Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Lavinia Cosmina Ardelean | -- | 1073 | 2022-09-15 17:30:27 | | | |
| 2 | Dean Liu | Meta information modification | 1073 | 2022-09-16 03:01:57 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Tigmeanu, C.V.; Ardelean, L.C.; Rusu, L.; Negrutiu, M. 3D Printing Technologies in Dentistry. Encyclopedia. Available online: https://encyclopedia.pub/entry/27223 (accessed on 07 February 2026).
Tigmeanu CV, Ardelean LC, Rusu L, Negrutiu M. 3D Printing Technologies in Dentistry. Encyclopedia. Available at: https://encyclopedia.pub/entry/27223. Accessed February 07, 2026.
Tigmeanu, Codruta Victoria, Lavinia Cosmina Ardelean, Laura-Cristina Rusu, Meda-Lavinia Negrutiu. "3D Printing Technologies in Dentistry" Encyclopedia, https://encyclopedia.pub/entry/27223 (accessed February 07, 2026).
Tigmeanu, C.V., Ardelean, L.C., Rusu, L., & Negrutiu, M. (2022, September 15). 3D Printing Technologies in Dentistry. In Encyclopedia. https://encyclopedia.pub/entry/27223
Tigmeanu, Codruta Victoria, et al. "3D Printing Technologies in Dentistry." Encyclopedia. Web. 15 September, 2022.
Copy Citation
3D-printing application in dentistry not only enables the manufacture of patient-specific devices and tissue constructs, but also allows mass customization, as well as digital workflow, with predictable lower cost and rapid turnaround times.
3D printing
additive manufacturing
polymers
bioinks
bioprinting
1. Introduction
Polymer-based materials play an important role in dentistry, with a wide variety of applications, based on their surface characteristics, mechanical and biological properties, easy processing, and affordable cost [1].
Some of the most commonly used polymers in dentistry are polymethyl methacrylate (PMMA), polyurethane (PU), polyethylene (PE), polycarbonate (PC), polyetheretherketone (PEEK), polyethylene glycol (PEG), polydimethylsiloxane (PDMS), polylactic acid (PLA), poly(e-caprolactone) (PCL), acrylonitrile butadiene styrene (ABS), polypropylene (PP) [2].
Their mechanical properties are related to the bulk material characteristics, but the interaction with oral tissues is highly dependent on their surface, justifying the use of polymer coatings to increase their biocompatibility [3][4]. The specific applications of polymers cover almost every field of dentistry, including direct restorative procedures, prosthodontics, orthodontics, and even implantology, as synthetic PEEK has been recently proposed as an implant material [5][6]. Customized polymeric facial prostheses, with detailed morphology, can be easily obtained by 3D printing. Polymers have also been used to manufacture scaffolds, with role in regeneration of bone structures, dentin- and pulp-like tissues, membranes for guided tissue regeneration, and as drug delivery systems in treating numerous oral and periodontal pathologies [7].
Composite resins for direct restorations are probably the most used polymers in dentistry, in association with dental adhesives, which, besides bonding the restorations to the dental surface, play an important role in the adhesion of brackets, retainers, and bands in orthodontics. Moreover, fiber-reinforced composites are used for post-orthodontic tooth retention and for splinting mobile teeth. Various types of polymers are widely used in prosthodontics, as well, including denture manufacturing, and various other types of prosthodontic appliances, as adhesives for metal or ceramic, veneering materials etc., [1][2].
The continuous development of their applications and manufacturing technologies in prosthodontics, including injection and CAD/CAM milling, has finally resulted in a most versatile technique, namely 3D printing.
3D printing, also known as additive manufacturing or rapid prototyping, was first used in 1980s [8][9]. Due to the development of the printing techniques and devices, it currently allows a wide range of applications, medicine included. 3D printing has recently become in the forefront of research in biomedical fields, as it enables the manufacture of patient specific devices and tissue constructs [10].
This manufacturing technology is currently used in a large variety of medical and biomedical applications including anatomical or experimental models, medical devices, prostheses and implants, scaffolds, tissues and organs, anatomical structures, and drug delivery systems [11][12][13]. Vat photo-polymerization, droplet-based, extrusion-based, and powder-based 3D-printing techniques have already proven their importance for modern dentistry, covering a wide range of indications (Figure 1) [14].

Figure 1. Indications of 3D-printed polymers in dentistry.
