Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Aspasia Pachiou | -- | 1740 | 2022-07-26 09:29:23 | | | |
| 2 | Lindsay Dong | -6 word(s) | 1734 | 2022-07-27 03:48:53 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Roulias, P.; Kalantzis, N.; Doukaki, D.; Pachiou, A.; Karamesinis, K.; Damanakis, G.; Gizani, S.; Tsolakis, A.I. Teeth Eruption Disorders. Encyclopedia. Available online: https://encyclopedia.pub/entry/25513 (accessed on 28 February 2026).
Roulias P, Kalantzis N, Doukaki D, Pachiou A, Karamesinis K, Damanakis G, et al. Teeth Eruption Disorders. Encyclopedia. Available at: https://encyclopedia.pub/entry/25513. Accessed February 28, 2026.
Roulias, Panagiotis, Nikolaos Kalantzis, Dafni Doukaki, Aspasia Pachiou, Konstantinos Karamesinis, George Damanakis, Sotiria Gizani, Apostolos I. Tsolakis. "Teeth Eruption Disorders" Encyclopedia, https://encyclopedia.pub/entry/25513 (accessed February 28, 2026).
Roulias, P., Kalantzis, N., Doukaki, D., Pachiou, A., Karamesinis, K., Damanakis, G., Gizani, S., & Tsolakis, A.I. (2022, July 26). Teeth Eruption Disorders. In Encyclopedia. https://encyclopedia.pub/entry/25513
Roulias, Panagiotis, et al. "Teeth Eruption Disorders." Encyclopedia. Web. 26 July, 2022.
Copy Citation
Dental eruption refers to the vertical displacement of a tooth from its initial non-functional towards its functional position. Tooth eruption disorders may be expressed in various clinical conditions, which may be grouped as “primary retention” and “secondary retention”. Tooth eruption disorders can be manifested in several clinical conditions where the oral location, the number of the affected teeth, and the etiology of the disorders vary considerably. Eruption failure is often attributed to genetic factors.
primary failure of eruption
PFE
ankylosis
tooth eruption disorders
1. Introduction
Dental eruption constitutes the physiologic process where a tooth is vertically displaced from its initial non-functional, developmental position towards its functional position, emerging through the bone of the alveolar process and the mouth epithelium, in order to occlude with its antagonist. This process is triggered by the formation of the periodontal ligament [1].
The physiological eruption procedure of one or more teeth is likely to be disrupted by local or genetic factors. Due to the slow rate of the tooth eruption and the fact that access to this ongoing process is deemed challenging, the exact procedure remains unclear [1]. A variety of syndromes involving eruption failure have been mentioned, among which cleidocranial dysplasia, Gardner syndrome, osteoglophonic dwarfism, regional odontodysplasia, oculodental syndrome, Rutherfurd type, Nance–Horan syndrome, Cherubism, Albers-Schönberg osteopetrosis, McCune–Albright syndrome, hypodontia–dysplasia of nails syndrome, osteopetrosis, mucopolysaccharidosis, and GAPO syndrome [2]. In cleidocranial dysplasia patients, a combination of delayed tooth eruption and a high bone width of the upper and the lower arches was observed. In these patients, the paracrine signal for bone remodeling could account for the incomplete tooth eruption [3].
2. Eruption Failure
A non-normal tooth eruption path may occur from the presence of a given mechanical obstacle (with idiopathic or pathological origin) or as a result of the disruption of the tooth eruption mechanism itself [4]. The tooth eruption process involves a synchronized procedure where consecutive signaling events take place between the tooth pocket and the osteoblast and osteoclast cells of the alveolar process [5]. A disorder caused or not by a syndrome (of genetic or otherwise origin) might lead to the disruption of the aforementioned process, manifested either as a delayed eruption [6] or a complete eruption failure [7]. Eruption failure has been detected in either a single tooth or multiple teeth in both the primary and the permanent dentition and may also be partial or complete [8]. Apart from these factors, the eruption process of a permanent tooth could also be affected by genetic factors since numerous syndromes are found to give rise to similar clinical conditions where any genes responsible have already been discovered.
Tooth eruption failure may be referred to as either primary retention or as secondary retention [4]. Diagnosis of the initial eruption discontinuation concerns the local failure of a tooth to erupt without necessitating the coexistence of any other local or systematic factor. There has been an association between initial tooth eruption failure and idiopathic eruption failure [7]. Secondary retention refers to teeth that, although existing in the oral cavity, have manifested as an incomplete eruption [4][8].
