Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Jessica Chacon | -- | 1209 | 2022-09-13 17:39:00 | | | |
| 2 | Conner Chen | + 1 word(s) | 1210 | 2022-09-14 09:39:12 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Kye, Y.; Nagineni, L.; Gadad, S.; Ramirez, F.; Riva, H.; Fernandez, L.; Samaniego, M.; Holland, N.; Yeh, R.; Takigawa, K.; et al. Cancer and Immunotherapy. Encyclopedia. Available online: https://encyclopedia.pub/entry/27137 (accessed on 28 February 2026).
Kye Y, Nagineni L, Gadad S, Ramirez F, Riva H, Fernandez L, et al. Cancer and Immunotherapy. Encyclopedia. Available at: https://encyclopedia.pub/entry/27137. Accessed February 28, 2026.
Kye, Yae, Lokesh Nagineni, Shrikanth Gadad, Fabiola Ramirez, Hannah Riva, Lorena Fernandez, Michelle Samaniego, Nathan Holland, Rose Yeh, Kei Takigawa, et al. "Cancer and Immunotherapy" Encyclopedia, https://encyclopedia.pub/entry/27137 (accessed February 28, 2026).
Kye, Y., Nagineni, L., Gadad, S., Ramirez, F., Riva, H., Fernandez, L., Samaniego, M., Holland, N., Yeh, R., Takigawa, K., Dhandayuthapani, S., & Chacon, J. (2022, September 13). Cancer and Immunotherapy. In Encyclopedia. https://encyclopedia.pub/entry/27137
Kye, Yae, et al. "Cancer and Immunotherapy." Encyclopedia. Web. 13 September, 2022.
Copy Citation
The era of personalized cancer therapy is here. Advances in the field of immunotherapy have paved the way for the development of individualized neoantigen-based therapies that can translate into favorable treatment outcomes and fewer side effects for patients.
neoantigen
immunotherapy
tumor-associated antigens
1. Introduction
Immunotherapy has rapidly become a primary mode of cancer treatment due to the remarkable success and clinical improvement seen in patients with advanced-stage or aggressive, recurrent cancers such as melanoma, ovarian cancer, breast cancer, and gastrointestinal cancers [1]. A significant number of therapies that have seen success to date involve the utilization of T cells. This is because of the tumor cell’s unique ability to suppress the immune system by modulating its surrounding microenvironment, also known as the tumor microenvironment (TME). By targeting the TME with antigen-specific immune cells, it is able to essentially activate the immune system to mount an anti-cancer attack.
There has been much interest in identifying, developing, and producing immune cells and proteins that are able to mount a potent immune response against the tumor cells and their TME. This vested interest has led to the production of various immunotherapies including monoclonal antibodies (mAbs), tumor-infiltrating lymphocytes (TIL), and chimeric antigen receptor T-cells (CAR-T). Despite these advancements, due to the metabolic reprogramming and adaptability of cancer cells, these immunotherapies have been met with both innate and acquired resistance [2][3]. This has led to the search for new immunotherapy targets and has opened a new hallmark of cancer immunotherapy.
Neoantigens are tumor-specific proteins synthesized by tumor cells as protein by-products [4][5]. The rapid division and proliferation of tumor cells lead to various mutations in coding and non-coding loci [4][5]. The changes in the amino acid sequence that occur due to mutations in coding regions leads to the production of proteins that are not found in normal cells and are unique to tumor cells [4][5][6]. These tumor-specific by-products termed neoantigens are unique in that multiple patients can share the same neoantigens (shared neoantigens), but they can also be specific to an individual (personalized neoantigens) [4][5][6]. In addition, neoantigens are highly immunogenic, making them a favorable immunotherapy target [5][7].
2. Cancer and Immunotherapy
The relationship between cancer and the immune system is very dynamic. Cancer cells modulate the immune system to survive, proliferate, and metastasize. For instance, tumor cells express immuno-suppressive ligands on the cell surface such as programmed death ligand-1 (PDL-1) to evade immune cell recognition and inhibit the mounting of an immune response. In addition, tumor cells can also hijack and employ crosstalk to mediate immune cells and inflammation to aid with metastasis [8][9]. The basis of immunotherapy is to target these specific areas of crosstalk, intervene, and modulate the immune response to target the cancer cells. The ultimate goal of immunotherapy is to enhance recognition, target, and mount a toxic response against the cancer cells [4].
