
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sathish Kumar Natarajan | -- | 1867 | 2023-01-05 15:36:23 | | | |
| 2 | Camila Xu | Meta information modification | 1867 | 2023-01-06 01:43:14 | | | | |
| 3 | Sathish Kumar Natarajan | + 505 word(s) | 2372 | 2023-01-06 16:10:03 | | | | |
| 4 | Camila Xu | Meta information modification | 2372 | 2023-01-09 01:27:02 | | |
Video Upload Options
Zika virus (ZIKV) is a Flavivirus and was first isolated in a sentinel monkey kept for studying mosquito-borne diseases, and was also later isolated from Aedes africanus mosquitoes, confirming its vector-borne transmission, in the Ziika forest of Uganda.
1. Introduction
2. ZIKV Epidemiology
2.1. ZIKV Strains
2.2. Transmission of ZIKV
2.3. ZIKV Structure
| Protein | Function |
|---|---|
| Envelope (E) | Host cell binding and membrane fusion [38] |
| Capsid | Viral protein surrounds nucleic acid [39] |
| Membrane protein | Proteolytic cleavage of a pre membrane protein from membrane protein in the Golgi apparatus results in the release of the virus [40] |
| NS1 | RNA replication [41] |
| NS2A | Modulates different components of the virus during assembly [42] |
| NS2B | Cofactor of NS3 protease [43] |
| NS3 | Protease and helicase domain for polyprotein possessing & nucleoside triphosphtase (NTPase)/RNA triphosphatase (RTPase) activities [43] |
| NS4A | Evasion of the innate immune response, associated with replication complex [44][45] |
| NS4B | Evasion of the innate immune response [46] |
| NS5 | Methyl transferase (MTase) and RNA dependent RNA polymerase (RdRp) [47] |
2.4. ZIKV Replication
2.5. Clinical Findings and Congenital Zika Syndrome
2.6. Diagnosis, Treatment, and Prevention of ZIKV Infection
2.7. ZIKV Vaccines and Drug Development
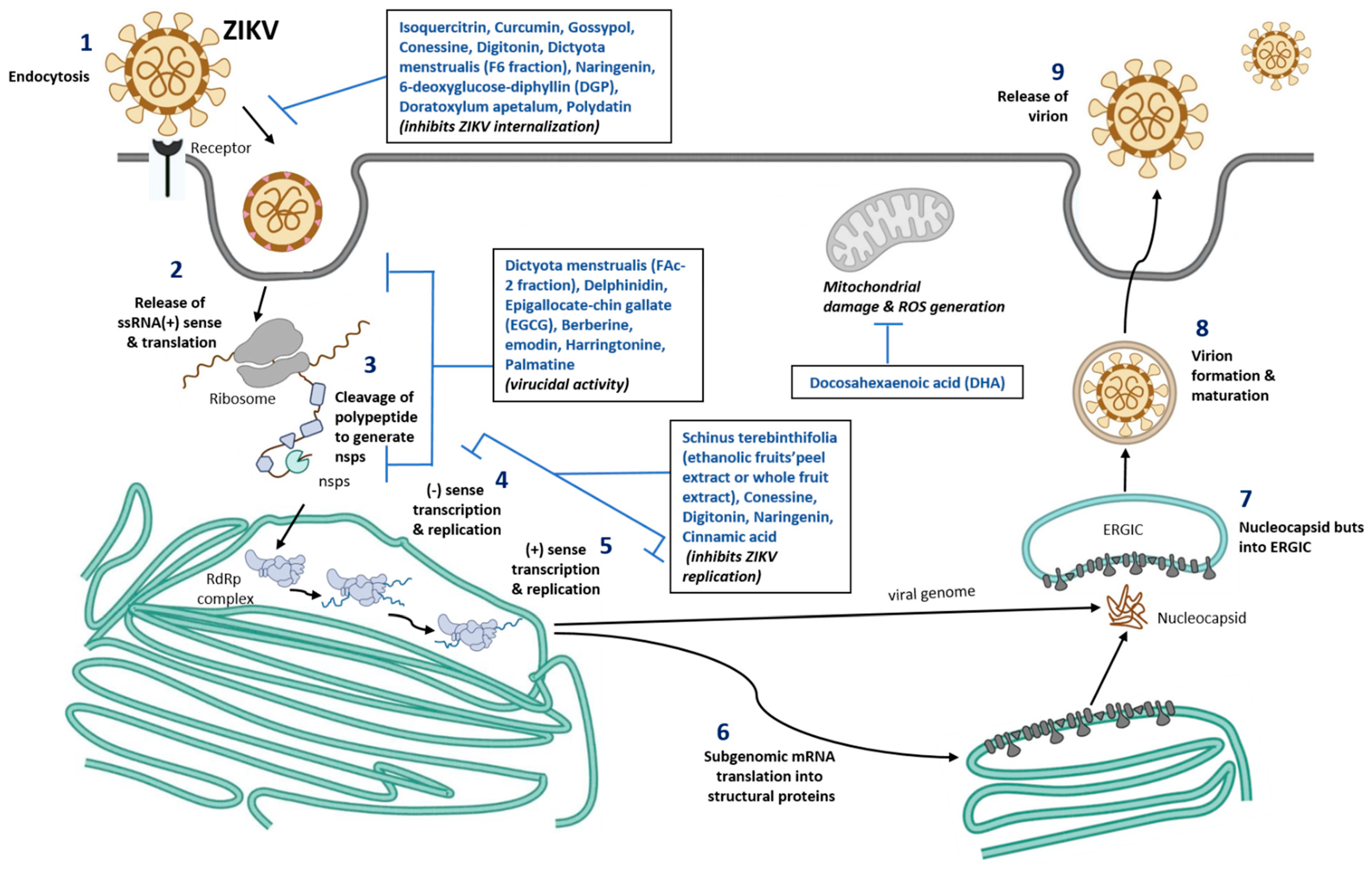
Table 2. List of novel nutrient molecules and mechanism of protection against ZIKV infection.
