
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Lola Llobat | -- | 3864 | 2022-08-30 12:08:41 | | | |
| 2 | Peter Tang | Meta information modification | 3864 | 2022-08-31 02:49:54 | | |
Video Upload Options
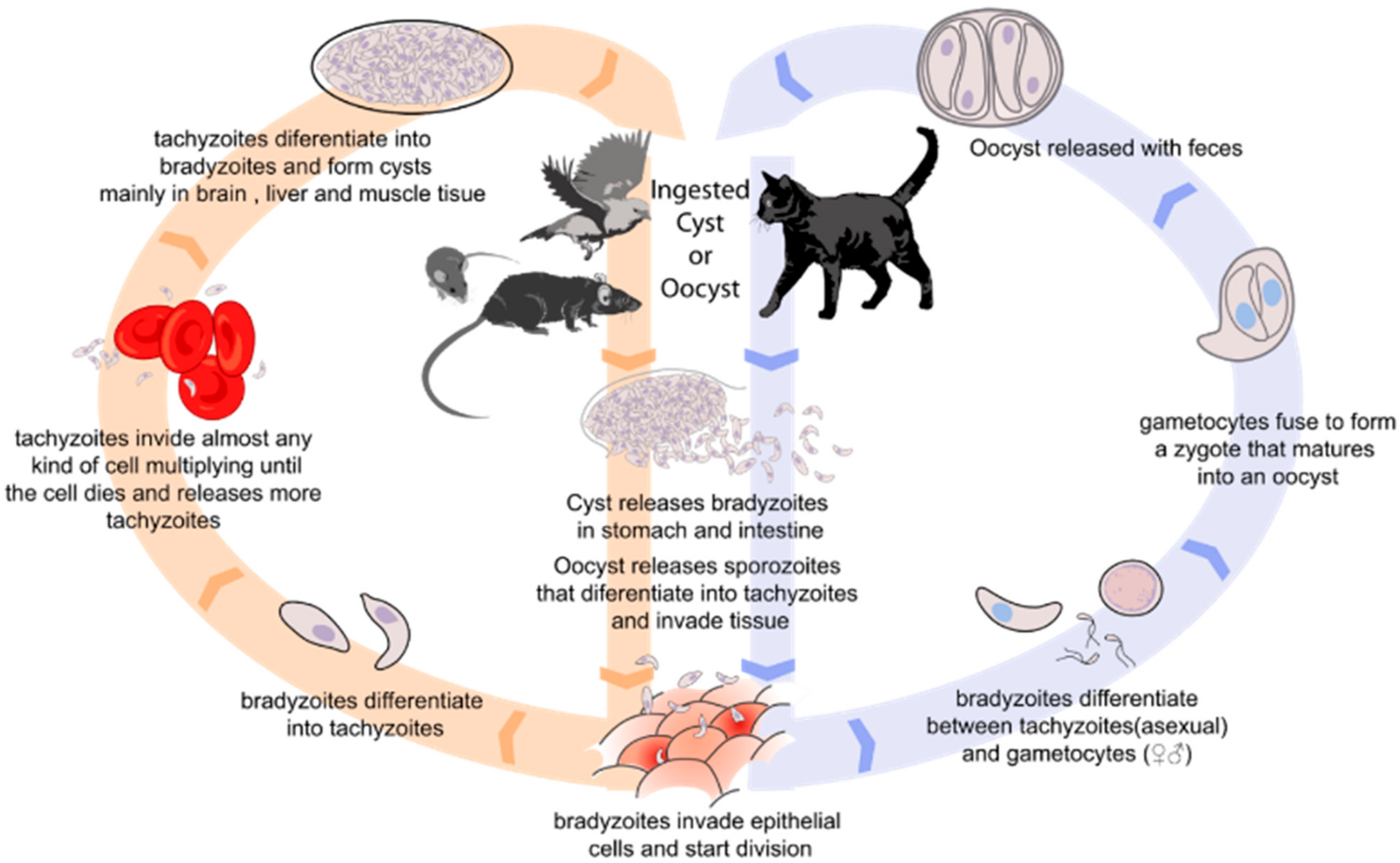
Toxoplasma gondii is an obligate intracellular parasite that causes toxoplasmosis, with approximately one third of the population around the world seropositive. The consumption of contaminated food is the main source of infection. These include meat products with T. gondii tissue cysts, and dairy products with tachyzoites.
1. Introduction
2. Methods for T. gondii Detection in Food Products
|
Detection Method |
Specific Method 1 |
Type of Food Product |
Detection Range (Sensitivity) 2 |
References |
|---|---|---|---|---|
|
Animal model bioassay |
Cat |
Milk |
25% |
|
|
Meat |
100% |
[31] |
||
|
Mouse |
Milk |
100% |
[29] |
|
|
Meat |
100% (10 tachyzoites) |
[24] |
||
|
Fresh products |
13% |
[32] |
||
|
Bivalve mollusks |
2.5% |
[33] |
||
|
Water |
100% |
[34] |
||
|
Cell culture |
Meat |
100% (10,000 tachyzoites) |
[24] |
|
|
Milk |
- |
[30] |
||
|
Microscopic method |
Meat |
- |
[31] |
|
|
Molecular methods |
PCR |
Meat |
47.1% |
[35] |
|
Fresh products |
95–100% |
|||
|
Water |
100% |
[36] |
||
|
Milk |
100% |
|||
|
Cheese |
100% |
[29] |
||
|
qPCR |
Meat |
92.3% (limit 0.01 pg) |
||
|
Fresh products |
100% (1 oocyst) |
|||
|
Bivalve mollusks |
100% |
[44] |
||
|
Water |
100% |
[44] |
||
|
LAMP |
Lymph nodes |
85.7% |
[45] |
|
|
Mussels |
5 oocyst/g |
[46] |
||
|
Fresh products |
25 oocyst/50 g |
[47] |
||
|
Water |
100% (1 fg) |
|||
|
Serological methods |
IHA |
Meat Juice |
100% (10,000 oocysts) |
[50] |
|
IFAT |
Meat |
97% |
[51] |
|
|
Meat Juice |
96.9% (10,000 oocysts) |
[50] |
||
|
MAT |
Meat |
86.6% |
[51] |
|
|
Milk |
- |
[52] |
||
|
ELISA |
Milk |
- |
[30] |
|
|
Meat |
91% |
[51] |
||
|
Meat Juice |
100% (10,000 oocysts) |
[50] |
||
|
BBMA |
Meat |
98.5% |
[53] |
1 PCR: Polymerase chain reaction; qPCR: real-time PCR; LAMP: Loop-mediated isothermal amplification; IHA: indirect hemagglutination antibody; IFAT: indirect fluorescent antibody test; MAT: modified agglutination test; ELISA: Enzyme-Linked Immunosorbent Assay; BBMA: bead-based multiplex assay. 2 The column shows the percentage of samples that were positively detected by the method and the quantity of parasites per quantity of food product that was detected if this data is known. The value (-) means that this data is not known.
3. Prevalence of Toxoplasma gondii in Food Products
3.1. Meat and Meat Products
|
Animal |
Sample Analyzed |
Detection Method 1 |
Number of Samples Tested |
Number of Positive Samples (%) |
Location |
Reference |
|---|---|---|---|---|---|---|
|
Sheep |
Serum |
ELISA |
150 |
26 (17.3%) |
Iran |
[57] |
|
Serum |
ELISA |
550 |
59 (10.8%) |
Iran |
[58] |
|
|
Serum |
ELISA |
1039 |
179 (17.2%) |
Latvia |
[59] |
|
|
Serum |
MAT |
100 |
42 (42%) |
Lebanon |
[60] |
|
|
Serum |
ELISA |
64 |
30 (47%) |
Slovakia |
[61] |
|
|
Serum |
DAT |
252 |
148 (58.2%) |
Ethiopia |
[62] |
|
|
Liver |
PCR |
150 |
26 (17.3%) |
Iran |
[57] |
|
|
Liver |
PCR |
90 |
13 (14.4%) |
Iran |
[63] |
|
|
Heart |
PCR |
150 |
48 (32%) |
Iran |
[57] |
|
|
Brain and heart |
MAT |
136 |
10 (7.4%) |
India |
[64] |
|
|
Meat juice |
ELISA |
227 |
126 (28.6%) |
Italy |
[65] |
|
|
Meat juice |
MAT |
166 |
11 (6.6%) |
China |
[66] |
|
|
Meat |
PCR |
150 |
33 (22%) |
Iran |
[57] |
|
|
Meat |
PCR |
438 |
43 (9.8) |
China |
[67] |
|
|
Meat |
PCR |
150 |
50 (33.3) |
Tunisia |
[68] |
|
|
Meat |
ELISA |
109 |
38 (34.9%) |
Malaysia |
[69] |
|
|
Meat |
PCR |
79 |
34 (43%) |
Australia |
[70] |
|
|
Meat |
PCR |
177 |
3 (1.7%) |
India |
[71] |
|
|
Goat |
Serum |
ELISA |
150 |
16 (10.7%) |
Iran |
[57] |
|
Serum |
ELISA |
185 |
37 (20%) |
Iran |
[58] |
|
|
Serum |
ELISA |
445 |
189 (42.5%) |
India |
[72] |
|
|
Serum |
MAT |
80 |
27 (34%) |
Lebanon |
[61] |
|
|
Serum |
ELISA |
39 |
8 (21%) |
Slovakia |
[61] |
|
|
Serum |
LAT |
116 |
64 (55.2%) |
Ethiopia |
[62] |
|
|
Liver |
PCR |
150 |
24 (16%) |
Iran |
[57] |
|
|
Liver |
PCR |
90 |
8 (8.8%) |
India |
[63] |
|
|
Heart |
PCR |
150 |
36 (24%) |
Iran |
[57] |
|
|
Brain and heart |
MAT |
57 |
4 (7%) |
India |
[64] |
|
|
Meat juice |
ELISA |
51 |
14 (27.5%) |
Italy |
[65] |
|
|
Meat |
PCR |
150 |
26 (17.3%) |
Iran |
[57] |
|
|
Meat |
PCR |
254 |
27 (10.7) |
China |
[67] |
|
|
Meat |
PCR |
120 |
39 (32.5) |
Tunisia |
[68] |
|
|
Meat |
ELISA |
75 |
41 (54.7%) |
Malaysia |
[69] |
|
|
Meat |
PCR |
223 |
3 (1.3%) |
India |
[72] |
|
|
Cattle |
Serum |
ELISA |
57 |
13 (22.8%) |
Italy |
[73] |
|
Serum |
DAT |
2411 |
313 (13%) |
Poland |
[74] |
|
|
Serum |
ELISA |
400 |
52 (13%) |
Iran |
[75] |
|
|
Serum |
IFAT |
500 |
2.3 (40.6%) |
Brazil |
[76] |
|
|
Meat |
PCR |
150 |
29 (19.3) |
Tunisia |
[68] |
|
|
Meat |
ELISA |
392 |
98 (25%) |
Malaysia |
[69] |
|
|
Meat |
PCR |
48 |
5 (10.4%) |
Brazil |
[76] |
|
|
Pig |
Serum |
ELISA |
653 |
4 (0.6%) |
Finland |
[77] |
|
Serum |
ELISA |
447 |
73 (16.3%) |
Denmark |
[78] |
|
|
Serum |
DAT |
3111 |
370 (11.9%) |
Poland |
[74] |
|
|
Serum |
IFAT |
94 |
44 (46.8%) |
Romania |
[79] |
|
|
Serum |
ELISA |
420 |
56 (23.3%) |
Cuba |
[80] |
|
|
Serum |
ELISA |
370 |
