
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Anusak Kerdsin | -- | 1686 | 2022-11-29 03:26:26 | | | |
| 2 | Lindsay Dong | Meta information modification | 1686 | 2022-11-29 12:34:15 | | |
Video Upload Options
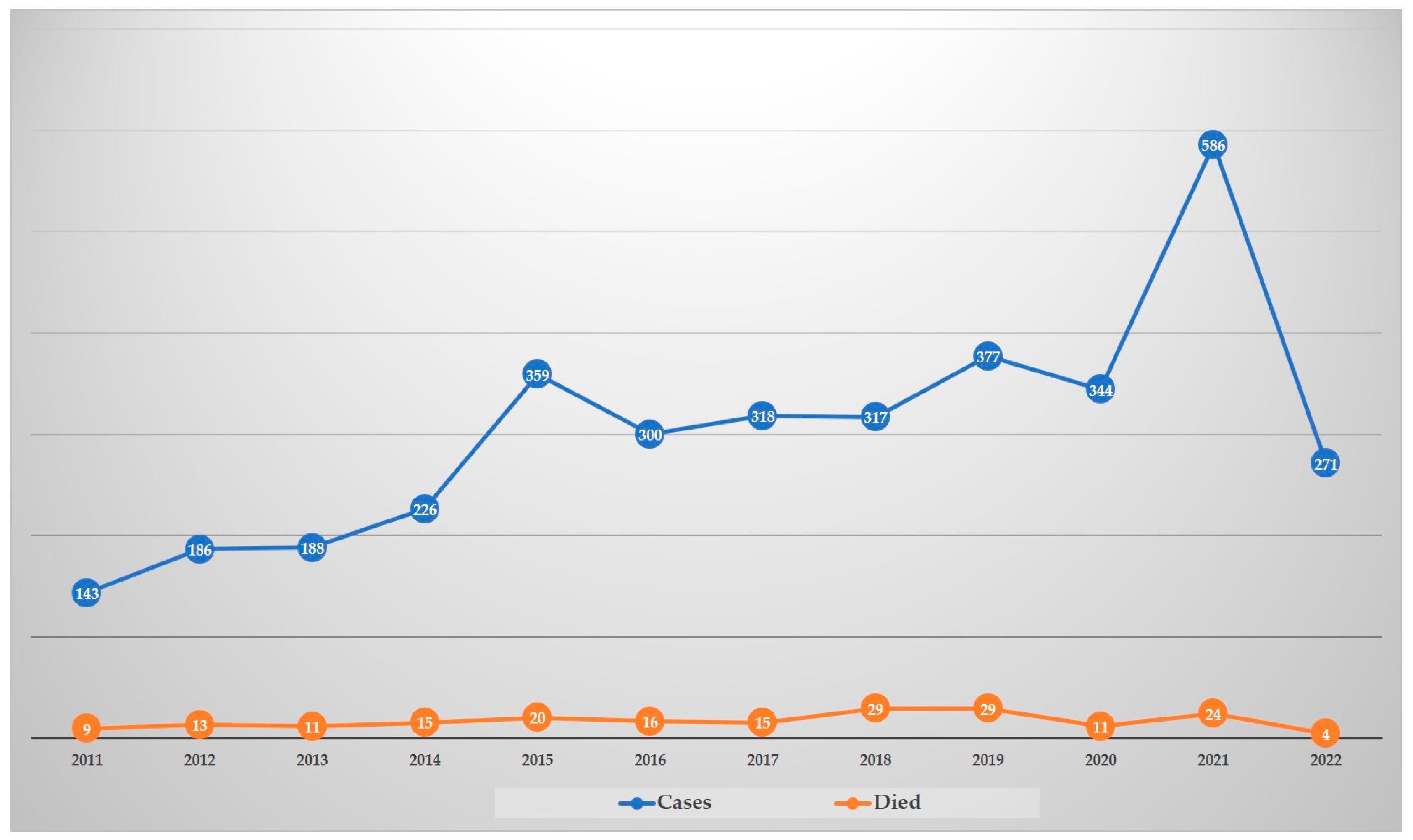
Streptococcus suis is a zoonotic pathogen causing substantial economic losses to the pig industry, as well as being a human health burden due to infections worldwide, especially in Southeast Asia. In Thailand, there was high cumulative incidence in humans during 1987–2021, mostly in males. At least five large outbreaks have been documented after the largest outbreak in China in 2005, which was related to the consumption of raw pork or dishes containing pig’s blood. The major clinical features are sepsis or meningitis, with hearing loss a major complication of S. suis disease. Thai human S. suis isolates have shown diversity in serotypes and sequence types (STs), with serotype 2 and STs 1 and 104 being major genotypes. β-Lactam antibiotics can be used in empirical treatment for human S. suis infections; however, intermediate resistance to penicillin has been reported. Reducing S. suis incidence in Thailand requires a multidimensional approach, with combined efforts from the government and public health sectors through policy, regulations, education, and active surveillance.