Monoclonal antibodies (mAbs) are a type of targeted immunotherapy that has shown promising therapeutic results that is currently being used to treat various cancers including breast cancer, colorectal cancer, and leukemias [5][7][10]. For instance, mAbs can mount a potent immune response and can be employed to trigger cytotoxicity and inhibit further tumorigenesis (Figure 1A) [1][11][12]. They are able to recognize both cell surface antigens and secreted antigens with high specificity, indicating their versality [10].
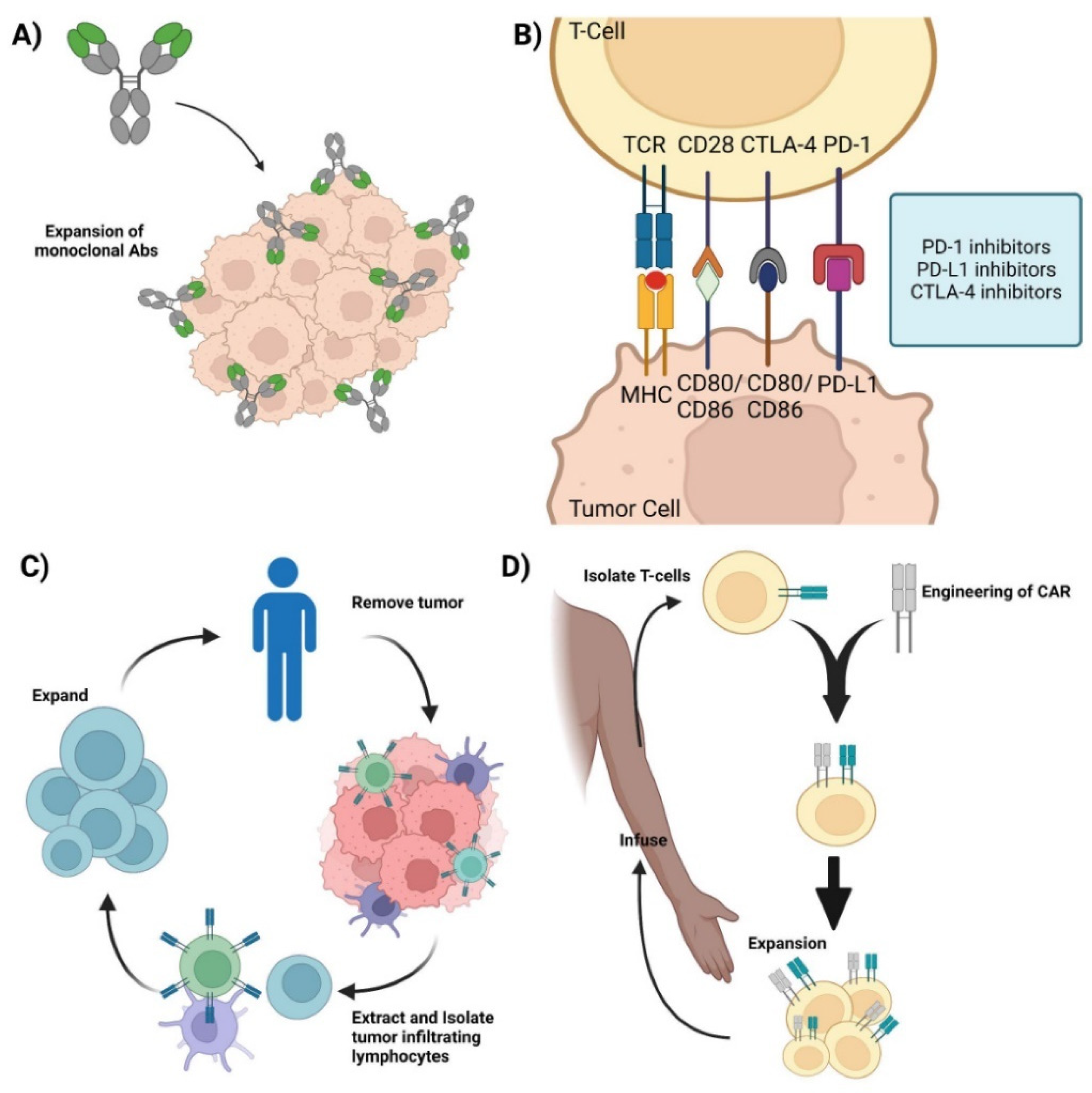
Figure 1. Current immunotherapies. (A) Monoclonal antibodies—representation of mAbs and the mechanism involved in mounting an immune response against cancer cells. (B) Immune checkpoint inhibitors—Graphic showcasing the immune crosstalk that occurs between T cells and tumor cells and the respective ligands and receptors targeted using mAbs. (C) Adoptive Cell Therapy—Graphic showing how TILs are synthesized by removing the respective tumor from the patient, isolating, extracting, and expanding the appropriate TILs, and its re-infusion back into the patient for therapy. (D) Chimeric Antigen Receptor T-cell therapy—Representation of CAR-T synthesis and production. Isolate T cells from the patient and mount a synthetic CAR onto the host T cells. Expand the modified T cell population and re-infuse back into the patient. Credits: Images were created using BioRender.
One of the more successful therapeutic mAbs are immune checkpoint inhibitors (ICIs) [4] This is possible because of the T cells’ unique ability to moderate their own immune response. T cells keep the immune system from becoming overly active and destructive. This self-modulating mechanism is conducted by immune checkpoint proteins such as CTLA-1 and PD-1, where the binding of the respective receptors and ligands on T cells induces a regulatory response and curtails the immune response [13][14]. Cancer cells take advantage of this self-regulating function of T cells by synthesizing and presenting these markers to the cell surface, inhibiting the T cell from mounting a response, allowing the cancer cell to evade apoptosis and survive [1][11][12]. ICIs target these immunosuppressive