Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Giovanni Ferrandino | -- | 919 | 2022-06-28 15:01:15 | | | |
| 2 | Nora Tang | + 59 word(s) | 978 | 2022-06-29 07:42:51 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Liguori, C.; Tamburrini, S.; Ferrandino, G.; Leboffe, S.; Rosano, N.; Marano, I. Acute Coronary Syndrome. Encyclopedia. Available online: https://encyclopedia.pub/entry/24583 (accessed on 07 February 2026).
Liguori C, Tamburrini S, Ferrandino G, Leboffe S, Rosano N, Marano I. Acute Coronary Syndrome. Encyclopedia. Available at: https://encyclopedia.pub/entry/24583. Accessed February 07, 2026.
Liguori, Carlo, Stefania Tamburrini, Giovanni Ferrandino, Silvio Leboffe, Nicola Rosano, Ines Marano. "Acute Coronary Syndrome" Encyclopedia, https://encyclopedia.pub/entry/24583 (accessed February 07, 2026).
Liguori, C., Tamburrini, S., Ferrandino, G., Leboffe, S., Rosano, N., & Marano, I. (2022, June 28). Acute Coronary Syndrome. In Encyclopedia. https://encyclopedia.pub/entry/24583
Liguori, Carlo, et al. "Acute Coronary Syndrome." Encyclopedia. Web. 28 June, 2022.
Copy Citation
Acute coronary syndrome (ACS) refers to a group of diseases in which blood flow to the heart is decreased. It is a manifestation of CHD (coronary heart disease) which usually results in plaque disruption in the coronary arteries (atherosclerosis) and the formation of thrombus. In some cases, ACS may be due to vasospasm with or without underlying atherosclerosis, but in both cases it determines a reduction in blood flow to a part of the heart, resulting first in ischemia and then infarction.
cardiac radiology
cardiac-CT
cardiac MRI
CT angiography
acute coronary syndrome
1. Introduction
ACS includes several conditions: ST-segment elevation myocardial infarction (STEMI), non-ST-segment elevation myocardial infarction (NSTEMI), and unstable angina, and it is responsible for one third of total deaths in people older than 35 [1].
In patients with suspected ACS, it will first be necessary to classify the patient in one of the two major sub-categories (STEMI and NSTEMI) and subsequently to distinguish the N-STEMI subtype (N-STEMI and unstable angina). STEMI is representative of an acute myocardial infarction with evidence of myocardial necrosis. Most of the patients presenting with ischemic symptoms and persistent ST-segment elevation on the electrocardiogram (ECG) > 20 min will show a typical rise in biomarkers of myocardial necrosis and progress to Q-wave myocardial infarction [2]. Patients with acute chest pain but no persistent ST-segment elevation may have a variety of ECG abnormalities such as transient ST-segment elevation, persistent or transient ST-segment depression, inversion of the T wave, flat T waves, or pseudo-normalization of the T waves up to a normal ECG. Cardiomyocyte necrosis [myocardial infarction without ST-segment elevation (NSTEMI)] or, less frequently, myocardial ischemia without cell damage (unstable angina) may be observed in the myocardium [3].