14 (3.8%) |
Italy |
[81] |
|
|
Serum |
ELISA and IFAT |
127 |
56 (44.1%) |
Italy |
[82] |
|
|
Serum |
MAT |
375 |
8 (2.1%) |
Italy |
[83] |
|
|
Serum |
ELISA |
414 |
214 (51.7%) |
Italy |
[84] |
|
|
Serum |
MAT |
182 |
31 (17%) |
Serbia |
[85] |
|
|
Serum |
MAT and IFAT |
356 |
25 (7%) and 48 (13.5%), respectively |
Brazil |
[86] |
|
|
Serum |
MAT and IFAT |
400 |
26 (6.5%) |
Brazil |
[87] |
|
|
Serum |
IFAT |
60 |
44 (77%) |
Brazil |
[88] |
|
|
Serum |
IHA |
784 |
156 (19.9%) |
China |
[89] |
|
|
Tongue |
PCR |
60 |
20 (33.3%) |
Brazil |
[88] |
|
|
Tongue and muscle |
PCR |
810 |
54 (6.7%) |
India |
[90] |
|
|
Brain |
PCR |
339 |
34 (10%) |
China |
[91] |
|
|
Brain |
PCR |
107 |
51 (47.7%) |
Italy |
[84] |
|
|
Heart |
PCR |
94 |
25 (26.6%) |
Romania |
[79] |
|
|
Heart |
qPCR |
103 |
12 (11.6%) |
Italy |
[92] |
|
|
Diaphragm |
PCR |
45 |
15 (33.3%) |
Serbia |
[85] |
|
|
Diaphragm |
PCR |
1223 |
107 (8.7%) |
China |
[93] |
|
|
Diaphragm |
PCR |
60 |
24 (40%) |
Brazil |
[88] |
|
|
Diaphragm |
qPCR |
103 |
2 (1.9%) |
Italy |
[94] |
|
|
Tissue of seropositive animals |
Mouse bioassay |
26 |
18 (69.2%) |
Brazil |
[87] |
|
|
Muscle |
PCR |
60 |
23 (38.3%) |
Brazil |
[88] |
|
|
Meat juice |
ELISA |
212 |
33 (15.6%) |
Denmark |
[78] |
|
|
Meat |
qPCR |
118 |
46 (39%) |
Brazil |
[94] |
|
|
Meat |
PCR |
498 |
165 (33.1%) |
Italy |
[95] |
|
|
Meat |
PCR |
49 |
3 (6.1%) |
Brazil |
[76] |
|
|
Raw meat products |
PCR |
3223 |
175 (5.4%) |
Poland |
[96] |
|
|
Chicken |
Serum |
IFAT |
200 |
72 (36%) |
Brazil |
[97] |
|
Serum |
ELISA |
522 |
34 (6.5%) |
India |
[98] |
|
|
Serum |
LACA |
267 |
29 (10.9%) |
Japan |
[99] |
|
|
Brain |
Mouse Bioassay |
14 |
2 (14.3%) |
Brazil |
[97] |
|
|
Heart juice |
MAT |
1185 |
230 (19.4%) |
USA |
[100] |
|
|
Muscle and heart |
PCR |
522 |
12 (2.3%) |
India |
[98] |
|
|
Meat |
PCR |
257 |
21 (8.2%) |
China |
[101] |
|
|
Ducks |
Meat |
PCR |
115 |
9 (7.8%) |
China |
[101] |
|
Geese |
Meat |
PCR |
42 |
2 (4.8%) |
China |
[101] |
|
Rabbit |
Brain and heart |
PCR |
470 |
13 (2.8%) |
China |
[102] |
|
Kibbeh |
Meat |
PCR |
44 |
1 (2.3%) |
Brazil |
[76] |
|
Water Buffalo |
Serum |
MAT and ELISA |
197 |
16 (8.1%) and 13 (6.6%), respectively |
Romania |
[103] |
|
Ostriches (farmed) |
Serum |
LAT |
409 |
149 (36%) |
Czech Republic |
[104] |
|
Common quails (farmed) |
Serum |
MAT |
620 |
59 (9.5%) |
China |
[105] |
|
Donkey (farmed) |
Meat |
PCR |
618 |
57 (9.2%) |
China |
[106] |
|
Tolai hares (farmed) |
Serum |
PCR |
358 |
29 (8.1%) |
China |
[107] |
|
Brain |
PCR |
358 |
23 (6.4%) |
China |
[107] |
|
|
Feral swine |
Serum |
ELISA |
376 |
34 (9%) |
USA |
[108] |
|
Wild boar (farmed) |
Serum |
LAT |
882 |
88 (10%) |
China |
[109] |
|
Wild boar |
Serum |
ELISA |
331 |
164 (49%) |
Italy |
[110] |
|
Serum |
ELISA |
181 |
17 (9%) |
Finland |
[111] |
|
|
Serum |
IFAT |
26 |
20 (76.9%) |
Brazil |
[112] |
|
|
Serum |
ELISA |
306 |
61 (20%) |
Germany |
[113] |
|
|
Tissue |
Mouse bioassay |
22 |
1 (4.5%) |
Brazil |
[112] |
|
|
Brain |
qPCR |
141 |
44 (31.2%) |
Italy |
[114] |
|
|
Brain |
PCR |
263 |
58 (22%) |
Italy |
[115] |
|
|
Heart |
qPCR |
166 |
47 (28.3%) |
Italy |
[114] |
|
|
Heart |
PCR |
310 |
70 (22.6%) |
Italy |
[115] |
|
|
Muscle |
qPCR |
165 |
40 (24.2%) |
Italy |
[114] |
|
|
Muscle |
PCR |
311 |
74 (23.8%) |
Italy |
[115] |
|
|
Meat juice |
ELISA |
97 |
42 (43.3%) |
Italy |
[116] |
|
|
Meat |
qPCR |
306 |
37 (12%) |
Germany |
[113] |
|
|
Venison |
Serum |
MAT |
914 |
329 (36%) |
USA |
[117] |
|
Heart |
Mouse bioassay |
36 |
11 (30.6%) |
USA |
[117] |
|
|
Roe deer |
Serum |
LAT |
356 |
141 (39.6%) |
Spain |
[118] |
|
Serum |
ELISA |
323 |
130 (40.2%) |
Italy |
[119] |
|
|
Serum |
ELISA |
184 |
20 (11%) |
Germany |
[113] |
|
|
Meat |
qPCR |
184 |
11 (6%) |
Germany |
[113] |
|
|
Fallow deer |
Serum |
LAT |
372 |
138 (37.1%) |
Spain |
[120] |
|
Serum |
ELISA |
167 |
17 (10%) |
Slovakia |
[61] |
|
|
Meat |
qPCR |
80 |
2 (2%) |
Germany |
[113] |
|
|
Red deer |
Serum |
LAT |
553 |
92 (16.6%) |
Spain |
[118] |
|
Serum |
ELISA |
96 |
19 (19.8%) |
Italy |
[110] |
|
|
Serum |
ELISA |
65 |
4 (6%) |
Germany |
[113] |
|
|
Meat |
qPCR |
65 |
2 (2%) |
Germany |
[113] |
|
|
Southern chamois |
Serum |
LAT |
186 |
26 (14%) |
Spain |
[118] |
|
Mouflon |
Serum |
LAT |
209 |
24 (11.5%) |
Spain |
[118] |
|
Serum |
ELISA |
50 |
12 (24%) |
Italy |
[110] |
|
|
Iberian wild goat |
Serum |
LAT |
346 |
27 (7.8%) |
Spain |
[118] |
|
Chamois |
Serum |
ELISA |
104 |
4 (3.8%) |
Italy |
[110] |
|
Barbary sheep |
Serum |
LAT |
18 |
1 (5.6%) |
Spain |
[118] |
|
Moose |
Serum |
DAT |
463 |
111 (23.9%) |
Estonia |
[119] |
|
Wild ducks |
Brain |
qPCR |
280 |
7 (2.5%) |
Czech Republic |
[120] |
|
Heart |
qPCR |
280 |
11 (3.9%) |
Czech Republic |
[120] |
|
|
Muscle |
qPCR |
280 |
4 (1.4%) |
Czech Republic |
[120] |
|
|
Common pheasants |
Brain |
qPCR |
350 |
8 (2.3%) |
Czech Republic |
[120] |
|
Heart |
qPCR |
350 |
4 (1.1%) |
Czech Republic |
[120] |
|
|
Muscle |
qPCR |
350 |
3 (0.9%) |
Czech Republic |
[120] |
1 ELISA: Enzyme-Linked Immunosorbent Assay; MAT: modified agglutination test; DAT: direct agglutination test; PCR: Polymerase chain reaction; LAT: latex agglutination test; IFAT: indirect fluorescent antibody test; qPCR: real-time PCR.