ligands and receptors and renders them inactive, thereby turning on and activating the immune system (Figure 1B). By targeting these immune checkpoint markers, cancer cells are unable to regulate or evade the immune system, making them susceptible to apoptosis. Retrospective studies have shown that ICIs, such as the CTLA-4 mAb, ipilimumab, are effective for the treatment of metastatic melanoma [15][16][17][18]. Additionally, the combination of anti-PD-1/PD-L1 and anti-CTLA-4 mAbs has been shown to be therapeutically responsive in treating various cancers including hepatocellular carcinoma and ovarian cancer [19][20][21][22].
Adoptive cell therapy (ACT) is a passive immunotherapy that uses tumor-infiltrating lymphocytes (TIL) to induce tumor-suppressive or cytotoxic effects. ACT entails isolating and extracting immune cells from patients, inducing cell differentiation ex vivo, and expanding and re-infusing the cells back into the patients (Figure 1C). It is used to grow a large army of immune cells outside the body that when re-infused back into the patient lead a potent immune response against antigen-specific tumor cells [6][7]. TIL therapy has shown significant results in the treatment of several cancers, especially metastatic melanoma [15][16][17][18][22]. One of the major advantages of utilizing TILs for immunotherapy is the diverse repertoire of antigens that TILs can recognize.
Other ACTs include T-cell Receptor-engineered T cell (TCR-T) and Chimeric Antigen Receptor T-cell (CAR-T) therapies. TCR-T therapy uses genetically modified natural T cells to target and destroy tumors and relies on the interaction between the peptide-MHC complex to mount a potent cytotoxic response against the tumor. TCR-T has been used to target various tumors and hematologic malignancies and current studies have shown TCR-T to be more effective against solid tumors rather than hematologic malignancies [7][23]. In contrast, CAR-T therapy uses genetically engineered T cells that can mount a cytotoxic response without the peptide–MHC complex interaction (Figure 1D) and has shown clinical efficacy against hematologic malignancies, with efficacy against solid tumors currently being thoroughly investigated [24][25].
