
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Peter Frost | -- | 2515 | 2022-10-19 15:53:20 | | | |
| 2 | Lindsay Dong | Meta information modification | 2515 | 2022-10-20 11:07:52 | | |
Video Upload Options
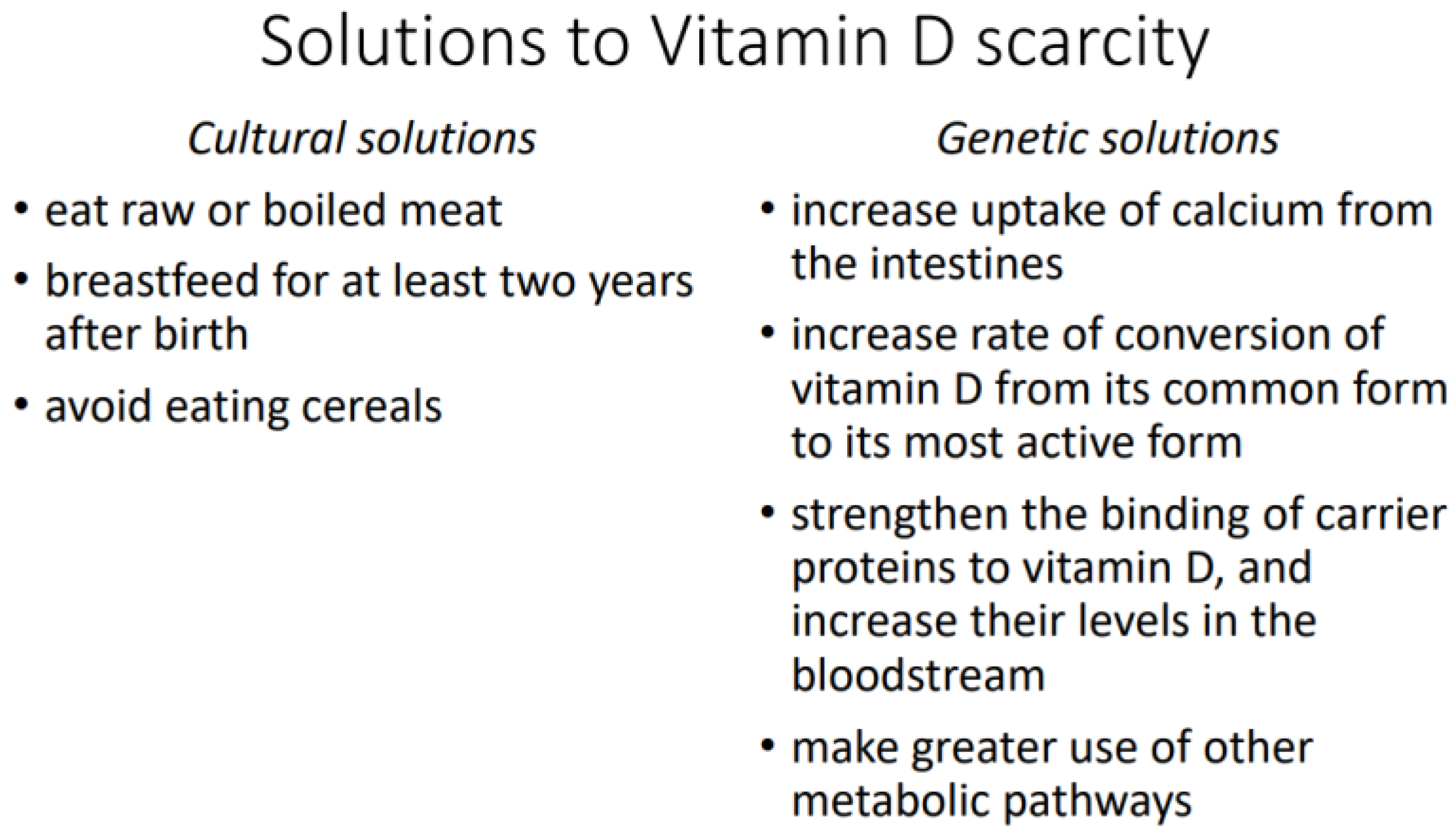
Vitamin D metabolism differs among human populations because the species has adapted to different natural and cultural environments. Two environments are particularly difficult for the production of vitamin D by the skin: the Arctic, where the skin receives little solar UVB over the year; and the Tropics, where the skin is highly melanized and blocks UVB. In both cases, natural selection has favored the survival of those individuals who use vitamin D more efficiently or have some kind of workaround that ensures sufficient uptake of calcium and other essential minerals from food passing through the intestines. Vitamin D scarcity has either cultural or genetic solutions. Cultural solutions include consumption of meat in a raw or boiled state and extended breastfeeding of children. Genetic solutions include higher uptake of calcium from the intestines, higher rate of conversion of vitamin D to its most active form, stronger binding of vitamin D to carrier proteins in the bloodstream, and greater use of alternative metabolic pathways for calcium uptake. Because their bodies use vitamin D more sparingly, indigenous Arctic and Tropical peoples can be misdiagnosed with vitamin D deficiency and wrongly prescribed dietary supplements that may push their vitamin D level over the threshold of toxicity.
