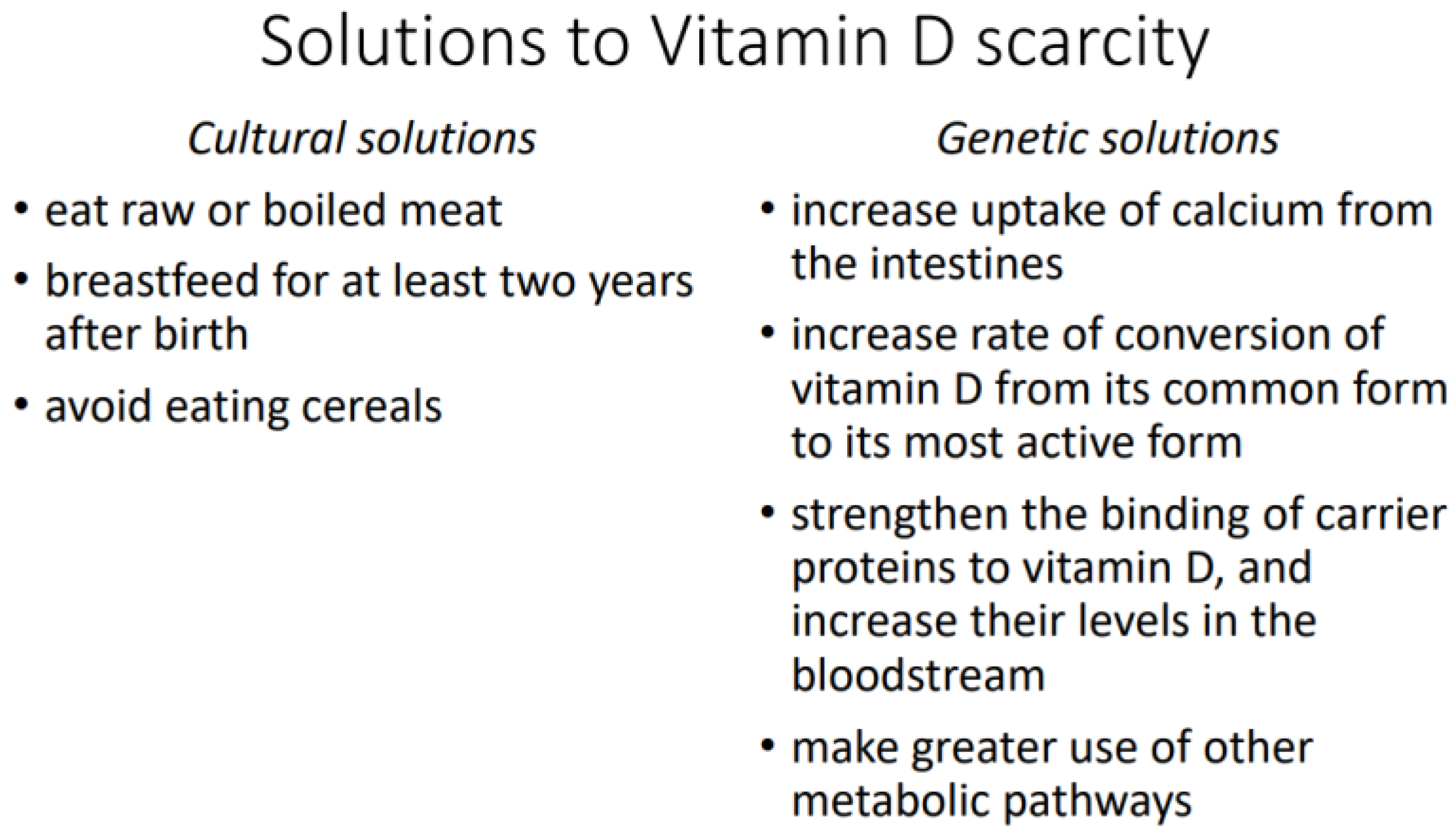
Vitamin D metabolism differs among human populations because ourthe species has adapted to different natural and cultural environments. Two environments are particularly difficult for the production of vitamin D by the skin: the Arctic, where the skin receives little solar UVB over the year; and the Tropics, where the skin is highly melanized and blocks UVB. In both cases, natural selection has favored the survival of those individuals who use vitamin D more efficiently or have some kind of workaround that ensures sufficient uptake of calcium and other essential minerals from food passing through the intestines. Vitamin D scarcity has either cultural or genetic solutions. Cultural solutions include consumption of meat in a raw or boiled state and extended breastfeeding of children. Genetic solutions include higher uptake of calcium from the intestines, higher rate of conversion of vitamin D to its most active form, stronger binding of vitamin D to carrier proteins in the bloodstream, and greater use of alternative metabolic pathways for calcium uptake. Because their bodies use vitamin D more sparingly, indigenous Arctic and Tropical peoples can be misdiagnosed with vitamin D deficiency and wrongly prescribed dietary supplements that may push their vitamin D level over the threshold of toxicity.
