
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Bingxi Yan | -- | 2622 | 2022-12-06 18:27:03 | | | |
| 2 | Vivi Li | -50 word(s) | 2572 | 2022-12-07 07:16:41 | | |
Video Upload Options
The choice of actuators dictates how an implantable biomedical device moves. Specifically, the concept of implantable robots consists of the three pillars: actuators, sensors, and powering. Robotic devices that require active motion are driven by a biocompatible actuator. Depending on the actuating mechanism, different types of actuators vary remarkably in strain/stress output, frequency, power consumption, and durability. Most reviews to date focus on specific type of actuating mechanism (electric, photonic, electrothermal, etc.) for biomedical applications. With a rapidly expanding library of novel actuators, however, the granular boundaries between subcategories turns the selection of actuators a laborious task, which can be particularly time-consuming to those unfamiliar with actuation.
1. Introduction
2. Actuators for Various In Vivo Biomedical Applications
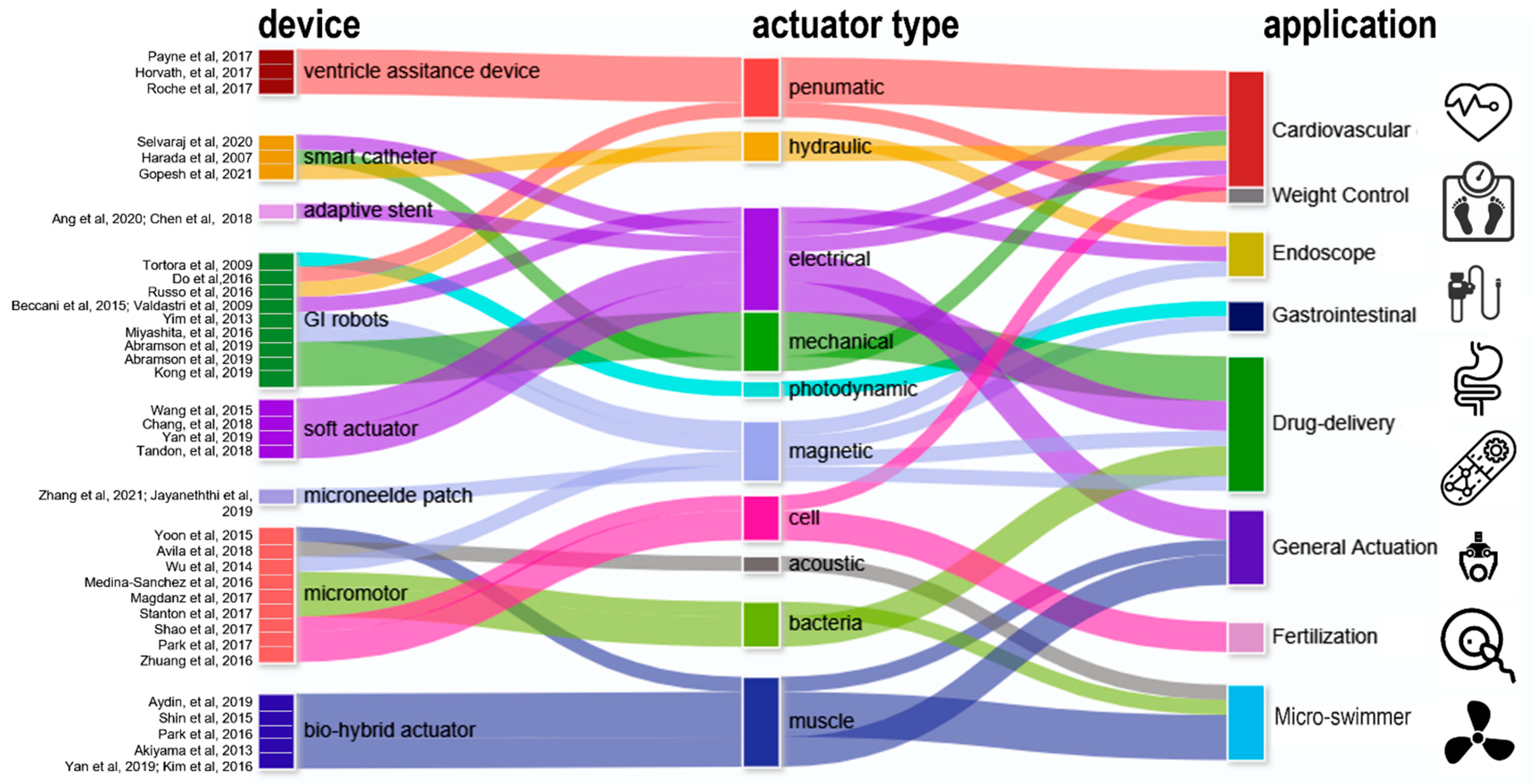
