Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Katarzyna Wilk-Śledziewska | -- | 1487 | 2022-05-06 13:30:48 | | | |
| 2 | Rita Xu | Meta information modification | 1487 | 2022-05-07 03:48:33 | | | | |
| 3 | Edyta Zbroch | Meta information modification | 1487 | 2024-01-11 21:10:39 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Wilk-Śledziewska, K.; Zbroch, E.; , .; Rosołowski, M.; Kakareko, K.; Sledziewski, R.; Rydzewska-Rosołowska, A.; Hryszko, T. Cardiovascular Risk Factors on the Course of COVID-19. Encyclopedia. Available online: https://encyclopedia.pub/entry/22660 (accessed on 07 February 2026).
Wilk-Śledziewska K, Zbroch E, , Rosołowski M, Kakareko K, Sledziewski R, et al. Cardiovascular Risk Factors on the Course of COVID-19. Encyclopedia. Available at: https://encyclopedia.pub/entry/22660. Accessed February 07, 2026.
Wilk-Śledziewska, Katarzyna, Edyta Zbroch, , Mariusz Rosołowski, Katarzyna Kakareko, Rafal Sledziewski, Alicja Rydzewska-Rosołowska, Tomasz Hryszko. "Cardiovascular Risk Factors on the Course of COVID-19" Encyclopedia, https://encyclopedia.pub/entry/22660 (accessed February 07, 2026).
Wilk-Śledziewska, K., Zbroch, E., , ., Rosołowski, M., Kakareko, K., Sledziewski, R., Rydzewska-Rosołowska, A., & Hryszko, T. (2022, May 06). Cardiovascular Risk Factors on the Course of COVID-19. In Encyclopedia. https://encyclopedia.pub/entry/22660
Wilk-Śledziewska, Katarzyna, et al. "Cardiovascular Risk Factors on the Course of COVID-19." Encyclopedia. Web. 06 May, 2022.
Copy Citation
The coronavirus disease 2019 (COVID-19) pandemic is spreading around the world and becoming a major public health crisis. All coronaviruses are known to affect the cardiovascular system. There is a strong correlation between cardiovascular risk factors and severe clinical complications, including death in COVID-19 patients. All the above-mentioned risk factors are widespread and constitute a significant worldwide health problem. Some of them are modifiable and the awareness of their connection with the COVID-19 progress may have a crucial impact on the current and possible upcoming infection.
COVID-19
cardiovascular
obesity
lipid profile
1. Introduction
