Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Mustafa Attrah | -- | 2714 | 2022-12-03 23:43:42 | | | |
| 2 | Camila Xu | -24 word(s) | 2690 | 2022-12-05 02:14:13 | | | | |
| 3 | Camila Xu | Meta information modification | 2690 | 2022-12-05 02:18:05 | | | | |
| 4 | Mustafa Attrah | Meta information modification | 2690 | 2022-12-05 11:42:17 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Attrah, M.; Elmanadely, A.; Akter, D.; Rene, E.R. Medical Waste Classification and Management Processes. Encyclopedia. Available online: https://encyclopedia.pub/entry/37908 (accessed on 28 February 2026).
Attrah M, Elmanadely A, Akter D, Rene ER. Medical Waste Classification and Management Processes. Encyclopedia. Available at: https://encyclopedia.pub/entry/37908. Accessed February 28, 2026.
Attrah, Mustafa, Amira Elmanadely, Dilruba Akter, Eldon R. Rene. "Medical Waste Classification and Management Processes" Encyclopedia, https://encyclopedia.pub/entry/37908 (accessed February 28, 2026).
Attrah, M., Elmanadely, A., Akter, D., & Rene, E.R. (2022, December 04). Medical Waste Classification and Management Processes. In Encyclopedia. https://encyclopedia.pub/entry/37908
Attrah, Mustafa, et al. "Medical Waste Classification and Management Processes." Encyclopedia. Web. 04 December, 2022.
Copy Citation
The term “medical waste”, mainly refers to the waste and by-products generated from hospitals and healthcare facilities, which are being produced in huge amounts. To be addressed properly, they need to be segregated and treated according to their properties, level of contamination, and danger to living organisms and the environment.
medical waste
human health
legislations
classification of medical waste
1. Introduction
The term “medical waste” is used in many countries, such as the US, South Korea, and China, while the European Union and World Health Organisation (WHO) refer to it as “healthcare waste” [1]. The World Health Organization (WHO) defines healthcare waste (medical waste) as any waste or by-products from hospitals and healthcare facilities for humans and animals used for diagnosis, treatment, or immunisation, e.g., used syringes, needles, metal sharps, dressings, blood samples, body parts, pharmaceutical, chemical, radioactive materials, and devices [2]. Generally, countries with high revenue generate up to 0.5 kg/hospital bed of hazardous medical waste [3]. Therefore, the healthcare sector’s waste extensively impacts the environment and public health, proving very costly. In addition, the manufacturing and discarding of medical and healthcare sector waste lead to increased levels of GHG emissions and pollution [4]. The types of plastics that are mainly used to make operating room tools and equipment are polyvinylchloride (PVC), polyethylene (PE), polypropylene (PP), polyurethane (PU), and copolymers. The first three types of plastics can and are being recycled. In general, most of the operating room’s waste can be considered non-hazardous because it is generated even before the patient arrives and is not contaminated or infected [5].
Face masks make up a considerable part of medical waste (MW), especially after the massive increase in use due to COVID-19 and mandatory face mask-wearing regulations. According to the findings of a recent study that included seven hospitals and medical centres in the state of Massachusetts, USA, along with three veterinary hospitals [6], plastic waste accounted for ~30% of the total waste produced by hospitals. Non-woven polyurethane, polypropylene, or polyacrylonitrile fabrics are used to produce face masks. However, these aforementioned materials are not readily degradable but decompose into smaller pieces and particles into microplastics. Additionally, the use of hand gloves made of latex or plastic for protection by ordinary people and workers in various sectors after the pandemic led to an increase in the amount of disposed of gloves. In addition, gloves also contribute to the pollution of the environment when disposed of improperly because they are made of unrecyclable and undegradable materials [7][8]. A study highlighted that 15% of the total global carbon budget is attributed to greenhouse gas (GHG) emissions resulting from the life cycle of plastics [9]. Therefore, poor management and disposal of plastics threaten the ability of the global community to meet carbon emissions targets and combat climate change [10].