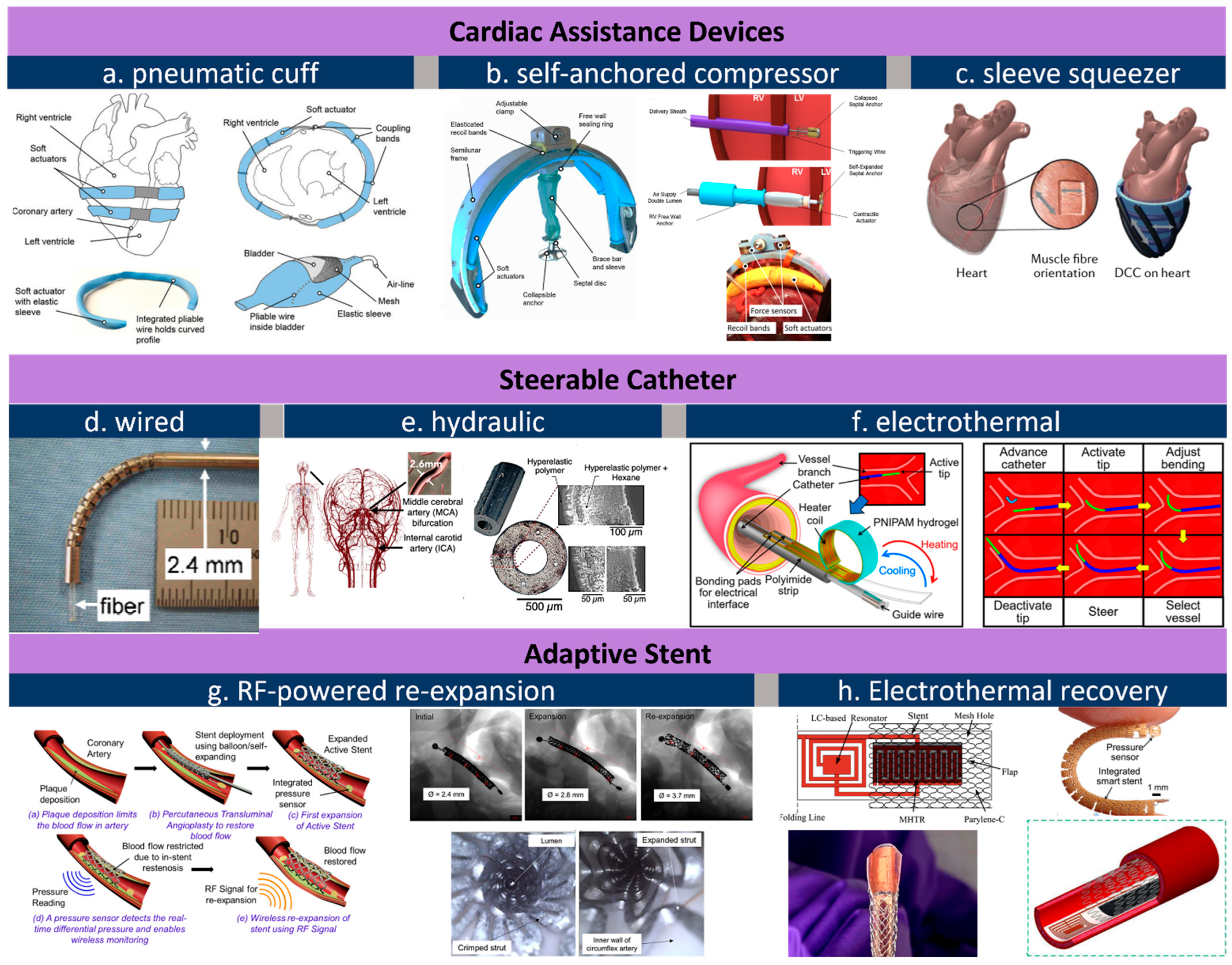
2.1. Actuators for Cardiac and Cardiovascular Devices
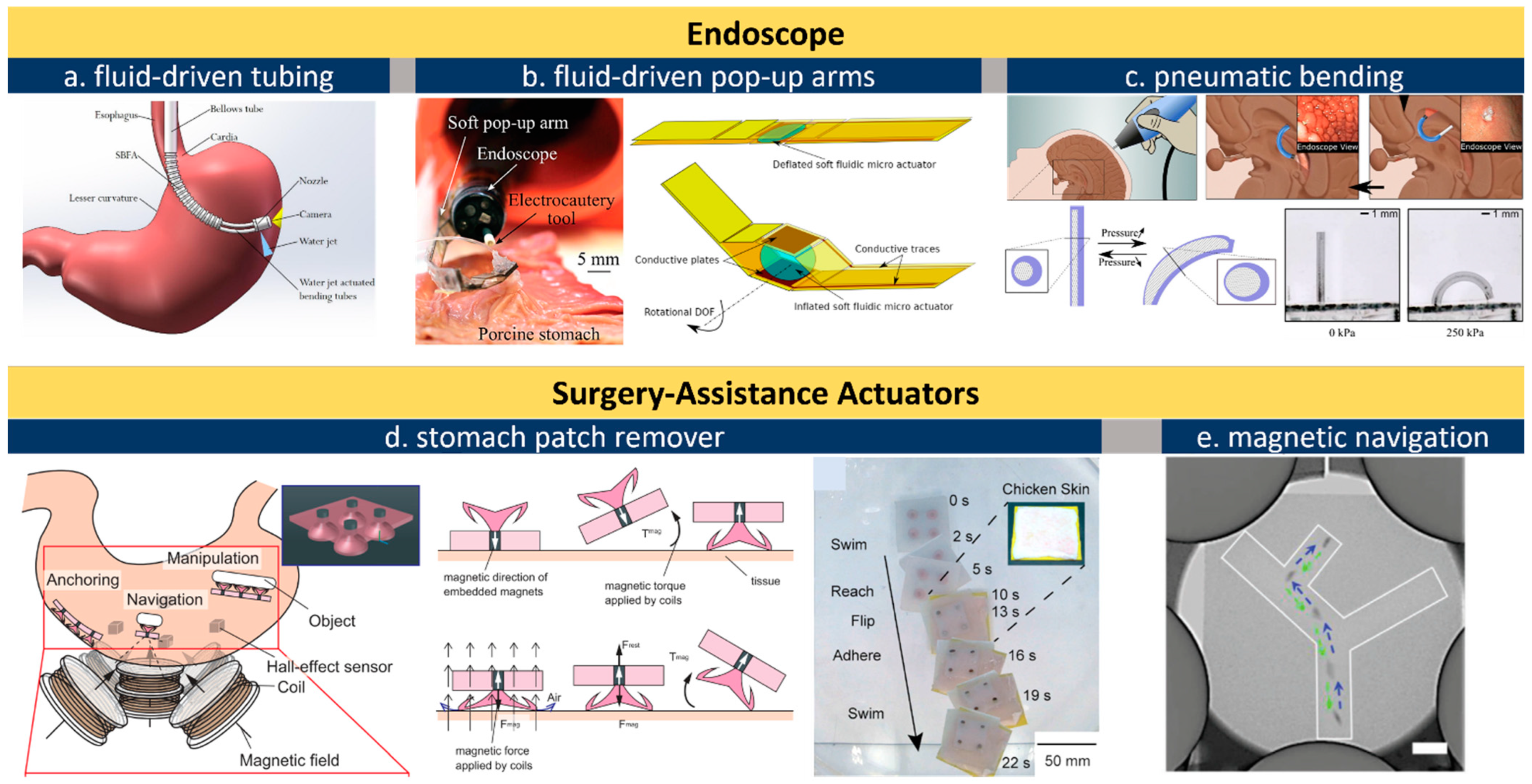
2.2. Actuators for Endoscope and Surgery Assistance
References
- Frontera, W.R.; Ochala, J. Skeletal muscle: A brief review of structure and function. Calcif. Tissue Int. 2015, 96, 183–195.
- MacIntosh, B.R.; Gardiner, P.F.; McComas, A.J. Skeletal Muscle: Form and Function; Human Kinetics: Champaign, IL, USA, 2006.
- Billard, A.; Kragic, D. Trends and challenges in robot manipulation. Science 2019, 364, eaat8414.
- Zhuang, K.Z.; Sommer, N.; Mendez, V.; Aryan, S.; Formento, E.; D’Anna, E.; Artoni, F.; Petrini, F.; Granata, G.; Cannaviello, G. Shared human–robot proportional control of a dexterous myoelectric prosthesis. Nat. Mach. Intell. 2019, 1, 400–411.
- Phan, H.V.; Aurecianus, S.; Au, T.K.L.; Kang, T.; Park, H.C. Towards the long-endurance flight of an insect-inspired, tailless, two-winged, flapping-wing flying robot. IEEE Robot. Autom. Lett. 2020, 5, 5059–5066.