|
Nutrient Molecule |
ZIKV Strain |
Cells |
Result |
Ref.No. |
|
Schinus terebinthifolia, Ethanolic fruits’peel extract (STPE) and whole fruits extract (STWFE) |
MR766 (African Strain) or PE243 (EH) ZIKV strains with 1 MOI |
HTR-8/SVneo cells |
Potential early antiviral effect, inhibited ZIKV entry |
|
|
Isoquercitrin |
PF-25013-18 (2 MOI for A549), and ZIKV MR766MC, viral clone derived African strain MR766-NIID (1 MOI for A549, Huh-7 and 10 MOI for SHSY5Y) |
A549, Huh-7, SH-SY5Y |
Potential inhibitor of ZIKV infection in different human cells tested |
[78] |
|
Curcumin (Pretreatment) |
HD78788 with 0.1, 1, and 1 MOI |
HeLa, BHK-21, and Vero-E |
Decreased ZIKV infection in a time and dose dependent manner |
[79] |
|
Gossypol, digitonin, and conessine |
PAN2016, R116265, PAN2015, FLR, R103451, PRVABC59, PLCal_ZV, IbH 30656, mosquito strain MEX 2–81, and African strain (MR 766) |
Vero E6 cells |
Compared to conessine and digitonin, gossypol exhibited the strong inhibitory activity against 10 different ZIKV strains |
[80] |
|
Dictyota menstrualis (F-6 and FAc-2 fractions) |
MR 766 with 0.01-1 MOI |
Vero cells |
Dose-dependent inhibition of ZIKV replication (>74%) |
[81] |
|
Polyphenols—Delphinidin (D) and Epigallocate-chin gallate (EGCG) |
African MR766 and the American PA259459 with ~106 PFU |
Vero cells |
D and EGCG shows virucidal effect which decreases the ZIKV infection The virucidal of D and EGCG was higher in MR766 compared to PA259459 strain |
|
|
Berberine and emodin |
Brazilian Zika virus strain isolated from a febrile patient in northeast Brazil with 106 PFU/ml |
Vero E6 cells |
Induces virucidal effect and decreases the ZIKV infection: 160 µM of berberine decreases infectivity by 77.6%, whereas 40 µM of emodin decreases by 83.3%. |
[84] |
|
Harringtonine |
PRVABC59 |
African Green Monkey Kidney cells |
Inhibits ZIKV entry, replication and virion release |
[85] |
|
Palmatine |
ATCC VR-1843 |
Vero cells |
Prevents ZIKV binding and entry |
[86] |
|
Cinnamic acid |
Asian ZIKV |
Vero cells, Huh7, A549 |
Prevent ZIKV replication |
[87] |
|
Naringenin (NAR) Treatment after infection |
Viruses isolated from serum of infected patients in South Brazil (2016) and Northeast (2015). Human A549 lung epithelial cells: ZIKV (ZV BR 2015/15261, ZV BR 2016/16288, ZV BR 2015/15098, ZIKV PE243, ZIKV MR766) with 0.1 MOI Human monocyte-derived dendritic cells: ZIKV (ZV BR 2015/15261) with 10 MOI |
In vitro NAR was effective against distinct ZIKV lineages (Asian and African) and seems to act during the late phase of the viral life cycle |
[88] |
|
|
6-deoxyglucose-diphyllin (DGP) |
HT1080, VERO, and CHME3 cells with ZIKV-MR766 and ZIKV-RVPs at ~1 MOI. CHME3 cells with PRVABC59, BeH819015, IBH30656, and DAK-ArD-41524 with 1, 0.2, 0.2 and 0.5 MOI, respectively |
Inhibits both in vitro and in vivo ZIKV infection |
[89] |
|
|
Doratoxylum apetalum |
A549, clinical isolate PF-25013-18 of ZIKV (ZIKV- PF13) with 2 MOI Huh7.5 cells, Brazilian strain (ZIKV-BR) with 2 MOI Recombinant Zika virus expressing the GFP reporter gene (ZIKVGFP) |