Sharma et al. [11] reviewed the detrimental impacts of the incineration of MW caused by the ashes and gaseous emissions. A vast variety of pollutants are released from a MW incinerator, including fly ashes as particulate matter (PM), carbon monoxide (CO), heavy metals, e.g., arsenic, chromium, nickel, cadmium, copper, lead, etc., acid gases such as sulphur dioxides, nitrogen oxides, and hydrogen chloride, and organic compounds such as carbon tetrachloride (CCl4), benzene, toluene, xylenes, and polycyclic aromatic hydrocarbons. In addition, leachable organic compounds form bottom residues and ashes containing heavy metals and dioxins. In addition, there is the carbon footprint of transportation, autoclave decontamination, thermal treatment (i.e., low and high-temperature incineration at ≥850 °C and 1000 °C, respectively), plus the carbon emissions produced during recycling [12]. A study in the UK has found considerable variation between different methods of MW treatment. It was estimated that the carbon footprint of MW treatment by high-temperature incineration was 1074 kg CO2e/t, making the choice of waste treatment method have an impact on the carbon footprint of up to 50-fold [12].
2. Classification of Medical Waste
According to estimates by the WHO, 15 to 20% of medical wastes can be classified as hazardous materials due to their infectivity, toxicity, and, sometimes, radioactivity [13][14]. However, medical waste management practices are not constant or standardised in all countries because this categorisation is unclear or decisive [15].
Medical waste refers directly or indirectly to infectious, toxic, or otherwise hazardous waste (HMW), illustrated in Figure 1 and described with examples in Table 1. Medical institutions generate this type of waste during medical or preventative care and related activities, specifically infectious, pathological, damaging, pharmaceutical, and chemical waste [1]. On the other hand, non-hazardous medical waste (NHMW) includes all different regular non-infectious fractions of waste, such as municipal solid waste. HMW is usually contaminated with pathogens. Therefore, it can cause a wide range of infections and diseases in the case of misuse or poor handling and discarding. Adding to that, it can cause environmental contamination in the case of poor management, causing pollution to land, water, plants, animals, and air, leading to the spread of diseases.