Despite significant increases in overall survival and the therapeutic success found with these immunotherapies, they are not without adverse effects or complications. Immunotherapeutic agents have led to the development of serious (and sometimes fatal) immune-related adverse events (irAEs) in a subset of patients [26]. Therapeutic response rates have also varied among patients and different solid tumor types [14][27] In addition, resistance to these immunotherapies is an unfortunate complication that limits the duration and efficacy of treatment. Although there have been various methods to combat these barriers including the use of a combination of mAbs to induce a polyclonal response, there still exists room for optimization and further development [1][11][12][24][25]. With the advancements in high-throughput sequencing, prediction algorithms, and screening and characterization technology, the focus of immunotherapy has turned towards neoantigens.
References
- Marrocco, I.; Romaniello, D.; Yarden, Y. Cancer Immunotherapy: The Dawn of Antibody Cocktails. In Human Monoclonal Antibodies; Steinitz, M., Ed.; Methods in Molecular Biology; Springer: New York, NY, USA, 2019; Volume 1904, pp. 11–51.
- O’Donnell, J.S.; Teng, M.W.L.; Smyth, M.J. Cancer immunoediting and resistance to T cell-based immunotherapy. Nat. Rev. Clin. Oncol. 2019, 16, 151–167.
- Lei, X.; Lei, Y.; Li, J.-K.; Du, W.-X.; Li, R.-G.; Yang, J.; Li, J.; Li, F.; Tan, H.-B. Immune cells within the tumor microenvironment: Biological functions and roles in cancer immunotherapy. Cancer Lett. 2019, 470, 126–133.
- Zhang, Z.; Lu, M.; Qin, Y.; Gao, W.; Tao, L.; Su, W.; Zhong, J. Neoantigen: A New Breakthrough in Tumor Immunotherapy. Front. Immunol. 2021, 12, 672356.
- Jiang, T.; Shi, T.; Zhang, H.; Hu, J.; Song, Y.; Wei, J.; Ren, S.; Zhou, C. Tumor neoantigens: From basic research to clinical applications. J. Hematol. Oncol. 2019, 12, 1–13.
- Zhang, Q.; Jia, Q.; Zhang, J.; Zhu, B. Neoantigens in precision cancer immunotherapy: From identification to clinical applications. Chin. Med. J. 2022; Publish Ah.
- Peng, M.; Mo, Y.; Wang, Y.; Wu, P.; Zhang, Y.; Xiong, F.; Guo, C.; Wu, X.; Li, Y.; Li, X.; et al. Neoantigen vaccine: An emerging tumor immunotherapy. Mol. Cancer 2019, 18, 1–14.
- Itoh, Y.; Nagase, H. Matrix metalloproteinases in cancer. Essays Biochem. 2002, 38, 21–36.
- Garner, H.; de Visser, K.E. Immune crosstalk in cancer progression and metastatic spread: A complex conversation. Nat. Rev. Immunol. 2020, 20, 483–497.
- Pelletier, J.P.R.; Mukhtar, F. Passive Monoclonal and Polyclonal Antibody Therapies. In Immunologic Concepts in Transfusion Medicine; Elsevier: Amsterdam, The Netherlands, 2020; pp. 251–348.
- Zahavi, D.J.; Weiner, L.M. Targeting Multiple Receptors to Increase Checkpoint Blockade Efficacy. Int. J. Mol. Sci. 2019, 20, 158.
- Ahmadzadeh, M.; Pasetto, A.; Jia, L.; Deniger, D.C.; Stevanović, S.; Robbins, P.F.; Rosenberg, S.A. Tumor-infiltrating human CD4 + regulatory T cells display a distinct TCR repertoire and exhibit tumor and neoantigen reactivity. Sci. Immunol. 2019, 4, eaao4310.
- Pearlman, A.H.; Hwang, M.S.; Konig, M.F.; Hsiue, E.H.-C.; Douglass, J.; DiNapoli, S.R.; Mog, B.J.; Bettegowda, C.; Pardoll, D.M.; Gabelli, S.B.; et al. Targeting public neoantigens for cancer immunotherapy. Nat. Cancer 2021, 2, 487–497.
