The relationship between migraine and tension-type headache (TTH) with Parkinson’s disease (PD) is controversial, while a common pathophysiological link remains obscure. The aim of researchers is to investigate the association between PD, migraine and TTH.
1. Introduction
Although Parkinson’s disease (PD) is classified as a motor neurodegenerative disorder, non-motor symptoms (NMSs)are common, such as sleep disorders, depression, cognitive deficits and pain
[1]. Among PD patients, different pain phenotypes and/or classification shave been described: PD-related (including fluctuation-related, dyskinesia -related and central pain) vs. non-PD-related pain; primary vs. secondary (musculoskeletal system) pain; nociceptive vs. neuropathic; chronic vs. acute; and pain according to different body parts
[2][3][4][5]. However, the exact pain etiology in PD remains unclear; as a consequence, therapeutic options are often ineffective
[6].
Primary headaches (i.e., migraine and tension-type headache (TTH)) are commonpain disorders with several comorbidities, such as cardiovascular disease, stroke, depression and various dementias, and are accompanied by a substantial socioeconomic impact
[7][8].Over the previous two decades, several studies have suggested a link between primary headaches and PD
[9][10][11], while others have produced conflicting results
[12][13]. Barbanti et al. identified a lifetime migraine prevalence of 27.8% and a current migraine prevalence of 13.1% in a population of PD patients
[14]. Moreover, a cohort study showed that subjects with a midlife history of headache and, particularly, those with migraine with aura had an increased likelihood of PD
[9].By contrast, Nunes et al.