1. Introduction
-
The Arctic, where sunlight is weak in summer and absent in winter. The skin thus receives little of the solar UVB that helps produce vitamin D. This is the environment of people indigenous to the North American and Eurasian Arctic, notably the Aleut, the Inuit (Eskimos), the Sámi (Lapps), the Samoyeds, the Khanty-Mansi, the Yakuts, the Yukaghir, the Tungus, the Koryaks, and the Chukchi.
-
The Tropics, where intense sunlight has favored the survival of individuals with highly melanized skin that blocks UVB. This is notably the environment of people indigenous to sub-Saharan Africa, southern India, Australia, Papua New Guinea, and Melanesia.
2. Vitamin D Scarcity in Arctic Peoples
2.1. Cultural Solutions
2.1.1. Consumption of Raw or Boiled Meat
2.1.2. Extended Breastfeeding
2.1.3. No Consumption of Cereals
2.2. Genetic Solutions
2.2.1. Higher Calcium Uptake
A study from northern Canada shows that Inuit children have less need for calcium in their diet and thus less need for vitamin D. Whereas the recommended daily calcium intake is 800 mg for children 4 to 8 years old and 1300 mg for those 9 years old or more, Inuit children on a traditional diet ingest only 20 mg per day. They also excrete excess calcium at an unusually high rate despite their low calcium intake. The explanation seems to be that their vitamin D receptor (bb genotype) is associated with a higher uptake of calcium from food passing through the intestines. The authors concluded: “Dietary calcium intakes based on North American guidelines may therefore result in iatrogenic hypercalciuria and renal damage” [21].
2.2.2. Higher Rate of Conversion
2.2.3. Stronger Binding by Carrier Proteins
3. Vitamin D Scarcity in Tropical Peoples
3.1. Cultural Solutions
3.2. Genetic Solutions
3.2.1. Higher Rate of Conversion
3.2.2. Greater Use of Alternative Metabolic Pathways
References
- Jiang, X.; Kiel, D.P.; Kraft, P. The genetics of vitamin D. Bone 2019, 126, 59–77.
- Jiang, X.; O’Reilly, P.F.; Aschard, H.; Hsu, Y.H.; Richards, J.B.; Dupuis, J.; Ingelsson, E.; Karasik, D.; Pilz, S.; Berry, D.; et al. Genome-wide association study in 79,366 European-ancestry individuals informs the genetic architecture of 25-hydroxyvitamin D levels. Nat. Commun. 2018, 9, 260.
- Harpending, H.; Cochran, G. In our genes. Proc. Natl. Acad. Sci. USA 2002, 99, 10–12.
- Acerbi, A.; Enquist, M.; Ghirlanda, S. Cultural evolution and individual development of openness and conservatism. Proc. Natl. Acad. Sci. USA 2009, 106, 18931–18935.