The coronavirus disease 2019 pandemic is spreading around the world and becoming a major public health crisis. All coronaviruses are known to affect the cardiovascular system. There is a strong correlation between cardiovascular risk factors and severe clinical complications including death in COVID-19 patients (Figure 1).
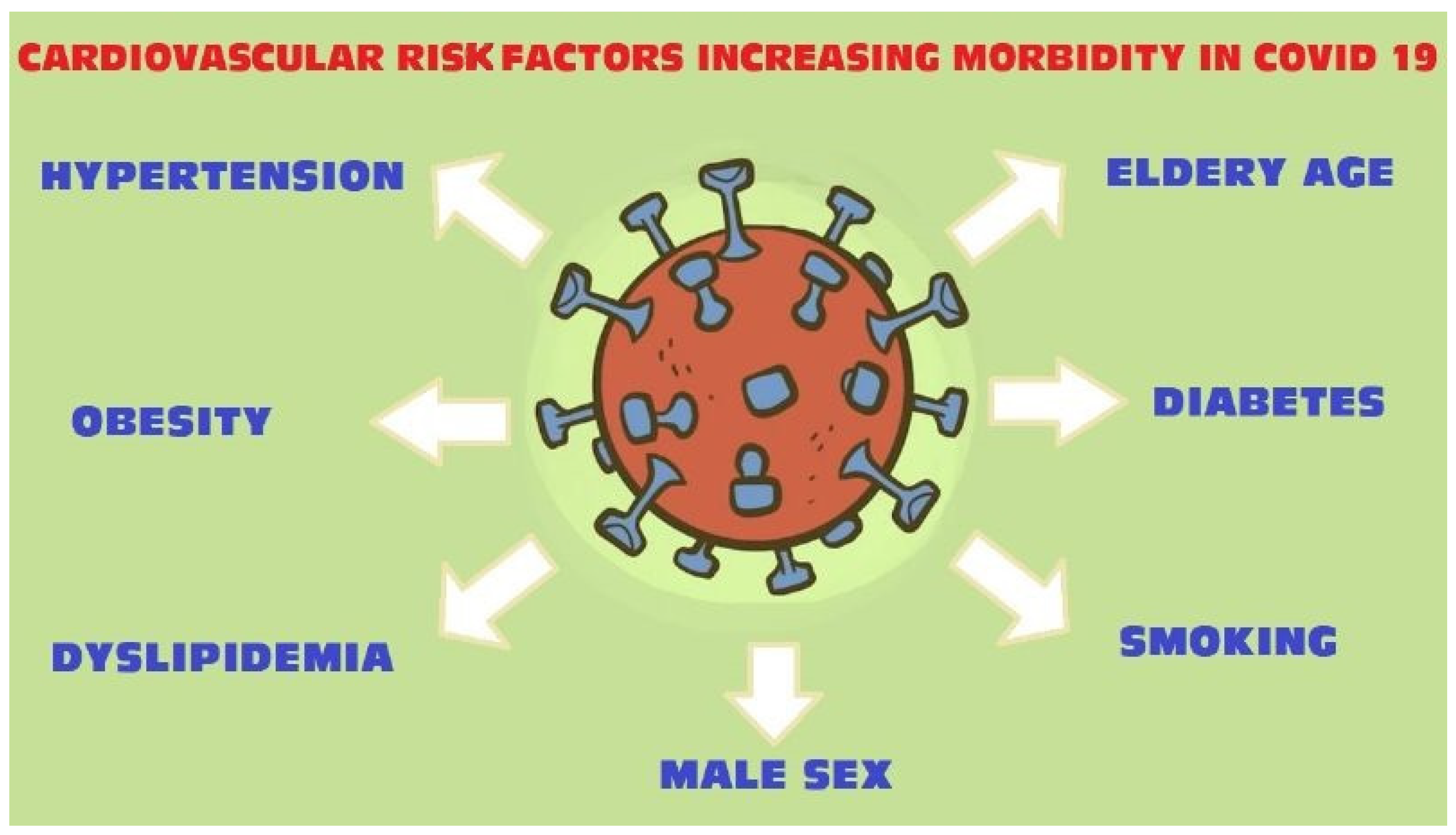
Figure 1. COVID-19 cardiovascular risk factors.
Diversified lifestyle, access to health care and prophylaxis, and an aging society contribute to the increasing number of patients suffering from civilization diseases such as obesity, hypertension, hyperlipidemia and diabetes. The presence of those comorbidities may deteriorate the course of COVID-19 infection.
Obesity was significantly associated with a higher in-hospital mortality as well as older age and male sex. Obese patients, <60 years old with Body Mass Index (BMI) ≥ 35 are 3.6 times more likely to be admitted to acute and critical care units, compared to patients with normal BMI in the same age [1].
Hyperlipidemia itself, as well as its treatment, contributes to the course of COVID-19 infection in a different way [2].
Hypertension is one of the most common and major cardiovascular risk factors. Worldwide, 1.33 billion people have elevated blood pressure. Chinese scientists who were the pioneers facing the COVID-19 infection indicated the connection between hypertension and higher risk of a severe course of COVID-19, including death [3].
Type 2 diabetes, especially with poorly controlled blood glucose, was found to be related to greater risk of acute respiratory distress syndrome (ARDS) development [4].
As coronavirus mostly affects the lungs, it is understandable that smoking, current and past, may be involved in the progress of COVID-19 [5].
2. Obesity
2.1. Methods
Researchers searched PubMed and Google Scholar databases, using the terms, “COVID-19 obesity”, “COVID-19 mortality obesity patients” as well as keywords such as “cardiovascular risk factors”, “obesity risk infections”. Further studies were sought by manually searching reference lists of the relevant articles. Relevant articles were selected based on their title, abstract or full text. Articles were excluded if they were clearly related to another subject matter or were not published in English. Out of 163 publications, researchers selected 20 for this subtitle.
