Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Pamela Acha | -- | 1454 | 2022-11-14 08:04:34 | | | |
| 2 | Camila Xu | -1 word(s) | 1453 | 2022-11-16 09:00:42 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Acha, P.; Mallo, M.; Solé, F. Myelodysplastic Syndromes with Isolated del(5q). Encyclopedia. Available online: https://encyclopedia.pub/entry/34412 (accessed on 07 February 2026).
Acha P, Mallo M, Solé F. Myelodysplastic Syndromes with Isolated del(5q). Encyclopedia. Available at: https://encyclopedia.pub/entry/34412. Accessed February 07, 2026.
Acha, Pamela, Mar Mallo, Francesc Solé. "Myelodysplastic Syndromes with Isolated del(5q)" Encyclopedia, https://encyclopedia.pub/entry/34412 (accessed February 07, 2026).
Acha, P., Mallo, M., & Solé, F. (2022, November 14). Myelodysplastic Syndromes with Isolated del(5q). In Encyclopedia. https://encyclopedia.pub/entry/34412
Acha, Pamela, et al. "Myelodysplastic Syndromes with Isolated del(5q)." Encyclopedia. Web. 14 November, 2022.
Copy Citation
Myelodysplastic syndromes (MDS) are a group of clonal hematological neoplasms characterized by ineffective hematopoiesis in one or more bone marrow cell lineages. Myelodysplastic syndromes with isolated del(5q) constitute the only MDS subtype defined by a cytogenetic alteration.
myelodysplastic syndromes
chromosome 5q deletion
somatic mutations
1. Introduction
Myelodysplastic syndromes (MDS) are a group of clonal hematological neoplasms characterized by ineffective hematopoiesis in one or more bone marrow (BM) cell lineages. Consequently, patients present with variable degrees of cytopenia and dysplasia, which are essential features for establishing a diagnosis according to the World Health Organization (WHO) classification [1][2].
Although nearly half of newly diagnosed patients present a cytogenetic alteration and almost 90% of them harbor at least one somatic mutation, MDS with isolated chromosome 5q deletion (MDS-5q) constitutes the only subtype clearly defined by a cytogenetic alteration [3][4][5][6]. The results of several clinical studies and advances in new technologies have allowed better characterization of this entity. As a consequence, since the first report of the 5q- syndrome, changes and refinements have been made in the definition and characteristics of the patients that pertain to this subtype [7]. Moreover, specific genetic alterations have been found to be associated with prognosis and response to treatments [1][2][8][9].
While preparing this research, the overview of the next WHO classification and the proposal of the International Consensus Classification (ICC) of myeloid neoplasms and acute leukemias were published [2][8]. Consequently, MDS-5q will be renamed and the inclusion criteria will be slightly modified, as will be explained in the subsequent section.
2. From “5q- Syndrome” to MDS-5q
In 1974, Van den Berghe et al. reported a group of three patients with refractory anemia and interstitial deletion of the long arm of chromosome 5. Such cases were later recognized as the “5q- syndrome”. Features of the syndrome included macrocytic anemia, low-normal leukocyte counts, and normal to elevated platelet counts. The BM showed erythroid hypoplasia, hypolobulated megakaryocytes, and a blast count <15% [7]. According to the French–American–British (FAB) cooperative group classification criteria, most of the patients with these characteristics pertain to the group of patients with refractory anemia [10].
It was not until the 2001 edition of the WHO classification that the 5q- syndrome was recognized as a unique and well-defined MDS subtype [11]. In addition to previously described characteristics of this syndrome, in this classification, the blast count threshold was redefined to <5%, and the absence of Auer roads was considered to define 5q- syndrome patients. In 2008, the subtype “MDS with isolated del(5q)” was introduced and the term 5q- syndrome remained restricted to a subset of cases within this category that presented with macrocytic anemia, normal or elevated platelet count, BM erythroid hypoplasia, and a blast count <5% in BM and <1% in peripheral blood (PB) [12]. In the 2017 WHO classification, these cases remained within the MDS with isolated del(5q) subtype. Additionally, the diagnosis of this subtype can be established even if there is one additional cytogenetic abnormality besides the del(5q), unless this abnormality is monosomy 7 or del(7q) [1][13]. This is based on data showing that there is no adverse effect of one chromosomal abnormality in addition to the del(5q) in such patients [14].