- Dunnigan, M.G.; Henderson, J.B.; Hole, D.J.; Mawer, E.B.; Berry, J.L. Meat Consumption Reduces the Risk of Nutritional Rickets and Osteomalacia. Br. J. Nutr. 2005, 94, 983–991.
- Mellanby, E. The part played by an ‘accessory factor’ in the production of experimental rickets. Proc. Physiol. Soc. 1918, 52, xi–xii.
- Draper, H.H. The Aboriginal Eskimo Diet in Modern Perspective. Am. Anthropol. 1977, 79, 309–316.
- Geraci, J.R.; Smith, T.G. Vitamin C in the Diet of Inuit Hunters from Holman, Northwest Territories. Arctic 1979, 32, 135–139.
- Sinclair, H. The Diet of Canadian Indians and Eskimos. Proc. Nutr. Soc. 1953, 12, 69–82.
- Heinbecker, P. Studies on the metabolism of Eskimos. J. Biol. Chem. 1928, 80, 461–475.
- Reclus, E. Studies in Comparative Ethnology. In Primitive Folk; Walter Scott: London, UK, 1891.
- Taylor, J.G. Did the First Eskimos Speak Algonquian? Papers of the Ninth Algonquian Conference; Carleton University: Ottawa, ON, Canada, 1978; Volume 9.
- Clifford, W.M. The effect of cooking on the digestibility of meat. Biochem. J. 1930, 24, 1728–1733.
- Searles, E. Inuit identity in the Canadian Arctic. Ethnology 2008, 47, 239–255.
- Lönnerdal, B. Nutritional and Physiologic Significance of Human Milk Proteins. Am. J. Clin. Nutr. 2003, 77, 1537S–1543S.
- Kent, J.C.; Arthur, P.G.; Mitoulas, L.R.; Hartmann, P.E. Why calcium in breastmilk is independent of maternal dietary calcium and vitamin D. Breastfeed. Rev. 2009, 17, 5–11.
- Harrison, D.C.; Mellanby, E. Phytic acid and the rickets-producing action of cereals. Biochem. J. 1939, 33, 1660–1680.
- McCance, R.A.; Widdowson, E.M. Mineral metabolism of healthy adults on white and brown bread dietaries. J. Physiol. 1942, 101, 44–85.
- McCance, R.A.; Widdowson, E.M. Mineral metabolism on dephytinized bread. J. Physiol. 1942, 101, 304–313.
- Wills, M.R.; Phillips, J.B.; Day, R.C.; Bateman, E.C. Phytic acid and nutritional rickets in immigrants. Lancet 1972, 299, 771–773.
- Sellers, E.A.C.; Sharma, A.; Rodd, C. Adaptation of Inuit children to a low-calcium diet. Can. Med. Assoc. J. 2003, 168, 1141–1143.
- Rejnmark, L.; Jørgensen, M.E.; Pedersen, M.B.; Hansen, J.C.; Heickendorff, L.; Lauridsen, A.L.; Mulvad, G.; Siggaard, C.; Skjoldborg, H.; Sørensen, T.B.; et al. Vitamin D insufficiency in Greenlanders on a Westernized fare: Ethnic differences in calcitropic hormones between Greenlanders and Danes. Calcif. Tissue Int. 2004, 74, 255–263.
- Malyarchuk, B.A. Polymorphism of GC gene, encoding vitamin D binding protein, in aboriginal populations of Siberia. Ecol. Genet. 2020, 18, 243–250.
- Signorello, L.B.; Williams, S.M.; Zheng, W.; Smith, J.R.; Long, J.; Cai, Q.; Hargreaves, M.K.; Hollis, B.W.; Blot, W.J. Blood vitamin D levels in relation to genetic estimation of African ancestry. Cancer Epidem. Biomar. 2010, 19, 2325–2331.
- Harris, S.S. Vitamin D and African Americans. J. Nutr. 2006, 136, 1126–1129.
- Harinarayan, C.V.; Ramalakshmi, T.; Prasad, U.V.; Sudhakar, D.; Srinivasarao, P.V.L.N.; Sarma, K.V.S.; Kumar, E.G.T. High prevalence of low dietary calcium, high phytate consumption, and vitamin D deficiency in healthy south Indians. Am. J. Clin. Nutr. 2007, 85, 1062–1067.