Different types of materials, including polymers, metals, and ceramics, are used for 3D printing in dentistry. However, because of their high versatility associated with the wide variety of available materials, 3D printing in dentistry predominantly targets the production of polymeric constructs [15].
3D bioprinting uses so-called “bioinks” to fabricate complex organ structures and functional tissues that can support live cells and other biological factors [16]. By means of 3D bioprinting, tailored tissue-engineered constructs, with defined structures and properties can be speedily manufactured, including cells, DNA, growth factors, and other bioactive components as integral parts of the building process [16].
2. 3D Printing Technologies in Dentistry
The 3D-printing technologies used for dental purposes show noticeable differences in the technology, as well as in resolution, accuracy, and repeatability [17] (Table 1).
Table 1. Main characteristics of commonly used 3D-printing technologies for polymers in dentistry.
| Characteristic | SLA | DLP | MJT | FDM |
|---|---|---|---|---|
| Type | vat photo-polymerization | vat photo-polymerization | material jetting | material extrusion |
| Resolution | high | high | high | low |
| Accuracy | medium | high | high | medium |
| Speed | medium | high | high | medium |
| Object size | scalable | scalable | scalable | scalable |
| Cost | medium | medium | high | low |
Currently, the most widespread additive technology in dentistry is vat photo-polymerization, including the stereolithography (SLA) and digital light processing (DLP) methods. The principle is based on liquid photopolymer in a vat being selectively cured by light-activated polymerization [18]. In SLA, the polymerization is performed by a directed UV-laser beam, used to sequentially cure liquid photopolymer resin layers, while in DLP, a whole layer of photosensitive liquid resin is simultaneously polymerized by a UV-light mask. SLA is characterized by high resolution and good accuracy, being suitable for fine details and functional prototyping, while DLP is characterized by high printing resolution, fast production rate, and affordable costs [19].