3.2. Milk and Dairy Products
|
Animal |
Sample Analyzed |
Detection Method 1 |
Number of Samples Tested |
Number of Positive Samples (%) |
Location |
Reference |
|---|---|---|---|---|---|---|
|
Donkey |
Milk |
ELISA |
418 |
41 (9.2%) |
China |
[123] |
|
Goat |
Milk |
ELISA |
30 |
19 (63.3%) |
Italy |
[129] |
|
Milk |
PCR |
60 |
39 (65%) |
Poland |
[130] |
|
|
Milk |
ELISA and qPCR |
30 |
27 (90%) and 1 (3.3%), respectively |
Egypt |
[131] |
|
|
Bulk tank milk |
ELISA |
100 |
59 (59%) |
Italy |
[129] |
|
|
Sheep |
Milk |
PCR |
58 |
1 (1.7%) |
Mongolia |
[124] |
|
Milk |
ELISA and qPCR |
30 |
18 (60%) and 1 (3.3%), respectively |
Egypt |
[131] |
|
|
Camel |
Milk |
PCR |
9 |
8 (88.9%) |
Mongolia |
[124] |
|
Milk |
ELISA and qPCR |
30 |
1 (3.33%) and 0 (0%), respectively |
Egypt |
[131] |
|
|
Cattle |
Bulk tank milk |
ELISA |
149 |
8 (5.4%) |
Iran |
[132] |
1 ELISA: Enzyme-Linked Immunosorbent Assay; PCR: Polymerase chain reaction; qPCR: real-time PCR.
3.3. Fresh Products and Vegetables
|
Product Analyzed |
Detection Method 1 |
Number of Samples Tested |
Number of Positive Samples (%) |
Location |
Reference |
|---|---|---|---|---|---|
|
Mixed-salad packages |
qPCR |
648 packages |
5 (0.8%) |
Italy |
[141] |
|
PCR |
90 packages |
8 (8.9%) |
Czech Republic |
[142] |
|
|
Leafy greens |
qPCR |
152 |
45 (29.6%) |
Morocco |
[143] |
|
Carrot |
qPCR |
30 |
3 (10%) |
Morocco |
[144] |
|
qPCR |
46 |
9 (19.5%) |
Poland |
[135] |
|
|
PCR |
93 |
7 (7.5%) |
Czech Republic |
[142] |
|
|
Chicory |
PCR |
40 |
2 (5%) |
Brazil |
[145] |
|
Red cabbage |
qPCR |
8 |
1 (1.2%) |
China |
[42] |
|
Coriander |
qPCR |
29 |
8 (27.6%) |
Morocco |
[144] |
|
Cucumber |
PCR |
109 |
13 (11.9%) |
Czech Republic |
[142] |
|
Lettuce |
qPCR |
28 |
3 (10.7%) |
Morocco |
[144] |
|
qPCR |
50 |
9 (18%) |
Poland |
[135] |
|
|
qPCR |
71 |
5 (7%) |
China |
[42] |
|
|
PCR |
168 |
5 (3%) |
Brazil |
[145] |
|
|
Spinach |
qPCR |
50 |
2 (4%) |
China |
[42] |
|
Parsley |
qPCR |
29 |
13 (44.8%) |
Morocco |
[144] |
|
PCR |
5 |
1 (20%) |
Brazil |
[145] |
|
|
Pak Choi |
qPCR |
34 |
1 (2.9%) |
China |
[42] |
|
Radish |
qPCR |
16 |
1 (6.3%) |
Morocco |
[144] |
|
qPCR |
60 |
3 (5%) |
Poland |
[42] |
|
|
Rape |
qPCR |
22 |
1 (4.5%) |
China |
[42] |
|
Rocket |
PCR |
7 |
1 (14.3%) |
Brazil |
[145] |
1 PCR: Polymerase chain reaction; qPCR: real-time PCR.
3.4. Marine Products
|
Animal |
Sample Analyzed |
Detection Method 1 |
Number of Samples Tested |
Number of Positive Samples (%) |
Location |
Reference |
|---|---|---|---|---|---|---|
|
Bivalve shellfish |
Tissue |
PCR |
2907 |
82 (2.8%) |
China |
[152] |
|
Green-lipped mussels |
Tissue |
PCR |
104 |
13 (16.4%) |
New Zealand |
[153] |
|
Mediterranean mussel |
Gills |
qPCR |
53 pools at 795 specimens |
21 (39.6%) |
Turkey |
[147] |
|
Clam |
Tissue |
qPCR |
61 pools at 1020 specimens |
4 (6.6%) |
Tunisia |
[148] |
|
Digestive gland |
PCR |
390 |
6 (1.5%) |
Canada |
[154] |
|
|
Haemolymph |
PCR |
390 |
2 (0.6%) |
Canada |
[154] |
|
|
Mediterranean scald fish |
Gills |
PCR |
1 pool at 6 specimens |
1 (100%) |
Italy |
[155] |
|
Pacific oyster |
Gills |
PCR |
6 pools at 109 specimens |
1 (16.67%) |
Italy |
[156] |
|
Oyster |
Mantle, gills, and rectum |
qPCR |
1440 |
447 (31%) |
USA |
[157] |
|
Bogue |
Gills |
PCR |
26 pools at 260 specimens |
4 (15.4%) |
Italy |
[155] |
|
Intestine |
PCR |
26 pools at 260 specimens |
3 (11.5%) |
Italy |
[155] |
|
|
Muscle |
PCR |
26 pools at 260 fish |
6 (23.1%) |
Italy |
[155] |
|
|
White seabream |
Muscle |
PCR |
3 pools of 18 specimens |
1 (33.3%) |
Italy |
[155] |
|
European anchovy |
Gills |
PCR |
35 pools at 350 specimens |
2 (5.7%) |
Italy |
[155] |
|
Intestine |
PCR |
35 pools at 350 specimens |
1 (2.9%) |
Italy |
[155] |
|
|
European hake |
Gills |
PCR |
15 pools at 90 specimens |
1 (6.7%) |
Italy |
[155] |
|
Muscle |
PCR |
15 pools at 90 specimens |
1 (6.7%) |
Italy |
[155] |
|
|
Red mullet |
Intestine |
PCR |
11 pools at 110 specimens |
3 (27.3%) |
Italy |
[155] |
|
American prawn |
Muscle |
PCR |
618 |
4 |
China |
[155] |
|
Nippon shrimp |
Muscle |
PCR |
813 |
1 |
China |
[158] |
|
Axillary seabream |
Gills |
PCR |
8 pools at 80 specimens |
2 (25%) |
Italy |
[155] |
|
Intestine |
PCR |
8 pools at 80 specimens |
1 (12.5%) |
Italy |
[155] |
|
|
Muscle |
PCR |
8 pools at 80 specimens |
1 (12.5%) |
Italy |
[155] |
|
|
Common pandora |
Gills |
PCR |
3 pools at 18 specimens |
1 (33.3%) |
Italy |
[155] |
|
Intestine |
PCR |
3 pools at 18 specimens |
2 (66.7%) |
Italy |
[155] |
|
|
Muscle |
PCR |
3 pools at 18 specimens |
1 (33.3%) |
Italy |
[155] |
|
|
Thornback ray |
Muscle |
PCR |
1 fish |
1 (100%) |
Italy |
[156] |
|
Red scorpionfish |
Intestine |
PCR |
1 pool at 3 specimens |
1 (100%) |
Italy |
[155] |
|
Blotched picarel |
Muscle |
PCR |
4 pools at 24 specimens |
1 (25%) |
Italy |
[155] |
|
Atlantic horse mackerel |
Muscle |
PCR |
15 pools at 120 specimens |
4 (26.7%) |
Italy |
[155] |
1 PCR: Polymerase chain reaction; qPCR: real-time PCR.
4. Control and Food Safety
References
- Rabilloud, M.; Wallon, M.; Peyron, F. In Utero and at Birth Diagnosis of Congenital Toxoplasmosis: Use of Likelihood Ratios for Clinical Management. Pediatr. Infect. Dis. J. 2010, 29, 421–425.
- Maldonado, Y.A.; Read, J.S.; Committee on Infectious Diseases. Diagnosis, Treatment, and Prevention of Congenital Toxoplasmosis in the United States. Pediatrics 2017, 139, e20163860.
- Wallon, M.; Peyron, F. Effect of Antenatal Treatment on the Severity of Congenital Toxoplasmosis. Clin. Infect Dis. 2016, 62, 811–812.
- Conceição, A.R.; Belucik, D.N.; Missio, L.; Gustavo Brenner, L.; Henrique Monteiro, M.; Ribeiro, K.S.; Costa, D.F.; Valadão, M.C.d.S.; Commodaro, A.G.; de Oliveira Dias, J.R.; et al. Ocular Findings in Infants with Congenital Toxoplasmosis after a Toxoplasmosis Outbreak. Ophthalmology 2021, 128, 1346–1355.
- Daher, D.; Shaghlil, A.; Sobh, E.; Hamie, M.; Hassan, M.E.; Moumneh, M.B.; Itani, S.; El Hajj, R.; Tawk, L.; El Sabban, M.; et al. Comprehensive Overview of Toxoplasma Gondii-Induced and Associated Diseases. Pathogens 2021, 10, 1351.
- Robert-Gangneux, F.; Dardé, M.-L. Epidemiology of and Diagnostic Strategies for Toxoplasmosis. Clin. Microbiol. Rev. 2012, 25, 264–296.
- Rajapakse, S.; Weeratunga, P.; Rodrigo, C.; de Silva, N.L.; Fernando, S.D. Prophylaxis of Human Toxoplasmosis: A Systematic Review. Pathog. Glob. Health 2017, 111, 333–342.
- Yazdani, M.R.; Mehrabi, Z.; Ataei, B.; Ghahfarokhi, A.B.; Moslemi, R.; Pourahmad, M. Frequency of Sero-Positivity in Household Members of the Patients with Positive Toxoplasma Serology. Rev. Esp. Quim. 2018, 31, 506–510.
- Montoya, J.G.; Liesenfeld, O. Toxoplasmosis. Lancet 2004, 363, 1965–1976.
- Matta, S.K.; Rinkenberger, N.; Dunay, I.R.; Sibley, L.D. Toxoplasma gondii Infection and Its Implications within the Central Nervous System. Nat. Rev. Microbiol. 2021, 19, 467–480.
- Hermes, G.; Ajioka, J.W.; Kelly, K.A.; Mui, E.; Roberts, F.; Kasza, K.; Mayr, T.; Kirisits, M.J.; Wollmann, R.; Ferguson, D.J.; et al. Neurological and Behavioral Abnormalities, Ventricular Dilatation, Altered Cellular Functions, Inflammation, and Neuronal Injury in Brains of Mice Due to Common, Persistent, Parasitic Infection. J. Neuroinflammation 2008, 5, 48.
- Xiao, J.; Li, Y.; Gressitt, K.L.; He, H.; Kannan, G.; Schultz, T.L.; Svezhova, N.; Carruthers, V.B.; Pletnikov, M.V.; Yolken, R.H.; et al. Cerebral Complement C1q Activation in Chronic Toxoplasma Infection. Brain Behav. Immun. 2016, 58, 52–56.
- Johnson, H.J.; Koshy, A.A. Latent Toxoplasmosis Effects on Rodents and Humans: How Much Is Real and How Much Is Media Hype? mBio 2020, 11, e02164-19.
- Johnson, S.K.; Johnson, P.T.J. Toxoplasmosis: Recent Advances in Understanding the Link Between Infection and Host Behavior. Annu. Rev. Anim. Biosci. 2021, 9, 249–264.
- Vallochi, A.L.; Goldberg, A.C.; Falcai, A.; Ramasawmy, R.; Kalil, J.; Silveira, C.; Belfort, R.; Rizzo, L.V. Molecular Markers of Susceptibility to Ocular Toxoplasmosis, Host and Guest Behaving Badly. Clin. Ophthalmol. 2008, 2, 837–848.