- Arctic
- culture
- genetics
- Tropics
- UVB
- vitamin D
1. Introduction
-
The Arctic, where sunlight is weak in summer and absent in winter. The skin thus receives little of the solar UVB that helps produce vitamin D. This is the environment of people indigenous to the North American and Eurasian Arctic, notably the Aleut, the Inuit (Eskimos), the Sámi (Lapps), the Samoyeds, the Khanty-Mansi, the Yakuts, the Yukaghir, the Tungus, the Koryaks, and the Chukchi.
-
The Tropics, where intense sunlight has favored the survival of individuals with highly melanized skin that blocks UVB. This is notably the environment of people indigenous to sub-Saharan Africa, southern India, Australia, Papua New Guinea, and Melanesia.
2. Vitamin D Scarcity in Arctic Peoples
2.1. Cultural Solutions
Although Arctic peoples cannot obtain sufficient vitamin D from their skin or their diet, it is only in recent times that they have begun to suffer from rickets and other adverse effects of vitamin D deficiency. Those adverse effects were prevented by certain aspects of their traditional diet: consumption of meat in a raw or boiled state; extended breastfeeding of children for at least two years after birth; and no consumption of cereals.2.1.1. Consumption of Raw or Boiled Meat
Meat consumption reduces the risk of rickets and osteomalacia independently of the meat’s vitamin D content, with no further risk reduction above 60 g of meat per day [6][5]. The anti-rickets component of meat remains unknown, although meat protein has been ruled out [7][6]. Arctic peoples traditionally ate large quantities of meat. The Inuit, for instance, subsisted largely on raw or boiled meat from fish, marine mammals, and land mammals [8,9,10,11][7][8][9][10]. Although Arctic peoples had to eat meat, there being few other food sources, they were not forced to eat it in a raw or boiled state. Yet such consumption was the norm: “The preparation of Eskimo food is simple. Most meat is eaten partly boiled and the remainder raw” [11][10] (p. 462). That norm was unknown to, and scorned by, indigenous peoples who lived farther south, such as the Amerindians of temperate North America. “If the Indians are to be believed, their hatred [of the Inuit] springs from another source. They do not know how to forgive the Esquimaux the crime of eating raw fish” [12][11] (p. 9). The name “Eskimo” is alleged to have come from an Algonkian term meaning “eaters of raw meat” and has been replaced by “Inuit” because of its negative connotation [10][9] (p. 69), [13][12] (p. 101). Although cooking makes meat easier to digest and tastier, it appears to destroy certain nutritional cofactors that may be difficult to obtain from other food sources, particularly in the Arctic [15][13]. Arctic peoples may not understand the why or the how, but they do understand the health benefits of uncooked meat: “Inuit emphasize how eating raw seal meat or hunting at the floe edge produces healthy bodies and intelligent minds … One Inuit man, who had spent much of his youth at a hunting camp and later moved to live in Iqaluit, said that his town diet of white foods made him weak, lazy, and ill equipped to deal with the strength and stamina needed to live off the land” [16][14] (p. 247).2.1.2. Extended Breastfeeding
A mother can reduce her child’s need for vitamin D by breastfeeding for a longer period after birth. Breast milk is rich in a phosphoprotein called β-casein, which helps keep calcium soluble during digestion and contributes to its bioavailability [18][15]. A similar role is played in milk by phosphate, citrate, and other caseins [19][16]. Consequently, breastfeeding reduces a child’s need for vitamin D.2.1.3. No Consumption of Cereals
Finally, the need for vitamin D can be reduced by not eating cereals. Consumption of cereals increases the risk of rickets independently of the body’s supply of vitamin D [7,25,26,27,28][6][17][18][19][20]. The actual risk factor seems to be phytic acid, which is found in the hulls of nuts, seeds, and grains and is most often ingested from store-bought bread. By binding to minerals to form insoluble precipitates, it reduces the body’s supply of usable essential minerals, like calcium, and increases the body’s need for vitamin D. That effect has been shown by animal and human studies. When puppies are fed oatmeal, they develop rickets in proportion to its phytic acid content [25][17]. When humans are fed a 92% flour diet, they absorb less calcium, magnesium, phosphorus, and potassium than they do on a 69% flour diet. When the diet is 92% flour, the loss of usable calcium cannot be counteracted by adding vitamin D [26][18]. Calcium, magnesium, and phosphorus are absorbed in inverse proportion to the phytic acid content of the flour diet [27][19].2.2. Genetic Solutions