2.2. Findings
Obesity, defined as BMI over 30 kg/m2 is associated with various disorders such as cardiovascular diseases, insulin resistance, type 2 diabetes mellitus, obstructive sleep apnea and some cancers [6][7]. It affects the immune response [8], endothelium imbalance [9], release of cytokines [10] and promotes chronic systemic inflammation [11]. All these features contribute to a worse course of infectious disease, prolonged hospitalization and worse outcomes in obese patients [12][13][14]. Therefore COVID-19 patients with obesity require particular attention.
In a study of 10,544 COVID-19 population, patients with a BMI of 30–40 kg/m2 had an increased risk for hospitalization and clinical deterioration compared to patients with a BMI below 30 kg/m2 [15]. In another study considering the COVID-19 infection, obesity together with age ≥ 52 years was strongly associated with illness severity [16]. Obesity was also shown as a high-risk factor for middle aged adult in a 3615 patients study. The authors suggested that obese patients aged between 52 and 60 years were more exposed to increased morbidity rates compared to patients > 60 years old [1]. What is more interesting, is there are studies that have reported the relation between poor prognosis of obese COVID-19 patients and gender. In a study by Cai Q et al. [17], the increased disease severity was correlated with the male sex. Similarly, Chiumello D. [18] found strong association between acute respiratory distress and male sex in overweight/obese patients. In contrast, a study of 32,583 patients indicated higher odds ratios in females than males. The authors suggested that females with obesity, diabetes and hypertension are more susceptible to COVID-19 and have a higher odds ratio for a severe COVID-19 course [19].
Obese patients more often demonstrated a cough and fever as initial symptoms, compared to normal weight patients [17]. Interestingly, in a small clinical study it was found that the increased area of visceral adipose tissue (measured at the level of the first lumbar vertebra on chest computed tomography) and upper abdominal circumference were associated with a higher probability of intensive care unit treatment or mechanical ventilation (adjusted for age and sex) [20]. There is also a strong association between a high BMI and mortality among the COVID-19 population. In a cohort of 20,133 cases, Docherty et al. [21] proved that obesity was significantly associated with a higher in-hospital mortality as well as older age, male sex and comorbidities such as chronic cardiac disease, chronic pulmonary disease, chronic kidney disease and liver disease. Further data from a Mexican study with 4103 COVID-19 cases showed a significant increase in hospitalization and mortality rate in patients with obesity [22]. Likewise, numerous clinical studies confirm the influence of obesity on outcomes of SARS-CoV-2 infection [23][24].
3. Lipid Profile
3.1. Methods
Researchers choose 19 from 59 publications, found in PubMed, using keywords: “lipid profile and COVID-19 infections”, “hyperlipidemia/dyslipidemia and COVID-19”, “statins COVID”. The works researchers used are mainly relevant reviews, original publications and the literature they contain. Non-English articles were excluded.
3.2. Findings
The lipid profile plays a key role in viral infection. The cholesterol membrane was found as an important component for pathogenic viruses entering host cells [25]. Hao Wang et al. [26] indicated that a high level of cholesterol in the cellular membranes of tissue enhanced the entry of the virus. The authors suggested that high cellular cholesterol indicates SARS-CoV-2 infectivity. The average cellular cholesterol level in the lung increases with age, thereby the number of viral entry points rises. When cholesterol is low, as in children, there are only a few entry points. In chronically ill patients, where the cellular cholesterol level is high (mostly due to age and chronic inflammation), all the angiotensin I converting enzyme 2 (ACE2) receptors are positioned for viral infectivity. However, blood sample analysis did not correlate with cholesterol levels in the tissue cell membranes. This is because the chronic inflammatory process prompts the inhibition of cholesterol efflux proteins in the peripheral tissue. In a study with infectious bronchitis coronavirus, it was demonstrated that reduction of cholesterol prevented the binding of coronavirus with the host cells [27]. In another study with porcine deltacoronavirus, the authors observed the pharmacological reduction of cellular or viral cholesterol might block virus attachment and internalization [28]. On the other hand, a clinical study in China showed lower serum lipid levels (total cholesterol, HDL-cholesterol and LDL-cholesterol) in patients with COVID-19 infection compared to healthy controls. It was noticed that cholesterol level continued to drop during the first few days of infection and then gradually rose. The authors suggested the lipid changes might be related to viral–host cell fusion and entry, and thus may indirectly indicate the effectiveness of the COVID-19 treatment regimens [29].