[15] demonstrated that PD patients had a lower lifetime prevalence of headache than controls. Previous studies have focused on the relationship between migraine and PD, and a prior validation study reported that 80% of individuals with non-migrainous headache might have TTH
[16]. However, the supposed overlapping PD and headache pathophysiological mechanisms remain obscure
[17]. Despite the high prevalence of migraine across various PD populations
[14][15], headache remains an underestimated and undertreated NMS contributing to a poor quality of life among PD patients
[14].
A clarification of the examined relationship will provide valuable knowledge to neurologists in determining the modifiable causes of poor outcomes.
2. Headache Prevalence in PD Patients
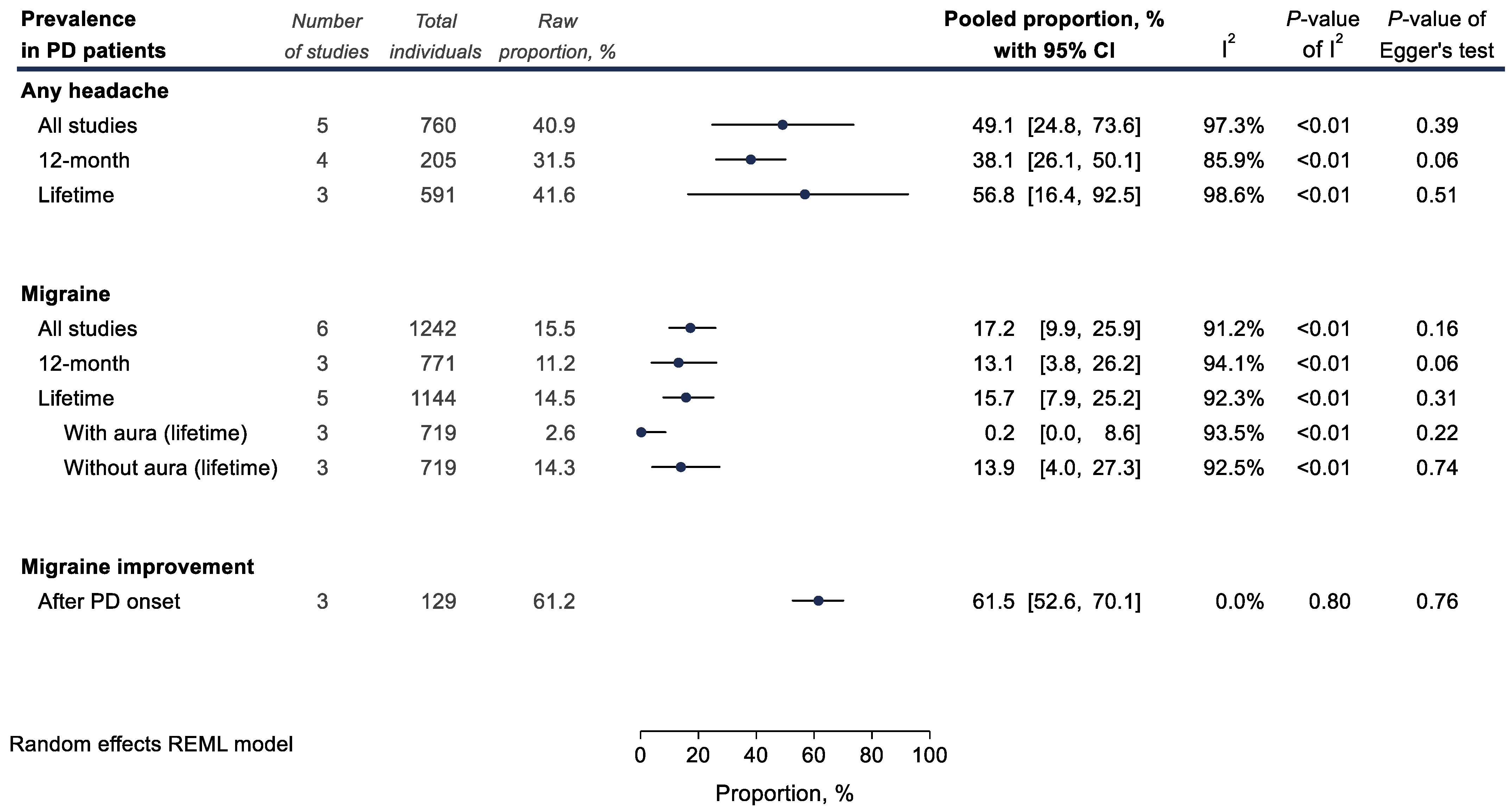
The overall pooled prevalence of any headache (including migraine and TTH) among PD patients was 49.1% (5 studies; 760 PD patients; 40.9%; 49.1% with 95% CI 24.8–73.6; and I2 = 97.3%, Figure 1). The 12-month prevalence of migraine among PD patients was calculated at 13.1% (3 studies; 771 PD patients; 11.2%; 13.1% with 95% CI 3.8–26.2; and I2 = 94.1%), while the lifetime prevalence was expectedly higher at 15.7% (5 studies; 1144 PD patients; 14.5%; 15.7% with 95% CI 7.9–25.2; and I2 = 92.3%, Figure 1). Only very few PD patients had received a diagnosis of migraine with aura (3 studies; 719 PD patients; 2.6%; 0.2% with 95% CI 0.0–8.6; and I2 = 93.5%).
Figure 2. Meta-analyses of proportions examining headache prevalence (%) among Parkinson’s disease (PD) patients. Results of each individual random effects meta-analysis are depicted as black data markers; 95% confidence intervals (CI) are indicated by the black error bars. I2 reflects each meta-analysis heterogeneity.
3. Association between PD and Migraine