Regardless of the method, the printed parts need subsequent cleaning with isopropanol, to remove the excessive monomer, and post-polymerization with UV-light (Figure 2) [10][18]. Both SLA and DLP are versatile techniques as they can be used with a wide variety of polymeric materials [20].
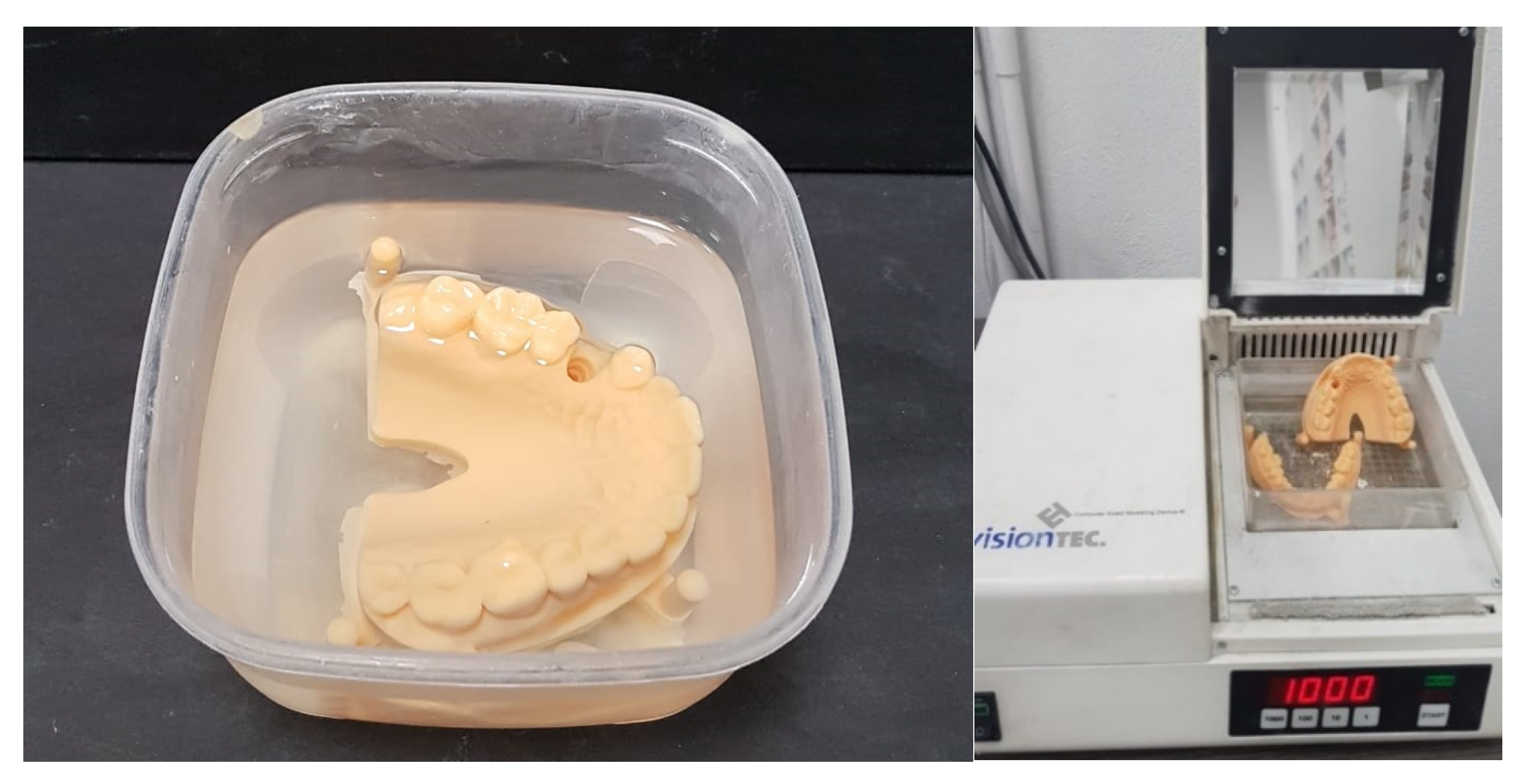
Figure 2. 3D vat photo-polymerized models, cleaned with isopropanol, and post-polymerized.
Continuous direct light processing (CDLP), based on the continuous liquid interface production (CLIP) technology, which was patented in 2015, involves a continuous high speed build process, and high object precision, suitable for denture bases and bite splints [21]. The additional use of a membrane allows oxygen permeation, and inhibits radical polymerization [20].
Material jetting (MJT) or photo-polymer jetting involves applying tiny drops of material directly to the build platform via the print head, followed by photo-polymerization in an intermediate exposure step, and requires no post-polymerization. The object is built on a layer by layer basis, extremely fast and highly accurate. A special feature is the multi-material 3D-printing multicolor mode [21].
Unlike vat photo-polymerization and MJT, which use photo-polymeric materials, fusion deposition modelling (FDM) is an extrusion-based printing technique in which melted thermoplastic materials are being used to manufacture the desired object, using layer by layer deposition. Initially used only for polymeric structures, it has been subsequently modified to process ceramics and composites [22]. Despite the low cost, because of the longer printing times and lower resolutions, FDM is currently considered of lesser relevance for dental purposes [21]. A wide range of polymeric materials, in a filament form, have been considered: ABS, PC, thermoplastics, polyamide (PA), polystyrene (PS), polyetherimide (PEI) and polyoxymethylene (POM) as well as polyethylene (PE) [23].
Selective laser sintering (SLS), which uses a high-power pulsed laser to fuse polymeric, metallic or ceramic powder particles, by creating surface layers, is currently mostly used in dentistry for printing metallic structures [10].
Binder jetting (BJ) utilizes selectively deposited liquid bonding agents to fuse powdered material [20].
The applications of most commonly used additive manufacturing technologies in dentistry are presented in Figure 3.