3. Primary Retention
The phenomenon where molars cease to erupt before they emerge, without a physical barrier in the eruption path or as a consequence of an atypical location, is defined as primary retention. The alveolar support of a primarily retained molar, which does not resorb occlusally, is considered a normal barrier to the eruption path. Primary retention is similar to “unerupted” and “embedded” teeth [9]. In the event that the eruption of a permanent tooth is at least 2 years delayed compared to what is normally expected, primary retention should be a clinical entity to take into account. A radiographical follow-up of a minimum of 6 months is suggested as an initial control to determine whether the tooth is showing any eruptive movement or not [10]. The suggested radiographic methods include a periapical or even panoramic X-ray. Primary retention is the possible result of a disturbance in the dental follicle that does not succeed in initiating the metabolic events responsible for bone resorption in the eruption traject [11] (Figure 1 and Figure 2).
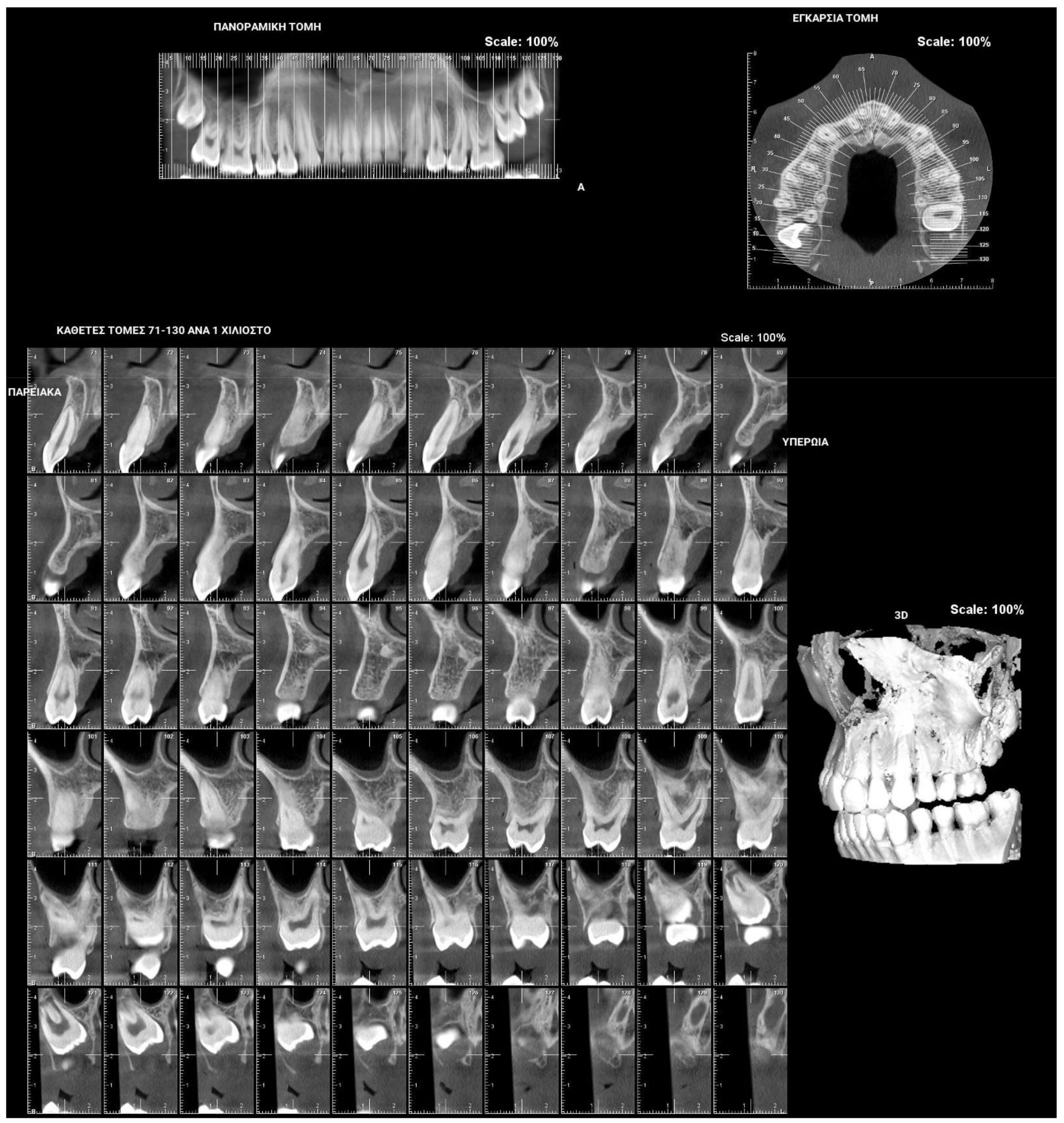
Figure 1. Patient presenting eruption failure of the upper left second molar due to primary retention.
