
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Rita El Feghali | -- | 2000 | 2022-07-29 13:52:30 | | | |
| 2 | Lindsay Dong | -4 word(s) | 1996 | 2022-07-30 03:36:11 | | |
Video Upload Options
Temporomandibular joint (TMJ) pain is the third most prevalent chronic pain condition worldwide after tension headache and backbone. The TMJ’s position and structure make it an intersection of information and influences that expand throughout the body. Therefore, joint injury generally affects systemic health and leads to serious symptoms and disorders known as temporomandibular disorders (TMDs). Photobiomodulation (PBM) is an effective tool in alleviating TMDs’ pain and increasing the range of movement in patients with Axis 1 of TMDs. However, TMDs’ pain related to underlying pathology cannot be solely treated by PBM. The causative factors must be treated first.
1. Introduction
2. Photobiomodulation in Management of Temporomandibular Joint Pain
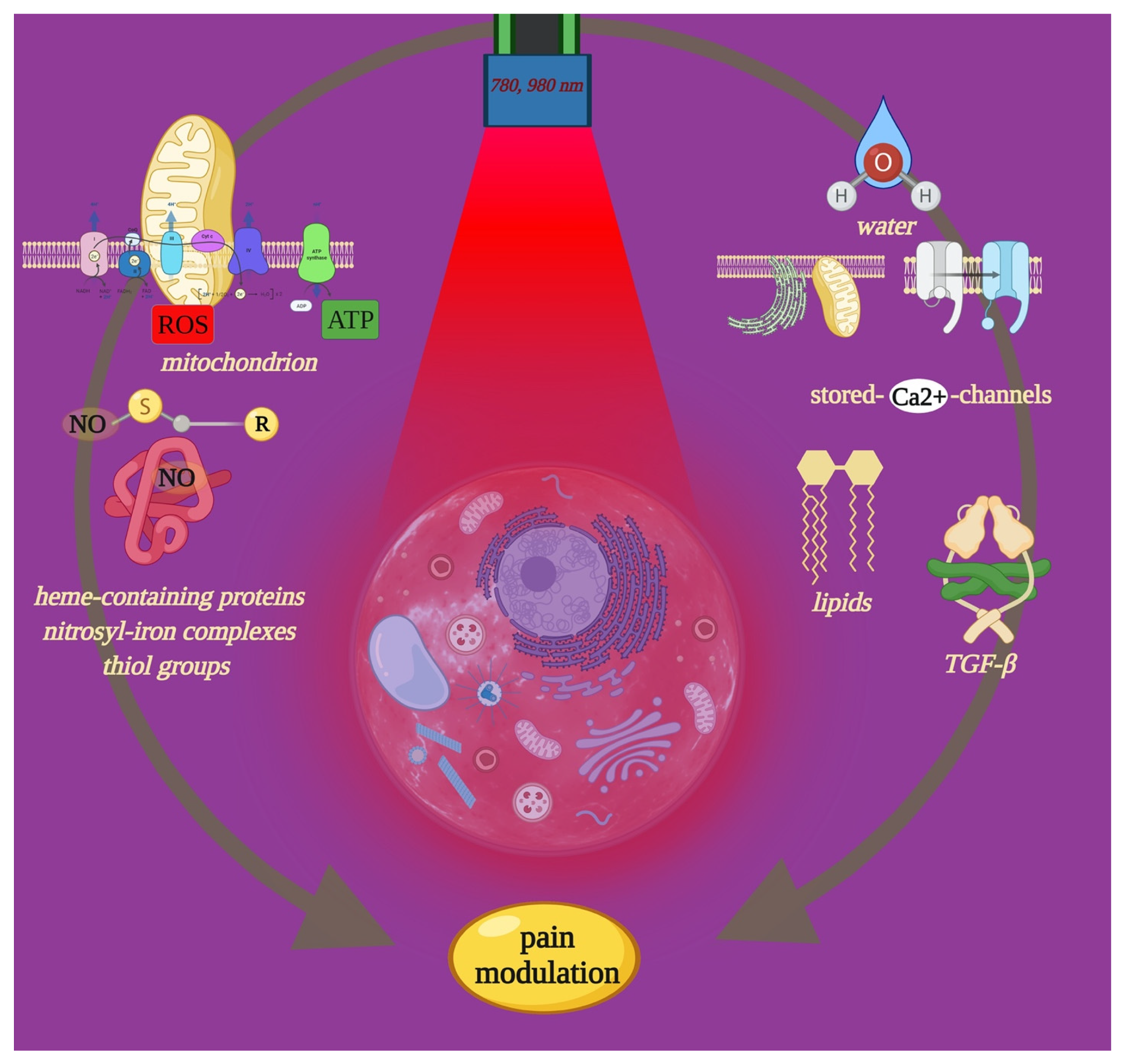
2.1. Effect of PBM-t on Cell Pathways of Pain
2.2. Influencing Pain Recovery through PBM-t
The main differences were related to the laser parameters according to the dose-dependency for the treatment and the irradiation time. All of the included studies used continuous wave mode with no thermal relaxation except Madani [40], which adopted the gated mode characterized by a thermal relaxation time (TRT). However, TRT is not an important factor in PBM therapy, as this treatment has no appreciable thermal effects in the irradiated area due to the low-power parameter values used [41]. The power values in the included studies ranged from 0.04 W [42][43], 0.07 W [44], 0.1 W [45][46], and 0.3 W [47] up to 0.6 W [48].