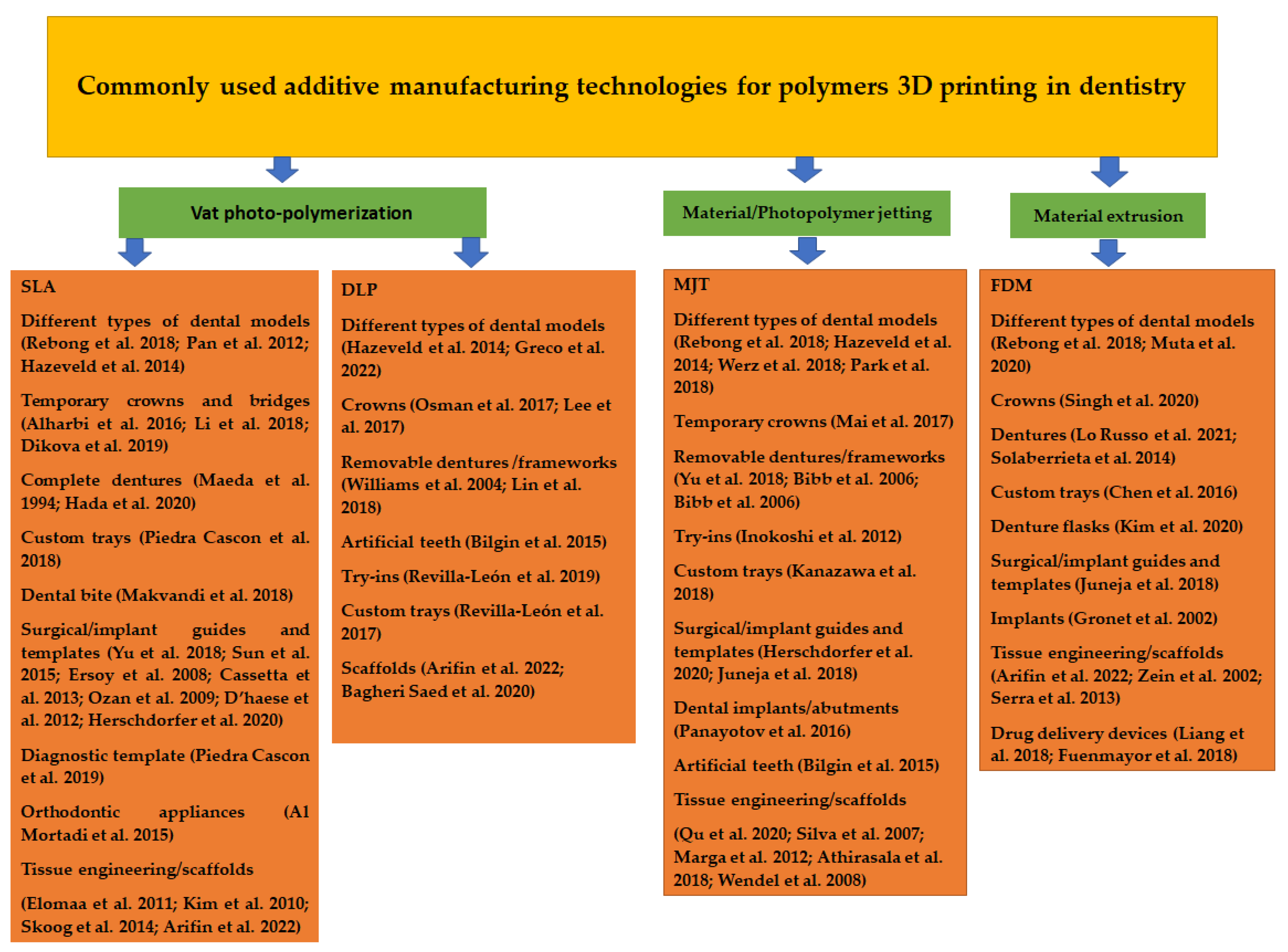
Figure 3. Most used additive manufacturing technologies and their applications for polymers 3D printing in dentistry [24][25][26][27][28][29][30][31][32][33][34][35][36][37][38][39][40][41][42][43][44][45][46][47][48][49][50][51][52][53][54][55][56][57][58][59][60][61][62][63][64][65][66][67][68][69][70][71][72][73][74][75][76][77][78][79][80].
References
- Thomé, T.; Erhardt, M.C.G.; Leme, A.A.; Al Bakri, I.; Bedran-Russo, A.K.; Bertassoni, L.E. Emerging Polymers in Dentistry. In Advanced Polymers in Medicine; Puoci, F., Ed.; Springer: Cham, Switzerland, 2015; pp. 265–296.
- Rokaya, D.; Srimaneepong, V.; Sapkota, J.; Qin, J.; Siraleartmukul, K.; Siriwongrungson, V. Polymeric materials and films in dentistry: An overview. J. Adv. Res. 2018, 14, 25–34.
- Smith, J.R.; Lamprou, D.A. Polymer coatings for biomedical applications: A review. Trans. Ins. Met. 2014, 92, 9–19.
- Nathanael, A.J.; Oh, T.H. Biopolymer Coatings for Biomedical Applications. Polymers 2020, 12, 3061.
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J. Prosthodont. Res. 2016, 60, 12–19.
- Al-Rabab’ah, M.; Hamadneh, W.; Alsalem, I.; Khraisat, A.; Karaky, A.A. Use of high performance polymers as dental implant abutments and frameworks: A case series report. J. Prosthodont. 2019, 28, 365–372.