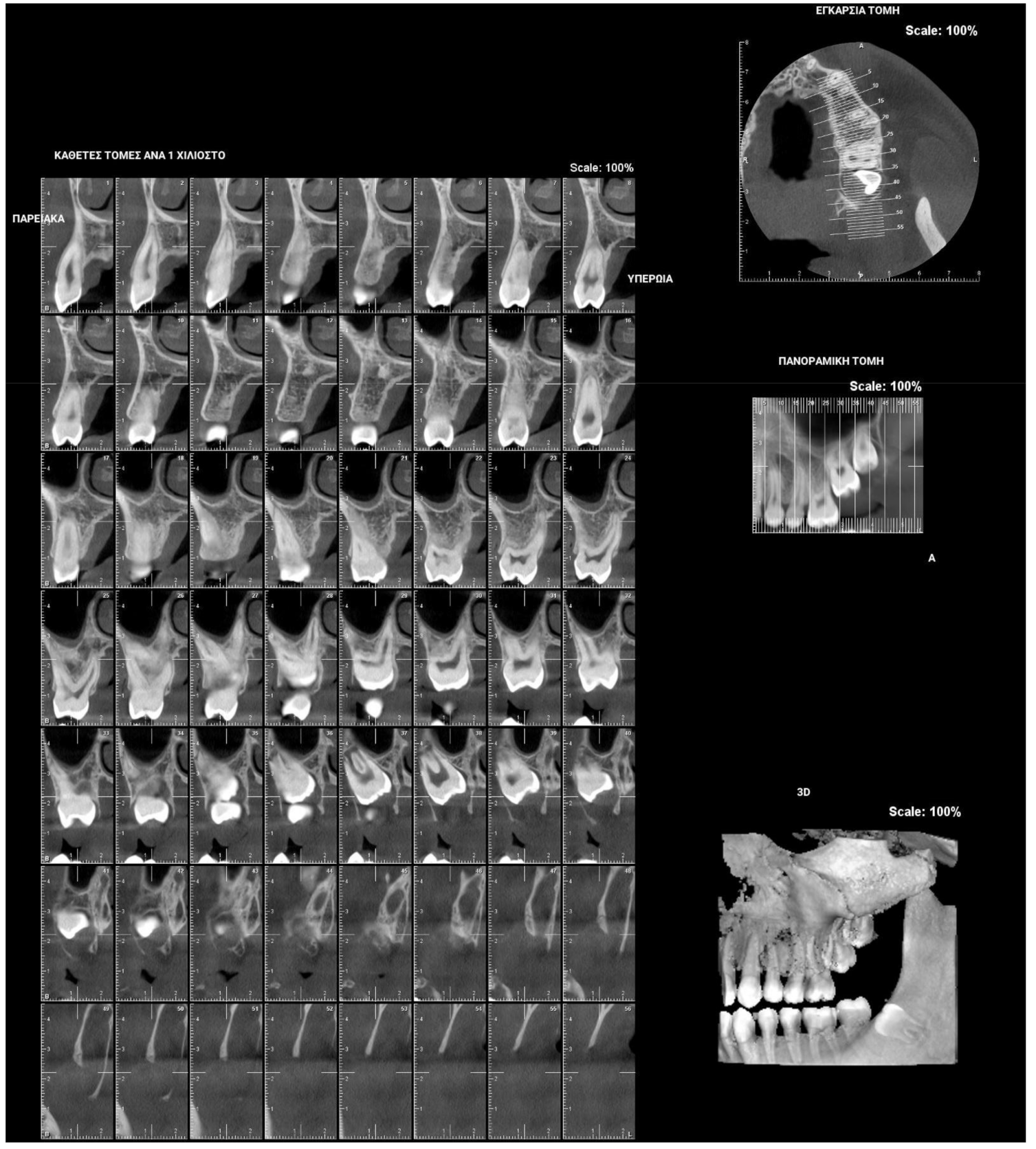
Figure 2. Patient presenting eruption failure of the upper left second molar due to primary retention.