2. Suspected Acute Coronary Syndrome
In patients with a high risk of ACS, a prompt invasive coronary angiography and/or revascularization should be performed to salvage the viable myocardium. In such a scenario, radiology techniques (CT or MRI) should not be employed, they should only be used in the post-treatment phase for assessing the extent of myocardial damage. In contrast, in patients with a low to moderate risk of ACS alongside the non-invasive clinical instrumental standard evaluation, radiological techniques and in particular CT can play a key role in making a faster diagnosis, compared to standard of care [4][5][6]. Standard protocol is associated with a long stay in the emergency room or coronary care unit waiting for any changes in the ECG or troponin to occur or waiting for stress tests, the results of which are emergency room overcrowding and an increase in cost. State-of-the-art CT scans (≥64 slices) can acquire images in moments, thereby reducing the possibility of artifacts and allowing the quick and reliable exclusion of ACS without ST-segment elevation by displaying the main coronary vessels and their main branches. The ROMICAT II and ACRIN studies have shown that CTA can lead to rapid and safe discharge from ED (47% vs. 12%, p < 0.001 and 49.6% vs. 22.7%, p < 0.001, respectively), reducing hospitalization times (8.6 h vs. 26.7 h, p < 0.001 and 18.0 h vs. 24.8 h, p < 0.001, respectively) and showing a better cost–benefit ratio than standard-of-care, thanks to the high negative predictive value of the CTA (excluding coronary stenosis > 50%) [7][8]. The main advantage of coronary CT is the possibility to evaluate the vessel wall with consequent plaque characterization. CT can also exclude or detect any serious complications of acute myocardial infarction (pulmonary edema and acute mitral regurgitation, due to the ischemic involvement of the papillary muscles, ventricular septal defect, free wall rupture, etc.) [9][10][11]. A type 1 acute myocardial infarction (AMI) is triggered by fissuring and the subsequent rupture of the vulnerable plaque, resulting in obstructive coronary stenosis or occlusion. Thus, a culprit lesion is often characterized at CT evaluation by a ≥70% stenosis with mixed or mainly noncalcified plaque [12]. A Type 2 AMI is caused by a mismatch of blood supply and demand. Type 2 AMI is often referred to as myocardial infarction with nonobstructive coronary arteries (MINOCA). In this context, cardiac-CT allows the evaluation of the presence of non-obstructive plaques (<50%) with vulnerable characteristics, as well as the presence of myocardial damage in the possible distribution area of the suspected lesion [5] (thanks to the acquisition of LIE-Late Iodine Enhancement). There are still major limitations related to available instruments, radiation dosage, and low positive predictive value in prognostic terms, especially in patients with calcifications, obesity and suboptimal heart rate. Coronary CT can identify coronary stenosis that is not functionally significant and decrease the number of coronary angiography procedures not followed by revascularization [13]. Theoretically, cardiac MRI is the ideal method for studying ACS. It allows not only the evaluation of myocardial perfusion and parietal motility abnormalities but the distinction between scar tissue and recent infarction. CMR, combining examination at rest and with stress can be used in acute chest pain that is suspected ACS. In clinical practice, in the emergency setting it carries very little application in the diagnostic phase [14] (Figure 1).
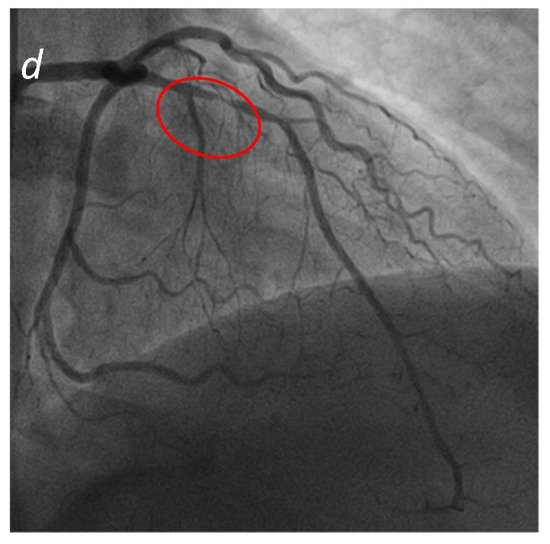
Figure 1. Acute Coronary Syndrome. A patient presenting to the emergency department with acute chest pain. No significant cardiac enzyme elevation and ECG alteration. Cardiac CTA shows absence of significant stenoses in the right coronary artery (a) and the left circumflex (b); a significant stenosis in the proximal anterior descending artery (c) is present, confirmed by subsequent coronary angiogram (d).
According to recent literature the integration of derived fractional flow reserve in CT (FFR-CT) studies using computational fluid dynamics gives the chance to enhance CT diagnostic accuracy. Moreover, in the emergency setting the use of FFR-CT allows a safer patient management thanks to the opportunity to detect, in the case of negative study, cardiac revascularization in chest pain patients. At the same time, it allows a significant reduction in medical cost [15].
Alternatively, it is now possible to combine a coronary CT angiography with myocardial CT perfusion to define the hemodynamic significance of a coronary stenosis. Combined stress CT perfusion and CTA are strictly correlated to a shortened period of hospitalization and lower costs [16].
References
- Singh, A.; Museedi, A.S.; Grossman, S.A. Acute coronary syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022.
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur. Heart J. 2018, 39, 119–177.
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthelemy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Rev. Esp. Cardiol. 2021, 74, 544.
- Lee, H.Y.; Yoo, S.M.; White, C.S. Coronary CT angiography in emergency department patients with acute chest pain: Triple rule-out protocol versus dedicated coronary CT angiography. Int. J. Cardiovasc. Imaging 2009, 25, 319–326.