As mentioned previously, the overview of the next WHO classification has recently been published [2]. In this new proposal, MDS with isolated del(5q) has been renamed as “myelodysplastic neoplasm with low blast and isolated del(5q)” (abbreviated MDS-5q). The diagnostic criteria have not changed, and it is stated that although an SF3B1 or TP53 mutation (not multi-hit) may potentially alter the biology and/or prognosis of the disease, the presence of such mutations does not per se override the diagnosis of this entity. Regarding the ICC proposal for the classification of MDS, MDS with isolated del(5q) has been retained with no changes from the revised fourth edition of the WHO classification, although the name has been simplified to “MDS with del(5q)”. Similarly to the new WHO proposal, the ICC also specifies that TP53 mutations are admitted in this MDS subtype unless a multi-hit state is detected [8].
It is important to remark that although del(5q) is the most frequent cytogenetic alteration in MDS and is present in roughly 20% of cytogenetic abnormal cases, only about 5% are classified in the MDS-5q category. Features such as higher blast count, alterations in chromosome 7, or a multi-hit TP53 state impact disease prognosis and would reclassify these remaining patients into other, more aggressive, disease subtypes [2][8][15].
The changes in terms and inclusion criteria over time are produced as a consequence of the advances in technology and discoveries, which directly impact knowledge and the management of this disease (Figure 1).
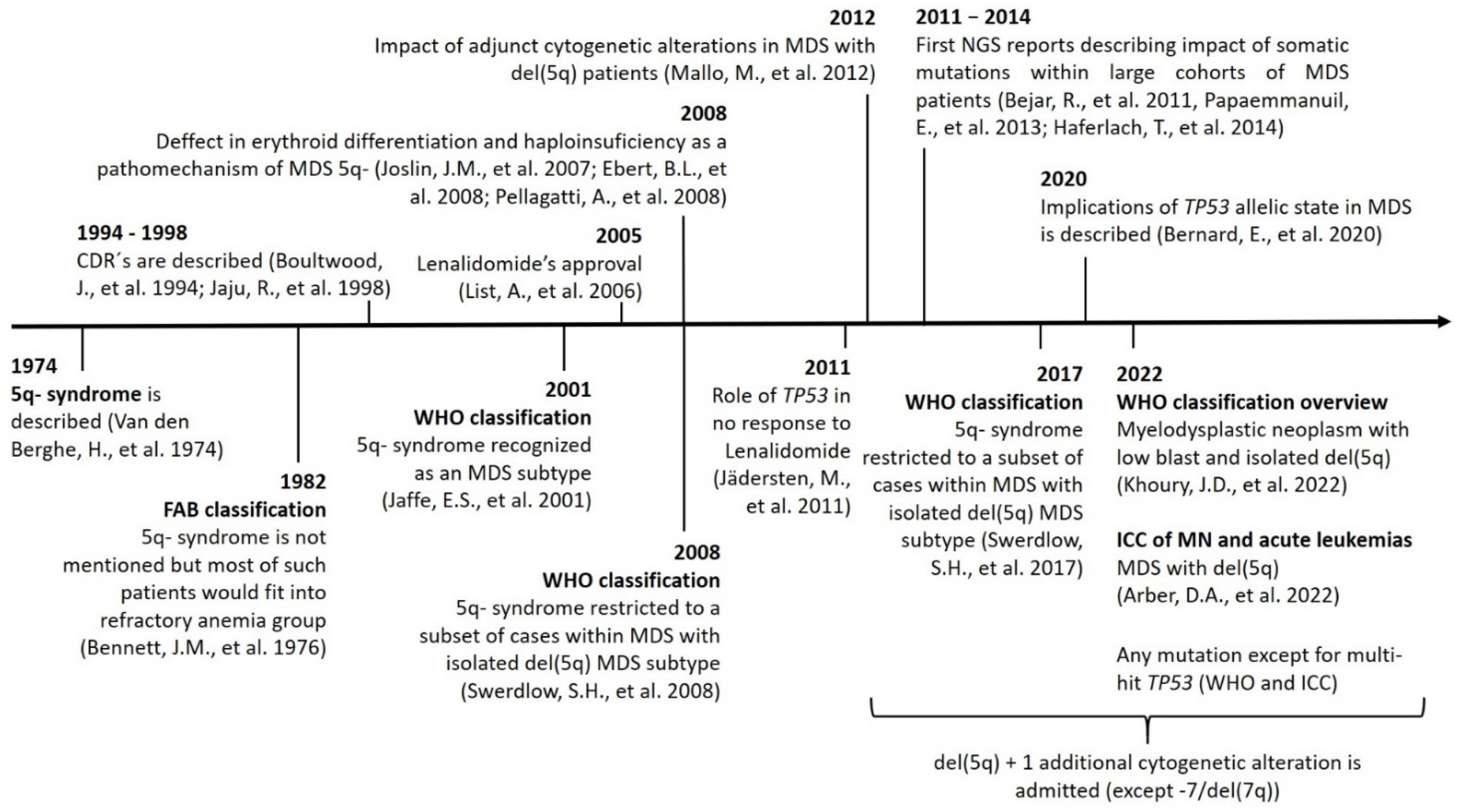
Figure 1. Timeline showing the main discoveries involving MDS-5q and the changes in nomenclature and inclusion criteria. Abbreviations: CDR, commonly deleted region; chr, chromosome; ICC: International Consensus Classification; MN, myeloid neoplasms; NGS, next-generation sequencing.
