Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Polymer Science
3D-printing application in dentistry not only enables the manufacture of patient-specific devices and tissue constructs, but also allows mass customization, as well as digital workflow, with predictable lower cost and rapid turnaround times.
- 3D printing
- additive manufacturing
- polymers
- bioinks
- bioprinting
1. Introduction
Polymer-based materials play an important role in dentistry, with a wide variety of applications, based on their surface characteristics, mechanical and biological properties, easy processing, and affordable cost [1].
Some of the most commonly used polymers in dentistry are polymethyl methacrylate (PMMA), polyurethane (PU), polyethylene (PE), polycarbonate (PC), polyetheretherketone (PEEK), polyethylene glycol (PEG), polydimethylsiloxane (PDMS), polylactic acid (PLA), poly(e-caprolactone) (PCL), acrylonitrile butadiene styrene (ABS), polypropylene (PP) [2].
Their mechanical properties are related to the bulk material characteristics, but the interaction with oral tissues is highly dependent on their surface, justifying the use of polymer coatings to increase their biocompatibility [3,4]. The specific applications of polymers cover almost every field of dentistry, including direct restorative procedures, prosthodontics, orthodontics, and even implantology, as synthetic PEEK has been recently proposed as an implant material [5,6]. Customized polymeric facial prostheses, with detailed morphology, can be easily obtained by 3D printing. Polymers have also been used to manufacture scaffolds, with role in regeneration of bone structures, dentin- and pulp-like tissues, membranes for guided tissue regeneration, and as drug delivery systems in treating numerous oral and periodontal pathologies [7].
Composite resins for direct restorations are probably the most used polymers in dentistry, in association with dental adhesives, which, besides bonding the restorations to the dental surface, play an important role in the adhesion of brackets, retainers, and bands in orthodontics. Moreover, fiber-reinforced composites are used for post-orthodontic tooth retention and for splinting mobile teeth. Various types of polymers are widely used in prosthodontics, as well, including denture manufacturing, and various other types of prosthodontic appliances, as adhesives for metal or ceramic, veneering materials etc., [1,2].
The continuous development of their applications and manufacturing technologies in prosthodontics, including injection and CAD/CAM milling, has finally resulted in a most versatile technique, namely 3D printing.
3D printing, also known as additive manufacturing or rapid prototyping, was first used in 1980s [8,9]. Due to the development of the printing techniques and devices, it currently allows a wide range of applications, medicine included. 3D printing has recently become in the forefront of research in biomedical fields, as it enables the manufacture of patient specific devices and tissue constructs [10].
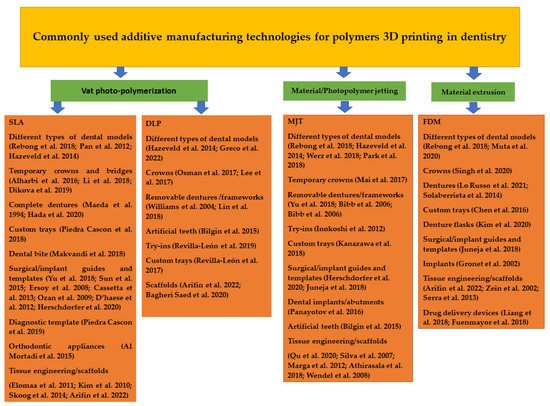
This manufacturing technology is currently used in a large variety of medical and biomedical applications including anatomical or experimental models, medical devices, prostheses and implants, scaffolds, tissues and organs, anatomical structures, and drug delivery systems [11,12,13]. Vat photo-polymerization, droplet-based, extrusion-based, and powder-based 3D-printing techniques have already proven their importance for modern dentistry, covering a wide range of indications (Figure 1) [14].
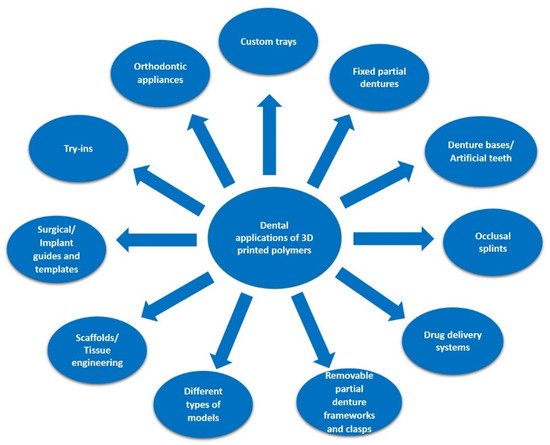
Figure 1. Indications of 3D-printed polymers in dentistry.