- Scallan, E.; Hoekstra, R.M.; Angulo, F.J.; Tauxe, R.V.; Widdowson, M.-A.; Roy, S.L.; Jones, J.L.; Griffin, P.M. Foodborne Illness Acquired in the United States--Major Pathogens. Emerg. Infect. Dis. 2011, 17, 7–15.
- Chaichan, P.; Mercier, A.; Galal, L.; Mahittikorn, A.; Ariey, F.; Morand, S.; Boumédiène, F.; Udonsom, R.; Hamidovic, A.; Murat, J.B.; et al. Geographical Distribution of Toxoplasma gondii Genotypes in Asia: A Link with Neighboring Continents. Infect. Genet. Evol. 2017, 53, 227–238.
- Almeria, S.; Dubey, J.P. Foodborne Transmission of Toxoplasma gondii Infection in the Last Decade. An Overview. Res. Vet. Sci. 2021, 135, 371–385.
- Shapiro, K.; Kim, M.; Rajal, V.B.; Arrowood, M.J.; Packham, A.; Aguilar, B.; Wuertz, S. Simultaneous Detection of Four Protozoan Parasites on Leafy Greens Using a Novel Multiplex PCR Assay. Food Microbiol. 2019, 84, 103252.
- Luna, J.C.; Zamora, A.; Hernández-Arango, N.; Muñoz-Sánchez, D.; Pinzón, M.I.; Cortés-Vecino, J.A.; Lora-Suarez, F.; Gómez-Marín, J.E. Food Safety Assessment and Risk for Toxoplasmosis in School Restaurants in Armenia, Colombia. Parasitol. Res. 2019, 118, 3449–3457.
- EFSA Panel on Biological Hazards (BIOHAZ); Koutsoumanis, K.; Allende, A.; Alvarez-Ordóñez, A.; Bolton, D.; Bover-Cid, S.; Chemaly, M.; Davies, R.; De Cesare, A.; Herman, L.; et al. Public Health Risks Associated with Food-Borne Parasites. EFSA J. 2018, 16, e05495.
- European Food Safety Authority and European Centre for Disease Prevention and Control (EFSA and ECDC). The European Union One Health 2018 Zoonoses Report. EFSA J. 2019, 17, e05926.
- European Food Safety Authority; European Centre for Disease Prevention and Control. The European Union One Health 2019 Zoonoses Report. EFSA J. 2021, 19, e06406.
- Opsteegh, M.; Dam-Deisz, C.; de Boer, P.; DeCraeye, S.; Faré, A.; Hengeveld, P.; Luiten, R.; Schares, G.; van Solt-Smits, C.; Verhaegen, B.; et al. Methods to Assess the Effect of Meat Processing on Viability of Toxoplasma Gondii: Towards Replacement of Mouse Bioassay by in Vitro Testing. Int. J. Parasitol. 2020, 50, 357–369.
- Duong, H.D.; Taniguchi, Y.; Takashima, Y.; Sekiguchi, S.; Aye, K.M.; Ahmadi, P.; Bui, L.K.; Irie, T.; Nagayasu, E.; Yoshida, A. Diagnostic Value of Recombinant Nanoluciferase Fused Toxoplasma gondii Antigens in Luciferase-Linked Antibody Capture Assay (LACA) for Toxoplasma Infection in Pigs. J. Vet. Med. Sci. 2022, 84, 905–913.
- Suwan, E.; Chalermwong, P.; Rucksaken, R.; Sussadee, M.; Kaewmongkol, S.; Udonsom, R.; Jittapalapong, S.; Mangkit, B. Development and Evaluation of Indirect Enzyme-Linked Immunosorbent Assay Using Recombinant Dense Granule Antigen 7 Protein for the Detection of Toxoplasma gondii Infection in Cats in Thailand. Vet. World 2022, 15, 602–610.
- Mancusi, A.; Giordano, A.; Bosco, A.; Girardi, S.; Proroga, Y.T.R.; Morena, L.; Pinto, R.; Sarnelli, P.; Cringoli, G.; Rinaldi, L.; et al. Development of a Droplet Digital Polymerase Chain Reaction Tool for the Detection of Toxoplasma gondii in Meat Samples. Parasitol. Res. 2022, 121, 1467–1473.
- Bouwknegt, M.; Devleesschauwer, B.; Graham, H.; Robertson, L.J.; van der Giessen, J.W. The Euro-Fbp Workshop Participants Prioritisation of Food-Borne Parasites in Europe, 2016. Eurosurveillance 2018, 23, 17–00161.
- Dubey, J.P.; Verma, S.K.; Ferreira, L.R.; Oliveira, S.; Cassinelli, A.B.; Ying, Y.; Kwok, O.C.H.; Tuo, W.; Chiesa, O.A.; Jones, J.L. Detection and Survival of Toxoplasma gondii in Milk and Cheese from Experimentally Infected Goats. J. Food Prot. 2014, 77, 1747–1753.
- Dehkordi, F.S.; Borujeni, M.R.H.; Rahimi, E.; Abdizadeh, R. Detection of Toxoplasma gondii in Raw Caprine, Ovine, Buffalo, Bovine, and Camel Milk Using Cell Cultivation, Cat Bioassay, Capture ELISA, and PCR Methods in Iran. Foodborne Pathog. Dis. 2013, 10, 120–125.
- Opsteegh, M.; Maas, M.; Schares, G.; van der Giessen, J. Relationship between Seroprevalence in the Main Livestock Species and Presence of Toxoplasma gondii in Meat (GP/EFSA/BIOHAZ/2013/01) An Extensive Literature Review. Final Report. EFSA Support. Publ. 2016, 13, 996E.
- El-Tras, W.F.; Tayel, A.A.; El-Kady, N.N. Source Diversity of Toxoplasma gondii Infection During Meal Preparation. J. Food Saf. 2012, 32, 1–5.
- Esmerini, P.O.; Gennari, S.M.; Pena, H.F.J. Analysis of Marine Bivalve Shellfish from the Fish Market in Santos City, São Paulo State, Brazil, for Toxoplasma gondii. Vet. Parasitol. 2010, 170, 8–13.
- Dubey, J.P. Toxoplasma gondii Oocyst Survival under Defined Temperatures. J. Parasitol. 1998, 84, 862–865.
- De Oliveira Mendonça, A.; Domingues, P.F.; Vieira Da Silva, A.; Bergamaschi Pezerico, S.; Langoni, H. Detection of Toxoplasma gondii in Swine Sausages. Parasitol. Latinoam. 2004, 59, 42–45.
- Reiling, S.J.; Merks, H.; Zhu, S.; Boone, R.; Corneau, N.; Dixon, B.R. A Cloth-Based Hybridization Array System for Rapid Detection of the Food- and Waterborne Protozoan Parasites Giardia duodenalis, Cryptosporidium spp. and Toxoplasma gondii. Food Waterborne Parasitol. 2021, 24, e00130.
- Marques, C.S.; Sousa, S.; Castro, A.; da Costa, J.M.C. Detection of Toxoplasma gondii Oocysts in Fresh Vegetables and Berry Fruits. Parasites Vectors 2020, 13, 180.
- Deljavan, N.; Moosavy, M.-H.; Hajipour, N. Molecular Detection of Toxoplasma gondii DNA in Goats (Capra hircus), Sheep (Ovis aries), and Donkey (Equus asinus) Milk Using PCR in East Azerbaijan Province, Iran. Res. Vet. Sci. 2022, 152, 58–60.
- Aigner, C.P.; da Silva, A.V.; Sandrini, F.; Osório, P.d.S.; Poiares, L.; Largura, A. Real-Time PCR-Based Quantification of Toxoplasma gondii in Tissue Samples of Serologically Positive Outdoor Chickens. Mem. Inst. Oswaldo Cruz 2010, 105, 935–937.
- Marino, A.M.F.; Percipalle, M.; Giunta, R.P.; Salvaggio, A.; Caracappa, G.; Alfonzetti, T.; Aparo, A.; Reale, S. Development and Validation of a Real-Time PCR Assay for the Detection of Toxoplasma gondii DNA in Animal and Meat Samples. J. Vet. Diagn. Investig. 2017, 29, 203–207.
- Temesgen, T.T.; Robertson, L.J.; Tysnes, K.R. A Novel Multiplex Real-Time PCR for the Detection of Echinococcus multilocularis, Toxoplasma gondii, and Cyclospora cayetanensis on Berries. Food Res. Int. 2019, 125, 108636.
- Lass, A.; Ma, L.; Kontogeorgos, I.; Zhang, X.; Li, X.; Karanis, P. First Molecular Detection of Toxoplasma gondii in Vegetable Samples in China Using Qualitative, Quantitative Real-Time PCR and Multilocus Genotyping. Sci. Rep. 2019, 9, 17581.
- Kim, M.; Shapiro, K.; Rajal, V.B.; Packham, A.; Aguilar, B.; Rueda, L.; Wuertz, S. Quantification of Viable Protozoan Parasites on Leafy Greens Using Molecular Methods. Food Microbiol. 2021, 99, 103816.
- Marangi, M.; Giangaspero, A.; Lacasella, V.; Lonigro, A.; Gasser, R.B. Multiplex PCR for the Detection and Quantification of Zoonotic Taxa of Giardia, Cryptosporidium and Toxoplasma in Wastewater and Mussels. Mol. Cell. Probes 2015, 29, 122–125.
- Zhang, H.; Thekisoe, O.M.M.; Aboge, G.O.; Kyan, H.; Yamagishi, J.; Inoue, N.; Nishikawa, Y.; Zakimi, S.; Xuan, X. Toxoplasma gondii: Sensitive and Rapid Detection of Infection by Loop-Mediated Isothermal Amplification (LAMP) Method. Exp. Parasitol. 2009, 122, 47–50.
- Durand, L.; La Carbona, S.; Geffard, A.; Possenti, A.; Dubey, J.P.; Lalle, M. Comparative Evaluation of Loop-Mediated Isothermal Amplification (LAMP) vs QPCR for Detection of Toxoplasma gondii Oocysts DNA in Mussels. Exp. Parasitol. 2020, 208, 107809.
- Lalle, M.; Possenti, A.; Dubey, J.P.; Pozio, E. Loop-Mediated Isothermal Amplification-Lateral-Flow Dipstick (LAMP-LFD) to Detect Toxoplasma gondii Oocyst in Ready-to-Eat Salad. Food Microbiol. 2018, 70, 137–142.
- Mahmoudi, M.R.; Kazemi, B.; Haghighi, A.; Karanis, P. Detection of Acanthamoeba and Toxoplasma in River Water Samples by Molecular Methods in Iran. Iran. J. Parasitol. 2015, 10, 250–257.