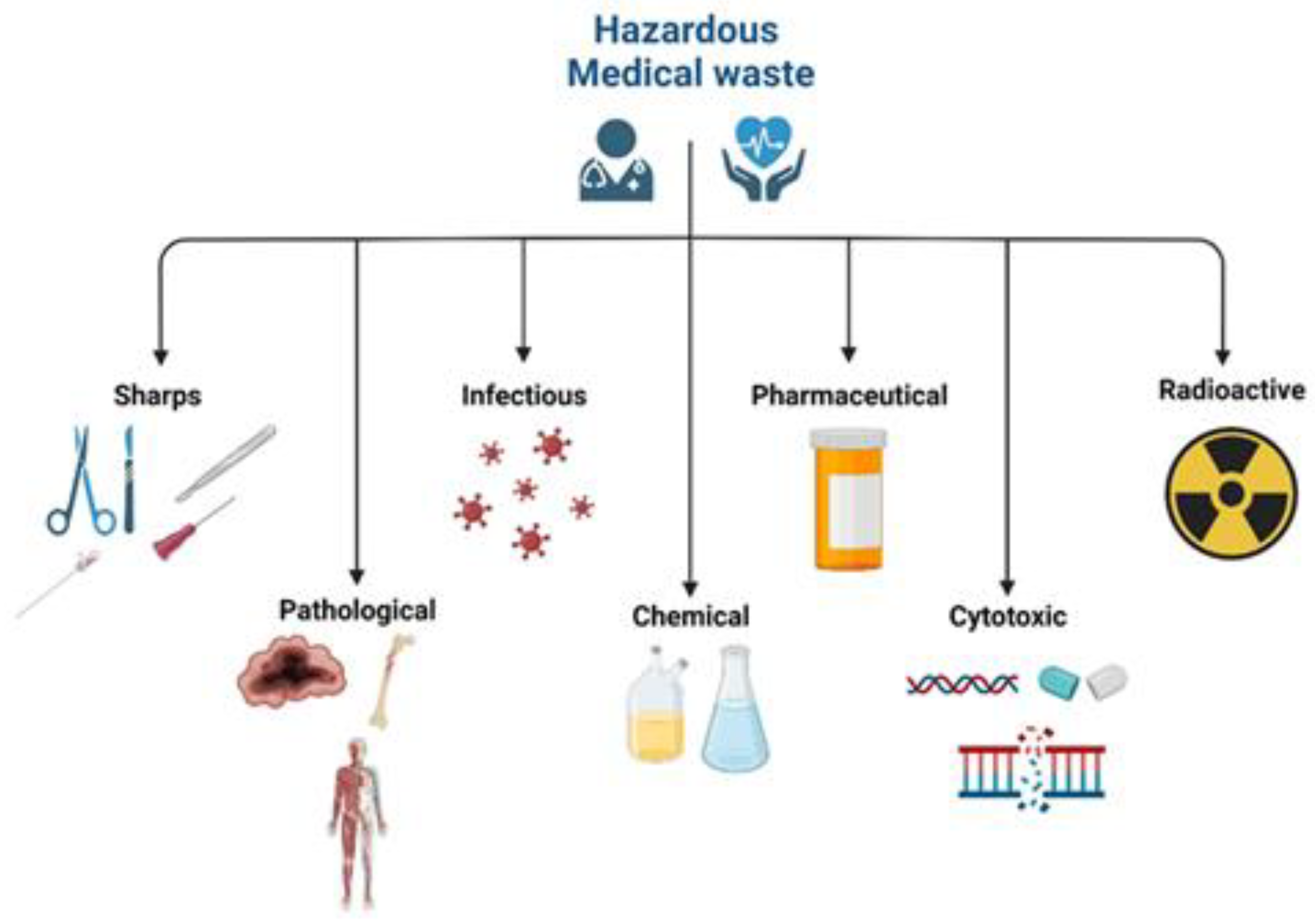
Figure 1. Different types of hazardous medical waste.
| Category (Examples) | World Health Organization (WHO) | EU | Source | |
|---|---|---|---|---|
| Hazardous | Sharps | Sharps | Sharps | Hospitals, clinics, laboratories, blood banks, nursing homes, veterinary clinics and labs |
| Organic matter, including body parts and blood | Pathological | Human tissue, body parts, organs, and blood preserves and bags | Hospitals, clinics, laboratories, mortuary and autopsy facilities, veterinary clinics and labs | |
| Waste with restrictions in collection and disposal due to infectivity | Infectious | Human and Animal Infectious | Hospitals, clinics, and laboratories | |
| Waste with no restrictions or special requirements for collection and disposal due to infectivity (e.g., plasters, casts, dressings, bed sheets, disposable clothing, etc.) | Infectious | Infectious | Hospitals, clinics, and laboratories | |
| Dangerous chemical materials and substances | Chemical | Chemical | Hospitals, clinics, and laboratories | |
| Other chemicals | Chemical | Chemical/ Unused hazardous medicines | Hospitals, clinics, and laboratories | |
| Cytotoxic and cytostatic medicines | Cytotoxic | Discarded unused medicines | Hospitals and laboratories | |
| Non-hazardous | Other chemicals (non-hazardous) | Pharmaceutical | Unused non-hazardous medicines | Hospitals, clinics, and laboratories |
| Dental clinics (care centres) amalgam waste | Amalgam (tooth filling) waste from dental clinics/centres | Amalgam waste from dental clinics/centres | Dental care centres and clinics |
MW can also affect physical and mental health and patients’ and health workers’ quality of life [17]. The plastic portion of MW is approximately 20% to 30% [18].
3. Medical Waste Management Process
Medical waste management is a series of steps where the MW generated is handled from the generation point until it can be disposed of safely. The steps of the MW management process are shown in Figure 2. The success of the waste management process is demonstrated in limiting the waste going for disposal and achieving a circular economy, where the materials used within the medical system are maximally utilised, reaching almost zero waste.