There is evidence suggesting statins influence the course of COVID-19 infection, which could be useful in treatment. Statins are cholesterol-lowering drugs that possess beneficial effects such as anti-thrombotic, immunomodulatory and anti-inflammatory functions [30]. As a result of controlling cytokine overexpression and modulating immune responses, statins may prevent ARDS and may reduce the incidence of cardiovascular complications in COVID-19 patients [31][32]. Statin treatment may block viral infectivity through inhibition of glycoprotein processing [33]. The SARS-CoV-2 main protease (Mpro), a key coronavirus enzyme, has been examined as a potential protein target to prevent infection expansion [34]. Željko Reiner et al. [2] indicated that statins could be SARS-CoV-2 Mpro inhibitors and may block entry of the virus into host cells.
There is also data indicating statins’ ability to upregulate ACE2 signaling pathways, which could mitigate the invasion of SARS-CoV-2 through the ACE2 receptor [35]. A high level of ACE2 in pulmonary endothelium was associated with reduced severity of ARDS [36]. Moreover, statins might counteract SARS-CoV-2-induced endothelitis in lungs by promoting endothelial repair and accelerate recovery from ARDS in COVID-19 patients [37][38]. Statins, through their anti-inflammatory effects, protect from the occurrence of plaque rupture and, therefore, reduce the risk of myocarditis and cardiac injury in COVID-19 patients [39][40].
Retrospective data showed a positive impact of statin use on mortality and in-hospital outcomes in the COVID-19 population. In a retrospective study of 2147 patients with COVID-19, the multivariate Cox model showed, after adjusting for age, gender, comorbidities, in-hospital medications and blood lipids, lower risk of mortality, acute respiratory distress syndrome or intensive care unit treatment in the statin group vs. the non-statin group [41]. Another study of 13,981 patients with COVID-19, among which 1219 received statins 28-day all-cause mortality was significantly lower than in the non-statin group [42]. On the other hand, in a meta-analysis of retrospective observational studies investigating the impact of previous statin use in COVID-19 patients, no significant reductions in either in-hospital mortality or COVID-19 severity were reported among statin users. However, such reductions were found after adjusting for confounding risk factors [43].
References
- Lighter, J.; Phillips, M.; Hochman, S.; Sterling, S.; Johnson, D.; Francois, F.; Stachel, A. Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission. Clin. Infect. Dis. 2020, 71, 896–897.
- Reiner, Ž.; Hatamipour, M.; Banach, M. Statins and the COVID-19 main protease: In silico evidence on direct interaction. Arch. Med. Sci. 2020, 16, 490–496.
- Shi, Y.; Yu, X.; Zhao, H.; Wang, H.; Zhao, R.; Sheng, J. Host susceptibility to severe COVID-19 and establishment of a host risk score: Findings of 487 cases outside Wuhan. Crit. Care 2020, 24, 108.
- Zhu, L.; She, Z.G.; Cheng, X.; Qin, J.J.; Zhang, X.J.; Cai, J.; Lei, F.; Wang, H.; Xie, J.; Wang, W.; et al. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020, 31, 1068–1077.
- Jiménez-Ruiz, C.A.; López-Padilla, D.; Alonso-Arroyo, A.; Aleixandre-Benavent, R.; Solano-Reina, S.; de Granda-Orive, J.I. COVID-19 and Smoking: A Systematic Review and Meta-Analysis of the Evidence. Arch. Bronconeumol. 2020, 57, 21–34.
- Hotamisligil, G.S. Inflammation, metaflammation and immunometabolic disorders. Nature 2017, 542, 177–185.
- Donohoe, C.L.; Lysaght, J.; O’Sullivan, J.; Reynolds, J.V. Emerging Concepts Linking Obesity with the Hallmarks of Cancer. Trends Endocrinol. Metab. 2017, 28, 46–62.