Anti-ZIKV activity with non-cytotoxic concentration in human cell lines |
[90] |
|
|
Docosahexaenoic acid (DHA) |
SH-SY5Y, ZIKVPE243 with 10 MOI |
DHA shows neuroprotective and anti-inflammatory potential |
[91] |
|
|
Polydatin (natural precursor of resveratrol and commonly found in grape, peanut etc.) |
Computational based approach: Molecular docking of phytochemical compounds against NS5 or RdRp, RNA dependent RNA polymerase |
Out of 5000 phytochemicals screened, Polydatin shows the best binding interaction with NS5 RNA dependent RNA polymerase active site with docking score -18.71 kcal/mol. Compared to sofosbuvir, Polydatin has more capacity for the receptor binding |
[75] |
|
References
- Dick, G.W.; Kitchen, S.F.; Haddow, A.J. Zika virus. I. Isolations and serological specificity. Trans. R. Soc. Trop. Med. Hyg. 1952, 46, 509–520.
- Dick, G.W.A. Zika virus (II). Pathogenicity and physical properties. Trans. R. Soc. Trop. Med. Hyg. 1952, 46, 521–534.
- Simpson, D.I.H. Zika virus infection in man. Trans. R. Soc. Trop. Med. Hyg. 1964, 58, 335–338.
- Smith, D.E.; Beckham, J.D.; Tyler, K.L.; Pastula, D.M. Zika virus disease for neurologists. Neurol. Clin. Pract. 2016, 6, 515–522.
- Duffy, M.R.; Chen, T.H.; Hancock, W.T.; Powers, A.M.; Kool, J.L.; Lanciotti, R.S.; Pretrick, M.; Marfel, M.; Holzbauer, S.; Dubray, C.; et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N. Engl. J. Med. 2009, 360, 2536–2543.
- Cao-Lormeau, V.-M.; Roche, C.; Teissier, A.; Robin, E.; Berry, A.-L.; Mallet, H.-P.; Sall, A.A.; Musso, D. Zika virus, French polynesia, South pacific, 2013. Emerg. Infect. Dis. 2014, 20, 1085–1086.
- Oehler, E.; Watrin, L.; Larre, P.; Leparc-Goffart, I.; Lastere, S.; Valour, F.; Baudouin, L.; Mallet, H.; Musso, D.; Ghawche, F. Zika virus infection complicated by Guillain-Barre syndrome--case report, French Polynesia, December 2013. Euro Surveill. Bull. Eur. Mal. Transm. = Eur. Commun. Dis. Bull. 2014, 19, 20720.
- Musso, D.; Gubler, D.J. Zika Virus. Clin. Microbiol. Rev. 2016, 29, 487–524.
- Kama, M.; Aubry, M.; Naivalu, T.; Vanhomwegen, J.; Mariteragi-Helle, T.; Teissier, A.; Paoaafaite, T.; Hue, S.; Hibberd, M.L.; Manuguerra, J.C.; et al. Sustained Low-Level Transmission of Zika and Chikungunya Viruses after Emergence in the Fiji Islands. Emerg. Infect. Dis. 2019, 25, 1535–1538.
- Calvez, E.; Mousson, L.; Vazeille, M.; O’Connor, O.; Cao-Lormeau, V.-M.; Mathieu-Daudé, F.; Pocquet, N.; Failloux, A.-B.; Dupont-Rouzeyrol, M. Zika virus outbreak in the Pacific: Vector competence of regional vectors. PLoS Negl. Trop. Dis. 2018, 12, e0006637.
- Delatorre, E.; Fernandez, J.; Bello, G. Investigating the Role of Easter Island in Migration of Zika Virus from South Pacific to Americas. Emerg. Infect. Dis. 2018, 24, 2119–2121.
- Pettersson, J.H.O.; Eldholm, V.; Seligman, S.J.; Lundkvist, Å.; Falconar, A.K.; Gaunt, M.W.; Musso, D.; Nougairède, A.; Charrel, R.; Gould, E.A.; et al. How Did Zika Virus Emerge in the Pacific Islands and Latin America? mBio 2016, 7, e01239-16.