- Phan, H.V.; Park, H.C. Insect-inspired, tailless, hover-capable flapping-wing robots: Recent progress, challenges, and future directions. Prog. Aerosp. Sci. 2019, 111, 100573.
- Jafferis, N.T.; Helbling, E.F.; Karpelson, M.; Wood, R.J. Untethered flight of an insect-sized flapping-wing microscale aerial vehicle. Nature 2019, 570, 491–495.
- Li, J.; Long, Y.; Yang, F.; Wang, X. Degradable piezoelectric biomaterials for wearable and implantable bioelectronics. Curr. Opin. Solid State Mater. Sci. 2020, 24, 100806.
- Curry, E.J.; Le, T.T.; Das, R.; Ke, K.; Santorella, E.M.; Paul, D.; Chorsi, M.T.; Tran, K.T.; Baroody, J.; Borges, E.R. Biodegradable nanofiber-based piezoelectric transducer. Proc. Natl. Acad. Sci. USA 2020, 117, 214–220.
- Miriyev, A.; Stack, K.; Lipson, H. Soft material for soft actuators. Nat. Commun. 2017, 8, 596.
- Yan, B. Geometrically Enabled Polypyrrole Composites. Ph.D. Thesis, The Ohio State University, Columbus, OH, USA, 2019.
- Yang, Q.; Park, H.; Nguyen, T.N.; Rhoads, J.F.; Lee, A.; Bentley, R.T.; Judy, J.W.; Lee, H. Anti-biofouling implantable catheter using thin-film magnetic microactuators. Sens. Actuators B Chem. 2018, 273, 1694–1704.
