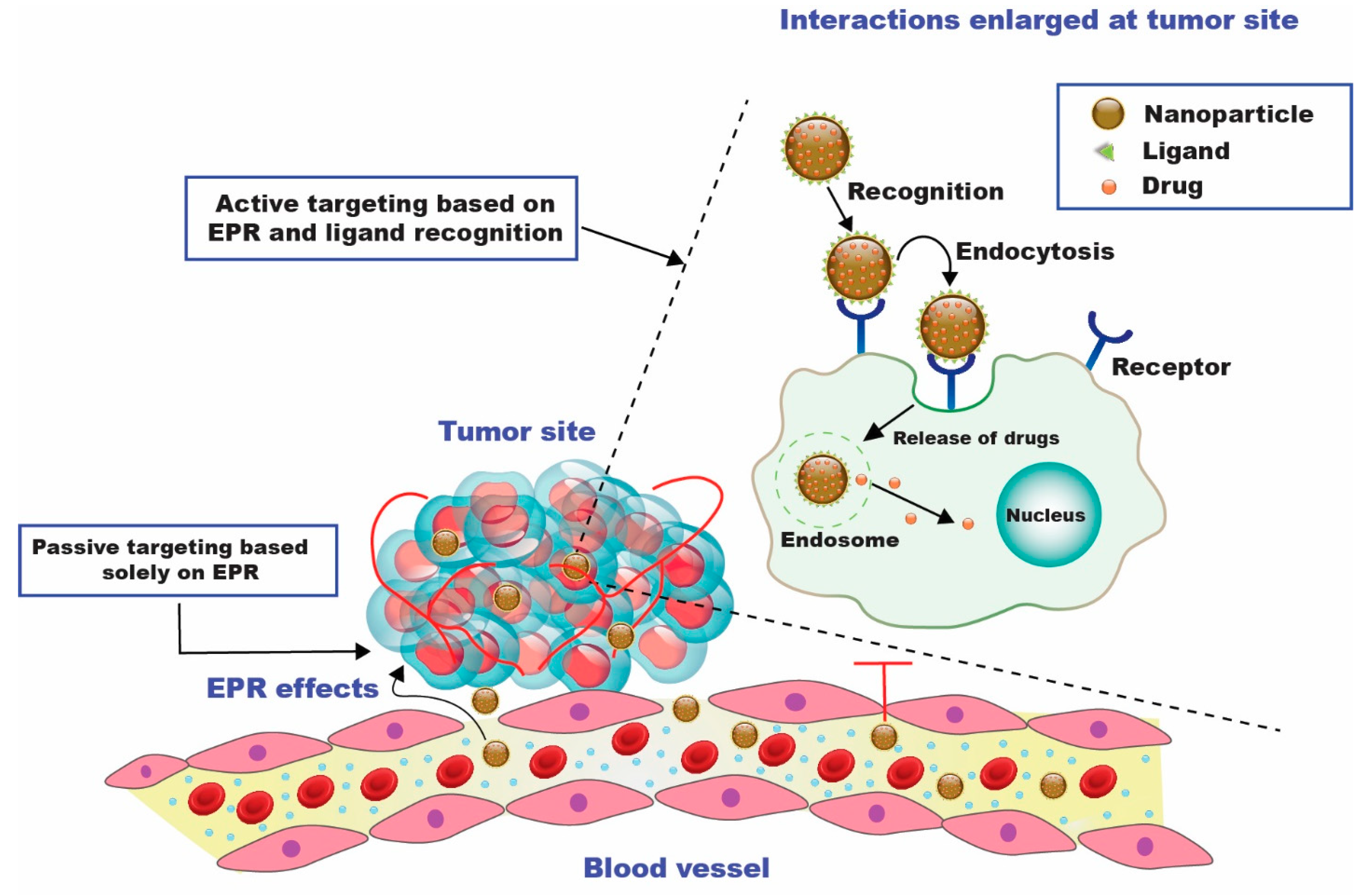
2. Passive Targeted Delivery Approach for Topotecan
3. Active Targeting
4. Combinatorial Drug Therapy Employing Topotecan

References
- Garg, P. Selective Preference of Antibody Mimetics over Antibody, as Binding Molecules, for Diagnostic and Therapeutic Applications in Cancer Therapy. Biointerface Res. Appl. Chem. 2021, 11, 10679–10689.