1. Introduction
2. Epidemiology of Human S. suis Infections in Thailand
3. Genotypes of Thai Human S. suis Strains
As shown in Table 1, for S. suis isolated from patients in Thailand, serotype 2 (93.4%) was dominant, followed by serotypes 14 (5.2%), 24 (0.6%), 5 (0.4%), 4 (0.1%), 9 (0.1%), 31 (0.1%), and unencapsulated (0.1%), respectively [17][20][21][22][23]. MLST classified serotype 2 into five CCs: CC1, CC25, CC28, CC104, and CC233/379. Of these, CC1 is a major CC of human S. suis infection in this country and ST1 is the main ST in CC1 [21], while serotype 14 was classified to only CC1, with ST105 predominant [21][23]. For serotype 2, ST104, ST25, ST28, and ST233 were the main STs in CC104, CC25, CC28, and CC233/379, respectively. Notably, STs 1 and 104 for serotype 2 are the predominant STs in Thai human infections, and CC104, CC233/379, and CC221/234 are found exclusively in Thailand [20][21][24].
| Serotype | Clonal Complex | Sequence Type | Reference |
|---|---|---|---|
| 2 | 1 | 1, 11, 105, 126, 144, 298, 337 | [17][18][19][20][21][22][23][25][26][27][28][29] https://pubmlst.org/organisms/streptococcus-suis (accessed on 5 October 2022) |
| 25 | 25, 102, 103, 380, 381, 395, 515, 516 | ||
| 28 | 28, 382 | ||
| 104 | 101, 104, 391, 392, 393, 512, 513, 514 | ||
| 233/379 | 233, 379, 1656, 1713 | ||
| 1687/1688 | 1687, 1688 | ||
| Singleton | 232, 236 | ||
| 4 | 94 | 94 | |
| 5 | 221/234 | 221 | |
| Singleton | 181, 235 | ||
| 9 | 16 | 16 | |
| 14 | 1 | 11, 105, 127 | |
| 24 | 221/234 | 221, 234 | |
| 31 (Unencapsulated) |
221/234 | 221 | |
| Unencapsulated serotype 2 or 1/2 |
28 | 28 |
4. Antimicrobial Susceptibility
Other studies have revealed that Thai S. suis isolates were susceptible to penicillin [13]. This contrasted with Nakaranurack et al. (2017), who reported that 6 out of 11 Thai S. suis isolates were intermediately resistance to penicillin, whereas cefotaxime and vancomycin were completely susceptible [33]. However, a study in 2021 demonstrated that 448 S. suis isolates recovered from human infections in Thailand had 8.2% intermediate resistance to penicillin, while they were all susceptible to cefepime and ceftriaxone [34].