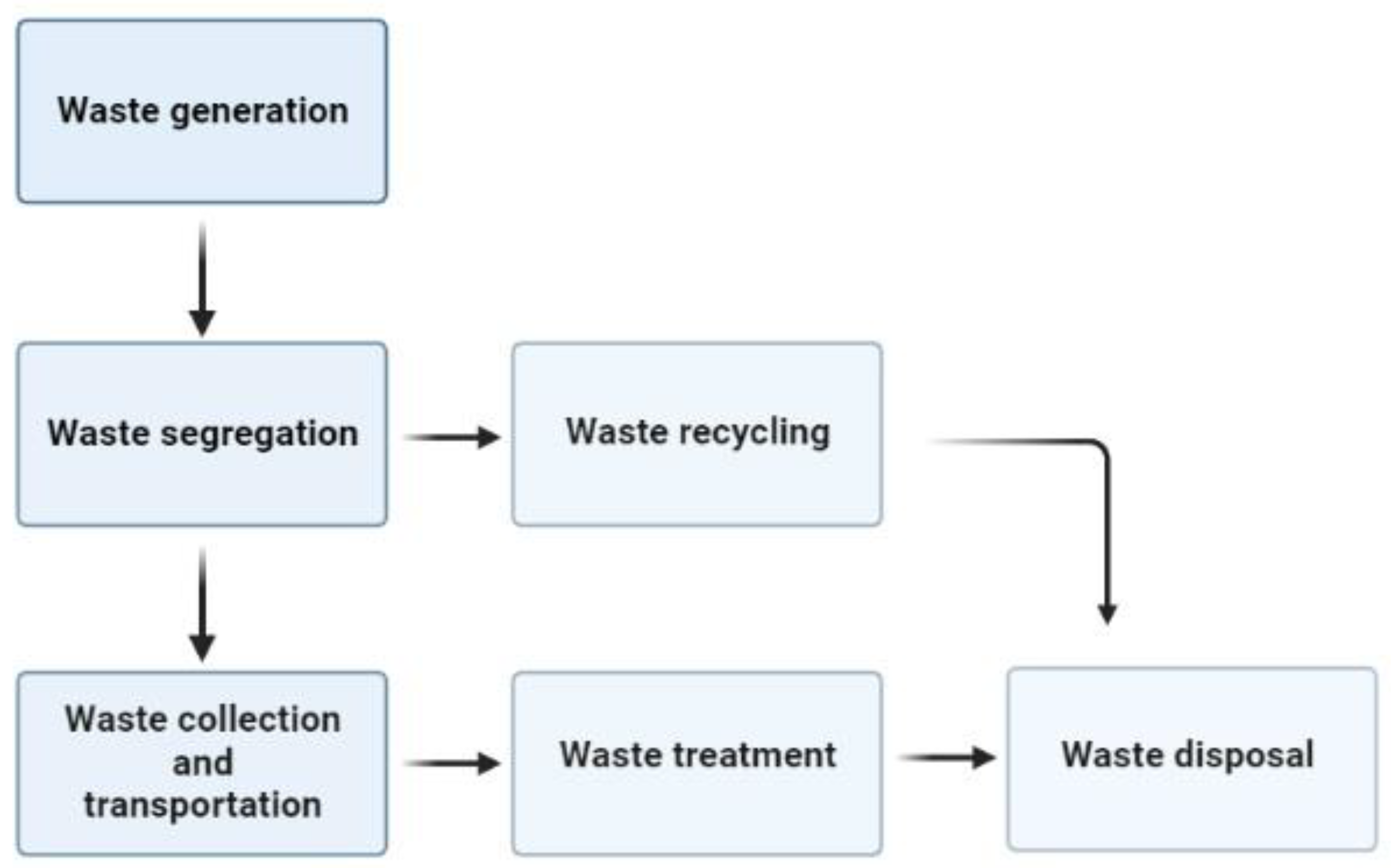
Figure 2. Flow scheme for medical waste management.
3.1. Waste Generation
The medical waste generated is of various classifications, as mentioned in the previous section. The critical aspect of this step is the amount of waste produced and how it is handled to prevent hazards to the personnel in contact with it. The waste generated from medical institutions can be minimised to reduce waste accumulation. The minimisation can be approached from different directions, such as reduction in waste at source, recycling, and stock management. The reduction in waste at the source can be achieved by reusing materials that will not harm the users, such as washable tablecloths, tableware, and refill containers for cleaning supplies [19]. Recycling can aid in minimising waste by recycling plastics and metals and composting food waste. Finally, stock management will help set an organised system of the medicines inventory to prevent duplication and purchase of unnecessary products that could expire, thus reducing potential waste [19].
3.2. Waste Segregation
Segregation identifies the various types of waste and how they can be collected separately. Segregation is mainly achieved by separating different categories of MW in different colour bins or bags specified for each category [19]. Therefore, this causes a problem when collecting from various sources due to the lack of standardisation of the colours associated with each waste category [14], thus increasing the needed time and financial cost of labour and equipment to separate the waste and direct it to the proper waste stream, resulting in a problem. The segregation should mostly occur at the point source except for the waste undergoing the same treatment, which could be separated in the treatment facility [19]. The sharp objects should always be separated at the source [19]. The segregation is carried out by medical staff, which requires training to safely dispose of waste to avoid infections [14]. If a mistake occurs while segregating waste, it should not be corrected to prevent the contamination of the other waste [19]. Medical waste should be stored safely to avoid unauthorised human contact, which can cause infections [14].