4. Secondary Retention
Secondary retention is the phenomenon where the eruption process stalls after the tooth has emerged without the evidence of a physical barrier in the eruption path or as a result of an abnormal position [12][13]. The etiology of secondary retention still remains unclear. It takes place when the tooth is still submerged or during the eruption process and always involves the first 2 mm of the radicular neck or the molar furcation region, i.e., the area that separates the attachment cord from the follicular sac and the anatomic neck, a region approximately 2 mm wide. As soon as ankylosis between the tooth and osseous support has taken place, not only the eruption but also the growth of the alveolar process in the influenced area is inhibited. The adjacent teeth carry on erupting and, as a consequence, the affected tooth is infraoccluded. This might lead to malocclusion, particularly after the inclination of the adjacent teeth towards the space [4].
Clinically secondary retention is often assumed when a molar is in infraocclusion at a time period when the tooth should typically be in occlusion. The probability of ankylosis can be recognized via a percussion test and radiographic examination of the periodontal ligament obliteration. Nevertheless, such diagnostic means do not always prove reliable due to the fact that the ankylosed area in secondary retention is usually difficult to observe [12] (Figure 3).
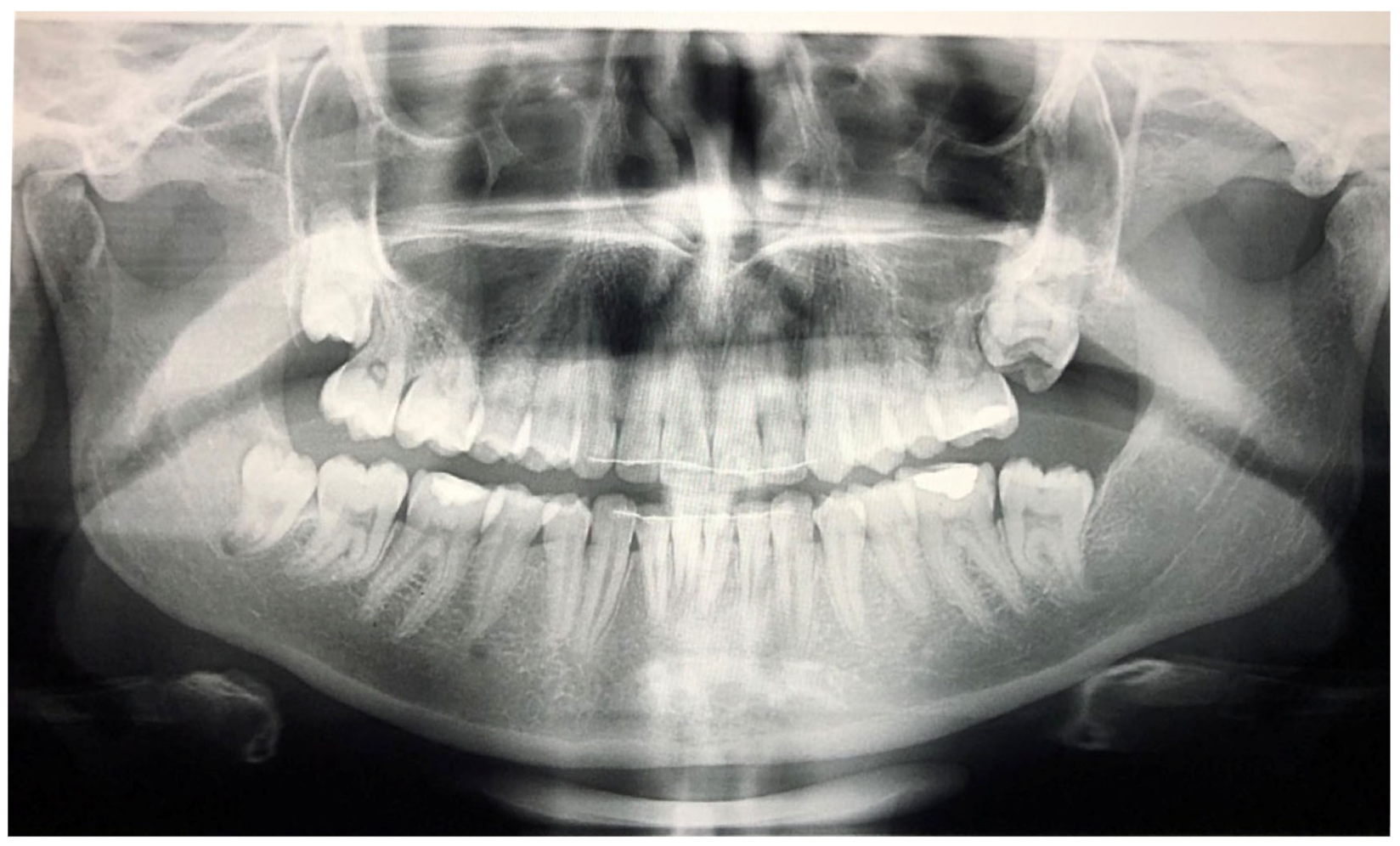
Figure 3. Patient after finishing the orthodontic treatment, presenting secondary retention due to fusion of the upper left second and third molars.
5. Primary Failure of Eruption (PFE)
“Primary Failure of Eruption” (PFE) is the clinical condition that is associated with failure during the tooth eruption process. Primary Failure of Eruption may present a number of the following characteristics: (1) a higher frequency of appearance in the posterior teeth area rather than in the anterior region, (2) the teeth may begin to erupt towards occlusion and stop erupting halfway through the process, (3) both primary and permanent molars may exhibit such a clinical condition, (4) this clinical condition may be spotted on either one side or both sides in the mouth, (5) permanent teeth with such a condition are likely to be ankylosed, (6) the application of any orthodontic force may result in tooth ankylosis, and (7) this clinical condition may be present without any relevant family history [7].