- Metsky, H.C.; Matranga, C.B.; Wohl, S.; Schaffner, S.F.; Freije, C.A.; Winnicki, S.M.; West, K.; Qu, J.; Baniecki, M.L.; Gladden-Young, A.; et al. Zika virus evolution and spread in the Americas. Nature 2017, 546, 411–415.
- Likos, A.; Griffin, I.; Bingham, A.M.; Stanek, D.; Fischer, M.; White, S.; Hamilton, J.; Eisenstein, L.; Atrubin, D.; Mulay, P.; et al. Local Mosquito-Borne Transmission of Zika Virus—Miami-Dade and Broward Counties, Florida, June-August 2016. MMWR. Morb. Mortal. Wkly. Rep. 2016, 65, 1032–1038.
- Beaver, J.T.; Lelutiu, N.; Habib, R.; Skountzou, I. Evolution of Two Major Zika Virus Lineages: Implications for Pathology, Immune Response, and Vaccine Development. Front. Immunol. 2018, 9, 1640.
- Haddow, A.D.; Schuh, A.J.; Yasuda, C.Y.; Kasper, M.R.; Heang, V.; Huy, R.; Guzman, H.; Tesh, R.B.; Weaver, S.C. Genetic characterization of Zika virus strains: Geographic expansion of the Asian lineage. PLoS Negl. Trop. Dis. 2012, 6, e1477.
- Sheridan, M.A.; Balaraman, V.; Schust, D.J.; Ezashi, T.; Roberts, R.M.; Franz, A.W.E. African and Asian strains of Zika virus differ in their ability to infect and lyse primitive human placental trophoblast. PLoS ONE 2018, 13, e0200086.
- Enfissi, A.; Codrington, J.; Roosblad, J.; Kazanji, M.; Rousset, D. Zika virus genome from the Americas. Lancet 2016, 387, 227–228.
- Musso, D. Zika Virus Transmission from French Polynesia to Brazil. Emerg. Infect. Dis. 2015, 21, 1887.
- Li, M.I.; Wong, P.S.; Ng, L.C.; Tan, C.H. Oral susceptibility of Singapore Aedes (Stegomyia) aegypti (Linnaeus) to Zika virus. PLoS Negl. Trop. Dis. 2012, 6, e1792.
- Foy, B.D.; Kobylinski, K.C.; Chilson Foy, J.L.; Blitvich, B.J.; Travassos da Rosa, A.; Haddow, A.D.; Lanciotti, R.S.; Tesh, R.B. Probable non-vector-borne transmission of Zika virus, Colorado, USA. Emerg. Infect. Dis. 2011, 17, 880–882.
- Mead, P.S.; Duggal, N.K.; Hook, S.A.; Delorey, M.; Fischer, M.; Olzenak McGuire, D.; Becksted, H.; Max, R.J.; Anishchenko, M.; Schwartz, A.M.; et al. Zika Virus Shedding in Semen of Symptomatic Infected Men. N. Engl. J. Med. 2018, 378, 1377–1385.
- Müller, J.A.; Harms, M.; Krüger, F.; Groß, R.; Joas, S.; Hayn, M.; Dietz, A.N.; Lippold, S.; von Einem, J.; Schubert, A.; et al. Semen inhibits Zika virus infection of cells and tissues from the anogenital region. Nat. Commun. 2018, 9, 2207.
- Sharma, A.; Lal, S.K. Zika Virus: Transmission, Detection, Control, and Prevention. Front. Microbiol. 2017, 8, 110.
- Elizondo-Quiroga, D.; Medina-Sánchez, A.; Sánchez-González, J.M.; Eckert, K.A.; Villalobos-Sánchez, E.; Navarro-Zúñiga, A.R.; Sánchez-Tejeda, G.; Correa-Morales, F.; González-Acosta, C.; Arias, C.F.; et al. Zika Virus in Salivary Glands of Five Different Species of Wild-Caught Mosquitoes from Mexico. Sci. Rep. 2018, 8, 809.
- Mourya, D.T.; Gokhale, M.D.; Majumdar, T.D.; Yadav, P.D.; Kumar, V.; Mavale, M.S. Experimental Zika virus infection in Aedes aegypti: Susceptibility, transmission & co-infection with dengue & chikungunya viruses. Indian J. Med. Res. 2018, 147, 88–96.
- Routhu, N.K.; Byrareddy, S.N. Host-Virus Interaction of ZIKA Virus in Modulating Disease Pathogenesis. J. Neuroimmune Pharm. 2017, 12, 219–232.
- Newman, C.; Friedrich, T.C.; O’Connor, D.H. Macaque monkeys in Zika virus research: 1947-present. Curr. Opin. Virol. 2017, 25, 34–40.
- Althouse, B.M.; Vasilakis, N.; Sall, A.A.; Diallo, M.; Weaver, S.C.; Hanley, K.A. Potential for Zika Virus to Establish a Sylvatic Transmission Cycle in the Americas. PLoS Negl. Trop. Dis. 2016, 10, e0005055.