- Abduo, J.; Lyons, K.; Bennamoun, M. Trends in Computer-Aided Manufacturing in Prosthodontics: A Review of the Available Streams. Int. J. Dent. 2014, 2014, 783948.
- Clark Ligon, S.; Liska, R.; Stampfl, J.; Gurr, M.; Mulhaupt, R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290.
- Okolie, O.; Stachurek, I.; Kandasubramanian, B.; Njuguna, J. 3D Printing for Hip Implant Applications: A Review. Polymers 2020, 12, 2682.
- Pillai, S.; Upadhyay, A.; Khayambashi, P.; Farooq, I.; Sabri, H.; Tarar, M.; Lee, K.T.; Harb, I.; Zhou, S.; Wang, Y.; et al. Dental 3D-Printing: Transferring Art from the Laboratories to the Clinics. Polymers 2021, 13, 157.
- Ujfalusi, Z.; Pentek, A.; Told, R.; Schiffer, A.; Nyitrai, M.; Maroti, P. Detailed Thermal Characterization of Acrylonitrile Butadiene Styrene and Polylactic Acid Based Carbon Composites Used in Additive Manufacturing. Polymers 2020, 12, 2960.
- Heo, H.; Jin, Y.; Yang, D.; Wier, C.; Minard, A.; Dahotre, N.B.; Neogi, A. Manufacturing and Characterization of Hybrid Bulk Voxelated Biomaterials Printed by Digital Anatomy 3D Printing. Polymers 2021, 13, 123.
- Kessler, A.; Hickel, R.; Reymus, M. 3D printing in dentistry—State of the art. Oper. Dent. 2020, 45, 30–40.
- Torabi, K.; Farjood, E.; Hamedani, E. Rapid prototyping technologies and their applications in prosthodontics, a review of literature. J. Dent. 2015, 16, 1–9.
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64.
- Theus, A.S.; Ning, L.; Hwang, B.; Gil, C.; Chen, S.; Wombwell, A.; Mehta, R.; Serpooshan, V. Bioprintability: Physiomechanical and Biological Requirements of Materials for 3D Bioprinting Processes. Polymers 2020, 12, 2262.
- Jockusch, J.; Özcan, M. Additive manufacturing of dental polymers: An overview on processes, materials and applications. Dent. Mater. J. 2020, 39, 345–354.
- Nold, J.; Wesemann, C.; Rieg, L.; Binder, L.; Witkowski, S.; Spies, B.C.; Kohal, R.J. Does Printing Orientation Matter? In-Vitro Fracture Strength of Temporary Fixed Dental Prostheses after a 1-Year Simulation in the Artificial Mouth. Materials 2021, 14, 259.
- Groth, C.; Kravitz, N.D.; Jones, P.E.; Graham, J.W.; Redmond, W.R. Three-dimensional printing technology. J. Clin. Orthod. 2014, 48, 475–485.
- Etemad-Shahidi, Y.; Qallandar, O.B.; Evenden, J.; Alifui-Segbaya, F.; Ahmed, K.E. Accuracy of 3-Dimensionally Printed Full-Arch Dental Models: A Systematic Review. J. Clin. Med. 2020, 9, 3357.
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010.
- Prasad, A.; Kandasubramanian, B. Fused Deposition Processing Polycaprolactone of Composites for Biomedical Applications. Polym. Plast. Technol. Mater. 2019, 58, 1365–1398.
- Rocha, C.R.; Perez, A.R.T.; Roberson, D.A.; Shemelya, C.M.; MacDonald, E.; Wicker, R.B. Novel ABS-based binary and ternary polymer blends for material extrusion 3D printing. J. Mater. Res. 2014, 29, 1859–1866.
- Rebong, R.E.; Stewart, K.T.; Utreja, A.; Ghoneima, A.A. Accuracy of three-dimensional dental resin models created by fused deposition modeling, stereolithography, and Polyjet prototype technologies: A comparative study. Angle Orthod. 2018, 88, 363–369.
- Pan, Y.; Zhou, C.; Chen, Y. A Fast Mask Projection Stereolithography Process for Fabricating Digital Models in Minutes. J. Manuf. Sci. Eng. 2012, 134, 051011.
- Hazeveld, A.; Huddleston Slater, J.J.R.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115.
- Greco, G.B.; Popi, D.; Di Stefano, D.A. Accuracy of 3-dimensional printing of dental casts: A proposal for quality standardization. J. Prosthet. Dent. 2022, 127, 899–910.