2.2.1. Higher Calcium Uptake
A study from northern Canada shows that Inuit children have less need for calcium in their diet and thus less need for vitamin D. Whereas the recommended daily calcium intake is 800 mg for children 4 to 8 years old and 1300 mg for those 9 years old or more, Inuit children on a traditional diet ingest only 20 mg per day. They also excrete excess calcium at an unusually high rate despite their low calcium intake. The explanation seems to be that their vitamin D receptor (bb genotype) is associated with a higher uptake of calcium from food passing through the intestines. The authors concluded: “Dietary calcium intakes based on North American guidelines may therefore result in iatrogenic hypercalciuria and renal damage” [29][21].
2.2.2. Higher Rate of Conversion
A study of adult Greenland Inuit has shown that they evolved at least two genetic solutions to the problem of vitamin D scarcity. In addition to having a different calcium metabolism, as indicated by a lower set-point for the calcium-regulated release of parathyroid hormone, they also have a higher rate of conversion of vitamin D from its common form to its most active form. Serum levels of 1,25(OH)2D are thus higher in Greenland Inuit than in Danes. “Due to a low endogenous 25OHD production in Greenlanders … evolution may have selected individuals with a relatively high 25-hydroxyvitamin D1α-hydroxylase activity” [33][22] (p. 261).2.2.3. Stronger Binding by Carrier Proteins
Among the indigenous peoples of Arctic and sub-Arctic Eurasia, vitamin D tends to be bound more strongly by the proteins that transport it via the bloodstream. There are also higher serum levels of the same carrier proteins. The main one is produced by the gene GC, which exists in two variants: the T variant, which is much less frequent in the northeast and center of Siberia than in the south and west; and the G variant, which is conversely much more frequent in the northeast and center than in the south and west. The G variant is associated with increased transportation of vitamin D via the bloodstream; it has thus been favored by natural selection in populations that are farther north and less able to produce vitamin D. This difference in geographic distribution cannot be explained by different levels of European admixture, since East Asians have very little European admixture and yet resemble southern and western Siberians in having the same high frequency of the T variant [34][23]. Natural selection seems to have likewise favored the G variant in Arctic and sub-Arctic North America, the population frequency being 71% among the Dene peoples of northern Canada.3. Vitamin D Scarcity in Tropical Peoples
It may seem strange that less vitamin D is produced in the skin of people from the Tropics, where sunlight is so intense. The same intense sunlight, however, has also selected for highly melanized skin that blocks UVB and thus limits production of vitamin D. That blocking effect has been shown in Americans with varying degrees of African ancestry. With each 10% increase in African ancestry, the serum 25(OH)D level decreases by 2.5 to 2.75 nmol/L [37][24]. Levels are lower than 50 nmol/L during the winter in 53 to 76% of African Americans who live in the southern states [38][25]. A similar situation prevails in other dark-skinned peoples, even those who have remained in the Tropics and are regularly exposed to intense solar UV. In south India, at 13.4° N, a study found that 44% of the men and 70% of the women had 25(OH)D levels lower than 50 nmol/L. They were “agricultural workers starting their day at 0800 and working outdoors until 1700 with their face, chest, back, legs, arms, and forearms exposed to sunlight” [39][26]. That finding is corroborated by another Indian study, which found levels higher than or equal to 50 nmol/L in only 31.5% of the participants, who had nonetheless been exposed to the sun for 5 h every day [40][27]. Two studies from the Middle East have reported levels lower than 50 nmol/L in 91% of healthy athletes [41][28] and lower than 25 nmol/L in 35%, 45%, 53%, and 50%, of Saudi, Jordanian, Egyptian, and other male university students in Riyadh [42][29].3.1. Cultural Solutions