3.3. Waste Collection and Transportation
The frequency of MW collection should be as high as once per day to avoid the accumulation of waste, which can spread infections. In addition, the personnel responsible for collection should be equipped with safety gear to prevent contaminations and infections that should be safely disposed of [19]. The waste is collected from the health care entity and transported using secondary transportation to the treatment facility for disposal, recycling, and treatment processes. Treatment facilities are either located within the health care facility or off-site in a separate location [14].
3.4. Waste Treatment
Medical waste treatment is a process carried out before the disposal of MW to limit the hazardous effects of this type of waste on the environment and health. The lack of proper treatment can have several impacts, as follows [20]:
-
Poisoning from toxic elements,
-
Bacterial and fungal infections,
-
Release of toxins into the atmosphere,
-
Leaching to the soil and underlying aquifers,
-
Bioaccumulation,
-
Leaving a footprint on the environment,
-
Destruction of habitats.
In the production phase of any medical equipment, the impact of these types of equipment must be considered by performing a life cycle analysis (LCA) and practicing proper treatment techniques. However, the methods and techniques for treatment have minimal impact in terms of carbon emissions released into the ambient air. For example, a single intravitreal injection causes the release of 0.05 kg CO2e during the disposal phase [21].
Several treatment methods for MW are illustrated in Table 2, with their primary advantages and disadvantages. Despite these challenges, these methods can reduce the hazards mentioned earlier. The treatments currently in the field are incineration, autoclave disinfection, microwave disinfection, and mechanical and chemical disinfection [20].
Table 2. A comparison between treatment methods in terms of advantages and disadvantages.
| Treatment Method | Advantages | Disadvantages |
|---|---|---|
| Incineration |
|
|
| Autoclave disinfection |
|
|
| Microwave disinfection |
|
|
| Chemical disinfection |
|
|
3.4.1. Incineration
Incineration is the most widely practised treatment method due to its applicability to treating all waste types [22]. The incineration process is carried out in furnaces operated at temperatures of 800–1200 °C [22]. High temperatures kill pathogens, destroy 90% of organics, and change waste characteristics such as weight, volume, and shape [22]. This process is governed by several parameters such as [20]:
-
Mixing of waste,
-
Moisture content,
-
Amount of waste in the furnace,
-
Temperature,
-
Residence time,
-
Maintenance and repair.
Incineration produces fly ash and emissions such as dioxins, furans, and mercury [22]. Dioxins and furans are considered carcinogenic, have a half-life ranging from 7 to 11 years, and are persistent footprints on the environment [22]. Dioxin emissions can be reduced if the complete combustion of waste is achieved [22]. The dioxins emitted can also be treated using selective non-catalytic reduction (SNCR) [23]. This technology depends on the production of free nitrogen via the reaction between nitric oxide and ammonia, and this gas is considered to be of high effectiveness and low cost [23]. Mercury represents 3–9% of the emissions from incineration, which impacts the nervous system and general health [22]. Fly ash is the solid residue from incineration, rich in heavy metals [24]. Fly ash can be recycled but has to undergo chemical pre-treatment first by using ethylene diamine tetra acetic acid disodium (EDTA) or sodium sulphide, which removes the heavy metals from the fly ash [24]. Approximately 3 kg of CO2 is produced from burning 1 kg of clinical waste, therefore, incinerating MW contributes to global warming by releasing significant amounts of greenhouse gases (GHG), mainly CO2 [25].
3.4.2. Autoclave Disinfection
Autoclave disinfection is a treatment method using temperature and steam simultaneously to kill microbes [14]. It is operated at a lower temperature than incineration but with pressure and steam influence to achieve disinfection [19]. The operating conditions are 60 min, at 121 °C and 1 bar, followed by a cycle of 60 min at 134 °C to ensure the complete disinfection of waste [19]. The following aspects govern the operation of the autoclave [20]:
-
Temperature (121–134 °C),
-
Steam penetration,
-
Waste load,
-
Length of the treatment cycle,
-
Chamber air removal.