PFE attributes combine elements that resemble both primary and secondary retention (Figure 4). The diagnosis of PFE is impeded to a great extent by the complexity of this clinical picture (Figure 5 and Figure 6). It appears that this clinical condition has two different mechanisms or two different aspects of the same mechanism since the tooth may erupt in its initial position and thereafter stop its further eruption (a clinical condition known as secondary retention) [7][8][14], or the tooth may not be able to erupt at all [11]. In this context, a definitive diagnosis of PFE cannot easily be decided, as it is possible that PFE presents two separate mechanisms [11] or two independent manifestations of the same mechanism. Only if scholars were to examine an environment where genetic, pathological, and environmental factors—all factors potentially responsible for the discontinuation of the tooth’s eruption—are absent would a PFE diagnosis through a retrospective examination be possible.

Figure 4. Patient’s orthopantomography presenting Primary Failure of Eruption in all four dental quadrants.

Figure 5. Right photo of the female patient with PFE in bite relationship.

Figure 6. Left photo of the same female patient depicted in Figure 5.
6. Clinical Characteristics of PFE
The variability in the clinical figure of PFE appears to have a genetic background and depends on the moment the defect of the tooth eruption occurs (which is also governed by genetic factors).
PFE is described as occurring in two distinct types: Type I is observed when a progressive open bite from the anterior towards the posterior area of the dental arches is established. It seems that in this case, the defect in the eruption process occurs in all the relative teeth simultaneously. In Type II, a progressive open bite from the anterior towards the posterior part is also observed, but the clinical expressions vary in multiple quadrants of the mouth, and the second molars erupt further but not sufficiently. It seems that in this case, a sequence of molecular events takes place, thus affecting the alveolar process in the posterior region more than in the anterior segment in terms of time and location [6]. Whenever Type I and II PFE are simultaneously present, a Type III PFE can be described [2].