- Fallahi, S.; Mazar, Z.A.; Ghasemian, M.; Haghighi, A. Challenging Loop-Mediated Isothermal Amplification (LAMP) Technique for Molecular Detection of Toxoplasma gondii. Asian Pac. J. Trop. Med. 2015, 8, 366–372.
- Glor, S.B.; Edelhofer, R.; Grimm, F.; Deplazes, P.; Basso, W. Evaluation of a Commercial ELISA Kit for Detection of Antibodies against Toxoplasma gondii in Serum, Plasma and Meat Juice from Experimentally and Naturally Infected Sheep. Parasites Vectors 2013, 6, 85.
- Schares, G.; Koethe, M.; Bangoura, B.; Geuthner, A.-C.; Randau, F.; Ludewig, M.; Maksimov, P.; Sens, M.; Bärwald, A.; Conraths, F.J.; et al. Toxoplasma gondii Infections in Chickens–Performance of Various Antibody Detection Techniques in Serum and Meat Juice Relative to Bioassay and DNA Detection Methods. Int. J. Parasitol. 2018, 48, 751–762.
- Mancianti, F.; Nardoni, S.; D’Ascenzi, C.; Pedonese, F.; Mugnaini, L.; Franco, F.; Papini, R. Seroprevalence, Detection of DNA in Blood and Milk, and Genotyping of Toxoplasma gondii in a Goat Population in Italy. Biomed. Res. Int. 2013, 2013, 905326.
- Fabian, B.T.; Hedar, F.; Koethe, M.; Bangoura, B.; Maksimov, P.; Conraths, F.J.; Villena, I.; Aubert, D.; Seeber, F.; Schares, G. Fluorescent Bead-Based Serological Detection of Toxoplasma gondii Infection in Chickens. Parasites Vectors 2020, 13, 388.
- Jones, J.L.; Dubey, J.P. Foodborne Toxoplasmosis. Clin. Infect. Dis. 2012, 55, 845–851.
- Opsteegh, M.; Prickaerts, S.; Frankena, K.; Evers, E.G. A Quantitative Microbial Risk Assessment for Meatborne Toxoplasma gondii Infection in The Netherlands. Int. J. Food Microbiol. 2011, 150, 103–114.
- Guo, M.; Dubey, J.P.; Hill, D.; Buchanan, R.L.; Gamble, H.R.; Jones, J.L.; Pradhan, A.K. Prevalence and Risk Factors for Toxoplasma gondii Infection in Meat Animals and Meat Products Destined for Human Consumption. J. Food Prot. 2015, 78, 457–476.
- Yousefvand, A.; Mirhosseini, S.A.; Ghorbani, M.; Mohammadzadeh, T.; Moghaddam, M.M.; Mohammadyari, S. Molecular and Serological Detection and of Toxoplasma gondii in Small Ruminants of Southwest Iran and the Potential Risks for Consumers. J. Verbrauch. Lebensm. 2021, 16, 117–127.
- Gharekhani, J.; Yakhchali, M.; Esmaeilnejad, B.; Mardani, K.; Majidi, G.; Sohrabi, A.; Berahmat, R.; Hazhir Alaei, M. Seroprevalence and Risk Factors of Neospora Caninum and Toxoplasma gondii in Small Ruminants in Southwest of Iran. Arch. Razi Inst. 2018, 73, 305–310.
- Deksne, G.; Ligere, B.; Šneidere, A.; Jokelainen, P. Seroprevalence and Factors Associated with Toxoplasma gondii Infections in Sheep in Latvia: Latvian Dark Headed Sheep Breed Associated with Higher Seroprevalence. Vector Borne Zoonotic Dis. 2017, 17, 478–482.
- El Safadi, D.; Abi Chahine, D.; Al Tarraf, A.; Raii, O.; Mesto, K.; Ismail, M.B.; Hamze, M. First Report on Seroprevalence and Risk Factors of Toxoplasma gondii Infection in Sheep and Goats in North Lebanon. J. Infect. Dev. Ctries. 2019, 13, 831–836.
- Moskwa, B.; Kornacka, A.; Cybulska, A.; Cabaj, W.; Reiterova, K.; Bogdaszewski, M.; Steiner-Bogdaszewska, Z.; Bien, J. Seroprevalence of Toxoplasma gondii and Neospora caninum Infection in Sheep, Goats, and Fallow Deer Farmed on the Same Area. J. Anim. Sci. 2018, 96, 2468–2473.
- Tegegne, D.; Kelifa, A.; Abdurahaman, M.; Yohannes, M. Seroepidemiology and Associated Risk Factors of Toxoplasma gondii in Sheep and Goats in Southwestern Ethiopia. BMC Vet. Res. 2016, 12, 280.
- Bahreh, M.; Hajimohammadi, B.; Eslami, G. Toxoplasma gondii in Sheep and Goats from Central Iran. BMC Res. Notes 2021, 14, 46.
- Satbige, A.S.; Sreekumar, C.; Rajendran, C.; Vijaya Bharathi, M. Isolation and Characterization of Toxoplasma gondii from Small Ruminants (Sheep and Goats) in Chennai City, South India. J. Parasit. Dis. 2017, 41, 869–873.
- Gazzonis, A.L.; Zanzani, S.A.; Villa, L.; Manfredi, M.T. Toxoplasma gondii Infection in Meat-Producing Small Ruminants: Meat Juice Serology and Genotyping. Parasitol. Int. 2020, 76, 102060.
- Jiang, N.; Su, R.; Jian, F.; Su, C.; Zhang, L.; Jiang, Y.; Yang, Y. Toxoplasma gondii in Lambs of China: Heart Juice Serology, Isolation and Genotyping. Int. J. Food Microbiol. 2020, 322, 108563.
- Ai, K.; Huang, C.-Q.; Guo, J.-J.; Cong, H.; He, S.-Y.; Zhou, C.-X.; Cong, W. Molecular Detection of Toxoplasma gondii in the Slaughter Sheep and Goats from Shandong Province, Eastern China. Vector Borne Zoonotic Dis. 2020, 20, 193–196.
- Amdouni, Y.; Rjeibi, M.R.; Rouatbi, M.; Amairia, S.; Awadi, S.; Gharbi, M. Molecular Detection of Toxoplasma gondii Infection in Slaughtered Ruminants (Sheep, Goats and Cattle) in Northwest Tunisia. Meat Sci. 2017, 133, 180–184.
- Abdul Hamid, N.; Sadiq, M.B.; Ramanoon, S.Z.; Mansor, R.; Watanabe, M.; Md Isa, N.M.; Kamaludeen, J.; Syed-Hussain, S.S. Seroprevalence and Risk Factors of Toxoplasma gondii in Ruminant Meats from Wet Markets in Klang Valley and Abattoirs in Selangor, Malaysia. Animals 2020, 10, 1139.
- Dawson, A.C.; Ashander, L.M.; Appukuttan, B.; Woodman, R.J.; Dubey, J.P.; Whiley, H.; Smith, J.R. Lamb as a Potential Source of Toxoplasma gondii Infection for Australians. Aust. N. Z. J. Public Health 2020, 44, 49–52.
- Kalambhe, D.; Gill, J.P.S.; Singh, B.B. Molecular Detection of Toxoplasma gondii in the Slaughter Sheep and Goats from North India. Vet. Parasitol. 2017, 241, 35–38.
- Bachan, M.; Deb, A.R.; Maharana, B.R.; Sudhakar, N.R.; Sudan, V.; Saravanan, B.C.; Tewari, A.K. High Seroprevalence of Toxoplasma gondii in Goats in Jharkhand State of India. Vet. Parasitol. Reg. Stud. Rep. 2018, 12, 61–68.
- Gazzonis, A.L.; Marino, A.M.F.; Garippa, G.; Rossi, L.; Mignone, W.; Dini, V.; Giunta, R.P.; Luini, M.; Villa, L.; Zanzani, S.A.; et al. Toxoplasma gondii Seroprevalence in Beef Cattle Raised in Italy: A Multicenter Study. Parasitol. Res. 2020, 119, 3893–3898.
- Sroka, J.; Karamon, J.; Wójcik-Fatla, A.; Piotrowska, W.; Dutkiewicz, J.; Bilska-Zając, E.; Zając, V.; Kochanowski, M.; Dąbrowska, J.; Cencek, T. Toxoplasma gondii Infection in Slaughtered Pigs and Cattle in Poland: Seroprevalence, Molecular Detection and Characterization of Parasites in Meat. Parasites Vectors 2020, 13, 223.
- Gharekhani, J.; Yakhchali, M. Risk Factors Associated to Toxoplasma gondii Infection in Dairy Farms in Hamedan Suburb, Iran. J. Parasit. Dis. 2020, 44, 116–121.
- Langoni, H.; Generoso, D.; Hayasaka, Ê.Y.; Mantovan, K.B.; Menozzi, B.D.; Richini-Pereira, V.B.; da Silva, R.C. Molecular Characterization of Toxoplasma gondii and Sarcocystis spp. in Raw Kibbeh and Other Meat Samples Commercialized in Botucatu, Southeastern Brazil. Rev. Bras. Parasitol. Vet. 2021, 30, e029320.
- Felin, E.; Hälli, O.; Heinonen, M.; Jukola, E.; Fredriksson-Ahomaa, M. Assessment of the Feasibility of Serological Monitoring and On-Farm Information about Health Status for the Future Meat Inspection of Fattening Pigs. Prev. Vet. Med. 2019, 162, 76–82.
- Olsen, A.; Sandberg, M.; Houe, H.; Nielsen, H.V.; Denwood, M.; Jensen, T.B.; Alban, L. Seroprevalence of Toxoplasma gondii Infection in Sows and Finishers from Conventional and Organic Herds in Denmark: Implications for Potential Future Serological Surveillance. Prev. Vet. Med. 2020, 185, 105149.
- Paştiu, A.I.; Cozma-Petruț, A.; Mercier, A.; Balea, A.; Galal, L.; Mircean, V.; Pusta, D.L.; Bogdan, L.; Györke, A. Prevalence and Genetic Characterization of Toxoplasma gondii in Naturally Infected Backyard Pigs Intended for Familial Consumption in Romania. Parasites Vectors 2019, 12, 586.
- Castillo-Cuenca, J.C.; Martínez-Moreno, Á.; Diaz-Cao, J.M.; Entrena-García, A.; Fraga, J.; Arias, P.C.; Almería, S.; García-Bocanegra, I. Seroprevalence of Toxoplasma gondii and Associated Risk Factors in Domestic Pigs Raised from Cuba. Parasitol. Res. 2021, 120, 2897–2903.