Due to the low operating temperatures of autoclaving, the waste appearance does not change, and the pathogens are not removed, which requires pre-treatment of the waste by incineration to be disposed of in landfills [14]. Thus, the autoclave is not optimum for all waste types.
3.4.3. Microwave Disinfection
Microwave disinfection uses low-temperature and high microwaves for the reverse polymerisation and degradation of organic substances and microorganisms [22]. The waves induce molecular bond vibrations, saving energy and preventing emissions, making it a more environmentally friendly method [22]. The disinfection is operated at temperatures ranging between 177 and 540 °C electromagnetic waves of wavelength ranging between 1 mm and 1 m and frequency ranges between 300 and 3000 MHz [22]. Microwave disinfection has high costs and can be combined with incineration and autoclave [22]. The following aspects govern the operation of this method [20]:
-
Waste characteristics,
-
Moisture content,
-
Microwave source strength,
-
Exposure time,
-
Degree of waste mixing.
3.4.4. Chemical Disinfection
Chemical disinfection is used to kill microorganisms and fight off pathogens by using chemicals [19]. It is primarily used for treating liquid infectious wastes such as blood, urine, faeces, or hospital sewage [19]. The chemical disinfectants that are commonly used are bleach solution (1%) or a diluted active chlorine solution (0.5%) [19]. In addition, other disinfectants such as lime, ozone, ammonium salts, and peracetic acid can be used [19]. This treatment method directly affects those in charge of the treatment due to the inhalation of volatile chemicals or irritations to the skin and eyes [19]. The following aspects govern the effectiveness of this method [20]:
-
pH,
-
Contact time,
-
Waste and chemical mixing,
-
Recirculation versus flow.
The residues of this treatment are liquid and solid residues [22]. The liquid residues are disposed of in the sewer system, and solid residues are disposed of in the landfill [22]. Determining an adequate treatment method involves defining the waste characteristics, type, and desired outcome, which should be checked against each treatment method to show the advantages and shortcomings of each process [20].
3.5. Waste Recycling
Waste recycling is using produced waste or by-products for the same or different purposes. Most of the waste produced by the medical sector is non-hazardous waste that is mainly disposed of in landfills. The use of waste dumps and landfills can be reduced by recycling used products such as plastics, batteries, paper, glass, metals, and silver used in photographic processing [19]. Food and organic waste can be used for composting purposes [19]. Fly ash from incineration can be used after treatment in concrete mixtures and as building blocks [24]. The heat produced from the incineration could be used to heat water for a centralised heating system [19].
3.6. Waste Disposal
Rejects of the previous steps are transported to a sanitary landfill for disposal. However, landfills are not the optimum solution for handling MW due to their environmental effects. These effects are soil and water pollution caused by leachate and gas emissions into the air due to waste degradation [22]. Thus, the waste being disposed of should be minimised to the most, and achieving a circular economy guarantees that. The long-term decomposition of waste is the primary process responsible for waste disposal in landfilling [22]. Preventive measures should be taken to ensure the safe disposal of MW, which are [19]:
-
Rapid cover of waste,
-
Burying it under the old municipal waste of minimum burial of three months,
-
Waterproof bottom,
-
Minimum 2 m above the water table,
-
No disposal of chemicals.
References
- Yoon, C.-W.; Kim, M.-J.; Park, Y.-S.; Jeon, T.-W.; Lee, M.-Y. A review of medical waste management systems in the Republic of Korea for hospital and medical waste generated from the COVID-19 pandemic. Sustainability 2022, 14, 3678.
- Prem Ananth, A.; Prashanthini, V.; Visvanathan, C. Healthcare waste management in Asia. Waste Manag. 2010, 30, 154–161.
- World Health Organization (WHO). Health-Care Waste. Available online: https://www.who.int/news-room/fact-sheets/detail/health-care-waste (accessed on 15 May 2022).
- Ordway, A.; Pitonyak, J.S.; Johnson, K.L. Durable medical equipment reuse and recycling: Uncovering hidden opportunities for reducing medical waste. Disabil. Rehabil. Assist. Technol. 2020, 15, 21–28.
- Harding, C.; Van Loon, J.; Moons, I.; De Win, G.; Du Bois, E. Design opportunities to reduce waste in operating rooms. Sustainability 2021, 13, 2207.