- Arifin, M.Z.; Parikesit, A.A.; Agustriawan, D. Molecular Simulation of MDM2 and E6AP Proteins as P53 Regulator in Cervical Cancer. Biointerface Res. Appl. Chem. 2020, 10, 5875–5879.
- Alavi, M.; Nokhodchi, A. Micro- and Nanoformulations of Paclitaxel Based on Micelles, Liposomes, Cubosomes, and Lipid Nanoparticles: Recent Advances and Challenges. Drug Discov. Today 2022, 27, 576–584.
- Abdelaziz, H.M.; Gaber, M.; Abd-Elwakil, M.M.; Mabrouk, M.T.; Elgohary, M.M.; Kamel, N.M.; Kabary, D.M.; Freag, M.S.; Samaha, M.W.; Mortada, S.M.; et al. Inhalable Particulate Drug Delivery Systems for Lung Cancer Therapy: Nanoparticles, Microparticles, Nanocomposites and Nanoaggregates. J. Control. Release 2018, 269, 374–392.
- Verma, D.; Thakur, P.S.; Padhi, S.; Khuroo, T.; Talegaonkar, S.; Iqbal, Z. Design Expert Assisted Nanoformulation Design for Co-Delivery of Topotecan and Thymoquinone: Optimization, in Vitro Characterization and Stability Assessment. J. Mol. Liq. 2017, 242, 382–394.
- Curcio, M.; Diaz-Gomez, L.; Cirillo, G.; Nicoletta, F.P.; Leggio, A.; Iemma, F. Dual-Targeted Hyaluronic Acid/Albumin Micelle-Like Nanoparticles for the Vectorization of Doxorubicin. Pharmaceutics 2021, 13, 304.
- Padhi, S.; Behera, A. Nanotechnology Based Targeting Strategies for the Delivery of Camptothecin. Sustain. Agric. Rev. 2020, 44, 243–272.
- Kundu, A.; Padhi, S.; Behera, A.; Hasnain, M.S.; Nayak, A.K. Tumor Targeting Strategies by Chitosan-Based Nanocarriers. In Chitosan in Biomedical Applications; Academic Press: Cambridge, MA, USA, 2022; pp. 163–188.
- Behera, A.; Mittu, B.; Padhi, S.; Singh, A. Antimicrobial Efficacy of Essential Oil Nanoemulsions. In Nanotechnological Approaches in Food Microbiology; CRC Press: Boca Raton, FL, USA, 2020; pp. 293–309.
- Hassan, N.; Firdaus, S.; Padhi, S.; Ali, A.; Iqbal, Z. Investigating Natural Antibiofilm Components: A New Therapeutic Perspective against Candidal Vulvovaginitis. Med. Hypotheses 2021, 148, 110515.
- Behera, A.; Patra, N.; Mittu, B.; Padhi, S.; Singh, J. Bimetallic Nanoparticles: Green Synthesis, Applications, and Future Perspectives. In Multifunctional Hybrid Nanomaterials for Sustainable Agri-food and Ecosystems; Elsevier: Amsterdam, The Netherlands, 2020; pp. 639–682.
- Padhi, S.; Behera, A. Advanced Drug Delivery Systems in the Treatment of Ovarian Cancer. In Advanced Drug Delivery Systems in the Management of Cancer; Academic Press: Cambridge, MA, USA, 2021; pp. 127–139.
- Behera, A.; Padhi, S.; Nayak, A.K. Engineered Liposomes as Drug Delivery and Imaging Agents. Des. Appl. Theranostic. Nanomed. 2022, 75.
- Padhi, S.; Mirza, M.A.; Verma, D.; Khuroo, T.; Panda, A.K.; Talegaonkar, S.; Khar, R.K.; Iqbal, Z. Revisiting the Nanoformulation Design Approach for Effective Delivery of Topotecan in Its Stable Form: An Appraisal of Its in Vitro Behavior and Tumor Amelioration Potential. Drug Deliv. 2015, 23, 2827–2837.
- Patnaik, S.; Gorain, B.; Padhi, S.; Choudhury, H.; Gabr, G.A.; Md, S.; Kumar, M.D.; Kesharwani, P. Recent Update of Toxicity Aspects of Nanoparticulate Systems for Drug Delivery. Eur. J. Pharm. Biopharm. 2021, 161, 100–119.