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767.
- Li, X.; Xie, B.; Jin, J.; Chai, Y.; Chen, Y. 3D Printing Temporary Crown and Bridge by Temperature Controlled Mask Image Projection Stereolithography. Procedia Manuf. 2018, 26, 1023–1033.
- Dikova, T. Production of high-quality temporary crowns and bridges by stereolithography. Scr. Sci. Med. Dent. 2019, 5, 33–38.
- Maeda, Y.; Minoura, M.; Tsutsumi, S.; Okada, M.; Nokubi, T. A CAD/CAM system for removable denture. Part I: Fabrication of complete dentures. Int. J. Prosthodont. 1994, 7, 17–21.
- Hada, T.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Soeda, Y.; Katheng, A.; Otake, R.; Minakuchi, S. Effect of printing direction on the accuracy of 3D-printed dentures using stereolithography technology. Materials 2020, 13, 3405.
- Piedra Cascon, W.; Revilla-León, M. Digital workflow for the design and additively manufacture of a splinted framework and custom tray for the impression of multiple implants: A dental technique. J. Prosthet. Dent. 2018, 120, 805–811.
- Makvandi, P.; Esposito Corcione, C.; Paladini, F.; Gallo, A.L.; Montagna, F.; Jamaledin, R.; Pollini, M.; Maffezzoli, A. Antimicrobial modified hydroxyapatite composite dental bite by stereolithography. Polym. Adv. Technol. 2018, 29, 364–371.
- Yu, J.H.; Wang, Y.T.; Lin, C.L. Customized surgical template fabrication under biomechanical consideration by integrating CBCT image, CAD system and finite element analysis. Dent. Mater. J. 2018, 37, 6–14.
- Sun, Y.; Luebbers, H.; Agbaje, J.O.; Schepers, S.; Politis, C.; Van Slycke, S.; Vrielinck, L. Accuracy of dental implant placement using CBCT-derived mucosa-supported stereolithographic template. Clin. Implant Dent. Relat. Res. 2015, 17, 862–870.
- Ersoy, A.E.; Turkyilmaz, I.; Ozan, O.; McGlumphy, E.A. Reliability of implant placement with stereolithographic surgical guides generated from computed tomography: Clinical data from 94 implants. J. Periodontol. 2008, 79, 1339–1345.
- Cassetta, M.; Di Carlo, S.; Pranno, N.; Sorrentino, V.; Di Giorgio, G.; Pompa, G. The use of stereolithographic surgical templates in oral implantology. Ann. Ital. Chir. 2013, 84, 589–593.
- Ozan, O.; Turkyilmaz, I.; Ersoy, A.E.; McGlumphy, E.A.; Rosenstiel, S.F. Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J. Oral Maxillofac. Surg. 2009, 67, 394–401.
- D’haese, J.; Van De Velde, T.; Komiyama, A.; Hultin, M.; De Bruyn, H. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: A review of the literature. Clin. Implant Dent. Relat. Res. 2012, 14, 321–335.
- Herschdorfer, L.; Negreiros, W.; Gallucci, G.; Hamilton, A. Comparison of the accuracy of implants placed with CAD-CAM surgical templates manufactured with various 3D printers: An in vitro study. J. Prosthet. Dent. 2020, 125, 905–910.
- Piedra Cascon, W.; Parra Nunez, A.; Charlen Diez, I.; Revilla León, M. Laboratory workflow to obtain long-term injected resin composite interim restorations from an additive manufactured esthetic diagnostic template. J. Esthet. Restor. Dent. 2019, 31, 13–19.
- Al Mortadi, N.; Jones, Q.; Eggbeer, D.; Lewis, J.; Williams, R.J. Fabrication of a resin appliance with alloy components using digital technology without an analog impression. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 862–867.
- Elomaa, L.; Teixeira, S.; Hakala, R.; Korhonen, H.; Grijpma, D.W.; Seppala, J.V. Preparation of poly(epsilon-caprolactone)-based tissue engineering scaffolds by stereolithography. Acta Biomater. 2011, 7, 3850–3856.
- Kim, K.; Yeatts, A.; Dean, D.; Fisher, J.P. Stereolithographic bone scaffold design parameters: Osteogenic differentiation and signal expression. Tissue Eng. Part B Rev. 2010, 16, 523–539.