- McLaughlin, T.; Ackerman, S.E.; Shen, L.; Engleman, E. Role of innate and adaptive immunity in obesity-associated metabolic disease. J. Clin. Investig. 2017, 127, 5–13.
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. American Heart Association., Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006, 113, 898–918.
- Febbraio, M.A. Role of interleukins in obesity: Implications for metabolic disease. Trends Endocrinol. Metab. 2014, 25, 312–319.
- Reilly, S.M.; Saltiel, A.R. Adapting to obesity with adipose tissue inflammation. Nat. Rev. Endocrinol. 2017, 13, 633–643.
- Honce, R.; Schultz-Cherry, S. Impact of Obesity on Influenza A Virus Pathogenesis, Immune Response, and Evolution. Front. Immunol. 2019, 10, 1071.
- Huttunen, R.; Syrjänen, J. Obesity and the risk and outcome of infection. Int. J. Obes. 2013, 37, 333–340.
- Ghilotti, F.; Bellocco, R.; Ye, W.; Adami, H.O.; Trolle Lagerros, Y. Obesity and risk of infections: Results from men and women in the Swedish National March Cohort. Int. J. Epidemiol. 2019, 48, 1783–1794.
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966.
- Ebinger, J.E.; Achamallah, N.; Ji, H.; Claggett, B.L.; Sun, N.; Botting, P.; Nguyen, T.T.; Luong, E.; Kim, E.H.; Park, E.; et al. Pre-existing traits associated with Covid-19 illness severity. PLoS ONE 2020, 15, e0236240.
- Cai, Q.; Chen, F.; Wang, T.; Luo, F.; Liu, X.; Wu, Q.; He, Q.; Wang, Z.; Liu, Y.; Liu, L.; et al. Obesity and COVID-19 Severity in a Designated Hospital in Shenzhen, China. Diabetes Care 2020, 43, 1392–1398.
- Chiumello, D.; Pozzi, T.; Storti, E.; Caccioppola, A.; Pontiroli, A.E.; Coppola, S. Body mass index and acute respiratory distress severity in patients with and without SARS-CoV-2 infection. Br. J. Anaesth. 2020, 125, e376–e377.
- Hernández-Garduño, E. Obesity is the comorbidity more strongly associated for Covid-19 in Mexico. A case-control study. Obes. Res. Clin. Pract. 2020, 14, 375–379.
- Petersen, A.; Bressem, K.; Albrecht, J.; Thieß, H.M.; Vahldiek, J.; Hamm, B.; Makowski, M.R.; Niehues, A.; Niehues, S.M.; Adams, L.C. The role of visceral adiposity in the severity of COVID-19: Highlights from a unicenter cross-sectional pilot study in Germany. Metabolism 2020, 110, 154317.
- Docherty, A.B.; Harrison, E.M.; Green, C.A.; Hardwick, H.E.; Pius, R.; Norman, L.; Holden, K.A.; Read, J.M.; Dondelinger, F.; Carson, G.; et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ 2020, 369, m1985.
- Carrillo-Vega, M.F.; Salinas-Escudero, G.; García-Peña, C.; Gutiérrez-Robledo, L.M.; Parra-Rodríguez, L. Early estimation of the risk factors for hospitalization and mortality by COVID-19 in Mexico. PLoS ONE 2020, 15, e0238905.
- Hussain, A.; Mahawar, K.; Xia, Z.; Yang, W.; El-Hasani, S. Obesity and mortality of COVID-19. Meta-analysis. Obes. Res. Clin. Pract. 2021, 14, 295–300.
- Ho, J.S.Y.; Fernando, D.I.; Chan, M.Y.; Sia, C.H. Obesity in COVID-19: A Systematic Review and Meta-analysis. Ann. Acad. Med. Singap. 2020, 49, 996–1008.
- Meher, G.; Bhattacharjya, S.; Chakraborty, H. Membrane Cholesterol Modulates Oligomeric Status and Peptide-Membrane Interaction of Severe Acute Respiratory Syndrome Coronavirus Fusion Peptide. J. Phys. Chem. B 2019, 123, 10654–10662.
- Wang, H.; Yuan, Z.; Pavel, M.A.; Hansen, S.B. The role of high cholesterol in age-related COVID19 lethality. BioRxiv 2020, 29, 086249.