- Terzian, A.C.B.; Zini, N.; Sacchetto, L.; Rocha, R.F.; Parra, M.C.P.; Del Sarto, J.L.; Dias, A.C.F.; Coutinho, F.; Rayra, J.; da Silva, R.A.; et al. Evidence of natural Zika virus infection in neotropical non-human primates in Brazil. Sci. Rep. 2018, 8, 16034.
- Passi, D.; Sharma, S.; Dutta, S.R.; Ahmed, M. Zika Virus Diseases—The New Face of an Ancient Enemy as Global Public Health Emergency (2016): Brief Review and Recent Updates. Int. J. Prev. Med. 2017, 8, 6.
- Sirohi, D.; Chen, Z.; Sun, L.; Klose, T.; Pierson, T.C.; Rossmann, M.G.; Kuhn, R.J. The 3.8 Å resolution cryo-EM structure of Zika virus. Science 2016, 352, 467–470.
- Basile, K.; Kok, J.; Dwyer, D.E. Zika virus: What, where from and where to? Pathology 2017, 49, 698–706.
- Faye, O.; Freire, C.C.; Iamarino, A.; Faye, O.; de Oliveira, J.V.; Diallo, M.; Zanotto, P.M.; Sall, A.A. Molecular evolution of Zika virus during its emergence in the 20(th) century. PLoS Negl. Trop. Dis. 2014, 8, e2636.
- Lee, I.; Bos, S.; Li, G.; Wang, S.; Gadea, G.; Desprès, P.; Zhao, R.Y. Probing Molecular Insights into Zika Virus⁻Host Interactions. Viruses 2018, 10, 233.
- Lindenbach, B.D.; Rice, C.M. Molecular biology of flaviviruses. Adv. Virus Res. 2003, 59, 23–61.
- Sironi, M.; Forni, D.; Clerici, M.; Cagliani, R. Nonstructural Proteins Are Preferential Positive Selection Targets in Zika Virus and Related Flaviviruses. PLoS Negl. Trop. Dis. 2016, 10, e0004978.
- Chellasamy, S.K.; Devarajan, S. Identification of Potential Lead Molecules for Zika Envelope Protein from In Silico Perspective. Avicenna J. Med. Biotechnol. 2019, 11, 94–103.
- Tan, T.Y.; Fibriansah, G.; Kostyuchenko, V.A.; Ng, T.-S.; Lim, X.-X.; Zhang, S.; Lim, X.-N.; Wang, J.; Shi, J.; Morais, M.C.; et al. Capsid protein structure in Zika virus reveals the flavivirus assembly process. Nat. Commun. 2020, 11, 895.
- Nambala, P.; Su, W.-C. Role of Zika Virus prM Protein in Viral Pathogenicity and Use in Vaccine Development. Front. Microbiol. 2018, 9, 1797.
- Moreira-Soto, A.; de Souza Sampaio, G.; Pedroso, C.; Postigo-Hidalgo, I.; Berneck, B.S.; Ulbert, S.; Brites, C.; Netto, E.M.; Drexler, J.F. Rapid decline of Zika virus NS1 antigen-specific antibody responses, northeastern Brazil. Virus Genes 2020, 56, 632–637.
- Zhang, X.; Xie, X.; Zou, J.; Xia, H.; Shan, C.; Chen, X.; Shi, P.Y. Genetic and biochemical characterizations of Zika virus NS2A protein. Emerg. Microbes Infect. 2019, 8, 585–602.
- Hilgenfeld, R.; Lei, J.; Zhang, L. The Structure of the Zik.ka Virus Protease, NS2B/NS3pro. In Dengue and Zika: Control and Antiviral Treatment Strategies; Hilgenfeld, R., Vasudevan, S.G., Eds.; Springer: Singapore, 2018; pp. 131–145.
- Hu, Y.; Dong, X.; He, Z.; Wu, Y.; Zhang, S.; Lin, J.; Yang, Y.; Chen, J.; An, S.; Yin, Y.; et al. Zika virus antagonizes interferon response in patients and disrupts RIG-I–MAVS interaction through its CARD-TM domains. Cell Biosci. 2019, 9, 46.
- Rodriguez, A.K.; Muñoz, A.L.; Segura, N.A.; Rangel, H.R.; Bello, F. Molecular characteristics and replication mechanism of dengue, zika and chikungunya arboviruses, and their treatments with natural extracts from plants: An updated review. EXCLI J. 2019, 18, 988–1006.
- Ngueyen, T.T.N.; Kim, S.J.; Lee, J.Y.; Myoung, J. Zika Virus Proteins NS2A and NS4A Are Major Antagonists that Reduce IFN-β Promoter Activity Induced by the MDA5/RIG-I Signaling Pathway. J. Microbiol. Biotechnol. 2019, 29, 1665–1674.