- Skoog, S.A.; Goering, P.L.; Narayan, R.J. Stereolithography in tissue engineering. J. Mater. Sci. Mater. Med. 2014, 25, 845–856.
- Arifin, N.; Sudin, I.; Ngadiman, N.H.A.; Ishak, M.S.A. A Comprehensive Review of Biopolymer Fabrication in Additive Manufacturing Processing for 3D-Tissue-Engineering Scaffolds. Polymers 2022, 14, 2119.
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build angle: Does it influence the accuracy of 3D-printed dental restorations using digital light-processing technology? Int. J. Prosthodont. 2017, 30, 182–188.
- Lee, H.; Son, K.B.D.; Lee, D.-H.; Kim, S.-Y.; Lee, K.-B. Comparison of wear of interim crowns in accordance with the build angle of digital light processing 3-dimensional printing: A pilot in vivo study. Res. Sq. 2022.
- Williams, R.J.; Bibb, R.; Rafik, T. A technique for fabricating patterns for removable partial denture frameworks using digitized casts and electronic surveying. J. Prosthet. Dent. 2004, 91, 85–88.
- Lin, W.-S.; Harris, B.T.; Pellerito, J.; Morton, D. Fabrication of an interim complete removable dental prosthesis with an in-office digital light processing three-dimensional printer: A proof-of-concept technique. J. Prosthet. Dent. 2018, 120, 331–334.
- Bilgin, M.S.; Erdem, A.; Aglarci, O.S.; Dilber, E. Fabricating complete dentures with CAD/CAM and RP technologies. J. Prosthodont. 2015, 24, 576–579.
- Revilla-León, M.; Besné-Torre, A.; Sánchez-Rubio, J.L.; Fábrega, J.J.; Özcan, M. Digital tools and 3D printing technologies integrated into the workflow of restorative treatment: A clinical report. J. Prosthet. Dent. 2019, 121, 3–8.
- Revilla-León, M.; Sánchez-Rubio, J.L.; Oteo-Calatayud, J.; Özcan, M. Impression technique for a complete-arch prosthesis with multiple implants using additive manufacturing technologies. J. Prosthet. Dent. 2017, 117, 714–720.
- Bagheri Saed, A.; Behravesh, A.H.; Hasannia, S.; Alavinasab Ardebili, S.A.; Akhoundi, B.; Pourghayoumi, M. Functionalized poly l-lactic acid synthesis and optimization of process parameters for 3D printing of porous scaffolds via digital light processing (DLP) method. J. Manuf. Process. 2020, 56, 550–561.
- Werz, S.M.; Zeichner, S.J.; Berg, B.I.; Zeilhofer, H.F.; Thieringer, F. 3D printed surgical simulation models as educational tool by maxillofacial surgeons. Eur. J. Dent. Educ. 2018, 22, e500–e505.
- Park, M.E.; Shin, S.Y. Three-dimensional comparative study on the accuracy and reproducibility of dental casts fabricated by 3D printers. J. Prosthet. Dent. 2018, 119, 861.e1–861.e7.
- Mai, H.-N.; Lee, K.-B.; Lee, D.-H. Fit of interim crowns fabricated using photopolymer-jetting 3D printing. J. Prosthet. Dent. 2017, 118, 208–215.
- Bibb, R.; Eggbeer, D.; Williams, R. Rapid manufacture of removable partial denture frameworks. Rapid Prototyp. J. 2006, 12, 95–99.
- Bibb, R.J.; Eggbeer, D.; Williams, R.; Woodward, A. Trial fitting of a removable partial denture framework made using computer-aided design and rapid prototyping techniques. Proc. Inst. Mech. Eng. H. 2006, 220, 793–797.
- Inokoshi, M.; Kanazawa, M.; Minakuchi, S. Evaluation of a complete denture trial method applying rapid prototyping. Dent. Mater. J. 2012, 31, 40–46.
- Kanazawa, M.; Iwaki, M.; Arakida, T.; Minakuchi, S. Digital impression and jaw relation record for the fabrication of CAD/CAM custom tray. J. Prosthodont. Res. 2018, 62, 509–513.
- Juneja, M.; Thakur, N.; Kumar, D.; Gupta, A.; Bajwa, B.; Jindal, P. Accuracy in dental surgical guide fabrication using different 3-D printing techniques. Addit. Manuf. 2018, 22, 243–255.
- Panayotov, I.V.; Orti, V.; Cuisinier, F.; Yachouh, J. Polyetheretherketone (PEEK) for medical applications. J. Mater. Sci. Mater. Med. 2016, 27, 118.