Resistance to tetracycline (98.2%), clindamycin (94%), erythromycin (92.4%), and azithromycin (82.6%) with the resistance genes tet(O) and ermB were the predominant determinant genes of tetracycline and erythromycin (also macrolide-lincosamide–streptogramin B (MLSB)) resistance detected in 448 S. suis isolates [34]. Resistance to tetracycline appeared common in S. suis from human infections worldwide [35][36][37][38][39], whereas the resistance rates to erythromycin were low in Poland, Hong Kong, and Vietnam [35][36][40]. Although tet(O) is prevalent in human S. suis in Thailand, the tet(M) gene is the most widespread in human S. suis in China and Vietnam [36][38]. The ermB gene was predominant in human isolates in Vietnam and Thailand, while mefA was present in Hong Kong [34][36]. This may indicate differences in the local spread of tetracycline and erythromycin-resistance genes among human S. suis isolates in different countries or geographical regions.
5. Public Health Control
6. Conclusions
References
- Goyette-Desjardins, G.; Auger, J.P.; Xu, J.; Segura, M.; Gottschalk, M. Streptococcus suis, an important pig pathogen and emerging zoonotic agent-an update on the worldwide distribution based on serotyping and sequence typing. Emerg. Microbes. Infect. 2014, 3, e45.
- Segura, M.; Aragon, V.; Brockmeier, S.L.; Gebhart, C.; De Greeff, A.; Kerdsin, A.; O’Dea, M.A.; Okura, M.; Saléry, M.; Schultsz, C.; et al. Update on Streptococcus suis Research and Prevention in the Era of Antimicrobial Restriction: 4th International Workshop on S. suis. Pathogens 2020, 9, 374.
- Kerdsin, A.; Segura, M.; Fittipaldi, N.; Gottschalk, M. Sociocultural Factors Influencing Human Streptococcus suis Disease in Southeast Asia. Foods 2022, 11, 1190.
- Thongsawad, S. Burden and Epidemiological Characterisations of Streptococcus suis in Chiang Mai, Thailand. Ph.D. Thesis, The University of Edinburgh, Edinburgh, UK, 2016.
- Rayanakorn, A.; Ademi, Z.; Liew, D.; Lee, L.-H. Burden of disease and productivity impact of Streptococcus suis infection in Thailand. PLoS Negl. Trop. Dis. 2021, 15, e0008985.
- Phuapradit, P.; Boongird, P.; Boonyakarnkul, S.; Niramarnsakul, S.; Ponglikitmongkol, S.; Vorachit, M. Meningitis caused by Streptococcus suis in humans. Intern. Med. 1987, 3, 120–122.
- Yu, H.; Jing, H.; Chen, Z.; Zheng, H.; Zhu, X.; Wang, H.; Wang, S.; Liu, L.; Zu, R.; Luo, L.; et al. Streptococcus suis study groups. Human Streptococcus suis outbreak, Sichuan, China. Emerg. Infect. Dis. 2006, 12, 914–920.
- Teekakirikul, P.; Wiwanitkit, V. Streptococcus suis infection: Overview of case reports in Thailand. S. Asian J. Trop. Med. Public Health 2003, 34 (Suppl. 2), 178–183.
- Vilaichone, R.K.; Vilaichone, W.; Nunthapisud, P.; Wilde, H. Streptococcus suis infection in Thailand. J. Med. Assoc. Thai. 2002, 85 (Suppl. 1), S109–S117.
- Donsakul, K.; Dejthevaporn, C.; Witoonpanich, R. Streptococcus suis infection: Clinical features and diagnostic pitfalls. S. Asian J. Trop. Med. Public Health 2003, 34, 154–158.
- Suankratay, C.; Intalapaporn, P.; Nunthapisud, P.; Arunyingmongkol, K.; Wilde, H. Streptococcus suis meningitis in Thailand. S. Asian J. Trop. Med. Public Health 2004, 35, 868–876.