- Padhi, S.; Behera, A.; Hasnain, M.S.; Nayak, A.K. Chitosan-Based Drug Delivery Systems in Cancer Therapeutics. Chitosan. Drug Deliv. 2022, 159–193.
- Padhi, S.; Dash, M.; Behera, A. Nanophytochemicals for the Treatment of Type II Diabetes Mellitus: A Review. Environ. Chem. Lett. 2021, 19, 4349–4373.
- Padhi, S.; Nayak, A.K.; Behera, A. Type II Diabetes Mellitus: A Review on Recent Drug Based Therapeutics. Biomed. Pharmacother. 2020, 131, 110708.
- De La Torre, P.; Jesús Pérez-Lorenzo, M.; Alcázar-Garrido, Á.; Flores, A.I.; Baeza, A.; Novio, F.; Paris, J.L. Cell-Based Nanoparticles Delivery Systems for Targeted Cancer Therapy: Lessons from Anti-Angiogenesis Treatments. Molecules 2020, 25, 715.
- Navya, P.N.; Kaphle, A.; Srinivas, S.P.; Bhargava, S.K.; Rotello, V.M.; Daima, H.K. Current Trends and Challenges in Cancer Management and Therapy Using Designer Nanomaterials. Nano Converg. 2019, 6, 1–30.
- Dehshahri, A.; Ashrafizadeh, M.; Ghasemipour, A.E.; Pardakhty, A.; Mandegary, A.; Mohammadinejad, R.; Sethi, G. Topoisomerase Inhibitors: Pharmacology and Emerging Nanoscale Delivery Systems. Pharmacol. Res. 2020, 151, 104551.
- Chen, A.Y.; Choy, H.; Rothenberg, M.L. DNA Topoisomerase I-Targeting Drugs as Radiation Sensitizers. Oncology 1999, 13, 39–46.
- Carmeliet, P.; Jain, R.K. Angiogenesis in Cancer and Other Diseases. Nature 2000, 407, 249–257.
- Behera, A.; Padhi, S. Passive and Active Targeting Strategies for the Delivery of the Camptothecin Anticancer Drug: A Review. Environ. Chem. Lett. 2020, 18, 1557–1567.
- Lim, E.-K.; Chung, B.H.; Chung, S.J. Recent Advances in PH-Sensitive Polymeric Nanoparticles for Smart Drug Delivery in Cancer Therapy. Curr. Drug Targets 2016, 19, 300–317.
- Martínez-Carmona, M.; Lozano, D.; Colilla, M.; Vallet-Regí, M. Selective Topotecan Delivery to Cancer Cells by Targeted PH-Sensitive Mesoporous Silica Nanoparticles. RSC Adv. 2016, 6, 50923–50932.
- Patankar, N.A.; Waterhouse, D.; Strutt, D.; Anantha, M.; Bally, M.B. Topophore C: A Liposomal Nanoparticle Formulation of Topotecan for Treatment of Ovarian Cancer. Investig. New Drugs 2012, 31, 46–58.
- Drummond, D.C.; Noble, C.O.; Guo, Z.; Hayes, M.E.; Connolly-Ingram, C.; Gabriel, B.S.; Hann, B.; Liu, B.; Park, J.W.; Hong, K.; et al. Development of a Highly Stable and Targetable Nanoliposomal Formulation of Topotecan. J. Control. Release 2010, 141, 13–21.
- Padhi, S.; Kapoor, R.; Verma, D.; Panda, A.K.; Iqbal, Z. Formulation and Optimization of Topotecan Nanoparticles: In Vitro Characterization, Cytotoxicity, Cellular Uptake and Pharmacokinetic Outcomes. J. Photochem. Photobiol. B Biol. 2018, 183, 222–232.
- Venâncio, J.H.; Andrade, L.M.; Esteves, N.L.S.; Brito, L.B.; Valadares, M.C.; Oliveira, G.A.R.; Lima, E.M.; Marreto, R.N.; Gratieri, T.; Taveira, S.F. Topotecan-Loaded Lipid Nanoparticles as a Viable Tool for the Topical Treatment of Skin Cancers. J. Pharm. Pharmacol. 2017, 69, 1318–1326.
- Xing, R.; Mustapha, O.; Ali, T.; Rehman, M.; Zaidi, S.S.; Baseer, A.; Batool, S.; Mukhtiar, M.; Shafique, S.; Malik, M.; et al. Development, Characterization, and Evaluation of SLN-Loaded Thermoresponsive Hydrogel System of Topotecan as Biological Macromolecule for Colorectal Delivery. Biomed. Res. Int. 2021, 2021, 1–14.