- Yunas, J.; Mulyanti, B.; Hamidah, I.; Mohd Said, M.; Pawinanto, R.E.; Wan Ali, W.A.F.; Subandi, A.; Hamzah, A.A.; Latif, R.; Yeop Majlis, B. Polymer-based MEMS electromagnetic actuator for biomedical application: A review. Polymers 2020, 12, 1184.
- De Volder, M.; Reynaerts, D. Pneumatic and hydraulic microactuators: A review. J. Micromech. Microeng. 2010, 20, 043001.
- Knick, C.R.; Sharar, D.J.; Wilson, A.A.; Smith, G.L.; Morris, C.J.; Bruck, H.A. High frequency, low power, electrically actuated shape memory alloy MEMS bimorph thermal actuators. J. Micromech. Microeng. 2019, 29, 075005.
- Sardesai, A.N.; Segel, X.M.; Baumholtz, M.N.; Chen, Y.; Sun, R.; Schork, B.W.; Buonocore, R.; Wagner, K.O.; Golecki, H.M. Design and characterization of edible soft robotic candy actuators. MRS Adv. 2018, 3, 3003–3009.
- Wang, B.; Zhang, Y.; Zhang, L. Recent progress on micro-and nano-robots: Towards in vivo tracking and localization. Quant. Imaging Med. Surg. 2018, 8, 461.
- Damian, D.D.; Price, K.; Arabagi, S.; Berra, I.; Machaidze, Z.; Manjila, S.; Shimada, S.; Fabozzo, A.; Arnal, G.; Van Story, D. In vivo tissue regeneration with robotic implants. Sci. Robot. 2018, 3, eaaq0018.
- Yan, B.X.; Wu, Y.; Guo, L. Recent Advances on Polypyrrole Electroactuators. Polymers 2017, 9, 446.
- Bhandari, B.; Lee, G.-Y.; Ahn, S.-H. A review on IPMC material as actuators and sensors: Fabrications, characteristics and applications. Int. J. Precis. Eng. Manuf. 2012, 13, 141–163.
- Polygerinos, P.; Polygerinos, P.; Correll, N.; Morin, S.A.; Mosadegh, B.; Onal, C.D.; Petersen, K.; Cianchetti, M.; Tolley, M.T.; Shepherd, R.F. Soft Robotics: Review of Fluid-Driven Intrinsically Soft Devices; Manufacturing, Sensing, Control, and Applications in Human-Robot Interaction. Adv. Eng. Mater. 2017, 19, 1700016.
- Jayathilaka, W.A.D.M.; Qi, K.; Qin, Y.; Chinnappan, A.; Serrano-García, W.; Baskar, C.; Wang, H.; He, J.; Cui, S.; Thomas, S.W.; et al. Significance of Nanomaterials in Wearables: A Review on Wearable Actuators and Sensors. Adv. Mater. 2019, 31, 1805921.
- Tawk, C.; Alici, G. A Review of 3D-Printable Soft Pneumatic Actuators and Sensors: Research Challenges and Opportunities. Adv. Intell. Syst. 2021, 3, 2000223.
- Roche, E.T.; Horvath, M.A.; Wamala, I.; Alazmani, A.; Song, S.-E.; Whyte, W.; Machaidze, Z.; Payne, C.J.; Weaver, J.C.; Fishbein, G. Soft robotic sleeve supports heart function. Sci. Transl. Med. 2017, 9, eaaf3925.
- Liu, Q.; Zuo, J.; Zhu, C.; Xie, S.Q. Design and control of soft rehabilitation robots actuated by pneumatic muscles: State of the art. Future Gener. Comput. Syst. 2020, 113, 620–634.
- Wang, Y.; Xu, Q. Design and testing of a soft parallel robot based on pneumatic artificial muscles for wrist rehabilitation. Sci. Rep. 2021, 11, 1273.
- Clayton, S.B.; Shin, C.M.; Ewing, A.; Blonski, W.; Richter, J. Pneumatic dilation improves esophageal emptying and symptoms in patients with idiopathic esophago-gastric junction outflow obstruction. Neurogastroenterol. Motil. 2019, 31, e13522.
- Dhorepatil, A.S.; Cottam, D.; Surve, A.; Medlin, W.; Zaveri, H.; Richards, C.; Cottam, A. Is pneumatic balloon dilation safe and effective primary modality of treatment for post-sleeve gastrectomy strictures? A retrospective study. BMC Surg. 2018, 18, 52.
- Yu, J.; Zhang, Y.; Ye, Y.; DiSanto, R.; Sun, W.; Ranson, D.; Ligler, F.S.; Buse, J.B.; Gu, Z. Microneedle-array patches loaded with hypoxia-sensitive vesicles provide fast glucose-responsive insulin delivery. Proc. Natl. Acad. Sci. USA 2015, 112, 8260–8265.
- Magdanz, V.; Sanchez, S.; Schmidt, O.G. Development of a sperm-flagella driven micro-bio-robot. Adv. Mater. 2013, 25, 6581–6588.