- Rusmeechan, S.; Sribusara, P. Streptococcus suis meningitis: The newest serious infectious disease. J. Med. Assoc. Thail. 2008, 91, 654–658.
- Wangkaew, S.; Chaiwarith, R.; Tharavichitkul, P.; Supparatpinyo, K. Streptococcus suis infection: A series of 41 cases from Chiang Mai University Hospital. J. Infect. 2006, 52, 455–460.
- Fongcom, A.; Pruksakorn, S.; Mongkol, R.; Tharavichitkul, P.; Yoonim, N. Streptococcus suis infection in northern Thailand. J. Med. Assoc. Thail. 2001, 84, 1502–1508.
- Le, H.T.T.; Sugiyama, N.; Duangsonk, K.; Tharavichitkul, P.; Osawa, R. Phenotypic and PCR-based identification of bacterial strains isolated from patients with suspected Streptococcus suis infection in northern Thailand. Jpn. J. Infect. Dis. 2012, 65, 171–174.
- Tarini, N.M.A.; Setiabudy, M.; Susilawathi, N.; Fatmawati, N.; Mayura, I.; Darwinata, E.; Sudiariani, N. Misidentification of S. suis as a Zoonotic Agent. Open Access Maced. J. Med. Sci. 2019, 7, 2309–2312.
- Hatrongjit, R.; Kerdsin, A.; Gottschalk, M.; Takeuchi, D.; Hamada, S.; Oishi, K.; Akeda, Y. First human case report of sepsis due to infection with Streptococcus suis serotype 31 in Thailand. BMC Infect. Dis. 2015, 15, 392.
- Prapasiri, P.; Owusu, J.T.; Thammathitiwat, S.; Ditsungnoen, D.; Boonmongkon, P.; Sangwichian, O.; Prasert, K.; Srihapanya, S.; Sornwong, K.; Kerdsin, A.; et al. Streptococcus suis Infection in Hospitalized Patients, Nakhon Phanom Province, Thailand. Emerg. Infect. Dis. 2015, 21, 345–348.
- Takeuchi, D.; Kerdsin, A.; Pienpringam, A.; Loetthong, P.; Samerchea, S.; Luangsuk, P.; Khamisara, K.; Wongwan, N.; Areeratana, P.; Chiranairadul, P.; et al. Population-Based Study of Streptococcus suis Infection in Humans in Phayao Province in Northern Thailand. PLoS ONE 2012, 7, e31265.
- Kerdsin, A.; Dejsirilert, S.; Puangpatra, P.; Sripakdee, S.; Chumla, K.; Boonkerd, N.; Polwichai, P.; Tanimura, S.; Takeuchi, D.; Nakayama, T.; et al. Genotypic Profile of Streptococcus suis Serotype 2 and Clinical Features of Infection in Humans, Thailand. Emerg. Infect. Dis. 2011, 17, 835–842.
- Kerdsin, A.; Akeda, Y.; Takeuchi, D.; Dejsirilert, S.; Gottschalk, M.; Oishi, K. Genotypic diversity of Streptococcus suis strains isolated from humans in Thailand. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 917–925.
- Takamatsu, D.; Wongsawan, K.; Osaki, M.; Nishino, H.; Ishiji, T.; Tharavichitkul, P.; Khantawa, B.; Fongcom, A.; Takai, S.; Sekizaki, T. Streptococcus suis in humans, Thailand. Emerg. Infect. Dis. 2008, 14, 181–183.
- Kerdsin, A.; Oishi, K.; Sripakdee, S.; Boonkerd, N.; Polwichai, P.; Nakamura, S.; Uchida, R.; Sawanpanyalert, P.; Dejsirilert, S. Clonal dissemination of human isolates of Streptococcus suis serotype 14 in Thailand. J. Med. Microbiol. 2009, 58, 1508–1513.