- Jeong, S.H.; Jang, J.H.; Lee, Y.B. Oral Delivery of Topotecan in Polymeric Nanoparticles: Lymphatic Distribution and Pharmacokinetics. J. Control. Release 2021, 335, 86–102.
- Egeblad, M.; Nakasone, E.S.; Werb, Z. Tumors as Organs: Complex Tissues That Interface with the Entire Organism. Dev. Cell 2010, 18, 884–901.
- Ediriwickrema, A.; Saltzman, W.M. Nanotherapy for Cancer: Targeting and Multifunctionality in the Future of Cancer Therapies. ACS Biomater. Sci. Eng. 2015, 1, 64–78.
- Lee, K.Y.; Seow, E.; Zhang, Y.; Lim, Y.C. Targeting CCL21-Folic Acid-Upconversion Nanoparticles Conjugates to Folate Receptor-α Expressing Tumor Cells in an Endothelial-Tumor Cell Bilayer Model. Biomaterials 2013, 34, 4860–4871.
- Vaillant, O.; Cheikh, K.E.; Warther, D.; Brevet, D.; Maynadier, M.; Bouffard, E.; Salgues, F.; Jeanjean, A.; Puche, P.; Mazerolles, C.; et al. Mannose-6-Phosphate Receptor: A Target for Theranostics of Prostate Cancer. Angew. Chem. Int. Ed. 2015, 54, 5952–5956.
- Yang, K.S.; Budin, G.; Tassa, C.; Kister, O.; Weissleder, R. Bioorthogonal Approach to Identify Unsuspected Drug Targets in Live Cells. Angew. Chem. 2013, 125, 10787–10791.
- Qu, W.; Meng, B.; Yu, Y.; Wang, S. Folic Acid-Conjugated Mesoporous Silica Nanoparticles for Enhanced Therapeutic Efficacy of Topotecan in Retina Cancers. Int. J. Nanomed. 2018, 13, 4379.
- Yoon, S.; Kim, Y.; Youn, Y.S.; Oh, K.T.; Kim, D.; Lee, E.S. Transferrin-Conjugated PH-Responsive γ-Cyclodextrin Nanoparticles for Antitumoral Topotecan Delivery. Pharmaceutics 2020, 12, 1109.
- Mokhtari, R.B.; Homayouni, T.S.; Baluch, N.; Morgatskaya, E.; Kumar, S.; Das, B.; Yeger, H. Combination Therapy in Combating Cancer. Oncotarget 2017, 8, 38022.
- Mokhtari, R.B.; Kumar, S.; Islam, S.S.; Yazdanpanah, M.; Adeli, K.; Cutz, E.; Yeger, H. Combination of Carbonic Anhydrase Inhibitor, Acetazolamide, and Sulforaphane, Reduces the Viability and Growth of Bronchial Carcinoid Cell Lines. BMC Cancer 2013, 13, 1–18.
- Kumar, R.; Chaudhary, K.; Gupta, S.; Singh, H.; Kumar, S.; Gautam, A.; Kapoor, P.; Raghava, G.P.S. CancerDR: Cancer drug resistance database. Sci. Rep. 2013, 3, 1445.
- Du, J.; Lu, W.L.; Ying, X.; Liu, Y.; Du, P.; Tian, W.; Men, Y.; Guo, J.; Zhang, Y.; Li, R.J.; et al. Dual-Targeting Topotecan Liposomes Modified with Tamoxifen and Wheat Germ Agglutinin Significantly Improve Drug Transport across the Blood-Brain Barrier and Survival of Brain Tumor-Bearing Animals. Mol. Pharm. 2009, 6, 905–917.
- Jain, A.; Jain, S.K. Multipronged, Strategic Delivery of Paclitaxel-Topotecan Using Engineered Liposomes to Ovarian Cancer. Drug Dev. Ind. Pharm. 2015, 42, 136–149.
- Khuroo, T.; Verma, D.; Talegaonkar, S.; Padhi, S.; Panda, A.K.; Iqbal, Z. Topotecan–Tamoxifen Duple PLGA Polymeric Nanoparticles: Investigation of in Vitro, in Vivo and Cellular Uptake Potential. Int. J. Pharm. 2014, 473, 384–394.