Different types of materials, including polymers, metals, and ceramics, are used for 3D printing in dentistry. However, because of their high versatility associated with the wide variety of available materials, 3D printing in dentistry predominantly targets the production of polymeric constructs [15].
3D bioprinting uses so-called “bioinks” to fabricate complex organ structures and functional tissues that can support live cells and other biological factors [16]. By means of 3D bioprinting, tailored tissue-engineered constructs, with defined structures and properties can be speedily manufactured, including cells, DNA, growth factors, and other bioactive components as integral parts of the building process [16].
2. 3D Printing Technologies in Dentistry
The 3D-printing technologies used for dental purposes show noticeable differences in the technology, as well as in resolution, accuracy, and repeatability [17] (Table 1).
Table 1. Main characteristics of commonly used 3D-printing technologies for polymers in dentistry.
| Characteristic | SLA | DLP | MJT | FDM |
|---|---|---|---|---|
| Type | vat photo-polymerization | vat photo-polymerization | material jetting | material extrusion |
| Resolution | high | high | high | low |
| Accuracy | medium | high | high | medium |
| Speed | medium | high | high | medium |
| Object size | scalable | scalable | scalable | scalable |
| Cost | medium | medium | high | low |
Currently, the most widespread additive technology in dentistry is vat photo-polymerization, including the stereolithography (SLA) and digital light processing (DLP) methods. The principle is based on liquid photopolymer in a vat being selectively cured by light-activated polymerization [18]. In SLA, the polymerization is performed by a directed UV-laser beam, used to sequentially cure liquid photopolymer resin layers, while in DLP, a whole layer of photosensitive liquid resin is simultaneously polymerized by a UV-light mask. SLA is characterized by high resolution and good accuracy, being suitable for fine details and functional prototyping, while DLP is characterized by high printing resolution, fast production rate, and affordable costs [19].
Regardless of the method, the printed parts need subsequent cleaning with isopropanol, to remove the excessive monomer, and post-polymerization with UV-light (Figure 2) [10,18]. Both SLA and DLP are versatile techniques as they can be used with a wide variety of polymeric materials [20].
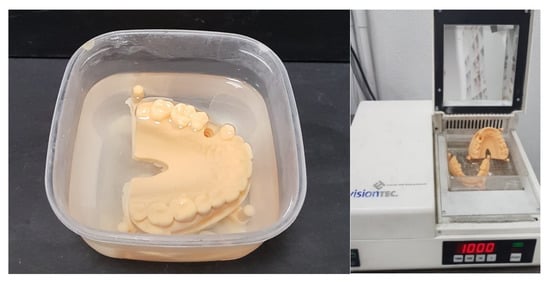
Figure 2. 3D vat photo-polymerized models, cleaned with isopropanol, and post-polymerized.
Continuous direct light processing (CDLP), based on the continuous liquid interface production (CLIP) technology, which was patented in 2015, involves a continuous high speed build process, and high object precision, suitable for denture bases and bite splints [21]. The additional use of a membrane allows oxygen permeation, and inhibits radical polymerization [20].
Material jetting (MJT) or photo-polymer jetting involves applying tiny drops of material directly to the build platform via the print head, followed by photo-polymerization in an intermediate exposure step, and requires no post-polymerization. The object is built on a layer by layer basis, extremely fast and highly accurate. A special feature is the multi-material 3D-printing multicolor mode [21].
Unlike vat photo-polymerization and MJT, which use photo-polymeric materials, fusion deposition modelling (FDM) is an extrusion-based printing technique in which melted thermoplastic materials are being used to manufacture the desired object, using layer by layer deposition. Initially used only for polymeric structures, it has been subsequently modified to process ceramics and composites [22]. Despite the low cost, because of the longer printing times and lower resolutions, FDM is currently considered of lesser relevance for dental purposes [21]. A wide range of polymeric materials, in a filament form, have been considered: ABS, PC, thermoplastics, polyamide (PA), polystyrene (PS), polyetherimide (PEI) and polyoxymethylene (POM) as well as polyethylene (PE) [23].
Selective laser sintering (SLS), which uses a high-power pulsed laser to fuse polymeric, metallic or ceramic powder particles, by creating surface layers, is currently mostly used in dentistry for printing metallic structures [10].
Binder jetting (BJ) utilizes selectively deposited liquid bonding agents to fuse powdered material [20].
The applications of most commonly used additive manufacturing technologies in dentistry are presented in Figure 3.
This entry is adapted from the peer-reviewed paper 10.3390/polym14173658
This entry is offline, you can click here to edit this entry!