- Pardoll, D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer 2012, 12, 252–264.
- Wolchok, J.D.; Chiarion-Sileni, V.; Gonzalez, R.; Rutkowski, P.; Grob, J.-J.; Cowey, C.L.; Lao, C.D.; Wagstaff, J.; Schadendorf, D.; Ferrucci, P.F.; et al. Overall Survival with Combined Nivolumab and Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2017, 377, 1345–1356.
- Hodi, F.S.; O’Day, S.J.; McDermott, D.F.; Weber, R.W.; Sosman, J.A.; Haanen, J.B.; Gonzalez, R.; Robert, C.; Schadendorf, D.; Hassel, J.C.; et al. Improved Survival with Ipilimumab in Patients with Metastatic Melanoma. N. Engl. J. Med. 2010, 363, 711–723.
- Ghisoni, E.; Wicky, A.; Bouchaab, H.; Imbimbo, M.; Delyon, J.; Moura, B.G.; Gérard, C.; Latifyan, S.; Özdemir, B.; Caikovski, M.; et al. Late-onset and long-lasting immune-related adverse events from immune checkpoint-inhibitors: An overlooked aspect in immunotherapy. Eur. J. Cancer 2021, 149, 153–164.
- Uhara, H.; Kiyohara, Y.; Uehara, J.; Fujisawa, Y.; Takenouchi, T.; Otsuka, M.; Uchi, H.; Fukushima, S.; Minami, H.; Hatsumichi, M.; et al. Five-year survival with nivolumab in previously untreated Japanese patients with advanced or recurrent malignant melanoma. J. Dermatol. 2021, 48, 592–599.
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905.
- Yau, T.; Kang, Y.-K.; Kim, T.-Y.; El-Khoueiry, A.B.; Santoro, A.; Sangro, B.; Melero, I.; Kudo, M.; Hou, M.-M.; Matilla, A.; et al. Efficacy and Safety of Nivolumab Plus Ipilimumab in Patients With Advanced Hepatocellular Carcinoma Previously Treated With Sorafenib: The CheckMate 040 Randomized Clinical Trial. JAMA Oncol. 2020, 6, e204564.
- Bagchi, S.; Yuan, R.; Engleman, E.G. Immune Checkpoint Inhibitors for the Treatment of Cancer: Clinical Impact and Mechanisms of Response and Resistance. Annu. Rev. Pathol. Mech. Dis. 2021, 16, 223–249.
- El-Osta, H.; Jafri, S. Predictors for clinical benefit of immune checkpoint inhibitors in advanced non-small-cell lung cancer: A meta-analysis. Immunotherapy 2019, 11, 189–199.
- Tsimberidou, A.-M.; Van Morris, K.; Vo, H.H.; Eck, S.; Lin, Y.-F.; Rivas, J.M.; Andersson, B.S. T-cell receptor-based therapy: An innovative therapeutic approach for solid tumors. J. Hematol. Oncol. 2021, 14, 1–22.
- Ma, S.; Li, X.; Wang, X.; Cheng, L.; Li, Z.; Zhang, C.; Ye, Z.; Qian, Q. Current Progress in CAR-T Cell Therapy for Solid Tumors. Int. J. Biol. Sci. 2019, 15, 2548–2560.
- Depil, S.; Duchateau, P.; Grupp, S.A.; Mufti, G.; Poirot, L. ‘Off-the-shelf’ allogeneic CAR T cells: Development and challenges. Nat. Rev. Drug Discov. 2020, 19, 185–199.
- Kunte, S.; Abraham, J.; Montero, A.J. Novel HER2–targeted therapies for HER2–positive metastatic breast cancer. Cancer 2020, 126, 4278–4288.
- Binnewies, M.; Roberts, E.W.; Kersten, K.; Chan, V.; Fearon, D.F.; Merad, M.; Coussens, L.M.; Gabrilovich, D.I.; Ostrand-Rosenberg, S.; Hedrick, C.C.; et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat. Med. 2018, 24, 541–550.
More
Information
Subjects:
Oncology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
854
Revisions:
2 times
(View History)
Update Date:
14 Sep 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