3. Role of Conventional Cytogenetics in MDS-5q
Conventional cytogenetics (CC) constitutes the gold standard for the genetic diagnosis and prognosis of MDS. However, fluorescence in situ hybridization (FISH) of 5q31 could be useful in cases without evidence of del(5q) by CC. When the presence of MDS-5q is suspected and/or if the cytogenetic study shows no metaphases or an aberrant karyotype with chromosome 5 is involved (no 5q deletion), it is recommended to perform FISH analysis [16][17]. Figure 2 shows the genetic studies available for the diagnosis and characterization of MDS-5q. During follow-up, genetics studies will be adapted to each patient, considering their comorbidities. A new BM aspiration, and the corresponding genetic study, will be performed on suspicion of disease evolution and no response to treatment. In the case of clonal evolution, the approach can be decided according to the general patient status.
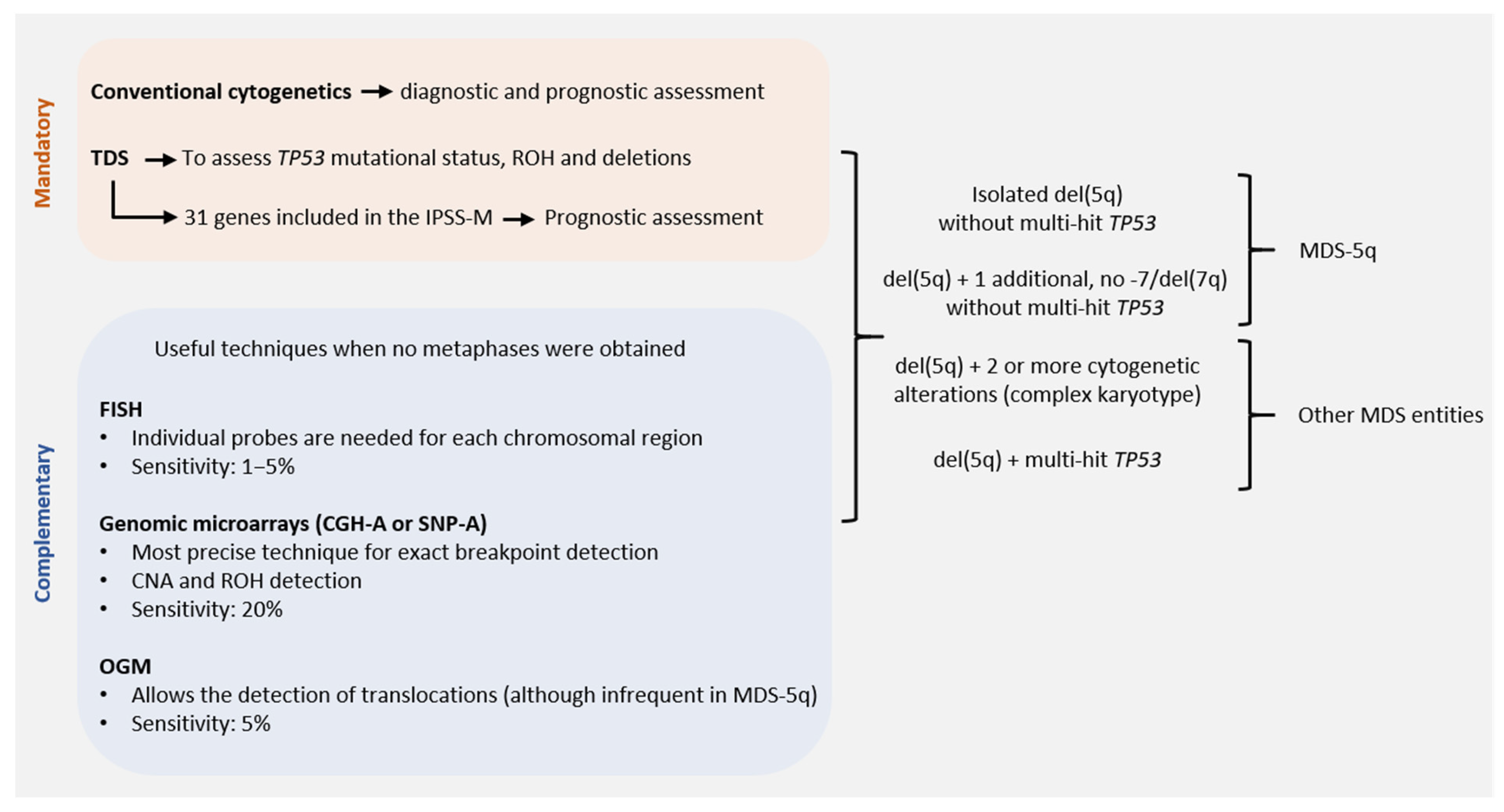
Figure 2. Genetic studies of MDS-5q according to the new diagnostic and prognostic guidelines: techniques available for correct diagnostic and prognostic assessment of MDS-5q according to the criteria of the next World Health Organization (WHO) classification, the proposal of the International Consensus Classification (ICC) and the Molecular International Prognosis Scoring System (IPSS-M). Abbreviations: CGH-A, comparative genomic hybridization; CNA, copy number alteration; FISH, fluorescence in situ hybridization; OGM, optical genome mapping; ROH, region of homozygosity; SNP-A, single nucleotide polymorphism array; TDS, targeted gene sequencing (assuming the use of probes that allow the detection of small CNA and ROH. Otherwise, SNP-A would be recommended to assess CNA and ROH in TP53 for accurate diagnostic and prognostic assessment).
The karyotype is a prognostic variable included in the International Prognostic Scoring System (IPSS) and the revised edition of the IPSS (IPSS-R) [18][19]. Del(5q) alone has always been considered a good prognostic variable and, in the IPSS-R, a concomitant cytogenetic alteration has been included. This change was based on a scoring system