- Yoo, S.M.; Jang, S.; Kim, J.A.; Chun, E.J. Troponin-positive non-obstructive coronary arteries and myocardial infarction with non-obstructive coronary arteries: Definition, etiologies, and role of CT and MR imaging. Korean J. Radiol. 2020, 21, 1305–1316.
- Yoo, S.M.; Rho, J.Y.; Lee, H.Y.; Song, I.S.; Moon, J.Y.; White, C.S. Current concepts in cardiac CT angiography for patients with acute chest pain. Korean Circ. J. 2010, 40, 543–549.
- Litt, H.I.; Gatsonis, C.; Snyder, B.; Singh, H.; Miller, C.D.; Entrikin, D.W.; Leaming, J.M.; Gavin, L.J.; Pacella, C.B.; Hollander, J.E. CT angiography for safe discharge of patients with possible acute coronary syndromes. N. Engl. J. Med. 2012, 366, 1393–1403.
- Hoffmann, U.; Truong, Q.A.; Schoenfeld, D.A.; Chou, E.T.; Woodard, P.K.; Nagurney, J.T.; Pope, J.H.; Hauser, T.H.; White, C.S.; Weiner, S.G.; et al. Coronary CT angiography versus standard evaluation in acute chest pain. N. Engl. J. Med. 2012, 367, 299–308.
- Moore, A.; Goerne, H.; Rajiah, P.; Tanabe, Y.; Saboo, S.; Abbara, S. Acute myocardial infarct. Radiol. Clin. N. Am. 2019, 57, 45–55.
- Kaul, U.A.; Singh, S.; Kalra, G.S.; Nair, M.; Mohan, J.C.; Nigam, M.; Arora, R. Mitral regurgitation following percutaneous transvenous mitral commissurotomy: A single-center experience. J. Heart Valve Dis. 2000, 9, 262–266; discussion 266–268.
- Figueras, J.; Cortadellas, J.; Soler-Soler, J. Left ventricular free wall rupture: Clinical presentation and management. Heart 2000, 83, 499–504.
- Son, M.J.; Yoo, S.M.; Lee, D.; Lee, H.Y.; Song, I.S.; Chun, E.J.; White, C.S. Current role of computed tomography in the evaluation of acute coronary syndrome. Diagnostics 2021, 11, 266.
- Nardi, F.; Pino, P.G.; Gabrielli, D.; Colivicchi, F.; Abrignani, M.G.; Amico, A.F.; Aspromonte, N.; Benedetto, F.A.; Bertella, E.; Boccardi, L.M.; et al. ANMCO/SICI-GISE/SIC/SIECVI/SIRM Consensus document: Appropriateness of multimodality imaging in cardiovascular disease. G. Ital. Cardiol. 2020, 21, 34–88.
- Rybicki, F.J.; Udelson, J.E.; Peacock, W.F.; Goldhaber, S.Z.; Isselbacher, E.M.; Kazerooni, E.; Kontos, M.C.; Litt, H.; Woodard, P.K. 2015 ACR/ACC/AHA/AATS/ACEP/ASNC/NASCI/SAEM/SCCT/SCMR/SCPC/SNMMI/STR/STS Appropriate utilization of cardiovascular imaging in emergency department patients with chest pain: A joint document of the American college of radiology appropriateness criteria committee and the American college of cardiology appropriate use criteria task force. J. Am. Coll. Cardiol. 2016, 67, 853–879.
- Chinnaiyan, K.M.; Safian, R.D.; Gallagher, M.L.; George, J.; Dixon, S.R.; Bilolikar, A.N.; Abbas, A.E.; Shoukfeh, M.; Brodsky, M.; Stewart, J.; et al. Clinical use of CT-derived fractional flow reserve in the emergency department. JACC Cardiovasc. Imaging 2020, 13, 452–461.
- Grandhi, G.R.; Batlle, J.C.; Maroules, C.D.; Janowitz, W.; Peña, C.S.; Ziffer, J.A.; Macedo, R.; Nasir, K.; Cury, R.C. Combined stress myocardial CT perfusion and coronary CT angiography as a feasible strategy among patients presenting with acute chest pain to the emergency department. J. Cardiovasc. Comput. Tomogr. 2021, 15, 129–136.
More
Information
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
828
Revisions:
2 times
(View History)
Update Date:
29 Jun 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