- Guo, H.; Huang, M.; Yuan, Q. The important role of lipid raft-mediated attachment in the infection of cultured cells by coronavirus infectious bronchitis virus beaudette strain. PLoS ONE 2017, 12, e0170123.
- Jeon, J.H.; Lee, C. Cholesterol is important for the entry process of porcine deltacoronavirus. Arch. Virol. 2018, 163, 3119–3124.
- Hu, X.; Chen, D.; Wu, L.; He, G.; Ye, W. Low Serum Cholesterol Level Among Patients with COVID-19 Infection in Wenzhou, China. SSRN Electron. J. 2020; under review.
- Piechota, M.; Barylski, M.; Hannam, S.; Piechota-Urbańska, M.; Banach, M.C. Review Rationale of statin therapy in septic patients. Urr. Vasc. Pharmacol. 2013, 11, 795–800.
- Liberale, L.; Carbone, F.; Montecucco, F.; Sahebkar, A. Statins reduce vascular inflammation in atherogenesis: A review of underlying molecular mechanisms. Int. J. Biochem. Cell Biol. 2020, 122, 795–800.
- Chruściel, P.; Sahebkar, A.; Rembek-Wieliczko, M. Impact of statin therapy on plasma adiponectin concentrations: A systematic review and meta-analysis of 43 randomized controlled trial arms. Atherosclerosis 2016, 253, 194–208.
- Shrivastava-Ranjan, P.; Flint, M.; Bergeron, É.; McElroy, A.K.; Chatterjee, P.; Albariño, C.G.; Nichol, S.T.; Spiropoulou, C.F. Statins suppress Ebola virus infectivity by interfering with glycoprotein processing. MBio 2018, 9, e00660-18.
- Liu, X.; Zhang, B.; Jin, Z.; Yang, H.; Rao, Z. The Crytal Structure of 2019-NCoV Main Protease in Complex with an Inhibitor N3. RCSB Protein Data Bank. 2020. Available online: https://www.wwpdb.org/pdb?id=pdb_00006lu7 (accessed on 5 May 2020).
- Tikoo, K.; Patel, G.; Kumar, S.; Karpe, P.A.; Sanghavi, M.; Malek, V. Tissue specific up regulation of ACE2 in rabbit model of atherosclerosis by atorvastatin: Role of epigenetic histone modifications. Biochem. Pharmacol. 2015, 93, 343–351.
- Wösten-van Asperen, R.M.; Bos, A.P.; Bem, R.A.; Dierdorp, B.S.; Dekker, T.; van Goor, H. Imbalance between pulmonary angiotensin-converting enzyme and angiotensin-converting enzyme 2 activity in acute respiratory distress syndrome. Pediatr. Crit. Care Med. 2013, 14, e438.
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418.
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128.
- Radenkovic, D.; Chawla, S.; Pirro, M.; Sahebkar, A.; Banach, M. Cholesterol in relation to COVID-19: Should we care about it? J. Clin. Med. 2020, 9, 1909.
- Madjid, M.; Safavi-Naeini, P.; Solomon, S.D.; Vardeny, O. Potential effects of coronaviruses on the cardiovascular system: A review. JAMA Cardiol. 2020, 5, 831–840.
- Fan, Y.; Guo, T.; Yan, F.; Gong, M.; Zhang, X.A.; Li, C.; He, T.; Luo, H.; Zhang, L.; Chen, M.; et al. Association of Statin Use With the In-Hospital Outcomes of 2019-Coronavirus Disease Patients: A Retrospective Study. Front. Med. 2020, 7, 584870.
- Zhang, X.-J.; Qin, J.-J.; Cheng, X. In-Hospital Use of Statins Is Associated with a Reduced Risk of Mortality among Individuals with COVID-19. Cell Metab. 2020, 32, 176–187.
- André J Scheen, Statins and clinical outcomes with COVID-19: Meta-analyses of observational studies. Diabetes Metab. 2020, 23, 101220.
More
Information
Subjects:
Medicine, General & Internal
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
996
Entry Collection:
COVID-19
Revisions:
3 times
(View History)
Update Date:
11 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