- Wang, B.; Thurmond, S.; Hai, R.; Song, J. Structure and function of Zika virus NS5 protein: Perspectives for drug design. Cell. Mol. Life Sci. CMLS 2018, 75, 1723–1736.
- Routhu, N.K.; Lehoux, S.D.; Rouse, E.A.; Bidokhti, M.R.M.; Giron, L.B.; Anzurez, A.; Reid, S.P.; Abdel-Mohsen, M.; Cummings, R.D.; Byrareddy, S.N. Glycosylation of Zika Virus is Important in Host-Virus Interaction and Pathogenic Potential. Int. J. Mol. Sci. 2019, 20, 5206.
- Šebera, J.; Dubankova, A.; Sychrovský, V.; Ruzek, D.; Boura, E.; Nencka, R. The structural model of Zika virus RNA-dependent RNA polymerase in complex with RNA for rational design of novel nucleotide inhibitors. Sci. Rep. 2018, 8, 11132.
- Sager, G.; Gabaglio, S.; Sztul, E.; Belov, G.A. Role of Host Cell Secretory Machinery in Zika Virus Life Cycle. Viruses 2018, 10, 559.
- Heinz, F.X.; Stiasny, K. The Antigenic Structure of Zika Virus and Its Relation to Other Flaviviruses: Implications for Infection and Immunoprophylaxis. Microbiol. Mol. Biol. Rev. 2017, 81, e00055-16.
- Pierson, T.C.; Diamond, M.S. The emergence of Zika virus and its new clinical syndromes. Nature 2018, 560, 573–581.
- Rawlinson, W. Pregnancy, the placenta and Zika virus (ZIKV) infection. Microbiol. Aust. 2016, 37, 170–172.
- Moore, C.A.; Staples, J.E.; Dobyns, W.B.; Pessoa, A.; Ventura, C.V.; Fonseca, E.B.d.; Ribeiro, E.M.; Ventura, L.O.; Neto, N.N.; Arena, J.F.; et al. Characterizing the Pattern of Anomalies in Congenital Zika Syndrome for Pediatric Clinicians. JAMA Pediatr. 2017, 171, 288–295.
- Oeser, C.; Ladhani, S. An update on Zika Virus and Congenital Zika Syndrome. Paediatr. Child. Health 2019, 29, 34–37.
- Lima, G.P.; Rozenbaum, D.; Pimentel, C.; Frota, A.C.C.; Vivacqua, D.; Machado, E.S.; Sztajnbok, F.; Abreu, T.; Soares, R.A.; Hofer, C.B. Factors associated with the development of Congenital Zika Syndrome: A case-control study. BMC Infect. Dis. 2019, 19, 277.
- Barbi, L.; Coelho, A.V.C.; Alencar, L.C.A.; Crovella, S. Prevalence of Guillain-Barré syndrome among Zika virus infected cases: A systematic review and meta-analysis. Braz. J. Infect. Dis. Off. Publ. Braz. Soc. Infect. Dis. 2018, 22, 137–141.
- St George, K.; Sohi, I.S.; Dufort, E.M.; Dean, A.B.; White, J.L.; Limberger, R.; Sommer, J.N.; Ostrowski, S.; Wong, S.J.; Backenson, P.B.; et al. Zika Virus Testing Considerations: Lessons Learned from the First 80 Real-Time Reverse Transcription-PCR-Positive Cases Diagnosed in New York State. J. Clin. Microbiol. 2017, 55, 535–544.
- Singh, R.K.; Dhama, K.; Karthik, K.; Tiwari, R.; Khandia, R.; Munjal, A.; Iqbal, H.M.N.; Malik, Y.S.; Bueno-Marí, R. Advances in Diagnosis, Surveillance, and Monitoring of Zika Virus: An Update. Front. Microbiol. 2018, 8, 2677.
- Basile, A.J.; Ao, J.; Horiuchi, K.; Semenova, V.; Steward-Clark, E.; Schiffer, J. Performance of InBios ZIKV Detect™ 2.0 IgM Capture ELISA in two reference laboratories compared to the original ZIKV Detect™ IgM Capture ELISA. J. Virol. Methods 2019, 271, 113671.
- Munoz-Jordan, J.L. Diagnosis of Zika Virus Infections: Challenges and Opportunities. J. Infect. Dis. 2017, 216, S951–S956.
- Peters, R.; Stevenson, M. Zika virus diagnosis: Challenges and solutions. Clin. Microbiol. Infect. 2019, 25, 142–146.
- Atif, M.; Azeem, M.; Sarwar, M.R.; Bashir, A. Zika virus disease: A current review of the literature. Infection 2016, 44, 695–705.