- Xu, H.; Medina-Sánchez, M.; Magdanz, V.; Schwarz, L.; Hebenstreit, F.; Schmidt, O.G. Sperm-Hybrid Micromotor for Targeted Drug Delivery. ACS Nano 2018, 12, 327–337.
- Do, T.N.; Ho, K.Y.; Phee, S.J. A magnetic soft endoscopic capsule-inflated intragastric balloon for weight management. Sci. Rep. 2016, 6, 39486.
- Yim, S.; Sitti, M. 3-D localization method for a magnetically actuated soft capsule endoscope and its applications. IEEE Trans. Robot. 2013, 29, 1139–1151.
- Stanton, M.M.; Park, B.-W.; Vilela, D.; Bente, K.; Faivre, D.; Sitti, M.; Sánchez, S. Magnetotactic bacteria powered biohybrids target E. coli biofilms. ACS Nano 2017, 11, 9968–9978.
- Zhang, X.; Chen, G.; Fu, X.; Wang, Y.; Zhao, Y. Magneto-Responsive Microneedle Robots for Intestinal Macromolecule Delivery. Adv. Mater. 2021, 33, 2104932.
- Payne, C.J.; Wamala, I.; Abah, C.; Thalhofer, T.; Saeed, M.; Bautista-Salinas, D.; Horvath, M.A.; Vasilyev, N.V.; Roche, E.T.; Pigula, F.A. An implantable extracardiac soft robotic device for the failing heart: Mechanical coupling and synchronization. Soft Robot. 2017, 4, 241–250.
- Horvath, M.A.; Wamala, I.; Rytkin, E.; Doyle, E.; Payne, C.J.; Thalhofer, T.; Berra, I.; Solovyeva, A.; Saeed, M.; Hendren, S. An intracardiac soft robotic device for augmentation of blood ejection from the failing right ventricle. Ann. Biomed. Eng. 2017, 45, 2222–2233.
- Selvaraj, M.; Takahata, K. Electrothermally driven hydrogel-on-flex-circuit actuator for smart steerable catheters. Micromachines 2020, 11, 68.
- Harada, K.; Bo, Z.; Enosawa, S.; Chiba, T.; Fujie, M.G. Bending laser manipulator for intrauterine surgery and viscoelastic model of fetal rat tissue. In Proceedings of the IEEE International Conference on Robotics and Automation, Rome, Italy, 10–14 April 2007; pp. 611–616.
- Gopesh, T.; Wen, J.H.; Santiago-Dieppa, D.; Yan, B.; Pannell, J.S.; Khalessi, A.; Norbash, A.; Friend, J. Soft robotic steerable microcatheter for the endovascular treatment of cerebral disorders. Sci. Robot. 2021, 6, eabf0601.
- Ang, Y.X.; Ghazali, F.A.M.; Ali, M.S.M. Micromachined shape memory alloy active stent with wireless monitoring and re-expansion features. In Proceedings of the IEEE 33rd International Conference on Micro Electro Mechanical Systems (MEMS), Vancouver, BC, Canada, 18–22 January 2020; pp. 396–399.
- Tortora, G.; Valdastri, P.; Susilo, E.; Menciassi, A.; Dario, P.; Rieber, F.; Schurr, M.O. Propeller-based wireless device for active capsular endoscopy in the gastric district. Minim. Invasive Ther. Allied Technol. 2009, 18, 280–290.
- Russo, S.; Ranzani, T.; Walsh, C.; Wood, R. A soft pop-up proprioceptive actuator for minimally invasive surgery. In Proceedings of the 9th Hamlyn Symposium on Medical Robotics, London, UK, 26–27 June 2016; pp. 25–28.
- Beccani, M.; Tunc, H.; Taddese, A.; Susilo, E.; Völgyesi, P.; Lédeczi, A.; Valdastri, P. Systematic design of medical capsule robots. IEEE Des. Test 2015, 32, 98–108.
- Valdastri, P.; Simi, M.; Webster, R.J., III. Advanced technologies for gastrointestinal endoscopy. Annu. Rev. Biomed. Eng. 2012, 14, 397–429.
- Miyashita, S.; Guitron, S.; Yoshida, K.; Li, S.; Damian, D.D.; Rus, D. Ingestible, controllable, and degradable origami robot for patching stomach wounds. In Proceedings of the 2016 IEEE International Conference on Robotics and Automation (ICRA), Stockholm, Sweden, 16–21 May 2016; pp. 909–916.
- Abramson, A.; Caffarel-Salvador, E.; Khang, M.; Dellal, D.; Silverstein, D.; Gao, Y.; Frederiksen, M.R.; Vegge, A.; Hubálek, F.; Water, J.J. An ingestible self-orienting system for oral delivery of macromolecules. Science 2019, 363, 611–615.
- Abramson, A.; Caffarel-Salvador, E.; Soares, V.; Minahan, D.; Tian, R.Y.; Lu, X.; Dellal, D.; Gao, Y.; Kim, S.; Wainer, J.; et al. A luminal unfolding microneedle injector for oral delivery of macromolecules. Nat. Med. 2019, 25, 1512–1518.