- Qu, H. Additive manufacturing for bone tissue engineering scaffolds. Mater. Today Commun. 2020, 24, 101024.
- Silva, D.S.; Wallace, D.B.; Cooley, P.W.; Radulescu, D.; Hayes, D.J. An inkjet printing station for neuroregenerative tissue engineering. In Proceedings of the 2007 IEEE Dallas Engineering in Medicine and Biology Workshop, Dallas, TX, USA, 11–12 November 2007.
- Marga, F.; Jakab, K.; Khatiwala, C.; Shepherd, B.; Dorfman, S.; Hubbard, B.; Colbert, S.; Forgacs, G. Toward engineering functional organ modules by additive manufacturing. Biofabrication 2012, 4, 022001.
- Athirasala, A.; Tahayeri, A.; Thrivikraman, G.; Franca, C.M.; Monteiro, N.; Tran, V.; Ferracane, J.; Bertassoni, L.E. A dentin-derived hydrogel bioink for 3D bioprinting of cell laden scaffolds for regenerative dentistry. Biofabrication 2018, 10, 024101.
- Wendel, B.; Rietzel, D.; Kühnlein, F.; Feulner, R.; Hülder, G.; Schmachtenberg, E. Additive processing of polymers. Macromol. Mater. Eng. 2008, 293, 799–809.
- Muta, S.; Ikeda, M.; Nikaido, T.; Sayed, M.; Sadr, A.; Suzuki, T.; Tagami, J. Chairside fabrication of provisional crowns on FDM 3D-printed PVA model. J. Prosthodont. Res. 2020, 64, 401–407.
- Singh, R.; Dureja, J.S. Dental Crowns by FDM Assisted Vapour Smoothing and Silicon Moulding. In 3D Printing in Biomedical Engineering. Materials Horizons: From Nature to Nanomaterials; Singh, S., Prakash, C., Singh, R., Eds.; Springer: Singapore, 2020; pp. 231–250.
- Lo Russo, L.; Lo Muzio, E.; Troiano, G.; Salamini, A.; Zhurakivska, K.; Guida, L. Accuracy of trial complete dentures fabricated by using fused deposition modeling 3-dimensional printing: An in vitro study. J. Prosthet. Dent. 2021, S0022–3913, 416–419.
- Solaberrieta, E.; Minguez, R.; Barrenetxea, L.; Sierra, E.; Etxaniz, O. Computer-aided dental prostheses construction using reverse engineering. Comput. Methods Biomech. Biomed. Eng. 2014, 17, 1335–1346.
- Chen, H.; Yang, X.; Chen, L.; Wang, Y.; Sun, Y. Application of FDM three-dimensional printing technology in the digital manufacture of custom edentulous mandible trays. Sci. Rep. 2016, 6, 19207.
- Kim, H.; Lee, D.; Young Lee, S.; Yang, H.; Park, S.W.; Lim, H.P.; Yun, K.D.; Park, C. Denture flask fabrication using fused deposition modeling three-dimensional printing. J. Prosthodont. Res. 2020, 64, 231–234.
- Gronet, P.M.; Waskewicz, G.A.; Richardson, C. Preformed acrylic cranial implants using fused deposition modeling: A clinical report. J. Prosthet. Dent. 2002, 90, 429–433.
- Zein, I.; Hutmacher, D.W.; Tan, K.C.; Teoh, S.H. Fused deposition modeling of novel scaffold architectures for tissue engineering applications. Biomaterials 2002, 23, 1169–1185.
- Serra, T.; Mateos-Timoneda, M.A.; Planell, J.A.; Navarro, M. 3D printed PLA-based scaffolds: A versatile tool in regenerative medicine. Organogenesis 2013, 9, 239–244.
- Liang, K.; Carmone, S.; Brambilla, D.; Leroux, J.C. 3D printing of a wearable personalized oral delivery device: A first-in-human study. Sci. Adv. 2018, 4, eaat2544.
- Fuenmayor, E.; Forde, M.; Healy, A.V.; Devine, D.M.; Lyons, J.G.; McConville, C.; Major, I. Material considerations for fused-filament fabrication of solid dosage forms. Pharmaceutics 2018, 10, 44.
More
Information
Subjects:
Polymer Science
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.5K
Revisions:
2 times
(View History)
Update Date:
16 Sep 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