Dark-skinned peoples are thus faced with a problem of vitamin D scarcity. Unlike Arctic peoples, they do not solve it by means of cultural practices, at least not at the present time. Meat provides a small proportion of the caloric intake in sub-Saharan Africa and is normally cooked, and cereals like sorghum and millet have long been consumed despite their high levels of phytic acid [44,45][30][31]. On the other hand, extended breastfeeding may have been formerly common [46][32] (p. 15), [47][33] (pp. 6–7). Cultural solutions are unlikely for both theoretical and evidentiary reasons. First, humans and their hominin forbears have lived much longer in the Tropics than in the Arctic—millions of years longer. Natural selection has thus had considerable time to replace the initial cultural solutions with genetic ones. Second, cultural solutions, if still needed, would surely include a prohibition against cooking of meat, a widespread dietary rule among Arctic peoples.3.2. Genetic Solutions
A genetic adaptation is often a hardwiring of something initially imposed by circumstance. In this case, dark-skinned peoples originally had low levels of vitamin D because their skin is less easily penetrated by UVB. Today, there is a second constraint, a homeostatic mechanism that resists any effort to increase the body’s supply of vitamin D. This has been shown in African Americans with varying degrees of African ancestry. Both sunlight and diet are 46% less effective in raising the 25(OH)D level of individuals with high African ancestry [37][24]. The tendency toward homeostasis suggests that a low 25(OH)D level is sufficient for African Americans. Indeed, few of them show signs of vitamin D deficiency. They have “a lower prevalence of osteoporosis, a lower incidence of fractures and a higher bone mineral density than white Americans, who generally exhibit a much more favorable vitamin D status” [48][34]. Among women 65 years of age, the risk of a hip fracture by age 80 is only 4% for African Americans versus 11% for European Americans [32,38][25][35]. A difference in metabolism is further shown by a finding that bone mineral density correlates with serum 25(OH)D in European Americans but not in African Americans or Hispanic Americans [52,53,54][36][37][38]. The non-correlation in Hispanic Americans may seem puzzling, although the research participants could have been Puerto Ricans and Dominicans with substantial African ancestry.3.2.1. Higher Rate of Conversion
Although a single UVB exposure causes the skin to produce less vitamin D3 in African Americans than in European Americans, the difference decreases after liver hydroxylation to 25(OH)D and is gone after kidney hydroxylation to 1,25(OH)2D. The most active form of vitamin D is thus produced at a constant rate regardless of how dark the skin is [55,56][39][40].3.2.2. Greater Use of Alternative Metabolic Pathways
Some calcium is absorbed into the body through pathways that function independently of vitamin D. Those pathways include passive diffusion of calcium ions [57,58][41][42] and transportation of calcium in the form of calcium chelate [59][43]. There is also suggestive evidence that bile salts, lactose, and prolactin assist calcium uptake independently of vitamin D [58][42]. Natural selection may have expanded such alternative pathways in populations that lack vitamin D.References
- Jiang, X.; Kiel, D.P.; Kraft, P. The genetics of vitamin D. Bone 2019, 126, 59–77.
- Jiang, X.; O’Reilly, P.F.; Aschard, H.; Hsu, Y.H.; Richards, J.B.; Dupuis, J.; Ingelsson, E.; Karasik, D.; Pilz, S.; Berry, D.; et al. Genome-wide association study in 79,366 European-ancestry individuals informs the genetic architecture of 25-hydroxyvitamin D levels. Nat. Commun. 2018, 9, 260.
- Harpending, H.; Cochran, G. In our genes. Proc. Natl. Acad. Sci. USA 2002, 99, 10–12.