- Van Rompay, K.K.A.; Keesler, R.I.; Ardeshir, A.; Watanabe, J.; Usachenko, J.; Singapuri, A.; Cruzen, C.; Bliss-Moreau, E.; Murphy, A.M.; Yee, J.L.; et al. DNA vaccination before conception protects Zika virus–exposed pregnant macaques against prolonged viremia and improves fetal outcomes. Sci. Transl. Med. 2019, 11, eaay2736.
- da Silva, S.; Oliveira Silva Martins, D.; Jardim, A.C.G. A Review of the Ongoing Research on Zika Virus Treatment. Viruses 2018, 10, 255.
- Singh, R.K.; Dhama, K.; Khandia, R.; Munjal, A.; Karthik, K.; Tiwari, R.; Chakraborty, S.; Malik, Y.S.; Bueno-Marí, R. Prevention and Control Strategies to Counter Zika Virus, a Special Focus on Intervention Approaches against Vector Mosquitoes-Current Updates. Front. Microbiol. 2018, 9, 87.
- Igbinosa, I.I.; Rabe, I.B.; Oduyebo, T.; Rasmussen, S.A. Zika Virus: Common Questions and Answers. Am. Fam. Physician 2017, 95, 507–513.
- Meghani, Z.; Boëte, C. Genetically engineered mosquitoes, Zika and other arboviruses, community engagement, costs, and patents: Ethical issues. PLoS Negl. Trop. Dis. 2018, 12, e0006501.
- Poland, G.A.; Ovsyannikova, I.G.; Kennedy, R.B. Zika Vaccine Development: Current Status. Mayo Clin. Proc. 2019, 94, 2572–2586.
- das Neves Almeida, R.; Racine, T.; Magalhães, K.G.; Kobinger, G.P. Zika Virus Vaccines: Challenges and Perspectives. Vaccines 2018, 6, 62.
- Pattnaik, A.; Sahoo, B.R.; Pattnaik, A.K. Current Status of Zika Virus Vaccines: Successes and Challenges. Vaccines 2020, 8, 266.
- Devillers, J. Repurposing drugs for use against Zika virus infection. SAR QSAR Environ. Res. 2018, 29, 103–115.
- Gardinali, N.R.; Marchevsky, R.S.; Oliveira, J.M.; Pelajo-Machado, M.; Kugelmeier, T.; Castro, M.P.; Silva, A.C.A.; Pinto, D.P.; Fonseca, L.B.; Vilhena, L.S.; et al. Sofosbuvir shows a protective effect against vertical transmission of Zika virus and the associated congenital syndrome in rhesus monkeys. Antivir. Res. 2020, 182, 104859.
- Mesci, P.; Macia, A.; Moore, S.M.; Shiryaev, S.A.; Pinto, A.; Huang, C.-T.; Tejwani, L.; Fernandes, I.R.; Suarez, N.A.; Kolar, M.J.; et al. Blocking Zika virus vertical transmission. Sci. Rep. 2018, 8, 1218.
- Rehman, A.; Ashfaq, U.A.; Javed, M.R.; Shahid, F.; Noor, F.; Aslam, S. The Screening of Phytochemicals Against NS5 Polymerase to Treat Zika Virus Infection: Integrated Computational Based Approach. Comb. Chem. High Throughput Screen 2022, 25, 738–751.
- Mohd, A.; Zainal, N.; Tan, K.K.; AbuBakar, S. Resveratrol affects Zika virus replication in vitro. Sci Rep 2019, 9, 14336, doi:10.1038/s41598-019-50674-3.
- Oliveira, M.B.S.; Valentim, I.B.; Rocha, T.S.; Santos, J.C.; Pires, K.S.N.; Tanabe, E.L.L.; Borbely, K.S.C.; Borbely, A.U.; Goulart, M.O.F. Schinus terebenthifolius Raddi extracts: From sunscreen activity toward protection of the placenta to Zika virus infection, new uses for a well-known medicinal plant. Ind Crops Prod 2020, 152, 112503, doi:10.1016/j.indcrop.2020.112503.
- 78. Gaudry, A.; Bos, S.; Viranaicken, W.; Roche, M.; Krejbich-Trotot, P.; Gadea, G.; Desprès, P.; El-Kalamouni, C. The Flavonoid Isoquercitrin Precludes Initiation of Zika Virus Infection in Human Cells. Int J Mol Sci 2018, 19, 1093, doi:10.3390/ijms19041093.
- 79. Mounce, B.C.; Cesaro, T.; Carrau, L.; Vallet, T.; Vignuzzi, M. Curcumin inhibits Zika and chikungunya virus infection by inhibiting cell binding. Antiviral research 2017, 142, 148-157, doi:10.1016/j.antiviral.2017.03.014.