- Gazzonis, A.L.; Marangi, M.; Villa, L.; Ragona, M.E.; Olivieri, E.; Zanzani, S.A.; Giangaspero, A.; Manfredi, M.T. Toxoplasma gondii Infection and Biosecurity Levels in Fattening Pigs and Sows: Serological and Molecular Epidemiology in the Intensive Pig Industry (Lombardy, Northern Italy). Parasitol. Res. 2018, 117, 539–546.
- Macaluso, G.; Di Bella, S.; Purpari, G.; Giudice, E.; Mira, F.; Gucciardi, F.; Marino, A.M.F.; Russo, C.; Gómez-Morales, M.A.; Guercio, A. Evaluation of a Commercial Enzyme-Linked Immunosorbent Assay (ELISA) for Detecting Antibodies against Toxoplasma gondii from Naturally and Experimentally Infected Pigs. Infect. Dis. 2019, 51, 26–31.
- Papini, R.; di Ciccio, P.; Marangi, M.; Ghidini, S.; Zanardi, E.; Vergara, A.; Giangaspero, A.; Nardoni, S.; Rocchigiani, G.; Mancianti, F.; et al. Occurrence of Toxoplasma gondii in Carcasses of Pigs Reared in Intensive Systems in Northern Italy. J. Food Prot. 2017, 80, 515–522.
- Pipia, A.P.; Varcasia, A.; Dessì, G.; Panzalis, R.; Gai, C.; Nonnis, F.; Veronesi, F.; Tamponi, C.; Scala, A. Seroepidemiological and Biomolecular Survey on Toxoplasma gondii Infection on Organic Pig Farms. Parasitol. Res. 2018, 117, 1637–1641.
- Kuruca, L.; Klun, I.; Uzelac, A.; Nikolić, A.; Bobić, B.; Simin, S.; Lalošević, V.; Lalošević, D.; Djurković-Djaković, O. Detection of Toxoplasma gondii in Naturally Infected Domestic Pigs in Northern Serbia. Parasitol. Res. 2017, 116, 3117–3123.
- Oliveira, G.C.; de Souza Almeida, H.M.; Sartori, R.S.; Rossi, G.A.M.; de Oliveira, L.G.; Langoni, H. Prevalence of Toxoplasma gondii Infections in Swine of Non-Tecnified Rearing Farms of the Northeastern Region of the State of São Paulo, Brazil and Associated Risk Factors. Parasite Epidemiol. Control. 2019, 4, e00080.
- Miura, A.C.; de Barros, L.D.; Ferreira, F.P.; Neto, J.M.F.; Sicupira Franco, P.M.L.; Su, C.; Vidotto, O.; Garcia, J.L. Genotyping of Toxoplasma gondii Isolated from Pigs for Human Consumption. Parasitol. Res. 2019, 118, 1593–1599.
- Silva, E.M.C.; Sousa, P.D.S.; de Carvalho, S.K.G.S.; Marques, I.C.L.; Costa, F.B.; da Costa, A.P.; Santos, L.S.D.; Braga, M.d.S.C.O.; Abreu-Silva, A.L.; Machado, R.Z.; et al. High Level of Infection by Toxoplasma gondii in Pigs Slaughtered in the City of São Luís, Maranhão. Rev. Bras. Parasitol. Vet. 2021, 30, e008721.
- Wu, F.; Wang, Y.-L.; Yang, Z.; Li, X.-L.; Li, Z.-R.; Lin, Q. Seroprevalence and Risk Factors of Toxoplasma gondii in Slaughter Pigs in Shaanxi Province, Northwestern China. Vector Borne Zoonotic Dis. 2017, 17, 517–519.
- Thakur, R.; Sharma, R.; Aulakh, R.S.; Gill, J.P.S.; Singh, B.B. Prevalence, Molecular Detection and Risk Factors Investigation for the Occurrence of Toxoplasma gondii in Slaughter Pigs in North India. BMC Vet. Res. 2019, 15, 431.
- Gui, B.-Z.; Zheng, W.-B.; Zou, Y.; Lv, Q.-Y.; Liu, M.-T.; Li, F.; Yuan, A.-W.; Li, R.-C.; Liu, G.-H. Molecular Detection and Genotyping of Toxoplasma gondii in Pigs for Human Consumption in Hunan Province, China. Foodborne Pathog. Dis. 2018, 15, 809–813.
- Vergara, A.; Marangi, M.; Caradonna, T.; Pennisi, L.; Paludi, D.; Papini, R.; Ianieri, A.; Giangaspero, A.; Normanno, G. Toxoplasma gondii Lineages Circulating in Slaughtered Industrial Pigs and Potential Risk for Consumers. J. Food Prot. 2018, 81, 1373–1378.
- Zhang, Y.; Xie, J.; Mi, R.; Ling, H.; Luo, L.; Jia, H.; Zhang, X.; Huang, Y.; Gong, H.; Han, X.; et al. Molecular Detection and Genetic Characterization of Toxoplasma gondii in Pork from Chongqing, Southwest China. Acta Trop. 2021, 224, 106134.
- Costa, D.F.; Fowler, F.; Silveira, C.; Nóbrega, M.J.; Nobrega, H.A.J.; Nascimento, H.; Rizzo, L.V.; Commodaro, A.G.; Belfort, R. Prevalence of Toxoplasma gondii DNA in Processed Pork Meat. Foodborne Pathog. Dis. 2018, 15, 734–736.
- Veronesi, F.; Santoro, A.; Milardi, G.L.; Diaferia, M.; Branciari, R.; Miraglia, D.; Cioffi, A.; Gabrielli, S.; Ranucci, D. Comparison of PCR Assays Targeting the Multi-Copy Targets B1 Gene and 529 Bp Repetitive Element for Detection of Toxoplasma gondii in Swine Muscle. Food Microbiol. 2017, 63, 213–216.
- Sroka, J.; Bilska-Zając, E.; Wójcik-Fatla, A.; Zając, V.; Dutkiewicz, J.; Karamon, J.; Piotrowska, W.; Cencek, T. Detection and Molecular Characteristics of Toxoplasma gondii DNA in Retail Raw Meat Products in Poland. Foodborne Pathog. Dis. 2019, 16, 195–204.
- Dos Santos Silva, A.C.; de Barros, L.D.; Barros, V.M.C.; de Alcântara, A.M.; Andrade, M.R.; Garcia, J.L.; Mota, R.A.; Porto, W.J.N. Occurrence of Atypical and New Genotypes of Toxoplasma gondii in Free-Range Chickens Intended for Human Consumption in Brazil. Acta Parasitol. 2020, 65, 774–778.
- Thakur, R.; Sharma, R.; Aulakh, R.S.; Singh, B.B. Toxoplasma gondii in Chickens (Gallus domesticus) from North India. Acta Parasitol. 2021, 66, 185–192.
- Duong, H.D.; Appiah-Kwarteng, C.; Takashima, Y.; Aye, K.M.; Nagayasu, E.; Yoshida, A. A Novel Luciferase-Linked Antibody Capture Assay (LACA) for the Diagnosis of Toxoplasma gondii Infection in Chickens. Parasitol. Int. 2020, 77, 102125.
- Ying, Y.; Verma, S.K.; Kwok, O.C.H.; Alibana, F.; Mcleod, R.; Su, C.; Dubey, J.P.; Pradhan, A.K. Prevalence and Genetic Characterization of Toxoplasma gondii in Free-Range Chickens from Grocery Stores and Farms in Maryland, Ohio and Massachusetts, USA. Parasitol. Res. 2017, 116, 1591–1595.
- Zou, Y.; Nie, L.-B.; Zhang, N.-Z.; Zou, F.-C.; Zhu, X.-Q.; Cong, W. First Genetic Characterization of Toxoplasma gondii Infection in Poultry Meat Intended for Human Consumption in Eastern China. Infect. Genet. Evol. 2017, 55, 172–174.
- Qian, W.; Yan, W.; Lv, C.; Bai, R.; Wang, T. Occurrence and Genetic Characterization of Toxoplasma gondii and Neospora Caninum in Slaughtered Domestic Rabbits in Central China. Parasite 2019, 26, 36.
- Bărburaș, D.; Gyӧrke, A.; Blaga, R.; Bărburaș, R.; Kalmár, Z.; Vişan, S.; Mircean, V.; Blaizot, A.; Cozma, V. Toxoplasma gondii in Water Buffaloes (Bubalus bubalis) from Romania: What Is the Importance for Public Health? Parasitol. Res. 2019, 118, 2695–2703.
- Bártová, E.; Kobédová, K.; Budíková, M.; Račka, K. Serological and Molecular Detection of Toxoplasma gondii in Farm-Reared Ostriches (Struthio camelus) in the Czech Republic. Int. J. Food Microbiol. 2021, 356, 109333.
- Cong, W.; Chi, W.-B.; Sun, W.-W.; Shan, X.-F.; Kang, Y.-H.; Meng, Q.-F.; Qian, A.-D. First Report of Toxoplasma gondii Infection in Common Quails (Coturnix coturnix) Intended for Human Consumption in Three Provinces of Northeastern China. Vector Borne Zoonotic Dis. 2017, 17, 351–353.
- Cong, W.; Chen, L.; Shan, X.-F.; Qian, A.-D.; Meng, Q.-F. First Genetic Characterization of Toxoplasma gondii Infection in Donkey Meat Slaughtered for Human Consumption in Shandong Province, Eastern China. Infect. Genet. Evol. 2018, 61, 1–3.
- Cong, W.; Zhou, C.-X.; Chen, L.; Zou, Y.; Wang, W.-L.; Meng, Q.-F.; Qian, A.-D. Toxoplasma gondii and Neospora Caninum in Tolai Hares (Lepus tolai) Intended for Human Consumption in China: Seroprevalence, DNA Detection, and Genotyping. Foodborne Pathog. Dis. 2018, 15, 544–547.
- Pedersen, K.; Bauer, N.E.; Rodgers, S.; Bazan, L.R.; Mesenbrink, B.T.; Gidlewski, T. Antibodies to Various Zoonotic Pathogens Detected in Feral Swine (Sus scrofa) at Abattoirs in Texas, USA. J. Food Prot. 2017, 80, 1239–1242.
- Bai, M.-J.; Zou, Y.; Elsheikha, H.M.; Ma, J.-G.; Zheng, W.-B.; Zhao, Q.; Zhang, X.-X.; Zhu, X.-Q. Toxoplasma gondii Infection in Farmed Wild Boars (Sus scrofa) in Three Cities of Northeast China. Foodborne Pathog. Dis. 2017, 14, 379–385.