- Lee, B.-K.; Ellenbecker, M.J.; Moure-Eraso, R. Analyses of the recycling potential of medical plastic wastes. Waste Manag. 2002, 22, 461–470.
- Patrício Silva, A.L.; Prata, J.C.; Walker, T.R.; Campos, D.; Duarte, A.C.; Soares, A.M.V.M.; Barcelò, D.; Rocha-Santos, T. Rethinking and optimising plastic waste management under COVID-19 pandemic: Policy solutions based on redesign and reduction of single-use plastics and personal protective equipment. Sci. Total Environ. 2020, 742, 140565.
- Talvitie, J.; Mikola, A.; Koistinen, A.; Setälä, O. Solutions to microplastic pollution—Removal of microplastics from wastewater effluent with advanced wastewater treatment technologies. Water Res. 2017, 123, 401–407.
- Zheng, J.; Suh, S. Strategies to reduce the global carbon footprint of plastics. Nat. Clim. Chang. 2019, 9, 374–378.
- United Nations (UN). Transforming Our World: The 2030 Agenda for Sustainable Development. Available online: https://sdgs.un.org/2030agenda (accessed on 8 May 2022).
- Sharma, R.; Sharma, M.; Sharma, R.; Sharma, V. The impact of incinerators on human health and environment. Rev. Environ. Health 2013, 28, 67–72.
- Rizan, C.; Bhutta, M.F.; Reed, M.; Lillywhite, R. The carbon footprint of waste streams in a UK hospital. J. Clean. Prod. 2021, 286, 125446.
- Tsai, W.-T. Analysis of medical waste management and impact analysis of COVID-19 on its generation in Taiwan. Waste Manag. Res. 2021, 39, 27–33.
- Windfeld, E.S.; Brooks, M.S.-L. Medical waste management—A review. J. Environ. Manag. 2015, 163, 98–108.
- Komilis, D.; Makroleivaditis, N.; Nikolakopoulou, E. Generation and composition of medical wastes from private medical microbiology laboratories. Waste Manag. 2017, 61, 539–546.
- Zhou, H.; Yu, X.; Alhaskawi, A.; Dong, Y.; Wang, Z.; Jin, Q.; Hu, X.; Liu, Z.; Kota, V.G.; Abdulla, M.H.A.H.; et al. A deep learning approach for medical waste classification. Sci. Rep. 2022, 12, 2159.
- Commision of the European Communities. Guidance on Classification of Waste According to EWC-Stat Categories, Supplement to the Manual for the Implementation of the Regulation (EC) No 2150/2002 on Waste Statistics; Commision of the European Communities: Brussels, Belgium, 2010; Volume 2.
- Huang, M.-C.; Lin, J.J. Characteristics and management of infectious industrial waste in Taiwan. Waste Manag. 2008, 28, 2220–2228.
- International Committee of the Red Cross (ICRC). Medical Waste Management; ICRC: Geneva, Switzerland, 2011; pp. 12–14, 51–77.
- Akter, N. Medical waste management: A review. Res. Rep. Health Stud. 2000, XXVIII, 370–394.
- Power, B.; Brady, R.; Connell, P. Analysing the carbon footprint of an intravitreal injection. J. Ophthalmic Vis. Res. 2021, 16, 367–376.
- Giakoumakis, G.; Politi, D.; Sidiras, D. Medical waste treatment technologies for energy, fuels, and materials production: A review. Energies 2021, 14, 8065.
- Wielgosiński, G.; Czerwińska, J.; Szymańska, O.; Bujak, J. Simultaneous NOx and dioxin removal in the SNCR process. Sustainability 2020, 12, 5766.
- Ababneh, A.; Al-Rousan, R.; Gharaibeh, W.; Abu-Dalo, M. Recycling of pre-treated medical waste fly ash in mortar mixtures. J. Mater. Cycles Waste Manag. 2020, 22, 207–220.
- Wyssusek, K.H.; Keys, M.T.; van Zundert, A.A.J. Operating room greening initiatives—The old, the new, and the way forward: A narrative review. Waste Manag. Res. 2018, 37, 3–19.
More
Information
Subjects:
Green & Sustainable Science & Technology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
5.6K
Revisions:
4 times
(View History)
Update Date:
06 Dec 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