Moreover, the irradiation time was not consistent among the studies. Refs. [40][42][44][46] stated the total time irradiation for each session, while refs. [43][45][48] provided the irradiation time for each trigger point. Sancakli [47] talked about the irradiation time without clarifying whether the corresponding values were the total processing time or the time per trigger point. In studies [40][42][43][44][45][48], the laser light beam was applied in contact mode. Studies [46][47] followed a non-contact protocol with a tip-to-tissue distance of 2 mm [47], while ref. [46] lacked to give any measurement. Consequently, the dose of energy density varied among studies and ranged between the least applied dose of 3 J/cm2 [47] and the highest applied dose of 100 J/cm2 [44]. In addition, the included studies did not specify in detail whether the fluences stated in their studies represented the total amount of energy density that was delivered to all the treated areas or the dose amount applied for each trigger point. Therefore, all this may present a distorted picture of the effectiveness of the applied dose. It is well-established that PBM is dependent on the dose delivered to the treated area [41]. The dose itself is dependent on the amount of energy delivered to the treated area at a certain time and through various delivery systems. Different dosages lead to different cellular responses and subsequently different clinical outcomes [10]. In addition, “if the power doubled and the time is halved, then the same energy is delivered but a different biological response is often observed” [11]. For deeper components such as TMJ, both the parameters and the procedure therapy description become mandatory. Thus, it is crucial to understand how much energy density should be applied to the skin to obtain this range of 4–10 J/cm2 at the cellular level, where the main problem exists, and taking into consideration the dramatical attenuation of light photonic energy as it crosses tissue multiple divergent layers. The Beer–Lambert law usually defines such a relationship. Additionally, none of the included studies mentioned any details about the beam profile characteristics, vitiating the therapy reproducibility of the selected studies. Indeed, the amount of energy density delivered into the treated area is closely related to the beam profile. With a conventional laser handpiece, the spatial beam profile is inherently Gaussian, and generally, as the tip-to-tissue distance increases, the energy density decreases [6]. These variables appear to be the main challenge for the PBM researchers and are key factors to take into consideration in PBM studies in the precision medicine field [49].
References
- Butts, R.; Dunning, J.; Perreault, T.; Mettille, J.; Escaloni, J. Pathoanatomical characteristics of temporomandibular dysfunction: Where do we stand? Narrative review. J. Bodyw. Mov. Ther. 2017, 21, 534–540.
- Liu, F.; Steinkeler, A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent. Clin. N. Am. 2013, 57, 465–479.
- Mercuri, L.G. Management of temporomandibular joint disorders. J. Oral. Biol. Craniofac. Res. 2012, 2, 141–142.
- Abdel Hamid, M.A.; Hassan, E.A.; Zaied, A.A.; Amaroli, A.; Sorour, N.H. Dose-Dependent Clinical, Radiographic, and Histopathologic Changes of 17β-Estradiol Levels within the Temporomandibular Joint: An Experimental Study in Ovariectomized Dogs. J. Oral. Maxillofac. Surg. 2020, 78, 1304–1313.