- Kerdsin, A.; Hatrongjit, R.; Wongsurawat, T.; Jenjaroenpun, P.; Chopjitt, P.; Boueroy, P.; Fittipaldi, N.; Zheng, H.; Gottschalk, M. Genomic Characterization of Streptococcus suis Serotype 24 Clonal Complex 221/234 From Human Patients. Front. Microbiol. 2021, 12, 812436.
- Brizuela, J.; Kajeekul, R.; Roodsant, T.; Riwload, A.; Boueroy, P.; Thaipadungpanit, J.; Jenjaroenpun, P.; Wongsurawat, T.; Batty, E.; van der Putten, B.; et al. Streptococcus suis outbreak in Thailand caused by an emerging zoonotic strain with acquired multidrug resistance. Microb. Genom. 2022; accepted.
- Kerdsin, A.; Gottschalk, M.; Hatrongjit, R.; Hamada, S.; Akeda, Y.; Oishi, K. Fatal Septic Meningitis in Child Caused by Streptococcus suis Serotype 24. Emerg. Infect. Dis. 2016, 22, 1519–1520.
- Kerdsin, A.; Dejsirilert, S.; Sawanpanyalert, P.; Boonnark, A.; Noithachang, W.; Sriyakum, D.; Simkum, S.; Chokngam, S.; Gottschalk, M.; Akeda, Y.; et al. Sepsis and spontaneous bacterial peritonitis in Thailand. Lancet 2011, 378, 960.
- Kerdsin, A.; Takeuchi, D.; Gottschalk, M.; Hamada, S.; Akeda, Y.; Oishi, K. A human case of Streptococcus suis infection caused by an unencapsulated strain. JMM Case Rep. 2014, 1, e002329.
- Kerdsin, A.; Hatrongjit, R.; Gottschalk, M.; Takeuchi, D.; Hamada, S.; Akeda, Y.; Oishi, K. Emergence of Streptococcus suis serotype 9 infection in humans. J. Microbiol. Immunol. Infect. 2017, 50, 545–546.
- Kerdsin, A.; Takeuchi, D.; Nuangmek, A.; Akeda, Y.; Gottschalk, M.; Oishi, K. Genotypic Comparison between Streptococcus suis Isolated from Pigs and Humans in Thailand. Pathogens 2020, 9, 50.
- Maneerat, K.; Yongkiettrakul, S.; Kramomtong, I.; Tongtawe, P.; Tapchaisri, P.; Luangsuk, P.; Chaicumpa, W.; Gottschalk, M.; Srimanote, P. Virulence Genes and Genetic Diversity of Streptococcus suis Serotype 2 Isolates from Thailand. Transbound. Emerg. Dis. 2013, 60 (Suppl. 2), 69–79.
- Tharavichitkul, P.; Wongsawan, K.; Takenami, N.; Pruksakorn, S.; Fongcom, A.; Gottschalk, M.; Khanthawa, B.; Supajatura, V.; Takai, S. Correlation between PFGE Groups and mrp/epf/sly Genotypes of Human Streptococcus suis Serotype 2 in Northern Thailand. J. Pathog. 2014, 2014, 350416.
- Nakaranurack, C.; Puttilerpong, C.; Suwanpimolkul, G. A Decennium of Etiology and Antimicrobial Susceptibility Patterns in Patients with Infective Endocarditis at a University Hospital, Thailand. Jpn. J. Infect. Dis. 2017, 70, 295–300.
- Bamphensin, N.; Chopjitt, P.; Hatrongjit, R.; Boueroy, P.; Fittipaldi, N.; Gottschalk, M.; Kerdsin, A. Non-Penicillin-Susceptible Streptococcus suis Isolated from Humans. Pathogens 2021, 10, 1178.
- Bojarska, A.; Molska, E.; Janas, K.; Skoczynska, A.; Stefaniuk, E.; Hryniewicz, W.; Sadowy, E. Streptococcus suis in invasive human infections in Poland: Clonality and determinants of virulence and antimicrobial resistance. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 917–925.