- Kong, Y.L.; Zou, X.; McCandler, C.A.; Kirtane, A.R.; Ning, S.; Zhou, J.; Abid, A.; Jafari, M.; Rogner, J.; Minahan, D. 3D-printed gastric resident electronics. Adv. Mater. Technol. 2019, 4, 1800490.
- Wang, Y.; Chen, H.; Liu, J.; Zhu, Z.; Chang, L.; Li, D.; Jia, S. Aided manufacturing techniques and applications in optics and manipulation for ionic polymer-metal composites as soft sensors and actuators. J. Polym. Eng. 2015, 35, 611–626.
- Yan, B.; An, D.; Wang, X.; DeLong, B.J.; Kiourti, A.; Dungan, K.; Volakis, J.L.; Ma, M.; Guo, L. Battery-free implantable insulin micropump operating at transcutaneously radio frequency-transmittable power. Med. Devices Sens. 2019, 2, e10055.
- Tandon, B.; Magaz, A.; Balint, R.; Blaker, J.J.; Cartmell, S.H. Electroactive biomaterials: Vehicles for controlled delivery of therapeutic agents for drug delivery and tissue regeneration. Adv. Drug Deliv. Rev. 2018, 129, 148–168.
- Jayaneththi, V.R.; Aw, K.; Sharma, M.; Wen, J.; Svirskis, D.; McDaid, A. Controlled transdermal drug delivery using a wireless magnetic microneedle patch: Preclinical device development. Sens. Actuators B Chem. 2019, 297, 126708.
- Yoon, J.; Eyster, T.W.; Misra, A.C.; Lahann, J. Cardiomyocyte-driven actuation in biohybrid microcylinders. Adv. Mater. 2015, 27, 4509–4515.
- Wu, Z.; Li, T.; Li, J.; Gao, W.; Xu, T.; Christianson, C.; Gao, W.; Galarnyk, M.; He, Q.; Zhang, L.; et al. Turning erythrocytes into functional micromotors. ACS Nano 2014, 8, 12041–12048.
- Chang, X.L.; Chee, P.S.; Lim, E.H.; Chong, W.C. Radio-frequency enabled ionic polymer metal composite (IPMC) actuator for drug release application. Smart Mater. Struct. 2018, 28, 015024.
- Esteban-Fernández de Ávila, B.; Angsantikul, P.; Li, J.; Gao, W.; Zhang, L.; Wang, J. Micromotors go in vivo: From test tubes to live animals. Adv. Funct. Mater. 2018, 28, 1705640.
- Medina-Sánchez, M.; Schwarz, L.; Meyer, A.K.; Hebenstreit, F.; Schmidt, O.G. Cellular cargo delivery: Toward assisted fertilization by sperm-carrying micromotors. Nano Lett. 2016, 16, 555–561.
- Magdanz, V.; Medina-Sánchez, M.; Schwarz, L.; Xu, H.; Elgeti, J.; Schmidt, O.G. Spermatozoa as functional components of robotic microswimmers. Adv. Mater. 2017, 29, 1606301.
- Shao, J.; Xuan, M.; Zhang, H.; Lin, X.; Wu, Z.; He, Q. Chemotaxis-guided hybrid neutrophil micromotors for targeted drug transport. Angew. Chem. 2017, 129, 13115–13119.
- Park, B.-W.; Zhuang, J.; Yasa, O.; Sitti, M. Multifunctional bacteria-driven microswimmers for targeted active drug delivery. ACS Nano 2017, 11, 8910–8923.
- Zhuang, J.; Sitti, M. Chemotaxis of bio-hybrid multiple bacteria-driven microswimmers. Sci. Rep. 2016, 6, 32135.
- Aydin, O.; Zhang, X.; Nuethong, S.; Pagan-Diaz, G.J.; Bashir, R.; Gazzola, M.; Saif, M.T.A. Neuromuscular actuation of biohybrid motile bots. Proc. Natl. Acad. Sci. USA 2019, 116, 19841–19847.
- Shin, S.R.; Shin, C.; Memic, A.; Shadmehr, S.; Miscuglio, M.; Jung, H.Y.; Jung, S.M.; Bae, H.; Khademhosseini, A.; Tang, X.; et al. Aligned carbon nanotube–based flexible gel substrates for engineering biohybrid tissue actuators. Adv. Funct. Mater. 2015, 25, 4486–4495.
- Park, S.-J.; Gazzola, M.; Park, K.S.; Park, S.; Di Santo, V.; Blevins, E.L.; Lind, J.U.; Campbell, P.H.; Dauth, S.; Capulli, A.K.; et al. Phototactic guidance of a tissue-engineered soft-robotic ray. Science 2016, 35, 158–162.
- Akiyama, Y.; Sakuma, T.; Funakoshi, K.; Hoshino, T.; Iwabuchi, K.; Morishima, K. Atmospheric-operable bioactuator powered by insect muscle packaged with medium. Lab Chip 2013, 13, 4870–4880.