proposed by Schanz et al. based on an international data collection of 2902 patients [15]. Deletion 5q is a classical alteration detected in around 15–20% of MDS patients, with half being isolated, around 17% having an additional alteration, and 36% being part of a complex karyotype [3]. The prognostic impact of the accompanying abnormalities in del(5q) is difficult to determine because double abnormalities are highly variable. In 2011, Mallo et al. published an international collaborative study including a large series of del(5q) patients to determine the prognostic impact of adjunct prognostic abnormalities. The multivariate analysis showed that karyotype complexity was one of the main prognostic factors together with platelet count and BM blasts [14]. The good prognosis of del(5q) with one accompanying alteration was included in the MDS with the del(5q) category of the 2017 WHO classification, excluding cases harboring a chromosome 7 alteration [1].
4. Prognostic Impact of Somatic Mutations in MDS-5q
It has been described that one-third of MDS-5q patients present with no somatic alterations, while nearly half of patients (43%) can present with an isolated mutation [20][21]. The pattern of recurrently mutated genes is similar to other MDS subtypes, except for TP53 mutations that were found to be enriched in this subtype of patients [20][22][23]. In the subsequent section, the genes most frequently mutated in MDS-5q are described and Table 1 summarizes their biological and clinical associations and main characteristics and frequencies.
Table 1. Recurrently mutated genes in MDS-5q: clinical and biological correlations.
| Gene | Pathway/Function | Frequency | Clinical and Biological Correlations |
|---|---|---|---|
| SF3B1 | Splicing factor | 19–20% |
|
| DNMT3A | DNA methylation | 18% |
|
| TP53 | Checkpoint/cell cycle | 18% |
|
| TET2 | DNA methylation | 12% |
|
| CSNK1A1 | Proliferation, apoptosis, DNA damage response | 7–10% |
|
| ASXL1 | Chromatin modification | 6% |
|
| JAK2 | Tyrosine kinase | 6% |
|
Abbreviations: AML, acute myeloid leukemia; DTA, DNMT3A, TET2, and ASXL1; OS, overall survival; RS, ring sideroblasts.