- Maia, M.L.; Bonjardim, L.R.; de Quintans, J.S.; Ribeiro, M.A.; Maia, L.G.; Conti, P.C. Effect of Low-Level Laser Therapy on pain levels in patients with temporomandibular disorders: A systematic review. J. Appl. Oral. Sci. 2012, 20, 594–602.
- Amaroli, A.; Colombo, E.; Zekiy, A.; Aicardi, S.; Benedicenti, S.; De Angelis, N. Interaction between Laser Light and Osteoblasts: Photobiomodulation as a Trend in the Management of Socket Bone Preservation—A Review. Biology 2020, 9, 409.
- De Freitas, L.F.; Hamblin, M.R. Proposed Mechanism of Photobiomodulation or Low-Level Light Therapy. Sel. Top. Quantum Electron. 2016, 22, 7000417.
- Hamblin, M.R. Photobiomodulation or Low-Level Laser Therapy. J. Biophotonics 2016, 9, 1122–1124.
- Amaroli, A.; Ravera, S.; Zekiy, A.; Benedicenti, S.; Pasquale, C. A Narrative Review on Oral and Periodontal Bacteria Microbiota Photobiomodulation, through Visible and Near-Infrared Light: From the Origins to Modern Therapies. Int. J. Mol. Sci. 2022, 25, 1372.
- Amaroli, A.; Ravera, S.; Parker, S.; Panfoli, I.; Benedicenti, A.; Benedicenti, S. An 808-nm Diode Laser with a Flat-Top Handpiece Positively Photobiomodulates Mitochondria Activities. Photomed. Laser Surg. 2016, 34, 564–571.
- Amaroli, A.; Ravera, S.; Parker, S.; Panfoli, I.; Benedicenti, A.; Benedicenti, S. 808-nm laser therapy with a flat-top handpiece photobiomodulates mitochondria activities of Paramecium primaurelia (Protozoa). Lasers Med. Sci. 2016, 31, 741–747.
- Amaroli, A.; Pasquale, C.; Zekiy, A.; Utyuzh, A.; Benedicenti, S.; Signore, A.; Ravera, S. Photobiomodulation and Oxidative Stress: 980 nm Diode Laser Light Regulates Mitochondrial Activity and Reactive Oxygen Species Production. Oxidative Med. Cell Longev. 2021, 3, 6626286.
- Pastore, D.; Greco, M.; Passarella, S. Specific helium-neon laser sensitivity of the purified cytochrome c oxidase. Int. J. Radiat. Biol. 2000, 76, 863–870.
- Colombo, E.; Signore, A.; Aicardi, S.; Zekiy, A.; Utyuzh, A.; Benedicenti, S.; Amaroli, A. Experimental and Clinical Applications of Red and Near-Infrared Photobiomodulation on Endothelial Dysfunction: A Review. Biomedicines 2021, 9, 274.
- Wang, Y.; Huang, Y.Y.; Wang, Y.; Lyu, P.; Hamblin, M.R. Photobiomodulation of human adipose-derived stem cells using 810 nm and 980 nm lasers operates via different mechanisms of action. Biochim. Biophys. Acta Gen. Subj. 2017, 1861, 441–449.
- Amaroli, A.; Ferrando, S.; Benedicenti, S. Photobiomodulation Affects Key Cellular Pathways of all Life-Forms: Considerations on Old and New Laser Light Targets and the Calcium Issue. Photochem. Photobiol. 2019, 95, 455–459.
- Ferrando, S.; Agas, D.; Mirata, S.; Signore, A.; De Angelis, N.; Ravera, S.; Utyuzh, A.S.; Parker, S.; Sabbieti, M.G.; Benedicenti, S.; et al. The 808 nm and 980 nm infrared laser irradiation affects spore germination and stored calcium homeostasis: A comparative study using delivery hand-pieces with standard (Gaussian) or flat-top profile. J. Photochem. Photobiol. 2019, 199, 111627.
- Jansen, K.; Wu, M.; van der Steen, A.F.; van Soest, G. Photoacoustic imaging of human coronary atherosclerosis in two spectral bands. Photoacoustics 2013, 2, 12–20.