- 80. Gao, Y.; Tai, W.; Wang, N.; Li, X.; Jiang, S.; Debnath, A.K.; Du, L.; Chen, S. Identification of Novel Natural Products as Effective and Broad-Spectrum Anti-Zika Virus Inhibitors. Viruses 2019, 11, 1019, doi:10.3390/v11111019.
- 81. Cirne-Santos, C.C.; Barros, C.d.S.; Gomes, M.W.L.; Gomes, R.; Cavalcanti, D.N.; Obando, J.M.C.; Ramos, C.J.B.; Villaça, R.C.; Teixeira, V.L.; Paixão, I.C.N.d.P. In Vitro Antiviral Activity Against Zika Virus From a Natural Product of the Brazilian Brown Seaweed Dictyota menstrualis. Natural Product Communications 2019, 14, 1934578X19859128, doi:10.1177/1934578X19859128.
- Vazquez-Calvo, A.; Jimenez de Oya, N.; Martin-Acebes, M.A.; Garcia-Moruno, E.; Saiz, J.C. Antiviral Properties of the Natural Polyphenols Delphinidin and Epigallocatechin Gallate against the Flaviviruses West Nile Virus, Zika Virus, and Dengue Virus. Front Microbiol 2017, 8, 1314, doi:10.3389/fmicb.2017.01314.
- Fong, Y.D.; Chu, J.J.H. Natural products as Zika antivirals. Med Res Rev 2022, 42, 1739-1780, doi:10.1002/med.21891.
- 84. Batista, M.N.; Braga, A.C.S.; Campos, G.R.F.; Souza, M.M.; Matos, R.P.A.d.; Lopes, T.Z.; Candido, N.M.; Lima, M.L.D.; Machado, F.C.; Andrade, S.T.Q.d., et al. Natural Products Isolated from Oriental Medicinal Herbs Inactivate Zika Virus. Viruses 2019, 11, 49, doi:10.3390/v11010049.
- 85. Lai, Z.Z.; Ho, Y.J.; Lu, J.W. Harringtonine Inhibits Zika Virus Infection through Multiple Mechanisms. Molecules 2020, 25, doi:10.3390/molecules25184082.
- 86. Ho, Y.J.; Lu, J.W.; Huang, Y.L.; Lai, Z.Z. Palmatine inhibits Zika virus infection by disrupting virus binding, entry, and stability. Biochem Biophys Res Commun 2019, 518, 732-738, doi:10.1016/j.bbrc.2019.08.120.
- 87. Chen, Y.; Li, Z.; Pan, P.; Lao, Z.; Xu, J.; Li, Z.; Zhan, S.; Liu, X.; Wu, Y.; Wang, W., et al. Cinnamic acid inhibits Zika virus by inhibiting RdRp activity. Antiviral research 2021, 192, 105117, doi:10.1016/j.antiviral.2021.105117.
- 88. Cataneo, A.H.D.; Kuczera, D.; Koishi, A.C.; Zanluca, C.; Silveira, G.F.; Arruda, T.B.d.; Suzukawa, A.A.; Bortot, L.O.; Dias-Baruffi, M.; Verri, W.A., et al. The citrus flavonoid naringenin impairs the in vitro infection of human cells by Zika virus. Scientific Reports 2019, 9, 16348, doi:10.1038/s41598-019-52626-3.
- 89. Martinez-Lopez, A.; Persaud, M.; Chavez, M.P.; Zhang, H.; Rong, L.; Liu, S.; Wang, T.T.; Sarafianos, S.G.; Diaz-Griffero, F. Glycosylated diphyllin as a broad-spectrum antiviral agent against Zika virus. EBioMedicine 2019, 47, 269-283, doi:https://doi.org/10.1016/j.ebiom.2019.08.060.
- 90. Haddad, J.G.; Koishi, A.C.; Gaudry, A.; Nunes Duarte Dos Santos, C.; Viranaicken, W.; Desprès, P.; El Kalamouni, C. Doratoxylon apetalum, an Indigenous Medicinal Plant from Mascarene Islands, Is a Potent Inhibitor of Zika and Dengue Virus Infection in Human Cells. Int J Mol Sci 2019, 20, 2382, doi:10.3390/ijms20102382.
- Braz-De-Melo, H.A.; Pasquarelli-do-Nascimento, G.; Corrêa, R.; das Neves Almeida, R.; de Oliveira Santos, I.; Prado, P.S.; Picolo, V.; de Bem, A.F.; Pizato, N.; Magalhães, K.G. Potential neuroprotective and anti-inflammatory effects provided by omega-3 (DHA) against Zika virus infection in human SH-SY5Y cells. Scientific Reports 2019, 9, 20119, doi:10.1038/s41598-019-56556-y.