References
- Swerdlow, S.H.; Campo, E.; Harris, N.L.; Jaffe, E.S.; Pileri, S.A.; Stein, H.; Thiele, J. (Eds.) WHO Classification of Tumours of Hematopoietic and Lymphoid Tissues, 4th ed.; IARC: Lyon, France, 2017.
- Khoury, J.D.; Solary, E.; Abla, O.; Akkari, Y.; Alaggio, R.; Apperley, J.F.; Bejar, R.; Berti, E.; Busque, L.; Chan, J.K.C.; et al. The 5th Edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia 2022, 36, 1703–1719.
- Haase, D. Cytogenetic Features in Myelodysplastic Syndromes. Ann. Hematol. 2008, 87, 515–526.
- Haase, D.; Germing, U.; Schanz, J.; Pfeilstocker, M.; Nosslinger, T.; Hildebrandt, B.; Kundgen, A.; Lubbert, M.; Kunzmann, R.; Giagounidis, A.A.N.; et al. New Insights into the Prognostic Impact of the Karyotype in MDS and Correlation with Subtypes: Evidence from a Core Dataset of 2124 Patients. Blood 2007, 110, 4385–4395.
- Papaemmanuil, E.; Gerstung, M.; Malcovati, L.; Tauro, S.; Gundem, G.; Van Loo, P.; Yoon, C.J.; Ellis, P.; Wedge, D.C.; Pellagatti, A.; et al. Clinical and Biological Implications of Driver Mutations in Myelodysplastic Syndromes. Blood 2013, 122, 3616–3627.
- Haferlach, T.; Nagata, Y.; Grossmann, V.; Okuno, Y.; Bacher, U.; Nagae, G.; Schnittger, S.; Sanada, M.; Kon, A.; Alpermann, T.; et al. Landscape of Genetic Lesions in 944 Patients with Myelodysplastic Syndromes. Leukemia 2014, 28, 241–247.
- Van Den Berghe, H.; Cassiman, J.-J.; David, G.; Fryns, J.-P.; Michaux, J.-L.; Sokal, G. Distinct Haematological Disorder with Deletion of Long Arm of No. 5 Chromosome. Nature 1974, 251, 437–438.
- Arber, D.A.; Orazi, A.; Hasserjian, R.P.; Borowitz, M.J.; Calvo, K.R.; Kvasnicka, H.-M.; Wang, S.A.; Bagg, A.; Barbui, T.; Branford, S.; et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: Integrating Morphologic, Clinical, and Genomic Data. Blood 2022, 140, 1200–1228.
- Bernard, E.; Tuechler, H.; Greenberg, P.L.; Hasserjian, R.P.; Arango Ossa, J.E.; Nannya, Y.; Devlin, S.M.; Creignou, M.; Pinel, P.; Monnier, L.; et al. Molecular International Prognostic Scoring System for Myelodysplastic Syndromes. NEJM Evid. 2022, 1.
- Bennett, J.M.; Catovsky, D.; Daniel, M.T.; Flandrin, G.; Galton, D.A.; Gralnick, H.R.; Sultan, C. Proposals for the Classification of the Acute Leukaemias. French-American-British (FAB) Co-Operative Group. Br. J. Haematol. 1976, 33, 451–458.
- Jaffe, E.S.; Harris, N.L.; Stein, H.; Vardiman, J.W. (Eds.) World Health Organization Classification of Tumours, Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues; IARC Press: Lyon, France, 2001.
- Swerdlow, S.H.; Campo, E.; Harris, N.L.; Jaffe, E.S.; Pileri, S.A.; Stein, H.; Thiele, J. (Eds.) WHO Classification of Tumours of Hematopoietic and Lymphoid Tissues; IARC: Lyon, France, 2008.
- Arber, D.A.; Orazi, A.; Hasserjian, R.; Thiele, J.; Borowitz, M.J.; Le Beau, M.M.; Bloomfield, C.D.; Cazzola, M.; Vardiman, J.W. The 2016 Revision to the World Health Organization Classification of Myeloid Neoplasms and Acute Leukemia. Blood 2016, 127, 2391–2405.