- Amaroli, A.; Marcoli, M.; Venturini, A.; Passalacqua, M.; Agnati, L.F.; Signore, A.; Raffetto, M.; Maura, G.; Benedicenti, S.; Cervetto, C. Near-infrared laser photons induce glutamate release from cerebrocortical nerve terminals. J. Biophotonics 2018, 11, 201800102.
- Bashkatov, A.; Genina, E.; Kochubey, V.; Tuchin, V. Optical properties of human skin, subcutaneous and mucous tissues in the wavelength range from 400 to 2000 nm. J. Phys. D Appl. Phys. 2005, 38, 2543–2555.
- Sui, B.D.; Xu, T.Q.; Liu, J.W.; Wei, W.; Zheng, C.X.; Guo, B.L.; Wang, Y.Y.; Yang, Y.L. Understanding the role of mitochondria in the pathogenesis of chronic pain. Postgrad. Med. J. 2013, 89, 709–714.
- Hamilton, S.G. ATP and pain. Pain Pract. 2002, 2, 289–294.
- Ryan, L.M.; Rachow, J.W.; McCarty, D.J. Synovial fluid ATP: A potential substrate for the production of inorganic pyrophosphate. J. Rheumatol. 1991, 18, 716–720.
- Wang, Z.Q.; Porreca, F.; Cuzzocrea, S. A newly identified role for superoxide in inflammatory pain. J. Pharmacol. Exp. Ther. 2004, 309, 869–878.
- Zheng, J.; Zhang, J.; Zhang, X.; Guo, Z.; Wu, W.; Chen, Z.; Li, J. Reactive Oxygen Species Mediate Low Back Pain by Upregulating Substance P in Intervertebral Disc Degeneration. Oxid. Med. Cell. Longev. 2021, 2021, 6681815.
- Chung, J.M. The role of reactive oxygen species (ROS) in persistent pain. Mol. Interv. 2004, 4, 248–250.
- Passarella, S.; Casamassima, E.; Molinari, S.; Pastore, D.; Quagliariello, E.; Catalano, I.M.; Cingolani, A. Increase of proton electrochemical potential and ATP synthesis in rat liver mitochondria irradiated in vitro by helium-neon laser. FEBS Lett. 1984, 175, 95–99.
- Pastore, D.; Greco, M.; Petragallo, V.A.; Passarella, S. Increase in <--H+/e− ratio of the cytochrome c oxidase reaction in mitochondria irradiated with helium-neon laser. Biochem. Mol. Biol. Int. 1994, 34, 817–826.
- Gonçalves de Faria, C.M.; Ciol, H.; Salvador Bagnato, V.; Pratavieira, S. Effects of photobiomodulation on the redox state of healthy and cancer cells. Biomed. Opt. Express. 2021, 12, 3902–3916.
- Ravera, S.; Bertola, N.; Pasquale, C.; Bruno, S.; Benedicenti, S.; Ferrando, S.; Zekiy, A.; Arany, P.; Amaroli, A. 808-nm Photobiomodulation Affects the Viability of a Head and Neck Squamous Carcinoma Cellular Model, Acting on Energy Metabolism and Oxidative Stress Production. Biomedicines 2021, 9, 1717.
- Amaroli, A.; Ravera, S.; Baldini, F.; Benedicenti, S.; Panfoli, I.; Vergani, L. Photobiomodulation with 808-nm diode laser light promotes wound healing of human endothelial cells through increased reactive oxygen species production stimulating mitochondrial oxidative phosphorylation. Lasers Med. Sci. 2019, 34, 495–504.
- Fernyhough, P.; Nigel Calcutt, A. Abnormal calcium homeostasis in peripheral neuropathies. Cell Calcium 2010, 47, 130–139.
- Zheng, J. Molecular mechanism of TRP channels. Compr. Physiol. 2013, 3, 221–242.
- Amaroli, A.; Benedicenti, A.; Ferrando, S.; Parker, S.; Selting, W.; Gallus, L.; Benedicenti, S. Photobiomodulation by Infrared Diode Laser: Effects on Intracellular Calcium Concentration and Nitric Oxide Production of Paramecium. Photochem. Photobiol. 2016, 92, 854–862.
- Miclescu, A.; Torsten, G. Nitric oxide and pain: ‘Something old, something new’. Acta Anaesthesiol. Scand. 2009, 53, 1107–1120.