- Kim, T.H.; Kwon, C.H.; Lee, C.; An, J.; Phuong, T.T.T.; Park, S.H.; Lima, M.D.; Baughman, R.H.; Kang, T.M.; Kim, S.J. Bio-inspired Hybrid Carbon Nanotube Muscles. Sci. Rep. 2016, 6, 26687.
- Yan, B.; Wang, Y.; Wu, Y.; Prox, J.D.; Yang, H.; Guo, L. Fast Electrochemical Netting of Composite Chains for Transferable Highly Conductive Polymeric Nanofilms. J. Phys. Chem. B 2019, 123, 8580–8589.
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.-P.; Fullerton, H.J. Heart disease and stroke statistics—2016 update: A report from the American Heart Association. Circulation 2016, 133, e38–e360.
- Berry, C.; Murdoch, D.R.; McMurray, J.J. Economics of chronic heart failure. Eur. J. Heart Fail. 2001, 3, 283–291.
- Blackstone, E.H.; Rajeswaran, J.; Cruz, V.B.; Hsich, E.M.; Koprivanac, M.; Smedira, N.G.; Hoercher, K.J.; Thuita, L.; Starling, R.C. Continuously updated estimation of heart transplant waitlist mortality. J. Am. Coll. Cardiol. 2018, 72, 650–659.
- Chou, C.-P.; Hannaford, B. Static and dynamic characteristics of McKibben pneumatic artificial muscles. In Proceedings of the IEEE International Conference on Robotics and Automation, San Diego, CA, USA, 8–13 May 1994; pp. 281–286.
- Rodriguez, L.E.; Suarez, E.E.; Loebe, M.; Bruckner, B.A. Ventricular assist devices (VAD) therapy: New technology, new hope? Methodist DeBakey Cardiovasc. J. 2013, 9, 32.
- Slepian, M.J.; Smith, R.G.; Copeland, J.G. The SynCardia CardioWestTM total artificial heart. In Treatment of Advanced Heart Disease; CRC Press: Boca Raton, FL, USA, 2006; pp. 503–520.
- Buckberg, G.; Hoffman, J.I.; Mahajan, A.; Saleh, S.; Coghlan, C. Cardiac mechanics revisited: The relationship of cardiac architecture to ventricular function. Circulation 2008, 118, 2571–2587.
- Sengupta, P.P.; Khandheria, B.K.; Narula, J. Twist and untwist mechanics of the left ventricle. Heart Fail. Clin. 2008, 4, 315–324.
- Kyo, S.; Takamoto, S. Ventricular assist device, Kyobu geka. Jpn. J. Thorac. Surg. 2009, 62 (Suppl. 8), 704–711.
- Thunberg, C.A.; Gaitan, B.D.; Arabia, F.A.; Cole, D.J.; Grigore, A.M. Ventricular assist devices today and tomorrow. J. Cardiothorac. Vasc. Anesth. 2010, 24, 656–680.
- Ang, Y.X.; Khudzari, A.Z.M.; Ali, M.S.M. Non-Invasive Treatment for Coronary In-Stent Restenosis via Wireless Revascularization with Nitinol Active Stent. IEEE Trans. Biomed. Eng. 2021, 68, 3681–3689.
- Huang, S.-W.; Yeh, C.-C.; Yang, Y.-J. A miniaturized wireless micro-heating strip integrated with an acrylate-composite temperature regulator for restenosis prevention. Sens. Actuators A Phys. 2020, 315, 112260.
- Bloss, P.; Rothe, W.; Wünsche, P.; Werner, C.; Rothe, A.; Kneissl, G.D.; Burger, W.; Rehberg, E. Investigations of the pushability behavior of cardiovascular angiographic catheters. Bio-Med. Mater. Eng. 2003, 13, 327–343.
- Lu, H.; Bekker, R.; Grundeken, M.; Woudstra, P.; Wykrzykowska, J.; Tijssen, J.; de Winter, R.; Koch, K. Five-year clinical follow-up of the STENTYS self-apposing stent in complex coronary anatomy: A single-centre experience with report of specific angiographic indications. Neth. Heart J. 2018, 26, 263–271.
- Rizas, K.D.; Mehilli, J. Stent polymers: Do they make a difference? Circ. Cardiovasc. Interv. 2016, 9, e002943.
- Chen, X.; Assadsangabi, B.; Hsiang, Y.; Takahata, K. Enabling angioplasty-ready “Smart” Stents to detect in-stent restenosis and occlusion. Adv. Sci. 2018, 5, 1700560.
- Gafford, J.; Ranzani, T.; Russo, S.; Degirmenci, A.; Kesner, S.; Howe, R.; Wood, R.; Walsh, C. Toward medical devices with integrated mechanisms, sensors, and actuators via printed-circuit MEMS. J. Med. Devices 2017, 11, 011007.
- Russo, S.; Ranzani, T.; Walsh, C.J.; Wood, R.J. An additive millimeter-scale fabrication method for soft biocompatible actuators and sensors. Adv. Mater. Technol. 2017, 2, 1700135.