- Mallo, M.; Cervera, J.; Schanz, J.; Such, E.; García-Manero, G.; Luño, E.; Steidl, C.; Espinet, B.; Vallespí, T.; Germing, U.; et al. Impact of Adjunct Cytogenetic Abnormalities for Prognostic Stratification in Patients with Myelodysplastic Syndrome and Deletion 5q. Leukemia 2011, 25, 110–120.
- Schanz, J.; Tüchler, H.; Solé, F.; Mallo, M.; Luño, E.; Cervera, J.; Granada, I.; Hildebrandt, B.; Slovak, M.L.; Ohyashiki, K.; et al. New Comprehensive Cytogenetic Scoring System for Primary Myelodysplastic Syndromes (MDS) and Oligoblastic Acute Myeloid Leukemia After MDS Derived From an International Database Merge. JCO 2012, 30, 820–829.
- Mallo, M.; Arenillas, L.; Espinet, B.; Salido, M.; Hernandez, J.M.; Lumbreras, E.; del Rey, M.; Arranz, E.; Ramiro, S.; Font, P.; et al. Fluorescence in Situ Hybridization Improves the Detection of 5q31 Deletion in Myelodysplastic Syndromes without Cytogenetic Evidence of 5q-. Haematologica 2008, 93, 1001–1008.
- Mallo, M.; Del Rey, M.; Ibáñez, M.; Calasanz, M.J.; Arenillas, L.; Larráyoz, M.J.; Pedro, C.; Jerez, A.; Maciejewski, J.; Costa, D.; et al. Response to Lenalidomide in Myelodysplastic Syndromes with Del(5q): Influence of Cytogenetics and Mutations. Br. J. Haematol. 2013, 162, 74–86.
- Greenberg, P.; Cox, C.; LeBeau, M.M.; Fenaux, P.; Morel, P.; Sanz, G.; Sanz, M.; Vallespi, T.; Hamblin, T.; Oscier, D.; et al. International Scoring System for Evaluating Prognosis in Myelodysplastic Syndromes. Blood 1997, 89, 2079–2088.
- Greenberg, P.L.; Tuechler, H.; Schanz, J.; Sanz, G.; Garcia-Manero, G.; Sole, F.; Bennett, J.M.; Bowen, D.; Fenaux, P.; Dreyfus, F.; et al. Revised International Prognostic Scoring System for Myelodysplastic Syndromes. Blood 2012, 120, 2454–2465.
- Meggendorfer, M.; Haferlach, C.; Kern, W.; Haferlach, T. Molecular Analysis of Myelodysplastic Syndrome with Isolated Deletion of the Long Arm of Chromosome 5 Reveals a Specific Spectrum of Molecular Mutations with Prognostic Impact: A Study on 123 Patients and 27 Genes. Haematologica 2017, 102, 1502–1510.
- Fernandez-Mercado, M.; Burns, A.; Pellagatti, A.; Giagounidis, A.; Germing, U.; Agirre, X.; Prosper, F.; Aul, C.; Killick, S.; Wainscoat, J.S.; et al. Targeted Re-Sequencing Analysis of 25 Genes Commonly Mutated in Myeloid Disorders in Del(5q) Myelodysplastic Syndromes. Haematologica 2013, 98, 1856–1864.
- Kulasekararaj, A.G.; Smith, A.E.; Mian, S.A.; Mohamedali, A.M.; Krishnamurthy, P.; Lea, N.C.; Gäken, J.; Pennaneach, C.; Ireland, R.; Czepulkowski, B.; et al. TP53 Mutations in Myelodysplastic Syndrome Are Strongly Correlated with Aberrations of Chromosome 5, and Correlate with Adverse Prognosis. Br. J. Haematol. 2013, 160, 660–672.
- Hosono, N.; Makishima, H.; Mahfouz, R.; Przychodzen, B.; Yoshida, K.; Jerez, A.; LaFramboise, T.; Polprasert, C.; Clemente, M.J.; Shiraishi, Y.; et al. Recurrent Genetic Defects on Chromosome 5q in Myeloid Neoplasms. Oncotarget 2017, 8, 6483–6495.
More
Information
Subjects:
Hematology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.0K
Revisions:
2 times
(View History)
Update Date:
16 Nov 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