- Hoa, N.T.; Chieu, T.T.; Nghia, H.D.; Mai, N.T.; Anh, P.H.; Wolbers, M.; Baker, S.; Campbell, J.I.; Chau, N.V.; Hien, T.T.; et al. The antimicrobial resistance patterns and associated determinants in Streptococcus suis isolated from humans in southern Vietnam, 1997–2008. BMC Infect. Dis. 2011, 11, 6.
- Marie, J.; Morvan, H.; Berthelot-Hérault, F.; Sanders, P.; Kempf, I.; Gautier-Bouchardon, A.V.; Jouy, E.; Kobisch, M. Antimicrobial susceptibility of Streptococcus suis isolated from swine in France and from humans in different countries between 1996 and 2000. J. Antimicrob. Chemother. 2002, 50, 201–209.
- Ye, C.; Bai, X.; Zhang, J.; Jing, H.; Zheng, H.; Du, H.; Cui, Z.; Zhang, S.; Jin, D.; Xu, Y.; et al. Spread of Streptococcus suis sequence type 7, China. Emerg. Infect. Dis. 2008, 14, 787–791.
- Chang, B.; Wada, A.; Ikebe, T.; Ohnishi, M.; Mita, K.; Endo, M.; Matsuo, H.; Asatuma, Y.; Kuramoto, S.; Sekiguchi, H.; et al. Characteristics of Streptococcus suis isolated from patients in Japan. Jpn. J. Infect. Dis. 2006, 59, 397–399.
- Chu, Y.W.; Cheung, T.K.; Chu, M.Y.; Tsang, V.Y.; Fung, J.T.; Kam, K.M.; Lo, J.Y. Resistance to tetracycline, erythromycin and clindamycin in Streptococcus suis serotype 2 in Hong Kong. Int. J. Antimicrob. Agents 2009, 34, 181–182.
- Takeuchi, D.; Kerdsin, A.; Akeda, Y.; Chiranairadul, P.; Loetthong, P.; Tanburawong, N.; Areeratana, P.; Puangmali, P.; Nakayama, T.; Yamamoto, K.; et al. Impact of a Food Safety Campaign on Streptococcus suis Infection in Humans in Thailand. Am. J. Trop. Med. Hyg. 2017, 96, 1370–1377.
- Nga, T.V.T.; Nghia, H.D.T.; Tu, L.T.P.; Diep, T.S.; Mai, N.T.H.; Chau, T.T.H.; Sinh, D.X.; Phu, N.H.; Chau, N.V.V.; Campbell, J.; et al. Real-time PCR for detection of Streptococcus suis serotype 2 in cerebrospinal fluid of human patients with meningitis. Diagn. Microbiol. Infect. Dis. 2011, 70, 461–467.
- Nakayama, T.; Zhao, J.; Takeuchi, D.; Kerdsin, A.; Chiranairadul, P.; Areeratana, P.; Loetthong, P.; Pienpringam, A.; Akeda, Y.; Oishi, K. Colloidal gold-based immunochromatographic strip test compromising optimised combinations of anti-S. suis capsular polysaccharide polyclonal antibodies for detection of Streptococcus suis. Biosens. Bioelectron. 2014, 60, 175–179.
- Zhang, X.; Wu, Z.; Wang, K. Diagnosis of Streptococcus suis Meningoencephalitis with metagenomic next-generation sequencing of the cerebrospinal fluid: A case report with literature review. BMC Infect. Dis. 2020, 20, 884.
- Thu, I.; Tragoolpua, K.; Intorasoot, S.; Anukool, U.; Khamnoi, P.; Kerdsin, A.; Tharinjaroen, C.S. Direct detection of Streptococcus suis from cerebrospinal fluid, positive hemoculture, and simultaneous differentiation of serotypes 1, 1/2, 2, and 14 within single reaction. Pathogens 2021, 10, 996.