- Acerbi, A.; Enquist, M.; Ghirlanda, S. Cultural evolution and individual development of openness and conservatism. Proc. Natl. Acad. Sci. USA 2009, 106, 18931–18935.
- Dunnigan, M.G.; Henderson, J.B.; Hole, D.J.; Mawer, E.B.; Berry, J.L. Meat Consumption Reduces the Risk of Nutritional Rickets and Osteomalacia. Br. J. Nutr. 2005, 94, 983–991.
- Mellanby, E. The part played by an ‘accessory factor’ in the production of experimental rickets. Proc. Physiol. Soc. 1918, 52, xi–xii.
- Draper, H.H. The Aboriginal Eskimo Diet in Modern Perspective. Am. Anthropol. 1977, 79, 309–316.
- Geraci, J.R.; Smith, T.G. Vitamin C in the Diet of Inuit Hunters from Holman, Northwest Territories. Arctic 1979, 32, 135–139.
- Sinclair, H. The Diet of Canadian Indians and Eskimos. Proc. Nutr. Soc. 1953, 12, 69–82.
- Heinbecker, P. Studies on the metabolism of Eskimos. J. Biol. Chem. 1928, 80, 461–475.
- Reclus, E. Studies in Comparative Ethnology. In Primitive Folk; Walter Scott: London, UK, 1891.
- Taylor, J.G. Did the First Eskimos Speak Algonquian? Papers of the Ninth Algonquian Conference; Carleton University: Ottawa, ON, Canada, 1978; Volume 9.
- Clifford, W.M. The effect of cooking on the digestibility of meat. Biochem. J. 1930, 24, 1728–1733.
- Searles, E. Inuit identity in the Canadian Arctic. Ethnology 2008, 47, 239–255.
- Lönnerdal, B. Nutritional and Physiologic Significance of Human Milk Proteins. Am. J. Clin. Nutr. 2003, 77, 1537S–1543S.
- Kent, J.C.; Arthur, P.G.; Mitoulas, L.R.; Hartmann, P.E. Why calcium in breastmilk is independent of maternal dietary calcium and vitamin D. Breastfeed. Rev. 2009, 17, 5–11.
- Harrison, D.C.; Mellanby, E. Phytic acid and the rickets-producing action of cereals. Biochem. J. 1939, 33, 1660–1680.
- McCance, R.A.; Widdowson, E.M. Mineral metabolism of healthy adults on white and brown bread dietaries. J. Physiol. 1942, 101, 44–85.
- McCance, R.A.; Widdowson, E.M. Mineral metabolism on dephytinized bread. J. Physiol. 1942, 101, 304–313.
- Wills, M.R.; Phillips, J.B.; Day, R.C.; Bateman, E.C. Phytic acid and nutritional rickets in immigrants. Lancet 1972, 299, 771–773.
- Sellers, E.A.C.; Sharma, A.; Rodd, C. Adaptation of Inuit children to a low-calcium diet. Can. Med. Assoc. J. 2003, 168, 1141–1143.
- Rejnmark, L.; Jørgensen, M.E.; Pedersen, M.B.; Hansen, J.C.; Heickendorff, L.; Lauridsen, A.L.; Mulvad, G.; Siggaard, C.; Skjoldborg, H.; Sørensen, T.B.; et al. Vitamin D insufficiency in Greenlanders on a Westernized fare: Ethnic differences in calcitropic hormones between Greenlanders and Danes. Calcif. Tissue Int. 2004, 74, 255–263.
- Malyarchuk, B.A. Polymorphism of GC gene, encoding vitamin D binding protein, in aboriginal populations of Siberia. Ecol. Genet. 2020, 18, 243–250.
- Signorello, L.B.; Williams, S.M.; Zheng, W.; Smith, J.R.; Long, J.; Cai, Q.; Hargreaves, M.K.; Hollis, B.W.; Blot, W.J. Blood vitamin D levels in relation to genetic estimation of African ancestry. Cancer Epidem. Biomar. 2010, 19, 2325–2331.
- Harris, S.S. Vitamin D and African Americans. J. Nutr. 2006, 136, 1126–1129.