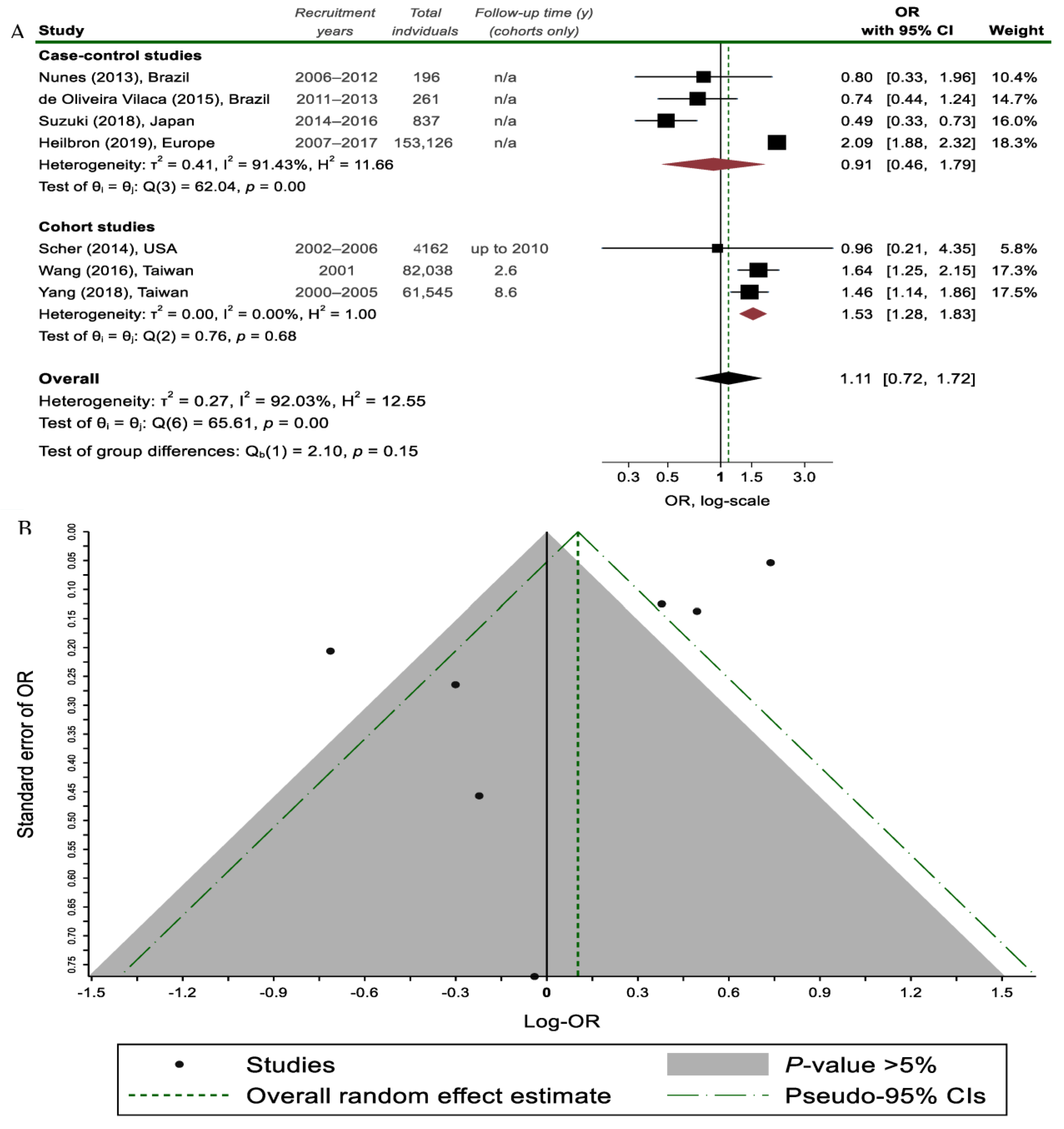
Overall, regarding the relationship between PD and migraine, no statistically significant association was found (7 studies; 302,165 individuals; ORpooled = 1.11, 95% CI 0.72–1.72; and I2 = 92.0%; Figure 2).
Figure 2. (
A) Random effects meta-analysis on the association between migraine headaches and Parkinson’s disease (PD) status stratified by study design; (
B) Funnel plot, where each study is depicted as a dot. The light grey shaded area contains studies with non-significant results (
p > 0.05)
[7][9][15][18][19][20][21].
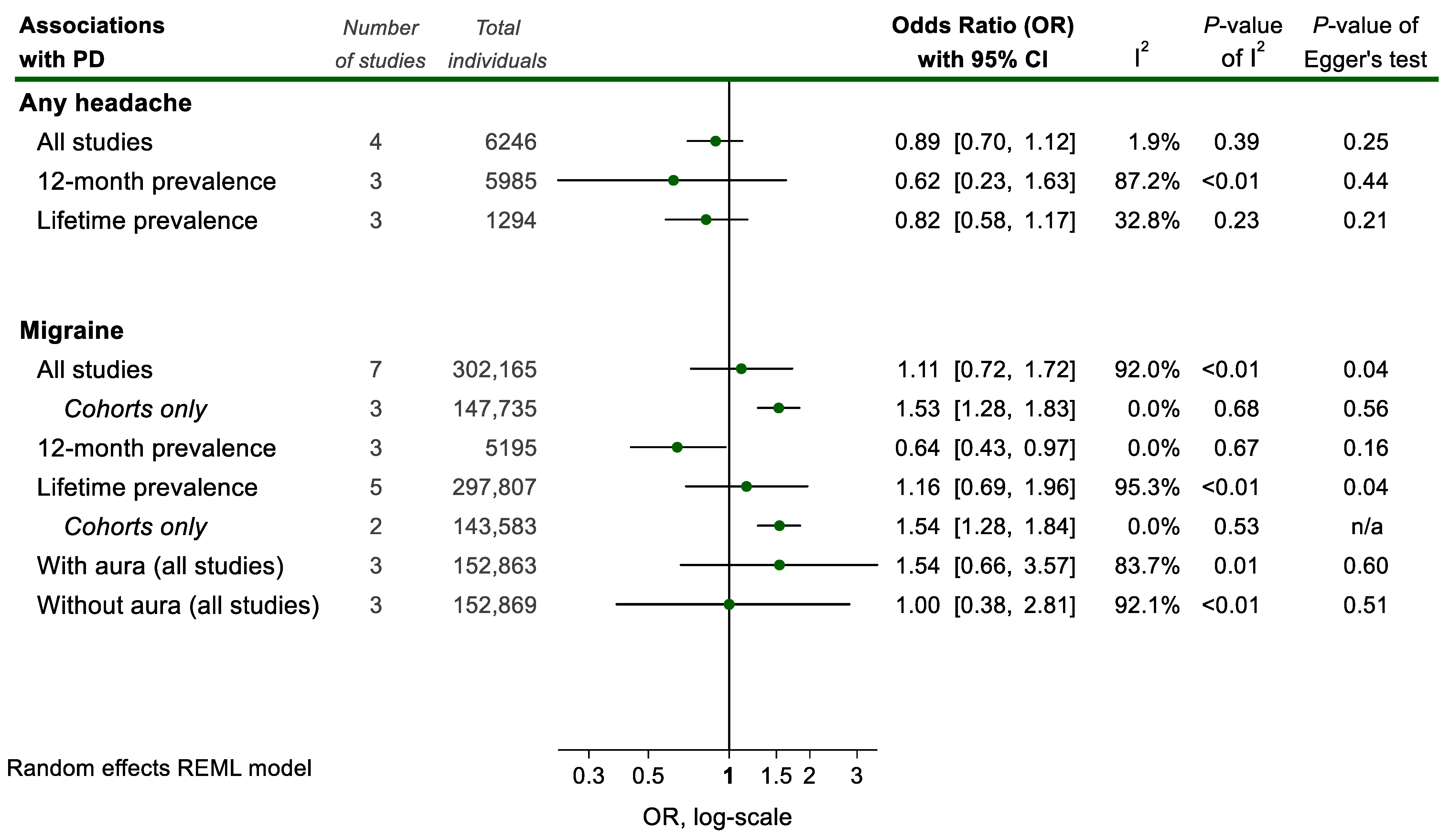
This was also the case when pooling studies specifically on migraine with or without aura (Figure 3).
Figure 3. Meta-analyses of associations between headache and Parkinson Disease (PD) status. Results of each individual random effects meta-analysis (odds ratios (OR)) are depicted as green data markers; 95% confidence intervals (CI) are indicated by the black error bars. I2 reflects each meta-analysis heterogeneity.
However, when restricting the analysis to the 2 cohort studies on lifetime migraine prevalence, the result achieves significance and translates to an increased risk of PD among lifetime migraineurs (2 studies; 143,583 individuals; ORpooled = 1.54, 95% CI 1.28–1.84; and I2 = 0%, Figure 2). Notably, case-control studies failed to show a statistically significant association, possibly due to considerable between-study heterogeneity (Figure 1). On the contrary, in studies focusing only on a 12-month migraine prevalence, an inverse association with PD was found (3 studies; 5195 individuals; ORpooled = 0.64, 95% CI 0.43–0.97; and I2 = 0%, Figure 3). These contrasting findings could be partially explained by the potentially favorable effect of PD on the course of migraine if seen together with the result regarding the proportion of PD patients reporting migraine improvement after PD onset (3 studies; 129 PD patients; 61.2%; 61.5%, 95% CI 52.6–70.1; and I2 = 0%, Figure 1).
4. Association between PD and TTH
Only 3 studies
[15][18][22] examined the prevalence and/or associations between TTH and PD with conflicting results. Researchers were unable to pool this data due to the vastly different methodological designs of the respective studies. Yang et al. suggest that TTH suffering individuals are at an increased risk of incident PD later in life. This is in line with the findings from a small PD patient sample by Sampaio Rocha-Filho et al.
[22], where TTH prevalence among PD individuals was high (67.4%). On the contrary, Nunes et al.
[15] suggest that PD is associated with a lower TTH 12-month prevalence. These results are directionally similar with the ones pertaining to the PD-migraine association.
5. Genetics and Family History of Migraines in PD Patients
Whether genetics and a family history of migraines in PD patients influences the course of PD is not clear, as relevant data are reported in only 3 studies
[13][14][18]. The course of migraine after the onset of PD in patients without a family history of migraine differed to that of those with a family history
[18]. PD onset seemed to alter the course of migraine among migraineurs without a family history of migraine but not among those with a self-reported family history.
[13]. However, Barbanti et al.
[14] indirectly refute this finding, as almost half of PD patients without a family history of migraine had current migraine. Moreover, the lower prevalence of family history of migraine among PD migraineurs could not be explained.