- Crotta, M.; Pellicioli, L.; Gaffuri, A.; Trogu, T.; Formenti, N.; Tranquillo, V.; Luzzago, C.; Ferrari, N.; Lanfranchi, P. Analysis of Seroprevalence Data on Hepatitis E Virus and Toxoplasma gondii in Wild Ungulates for the Assessment of Human Exposure to Zoonotic Meat-Borne Pathogens. Food Microbiol. 2022, 101, 103890.
- Fredriksson-Ahomaa, M.; London, L.; Skrzypczak, T.; Kantala, T.; Laamanen, I.; Biström, M.; Maunula, L.; Gadd, T. Foodborne Zoonoses Common in Hunted Wild Boars. Ecohealth 2020, 17, 512–522.
- Machado, D.M.R.; de Barros, L.D.; de Souza Lima Nino, B.; de Souza Pollo, A.; Dos Santos Silva, A.C.; Perles, L.; André, M.R.; Zacarias Machado, R.; Garcia, J.L.; Lux Hoppe, E.G. Toxoplasma gondii Infection in Wild Boars (Sus scrofa) from the State of São Paulo, Brazil: Serology, Molecular Characterization, and Hunter’s Perception on Toxoplasmosis. Vet. Parasitol. Reg. Stud. Rep. 2021, 23, 100534.
- Stollberg, K.C.; Schares, G.; Mayer-Scholl, A.; Hrushetska, I.; Diescher, S.; Johne, A.; Richter, M.H.; Bier, N.S. Comparison of Direct and Indirect Toxoplasma gondii Detection and Genotyping in Game: Relationship and Challenges. Microorganisms 2021, 9, 1663.
- Santoro, M.; Viscardi, M.; Sgroi, G.; DʼAlessio, N.; Veneziano, V.; Pellicano, R.; Brunetti, R.; Fusco, G. Real-Time PCR Detection of Toxoplasma gondii in Tissue Samples of Wild Boars (Sus scrofa) from Southern Italy Reveals High Prevalence and Parasite Load. Parasites Vectors 2019, 12, 335.
- Sgroi, G.; Viscardi, M.; Santoro, M.; Borriello, G.; D’Alessio, N.; Boccia, F.; Pacifico, L.; Fioretti, A.; Veneziano, V.; Fusco, G. Genotyping of Toxoplasma gondii in Wild Boar (Sus scrofa) in Southern Italy: Epidemiological Survey and Associated Risk for Consumers. Zoonoses Public Health 2020, 67, 805–813.
- Gazzonis, A.L.; Villa, L.; Riehn, K.; Hamedy, A.; Minazzi, S.; Olivieri, E.; Zanzani, S.A.; Manfredi, M.T. Occurrence of Selected Zoonotic Food-Borne Parasites and First Molecular Identification of Alaria Alata in Wild Boars (Sus scrofa) in Italy. Parasitol. Res. 2018, 117, 2207–2215.
- Dubey, J.P.; Cerqueira-Cézar, C.K.; Murata, F.H.A.; Verma, S.K.; Kwok, O.C.H.; Pedersen, K.; Rosenthal, B.M.; Su, C. White-Tailed Deer (Odocoileus virginianus) Are a Reservoir of a Diversity of Toxoplasma gondii Strains in the USA and Pose a Risk to Consumers of Undercooked Venison. Parasitology 2020, 147, 775–781.
- Castro-Scholten, S.; Cano-Terriza, D.; Jiménez-Ruiz, S.; Almería, S.; Risalde, M.A.; Vicente, J.; Acevedo, P.; Arnal, M.C.; Balseiro, A.; Gómez-Guillamón, F.; et al. Seroepidemiology of Toxoplasma gondii in Wild Ruminants in Spain. Zoonoses Public Health 2021, 68, 884–895.
- Remes, N.; Kärssin, A.; Must, K.; Tagel, M.; Lassen, B.; Jokelainen, P. Toxoplasma gondii Seroprevalence in Free-Ranging Moose (Alces alces) Hunted for Human Consumption in Estonia: Indicator Host Species for Environmental Toxoplasma gondii Oocyst Contamination. Vet. Parasitol. Reg. Stud. Rep. 2018, 11, 6–11.
- Skorpikova, L.; Reslova, N.; Lorencova, A.; Plhal, R.; Drimaj, J.; Kamler, J.; Slany, M. Molecular Detection of Toxoplasma gondii in Feathered Game Intended for Human Consumption in the Czech Republic. Int. J. Food Microbiol. 2018, 286, 75–79.
- Boughattas, S. Toxoplasma Infection and Milk Consumption: Meta-Analysis of Assumptions and Evidences. Crit. Rev. Food Sci. Nutr. 2017, 57, 2924–2933.
- Jones, J.L.; Dargelas, V.; Roberts, J.; Press, C.; Remington, J.S.; Montoya, J.G. Risk Factors for Toxoplasma gondii Infection in the United States. Clin. Infect. Dis. 2009, 49, 878–884.
- Chen, L.; Zhao, Z.-J.; Meng, Q.-F. Detection of Specific IgG-Antibodies Against Toxoplasma gondii in the Serum and Milk of Domestic Donkeys During Lactation in China: A Potential Public Health Concern. Front. Cell. Infect. Microbiol. 2021, 11, 760400.
- Iacobucci, E.; Taus, N.S.; Ueti, M.W.; Sukhbaatar, L.; Bastsukh, Z.; Papageorgiou, S.; Fritz, H. Detection and Genotypic Characterization of Toxoplasma gondii DNA within the Milk of Mongolian Livestock. Parasitol. Res. 2019, 118, 2005–2008.
- Luptakova, L.; Benova, K.; Rencko, A.; Petrovova, E. DNA Detection of Toxoplasma gondii in Sheep Milk and Blood Samples in Relation to Phase of Infection. Vet. Parasitol. 2015, 208, 250–253.
- Vismarra, A.; Barilli, E.; Miceli, M.; Mangia, C.; Bacci, C.; Brindani, F.; Kramer, L. Toxoplasma gondii and Pre-Treatment Protocols for Polymerase Chain Reaction Analysis of Milk Samples: A Field Trial in Sheep from Southern Italy. Ital. J. Food Saf. 2017, 6, 6501.
- Gomez-Samblas, M.; Vilchez, S.; Ortega-Velázquez, R.; Fuentes, M.V.; Osuna, A. Absence of Toxoplasma gondii in 100% Iberian Products from Experimentally Infected Pigs Cured Following a Specific Traditional Process. Food Microbiol. 2021, 95, 103665.
- Gazzonis, A.L.; Zanzani, S.A.; Stradiotto, K.; Olivieri, E.; Villa, L.; Manfredi, M.T. Toxoplasma gondii Antibodies in Bulk Tank Milk Samples of Caprine Dairy Herds. J. Parasitol. 2018, 104, 560–565.
- Gazzonis, A.L.; Zanzani, S.A.; Villa, L.; Manfredi, M.T. Toxoplasma gondii in Naturally Infected Goats: Monitoring of Specific IgG Levels in Serum and Milk during Lactation and Parasitic DNA Detection in Milk. Prev. Vet. Med. 2019, 170, 104738.
- Sroka, J.; Kusyk, P.; Bilska-Zajac, E.; Karamon, J.; Dutkiewicz, J.; Wojcik-Fatla, A.; Zajac, V.; Stojecki, K.; Rozycki, M.; Cencek, T. Seroprevalence of Toxoplasma gondii Infection in Goats from the South-West Region of Poland and the Detection of T. Gondii DNA in Goat Milk. Folia Parasitol. 2017, 64, 023.
- Saad, N.M.; Hussein, A.A.A.; Ewida, R.M. Occurrence of Toxoplasma gondii in Raw Goat, Sheep, and Camel Milk in Upper Egypt. Vet. World 2018, 11, 1262–1265.
- Gharekhani, J.; Yakhchali, M.; Afshari, A.; Adabi, M. Herd-Level Contamination of Neospora caninum, Toxoplasma gondii and Brucella in Milk of Iranian Dairy Farms. Food Microbiol. 2021, 100, 103873.
- Dumètre, A.; Dardé, M.L. How to Detect Toxoplasma gondii Oocysts in Environmental Samples? FEMS Microbiol. Rev. 2003, 27, 651–661.
- Lemmon, G.H.; Gardner, S.N. Predicting the Sensitivity and Specificity of Published Real-Time PCR Assays. Ann. Clin. Microbiol. Antimicrob. 2008, 7, 18.
- Lass, A.; Pietkiewicz, H.; Szostakowska, B.; Myjak, P. The First Detection of Toxoplasma gondii DNA in Environmental Fruits and Vegetables Samples. Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 1101–1108.
- Cabral Monica, T.; Pinto-Ferreira, F.; Martins, F.D.C.; de Matos, R.L.N.; de Matos, A.M.R.N.; Santos, A.C.; Nino, B.d.S.L.; Pereira, L.; Narciso, S.G.; Garcia, J.L.; et al. Epidemiology of a Toxoplasmosis Outbreak in a Research Institution in Northern Paraná, Brazil. Zoonoses Public Health 2020, 67, 760–764.
- Ekman, C.C.J.; Chiossi, M.F.d.V.; Meireles, L.R.; de Andrade Júnior, H.F.; Figueiredo, W.M.; Marciano, M.A.M.; Luna, E.J.D.A. Case-Control Study of an Outbreak of Acute Toxoplasmosis in an Industrial Plant in the State of São Paulo, Brazil. Rev. Inst. Med. Trop. Sao Paulo 2012, 54, 239–244.
- Vieira, F.P.; Alves, M.d.G.; Martins, L.M.; Rangel, A.L.P.; Dubey, J.P.; Hill, D.; Bahia-Oliveira, L.M.G. Waterborne Toxoplasmosis Investigated and Analysed under Hydrogeological Assessment: New Data and Perspectives for Further Research. Mem. Inst. Oswaldo Cruz 2015, 110, 929–935.
- Pinto-Ferreira, F.; Caldart, E.T.; Pasquali, A.K.S.; Mitsuka-Breganó, R.; Freire, R.L.; Navarro, I.T. Patterns of Transmission and Sources of Infection in Outbreaks of Human Toxoplasmosis. Emerg. Infect. Dis. 2019, 25, 2177–2182.
- Li, J.; Wang, Z.; Karim, M.R.; Zhang, L. Detection of Human Intestinal Protozoan Parasites in Vegetables and Fruits: A Review. Parasites Vectors 2020, 13, 380.
- Caradonna, T.; Marangi, M.; Del Chierico, F.; Ferrari, N.; Reddel, S.; Bracaglia, G.; Normanno, G.; Putignani, L.; Giangaspero, A. Detection and Prevalence of Protozoan Parasites in Ready-to-Eat Packaged Salads on Sale in Italy. Food Microbiol. 2017, 67, 67–75.