- Goswami, R.; Kochupillai, N.; Gupta, N.; Goswami, D.; Singh, N.; Dudha, A. Presence of 25(OH) D deficiency in a rural North Indian village despite abundant sunshine. J. Assoc. Physicians India 2008, 56, 755–757.
- Hamilton, B.; Grantham, J.; Racinais, S.; Chalabi, H. Vitamin D deficiency is endemic in Middle Eastern sportsmen. Public Health Nutr. 2020, 13, 1528–1534.
- Sedrani, S.H. Low 25-hydroxyvitamin D and normal serum calcium concentrations in Saudi Arabia: Riyadh region. Ann. Nutr. Metab. 1984, 28, 181–185.
- Jones, W.O. The Food and Agricultural Economies of Tropical Africa: A Summary View; Food Research Institute Studies; Stanford University, Food Research Institute: Stanford, CA, USA, 1961; Volume 2, pp. 1–18.
- Léder, I. Sorghum and Millets. In Cultivated Plants, Primarily as Food Sources; UNESCO: Oxford, UK, 2004; Volume 1, pp. 66–84.
- Parsons, R.T. Religion in an African Society; E.J. Brill: Leiden, The Netherlands, 1964.
- Altman, I.; Chemers, M.M. Culture and Environment; Brooks/Cole: Monterey, CA, USA, 1984.
- Robins, A.H. The evolution of light skin color: Role of vitamin D disputed. Am. J. Phys. Anthropol. 2009, 139, 447–450.
- Barrett-Connor, E.; Siris, E.S.; Wehren, L.E.; Miller, P.D.; Abbott, T.A.; Berger, M.L.; Santora, A.C.; Sherwood, L.M. Osteoporosis and Fracture Risk in Women of Different Ethnic Groups. J. Bone Miner. Res. 2005, 20, 185–194.
- Hannan, M.T.; Litman, H.J.; Araujo, A.B.; McLennan, C.E.; McLean, R.R.; McKinlay, J.B.; Chen, T.C.; Holick, M.F. Serum 25-hydroxyvitamin D and bone mineral density in a racially and ethnically diverse group of men. J. Clin. Endocrinol. Metab. 2008, 93, 40–46.
- Freedman, B.I.; Wagenknecht, L.E.; Hairston, K.G.; Bowden, D.W.; Carr, J.J.; Hightower, R.C.; Gordon, E.J.; Xu, J.; Langefeld, C.D.; Divers, J. Vitamin D, adiposity, and calcified atherosclerotic plaque in African-Americans. J. Clin. Endocr. Metab. 2010, 95, 1076–1083.
- Aloia, J.F.; Talwar, S.A.; Pollack, S.; Yeh, J. A randomized controlled trial of vitamin D3 supplementation in African American women. Arch. Intern. Med. 2005, 165, 1618–1623.
- Matsuoka, L.Y.; Wortsman, J.; Haddad, J.G.; Kolm, P.; Hollis, B.W. Racial pigmentation and the cutaneous synthesis of vitamin D. Arch. Dermatol. 1991, 127, 536–538.
- Matsuoka, L.Y.; Wortsman, J.; Chen, T.C.; Holick, M.F. Compensation for the interracial variance in the cutaneous synthesis of vitamin D. J. Lab. Clin. Med. 1995, 126, 452–457.
- Lips, P. Interaction between Vitamin D and calcium. Scand. J. Clin. Lab. Investig. 2012, 72, 60–64.
- Lee, D.B.; Hardwick, L.L.; Hu, M.S.; Jamgotchian, N. Vitamin D-independent regulation of calcium and phosphate absorption. Miner. Electrolyte Metab. 1990, 16, 167–173.
- Zhang, J.; Zhang, Z.; Yu, A. Discussion on the mechanism of the calcium absorption in the human body. Chin. Sci. Bull. 2001, 46, 1403–1408.