7. Differential Diagnosis of Teeth Eruption Disorders
The common element for any differential diagnosis among single ankylosis, secondary retention, and PFE is the occlusal relationship (if it is normal or not) between the upper and the lower teeth posteriorly, with the first molar being the most likely not to have fully erupted. PFE is more likely to be present if a family history in conjunction with the mutated PTH1R gene are also present. In cases where PFE is present, the affected teeth are expected to not respond to any orthodontic treatment. If a patient is believed to have PFE, a genetic test for a mutation in the PTH1R gene should be recommended before any orthodontic therapy so as to prevent ankylosis. Therefore, a definite diagnosis based on the clinical description of PFE may not be easily reached. Careful consideration should be given to the existence of possible clinical manifestations, and an observation period would be advisable. If the presence of such symptoms persists, a further genetic background search would be advisable.
The therapeutic approach is determined by the patient’s age and the clinical status, and, as such, it needs to be evaluated individually [2]. Considering that ankylosis concerns a single tooth, therapy could comprise the extraction of the ankylosed tooth and the subsequent orthodontic treatment for the space closure management or a prosthetic rehabilitation [15]. Alternatively, a local osteotomy, as well as an orthodontic traction of the whole piece, could be performed since a harmonic occlusion of the tooth may be achieved. In the event of the tooth’s partial eruption, the vertical dimension of the tooth in question could be regained by having its crown restored. When more than one tooth is affected, the treatment becomes increasingly challenging, and partial osteotomy is the preferred treatment approach [7].
References
- Proffit, W.R.; Frazier-Bowers, S.A. Mechanism and control of tooth eruption: Overview and clinical implications. Orthod. Craniofacial Res. 2009, 12, 59–66.
- Hanisch, M.; Hanisch, L.; Kleinheinz, J.; Jung, S. Primary failure of eruption (PFE): A systematic review. Head Face Med. 2018, 14, 5.
- Dorotheou, D.; Gkantidis, N.; Karamolegkou, M.; Kalyvas, D.; Kiliaridis, S.; Kitraki, E. Tooth eruption: Altered gene expression in the dental follicle of patients with cleidocranial dysplasia. Orthod. Craniofacial Res. 2012, 16, 20–27.
- Raghoebar, G.M.; Boering, G.; Vissink, A.; Stegenga, B. Eruption disturbances of permanent molars: A review. J. Oral Pathol. Med. 1991, 20, 159–166.
- Wise, G.E.; King, G.J. Mechanisms of Tooth Eruption and Orthodontic Tooth Movement. J. Dent. Res. 2008, 87, 414–434.
- Suri, L.; Gagari, E.; Vastardis, H. Delayed tooth eruption: Pathogenesis, diagnosis, and treatment. A literature review. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 432–445.
- Proffit, W.R.; Vig, K.W. Primary failure of eruption: A possible cause of posterior open-bite. Am. J. Orthod. 1981, 80, 173–190.
- Raghoebar, G.M.; Boering, G.; Vissink, A. Clinical, radiographic and histological characteristics of secondary retention of permanent molars. J. Dent. 1991, 19, 164–170.
- Shafer, W.G.; Hine, M.K.; Levy, B.M. A Textbook of Oral Pathology, 4th ed.; West Washington Square, WB Saunders Company: Philadelphia, PA, USA, 1983; pp. 66–69.
- Kracke, R.R. Delayed tooth eruption versus impaction. J. Dent. Child. 1975, 42, 371–374.
- Oliver, R.G.; Richmond, S.; Hunter, B. Submerged permanent molars: Four case reports. Br. Dent. J. 1986, 160, 128–130.
- Raghoebar, G.M.; Boering, G.; Jansen, H.; Vissink, A. Secondary retention of permanent molars: A histologic study. J. Oral Pathol. Med. 1989, 18, 427–431.
- Raghoebar, G.M.; Van Koldam, W.A.; Boering, G. Spontaneous reeruption of a secondarily retained permanent lower molar and an unusual migration of a lower third molar. Am. J. Orthod. Dentofac. Orthop. 1990, 97, 82–84.
- Hall, G.M.; Reade, P.C. Quadrilateral submersion of permanent teeth. Brief review and case report. Aust. Dent. J. 1981, 26, 73–76.
- Frazier-Bowers, S.A.; Simmons, D.; Wright, J.T.; Proffit, W.R.; Ackerman, J.L. Primary failure of eruption and PTH1R: The importance of a genetic diagnosis for orthodontic treatment planning. Am. J. Orthod. Dentofacial Orthop. 2010, 137, 160–167.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
2.6K
Revisions:
2 times
(View History)
Update Date:
27 Jul 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