- Slany, M.; Dziedzinska, R.; Babak, V.; Kralik, P.; Moravkova, M.; Slana, I. Toxoplasma gondii in Vegetables from Fields and Farm Storage Facilities in the Czech Republic. FEMS Microbiol. Lett. 2019, 366, fnz170.
- Berrouch, S.; Escotte-Binet, S.; Madline, A.; Aubert, D.; Nast, E.; La Carbona, S.; Hoummadi, L.; Hafid, J.; Villena, I. Protozoan Parasites and Leafy Greens in Marrakech: Study of Occurrence Using a Molecular Method. Acta Parasitol. 2021, 67, 546–554.
- Berrouch, S.; Escotte-Binet, S.; Amraouza, Y.; Flori, P.; Aubert, D.; Villena, I.; Hafid, J. Cryptosporidium spp., Giardia duodenalis and Toxoplasma gondii Detection in Fresh Vegetables Consumed in Marrakech, Morocco. Afr. Health Sci. 2020, 20, 1669–1678.
- Marchioro, A.A.; Tiyo, B.T.; Colli, C.M.; de Souza, C.Z.; Garcia, J.L.; Gomes, M.L.; Falavigna-Guilherme, A.L. First Detection of Toxoplasma gondii DNA in the Fresh Leafs of Vegetables in South America. Vector Borne Zoonotic Dis. 2016, 16, 624–626.
- Lindsay, D.S.; Dubey, J.P. Long-Term Survival of Toxoplasma gondii Sporulated Oocysts in Seawater. J. Parasitol. 2009, 95, 1019–1020.
- Aksoy, U.; Marangi, M.; Papini, R.; Ozkoc, S.; Bayram Delibas, S.; Giangaspero, A. Detection of Toxoplasma gondii and Cyclospora cayetanensis in Mytilus Galloprovincialis from Izmir Province Coast (Turkey) by Real Time PCR/High-Resolution Melting Analysis (HRM). Food Microbiol. 2014, 44, 128–135.
- Ghozzi, K.; Marangi, M.; Papini, R.; Lahmar, I.; Challouf, R.; Houas, N.; Ben Dhiab, R.; Normanno, G.; Babba, H.; Giangaspero, A. First Report of Tunisian Coastal Water Contamination by Protozoan Parasites Using Mollusk Bivalves as Biological Indicators. Mar. Pollut. Bull. 2017, 117, 197–202.
- Coupe, A.; Howe, L.; Shapiro, K.; Roe, W.D. Comparison of PCR Assays to Detect Toxoplasma gondii Oocysts in Green-Lipped Mussels (Perna canaliculus). Parasitol. Res. 2019, 118, 2389–2398.
- Moratal, S.; Dea-Ayuela, M.A.; Cardells, J.; Marco-Hirs, N.M.; Puigcercós, S.; Lizana, V.; López-Ramon, J. Potential Risk of Three Zoonotic Protozoa (Cryptosporidium spp., Giardia duodenalis, and Toxoplasma gondii) Transmission from Fish Consumption. Foods 2020, 9, 1913.
- Taghadosi, C.; Kojouri, G.A.; Taheri, M.A. Detection of Toxoplasma Antibodies in Sera of Salmonidae by ELISA. Comp. Clin. Pathol. 2010, 2, 203–206.
- Cong, W.; Li, M.-Y.; Zou, Y.; Ma, J.-Y.; Wang, B.; Jiang, Z.-Y.; Elsheikha, H.M. Prevalence, Genotypes and Risk Factors for Toxoplasma gondii Contamination in Marine Bivalve Shellfish in Offshore Waters in Eastern China. Ecotoxicol. Environ. Saf. 2021, 213, 112048.
- Coupe, A.; Howe, L.; Burrows, E.; Sine, A.; Pita, A.; Velathanthiri, N.; Vallée, E.; Hayman, D.; Shapiro, K.; Roe, W.D. First Report of Toxoplasma gondii Sporulated Oocysts and Giardia Duodenalis in Commercial Green-Lipped Mussels (Perna canaliculus) in New Zealand. Parasitol. Res. 2018, 117, 1453–1463.
- Fung, R.; Manore, A.J.W.; Harper, S.L.; Sargeant, J.M.; Shirley, J.; Caughey, A.; Shapiro, K. Clams and Potential Foodborne Toxoplasma gondii in Nunavut, Canada. Zoonoses Public Health 2021, 68, 277–283.
- Marino, A.M.F.; Giunta, R.P.; Salvaggio, A.; Castello, A.; Alfonzetti, T.; Barbagallo, A.; Aparo, A.; Scalzo, F.; Reale, S.; Buffolano, W.; et al. Toxoplasma gondii in Edible Fishes Captured in the Mediterranean Basin. Zoonoses Public Health 2019, 66, 826–834.
- Putignani, L.; Mancinelli, L.; Del Chierico, F.; Menichella, D.; Adlerstein, D.; Angelici, M.C.; Marangi, M.; Berrilli, F.; Caffara, M.; di Regalbono, D.A.F.; et al. Investigation of Toxoplasma gondii Presence in Farmed Shellfish by Nested-PCR and Real-Time PCR Fluorescent Amplicon Generation Assay (FLAG). Exp. Parasitol. 2011, 127, 409–417.
- Marquis, N.D.; Bishop, T.J.; Record, N.R.; Countway, P.D.; Fernández Robledo, J.A. Molecular Epizootiology of Toxoplasma gondii and Cryptosporidium parvum in the Eastern Oyster (Crassostrea virginica) from Maine (USA). Pathogens 2019, 8, 125.
- Zhang, M.; Yang, Z.; Wang, S.; Tao, L.; Xu, L.; Yan, R.; Song, X.; Li, X. Detection of Toxoplasma gondii in Shellfish and Fish in Parts of China. Vet. Parasitol. 2014, 200, 85–89.
- Jones, J.L.; Kruszon-Moran, D.; Wilson, M.; McQuillan, G.; Navin, T.; McAuley, J.B. Toxoplasma gondii Infection in the United States: Seroprevalence and Risk Factors. Am. J. Epidemiol. 2001, 154, 357–365.
- El-Nawawi, F.A.; Tawfik, M.A.; Shaapan, R.M. Methods for Inactivation of Toxoplasma gondii Cysts in Meat and Tissues of Experimentally Infected Sheep. Foodborne Pathog. Dis. 2008, 5, 687–690.
- Hill, D.; Dubey, J.P. Toxoplasma Gondii: Transmission, Diagnosis and Prevention. Clin. Microbiol. Infect. 2002, 8, 634–640.
- McCurdy, S.M.; Takeuchi, M.T.; Edwards, Z.M.; Edlefsen, M.; Kang, D.; Elaine Mayes, V.; Hillers, V.N. Food Safety Education Initiative to Increase Consumer Use of Food Thermometers in the United States. Br. Food J. 2006, 108, 775–794.
- Hill, D.E.; Luchansky, J.; Porto-Fett, A.; Gamble, H.R.; Fournet, V.M.; Hawkins-Cooper, D.S.; Urban, J.F.; Gajadhar, A.A.; Holley, R.; Juneja, V.K.; et al. Rapid Inactivation of Toxoplasma gondii Bradyzoites during Formulation of Dry Cured Ready-to-Eat Pork Sausage. Food Waterborne Parasitol. 2018, 12, e00029.
- Saridewi, R.; Lukman, D.; Sudarwanto, M.; Cahyanigsih, U.; Subekti, D. Survival of Toxoplasma gondii in Goat Milk after Pasteurization with Low Temperature and Long Time. Glob. Vet. 2013, 11, 789–793.
- Rani, S.; Pradhan, A.K. Evaluating Uncertainty and Variability Associated with Toxoplasma gondii Survival during Cooking and Low Temperature Storage of Fresh Cut Meats. Int. J. Food Microbiol. 2021, 341, 109031.
- Pinto-Ferreira, F.; Paschoal, A.T.P.; Pasquali, A.K.S.; Bernardes, J.C.; Caldart, E.T.; Freire, R.L.; Mitsuka-Breganó, R.; Navarro, I.T. Techniques for Inactivating Toxoplasma gondii Oocysts: A Systematic Review. Rev. Bras. Parasitol. Vet. 2021, 30, e026420.
- Djurković-Djaković, O.; Milenković, V. Effect of Refrigeration and Freezing on Survival of Toxoplasma gondii Tissue Cysts. Acta Vet. 2000, 50, 375–380.
- Kijlstra, A.; Jongert, E. Control of the Risk of Human Toxoplasmosis Transmitted by Meat. Int. J. Parasitol. 2008, 38, 1359–1370.
- Considine, K.M.; Kelly, A.L.; Fitzgerald, G.F.; Hill, C.; Sleator, R.D. High-Pressure Processing--Effects on Microbial Food Safety and Food Quality. FEMS Microbiol. Lett. 2008, 281, 1–9.
- Kannan, G.; Prandovszky, E.; Steinfeldt, C.B.; Gressitt, K.L.; Yang, C.; Yolken, R.H.; Severance, E.G.; Jones-Brando, L.; Pletnikov, M.V. One Minute Ultraviolet Exposure Inhibits Toxoplasma gondii Tachyzoite Replication and Cyst Conversion without Diminishing Host Humoral-Mediated Immune Response. Exp. Parasitol. 2014, 145, 110–117.
- Lacombe, A.; Breard, A.; Hwang, C.-A.; Hill, D.; Fan, X.; Huang, L.; Yoo, B.K.; Niemira, B.A.; Gurtler, J.B.; Wu, V.C.H. Inactivation of Toxoplasma gondii on Blueberries Using Low Dose Irradiation without Affecting Quality. Food Control 2017, 73, 981–985.
- Hill, D.E.; Benedetto, S.M.C.; Coss, C.; McCrary, J.L.; Fournet, V.M.; Dubey, J.P. Effects of Time and Temperature on the Viability of Toxoplasma gondii Tissue Cysts in Enhanced Pork Loin. J. Food Prot. 2006, 69, 1961–1965.
- Mirza Alizadeh, A.; Jazaeri, S.; Shemshadi, B.; Hashempour-Baltork, F.; Sarlak, Z.; Pilevar, Z.; Hosseini, H. A Review on Inactivation Methods of Toxoplasma gondii in Foods. Pathog. Glob. Health 2018, 112, 306–319.
- Herrero, L.; Gracia, M.J.; Pérez-Arquillué, C.; Lázaro, R.; Herrera, A.; Bayarri, S. Toxoplasma gondii in Raw and Dry-Cured Ham: The Influence of the Curing Process. Food Microbiol. 2017, 65, 213–220.
- Lindsay, D.S.; Collins, M.V.; Holliman, D.; Flick, G.J.; Dubey, J.P. Effects of High-Pressure Processing on Toxoplasma gondii Tissue Cysts in Ground Pork. J. Parasitol. 2006, 92, 195–196.