- Koch, A.; Zacharowski, K.; Boehm, O. Nitric oxide and pro-inflammatory cytokines correlate with pain intensity in chronic pain patients. Inflamm. Res. 2007, 56, 32–37.
- Lantero, A.; Tramullas, M.; Díaz, A. Transforming Growth Factor-β in Normal Nociceptive Processing and Pathological Pain Models. Mol. Neurobiol. 2012, 45, 76–86.
- Amaroli, A.; Agas, D.; Laus, F.; Cuteri, V.; Hanna, R.; Sabbieti, M.G.; Benedicenti, S. The Effects of Photobiomodulation of 808 nm Diode Laser Therapy at Higher Fluence on the in Vitro Osteogenic Differentiation of Bone Marrow Stromal Cells. Front. Physiol. 2018, 23, 123.
- Khan, I.; Rahman, S.U.; Tang, E. Accelerated burn wound healing with photobiomodulation therapy involves activation of endogenous latent TGF-β1. Sci. Rep. 2021, 11, 13371.
- Madani, A.S.; Ahrari, F.; Nasiri, F.; Abtahi, M.; Tunér, J. Low-level laser therapy for management of TMJ osteoarthritis. Cranio 2014, 32, 38–44.
- Kim, H.B.; Baik, K.Y.; Choung, P.H.; Chung, J.H. Pulse frequency dependency of photobiomodulation on the bioenergetic functions of human dental pulp stem cells. Sci. Rep. 2017, 7, 15927.
- Salmos-Brito, J.A.; de Menezes, R.F.; Teixeira, C.E.; Gonzaga, R.K.; Rodrigues, B.H.; Braz, R.; Bessa-Nogueira, R.V.; Gerbi, M.E. Evaluation of Low-Level Laser Therapy in patients with acute and chronic temporomandibular disorders. Lasers Med. Sci. 2013, 28, 57–64.
- Mazzetto, M.O.; Hotta, T.H.; Pizzo, R.C. Measurements of jaw movements and TMJ pain intensity in patients treated with GaAlAs laser. Braz. Dent. J. 2010, 21, 356–360.
- Da Silva, M.A.; Botelho, A.L.; Turim, C.V.; da Silva, A.M. Low level laser therapy as an adjunctive technique in the management of temporomandibular disorders. Cranio 2012, 30, 264–271.
- De Moraes Maia, M.L.; Ribeiro, M.A.; Maia, L.G.; Stuginski-Barbosa, J.; Costa, Y.M.; Porporatti, A.L.; Conti, P.C.; Bonjardim, L.R. Evaluation of Low-Level Laser Therapy effectiveness on the pain and masticatory performance of patients with myofascial pain. Lasers Med. Sci. 2014, 29, 29–35.
- Shobha, R.; Narayanan, V.S.; Jagadish Pai, B.S.; Jaishankar, H.P.; Jijin, M.J. Low-level laser therapy: A novel therapeutic approach to temporomandibular disorder—A randomized, double-blinded, placebo-controlled trial. Indian J. Dent. Res. 2017, 28, 380–387.
- Sancakli, E.; Gökçen-Röhlıg, B.; Balık, A.; Öngül, D.; Kıpırdı, S.; Keskın, H. Early results of low-level laser application for masticatory muscle pain: A double-blind randomized clinical study. BMC Oral. Health 2015, 15, 131.
- Sayed, N.; Murugavel, C.; Gnanam, A. Management of Temporomandibular Disorders with Low Level Laser Therapy. J. Maxillofac. Oral. Surg. 2014, 13, 444–450.
- Sommer, A.P.; Pinheiro, A.L.; Mester, A.R.; Franke, R.P.; Whelan, H.T. Biostimulatory windows in low-intensity laser activation: Lasers, scanners, and NASA’s light-emitting diode array system. J. Clin. Laser Med. Surg. 2001, 19, 29–33.
- Parker, S.; Cronshaw, M.; Anagnostaki, E.; Bordin-Aykroyd, S.R.; Lynch, E. Systematic Review of Delivery Parameters Used in Dental Photobiomodulation Therapy. Photobiomodul. Photomed. Laser Surg. 2019, 37, 784–797.