- Gorissen, B.; de Volder, M.; Reynaerts, D. Chip-on-tip endoscope incorporating a soft robotic pneumatic bending microactuator. Biomed. Microdevices 2018, 20, 73.
- Liu, J.; Yin, L.; Chandler, J.H.; Chen, X.; Valdastri, P.; Zuo, S. A dual-bending endoscope with shape-lockable hydraulic actuation and water-jet propulsion for gastrointestinal tract screening. Int. J. Med. Robot. Comput. Assist. Surg. 2021, 17, 1–13.
- Iwasaki, H.; Lefevre, F.; Damian, D.D.; Iwase, E.; Miyashita, S. Autonomous and reversible adhesion using elastomeric suction cups for in-vivo medical treatments. IEEE Robot. Autom. Lett. 2020, 5, 2015–2022.
- Nguyen, K.T.; Go, G.; Jin, Z.; Darmawan, B.A.; Yoo, A.; Kim, S.; Nan, M.; Lee, S.B.; Kang, B.; Kim, C.S. A Magnetically Guided Self-Rolled Microrobot for Targeted Drug Delivery, Real-Time X-Ray Imaging, and Microrobot Retrieval. Adv. Healthc Mater. 2021, 10, 2001681.
- Iddan, G.; Meron, G.; Glukhovsky, A.; Swain, P. Wireless capsule endoscopy. Nature 2000, 405, 417.
- Koulaouzidis, A.; Iakovidis, D.K.; Karargyris, A.; Rondonotti, E. Wireless endoscopy in 2020: Will it still be a capsule? World J. Gastroenterol. WJG 2015, 21, 5119.
- Mussetto, A.; Fuccio, L.; Dari, S.; Gasperoni, S.; Cantoni, F.; Brancaccio, M.L.; Triossi, O.; Casetti, T. MiroCam™ capsule for obscure gastrointestinal bleeding: A prospective, single centre experience. Dig. Liver Dis. 2013, 45, 124–128.
- Bang, S.; Park, J.Y.; Jeong, S.; Kim, Y.H.; Shim, H.B.; Kim, T.S.; Lee, D.H.; Song, S.Y. First clinical trial of the “MiRo” capsule endoscope by using a novel transmission technology: Electric-field propagation. Gastrointest. Endosc. 2009, 69, 253–259.
- Valdastri, P.; Webster, R.J.; Quaglia, C.; Quirini, M.; Menciassi, A.; Dario, P. A new mechanism for mesoscale legged locomotion in compliant tubular environments. IEEE Trans. Robot. 2009, 25, 1047–1057.
- Simi, M.; Valdastri, P.; Quaglia, C.; Menciassi, A.; Dario, P. Design, Fabrication, and Testing of a Capsule with Hybrid Locomotion for Gastrointestinal Tract Exploration. IEEE/ASME Trans. Mechatron. 2010, 15, 170–180.
- Kalantar-Zadeh, K.; Berean, K.J.; Ha, N.; Chrimes, A.F.; Xu, K.; Grando, D.; Ou, J.Z.; Pillai, N.; Campbell, J.L.; Brkljača, R.; et al. A human pilot trial of ingestible electronic capsules capable of sensing different gases in the gut. Nat. Electron. 2018, 1, 79–87.
- Fernandes, R.; Gracias, D.H. Toward a miniaturized mechanical surgeon. Mater. Today 2009, 12, 14–20.
- Ahnfelt, E.; Degerstedt, O.; Lilienberg, E.; Sjögren, E.; Hansson, P.; Lennernäs, H. Lipiodol-based emulsions used for transarterial chemoembolization and drug delivery: Effects of composition on stability and product quality. J. Drug Deliv. Sci. Technol. 2019, 53, 101143.
- Koseki, S.; Kawamura, K.; Inoue, F.; Ikuta, K.; Ikeuchi, M. Magnetically Controlled Microrobot for Embryo Transfer in Assisted Reproductive Technology. In Proceedings of the 20th International Conference on Solid-State Sensors, Actuators and Microsystems & Eurosensors XXXIII (TRANSDUCERS & EUROSENSORS XXXIII), Berlin, Germany, 23–27 June 2019; pp. 2217–2220.
- Li, J.; de Ávila, B.E.-F.; Gao, W.; Zhang, L.; Wang, J. Micro/nanorobots for biomedicine: Delivery, surgery, sensing, and detoxification. Sci. Robot. 2017, 2, 88–95.
- Kosa, G.; Hunziker, P. Small-Scale Robots in Fluidic Media. Adv. Intell. Syst. 2019, 1, 1900035.
- Chung, H.J.; Parsons, A.M.; Zheng, L. Magnetically controlled soft robotics utilizing elastomers and gels in actuation: A review. Adv. Intell. Syst. 2021, 3, 2000186.
- Wang, H.; Zhu, Z.; Jin, H.; Wei, R.; Bi, L.; Zhang, W. Magnetic soft robots: Design, actuation, and function. J. Alloys Compd. 2022, 922, 166219.
- Kim, Y.; Zhao, X.H. Magnetic Soft Materials and Robots. Chem. Rev. 2022, 122, 5317–5364.