- Harinarayan, C.V.; Ramalakshmi, T.; Prasad, U.V.; Sudhakar, D.; Srinivasarao, P.V.L.N.; Sarma, K.V.S.; Kumar, E.G.T. High prevalence of low dietary calcium, high phytate consumption, and vitamin D deficiency in healthy south Indians. Am. J. Clin. Nutr. 2007, 85, 1062–1067.
- Goswami, R.; Kochupillai, N.; Gupta, N.; Goswami, D.; Singh, N.; Dudha, A. Presence of 25(OH) D deficiency in a rural North Indian village despite abundant sunshine. J. Assoc. Physicians India 2008, 56, 755–757.
- Hamilton, B.; Grantham, J.; Racinais, S.; Chalabi, H. Vitamin D deficiency is endemic in Middle Eastern sportsmen. Public Health Nutr. 2020, 13, 1528–1534.
- Sedrani, S.H. Low 25-hydroxyvitamin D and normal serum calcium concentrations in Saudi Arabia: Riyadh region. Ann. Nutr. Metab. 1984, 28, 181–185.
- Jones, W.O. The Food and Agricultural Economies of Tropical Africa: A Summary View; Food Research Institute Studies; Stanford University, Food Research Institute: Stanford, CA, USA, 1961; Volume 2, pp. 1–18.
- Léder, I. Sorghum and Millets. In Cultivated Plants, Primarily as Food Sources; UNESCO: Oxford, UK, 2004; Volume 1, pp. 66–84.
- Parsons, R.T. Religion in an African Society; E.J. Brill: Leiden, The Netherlands, 1964.
- Altman, I.; Chemers, M.M. Culture and Environment; Brooks/Cole: Monterey, CA, USA, 1984.
- Robins, A.H. The evolution of light skin color: Role of vitamin D disputed. Am. J. Phys. Anthropol. 2009, 139, 447–450.
- Barrett-Connor, E.; Siris, E.S.; Wehren, L.E.; Miller, P.D.; Abbott, T.A.; Berger, M.L.; Santora, A.C.; Sherwood, L.M. Osteoporosis and Fracture Risk in Women of Different Ethnic Groups. J. Bone Miner. Res. 2005, 20, 185–194.
- Hannan, M.T.; Litman, H.J.; Araujo, A.B.; McLennan, C.E.; McLean, R.R.; McKinlay, J.B.; Chen, T.C.; Holick, M.F. Serum 25-hydroxyvitamin D and bone mineral density in a racially and ethnically diverse group of men. J. Clin. Endocrinol. Metab. 2008, 93, 40–46.
- Freedman, B.I.; Wagenknecht, L.E.; Hairston, K.G.; Bowden, D.W.; Carr, J.J.; Hightower, R.C.; Gordon, E.J.; Xu, J.; Langefeld, C.D.; Divers, J. Vitamin D, adiposity, and calcified atherosclerotic plaque in African-Americans. J. Clin. Endocr. Metab. 2010, 95, 1076–1083.
- Aloia, J.F.; Talwar, S.A.; Pollack, S.; Yeh, J. A randomized controlled trial of vitamin D3 supplementation in African American women. Arch. Intern. Med. 2005, 165, 1618–1623.
- Matsuoka, L.Y.; Wortsman, J.; Haddad, J.G.; Kolm, P.; Hollis, B.W. Racial pigmentation and the cutaneous synthesis of vitamin D. Arch. Dermatol. 1991, 127, 536–538.
- Matsuoka, L.Y.; Wortsman, J.; Chen, T.C.; Holick, M.F. Compensation for the interracial variance in the cutaneous synthesis of vitamin D. J. Lab. Clin. Med. 1995, 126, 452–457.
- Lips, P. Interaction between Vitamin D and calcium. Scand. J. Clin. Lab. Investig. 2012, 72, 60–64.
- Lee, D.B.; Hardwick, L.L.; Hu, M.S.; Jamgotchian, N. Vitamin D-independent regulation of calcium and phosphate absorption. Miner. Electrolyte Metab. 1990, 16, 167–173.
- Zhang, J.; Zhang, Z.; Yu, A. Discussion on the mechanism of the calcium absorption in the human body. Chin. Sci. Bull. 2001, 46, 1403–1408.
