Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Luca Giannoni | -- | 1435 | 2022-05-04 12:09:41 | | | |
| 2 | Jason Zhu | -12 word(s) | 1423 | 2022-05-05 03:31:09 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Giannoni, L.; Dallari, S.; , .; Fusco, I. CO2 Laser Transoral Laryngeal Microsurgery. Encyclopedia. Available online: https://encyclopedia.pub/entry/22589 (accessed on 08 February 2026).
Giannoni L, Dallari S, , Fusco I. CO2 Laser Transoral Laryngeal Microsurgery. Encyclopedia. Available at: https://encyclopedia.pub/entry/22589. Accessed February 08, 2026.
Giannoni, Luca, Stefano Dallari, , Irene Fusco. "CO2 Laser Transoral Laryngeal Microsurgery" Encyclopedia, https://encyclopedia.pub/entry/22589 (accessed February 08, 2026).
Giannoni, L., Dallari, S., , ., & Fusco, I. (2022, May 04). CO2 Laser Transoral Laryngeal Microsurgery. In Encyclopedia. https://encyclopedia.pub/entry/22589
Giannoni, Luca, et al. "CO2 Laser Transoral Laryngeal Microsurgery." Encyclopedia. Web. 04 May, 2022.
Copy Citation
CO2 laser transoral laryngeal microsurgery (TLM) is the preferred option for the majority of small–medium size glottic and supraglottic cancers and may also be used for bigger tumors, especially in older patients.
transoral laryngeal microsurgery
laser in ENT
laryngeal cancer
CO2 laser
Scanning micromanipulators
1. Introduction
In the early 1970s, Strong and Jako pioneered the so-called laryngeal laser surgery [1].
The CO2 laser, targeting water with its 10,600 wavelength, guarantees excellent cutting properties and low thermal spread [2][3]. It started to be used in microsurgery and endoscopic surgery, mainly in the field of otolaryngology and head and neck diseases [4].
Wolfgang Steiner holds the well-deserved title of father of the transoral laryngeal oncologic CO2 laser microsurgery [5].
From the 1980s onwards, several researchers significantly contributed to this field [6][7][8][9], and the technology and performance of laser systems improved significantly. Micro-spot micromanipulators and electronic scanning units were introduced, thus optimizing and simplifying the surgical techniques and encouraging more and more surgeons to adopt the CO2 laser, which became the gold standard in transoral laryngeal microsurgery (TLM) [10].
In 2000, on behalf of the European Laryngological Society (ELS), an ad hoc committee proposed a classification of the cordectomies [11] that was widely adopted. This contributed to the analysis and comparison of the oncologic and functional results of TLM or, as recently proposed [12], CO2 TOLMS (CO2 transoral laser microsurgery).
This classification was further updated in 2007 [13] with the introduction of a new category of cordectomy, type VI, and in 2009 [14] with a classification for supraglottic procedures.
This analyses and compares the experience gained with the SmartXide® HS and SmartXide2® CO2 laser systems in a series of 91 laryngeal cancers treated with TLM during the years 2009–2016 (Table 1).
Table 1. Case series.
| Type I | Type II | Type III | Type IV | Type V | Type VI | Enlarged | Total | |
|---|---|---|---|---|---|---|---|---|
| Number of patients (2009–2011) |
M 11 F - |
M 5 F 1 |
M 6 F - |
M 2 F 1 |
M 6 F1 |
M 3 F - |
M 6 F - |
M 39 F 3 |
| Number of patients (2012–2016) |
M 11 F - |
M 4 F - |
M 9 F - |
M 4 F - |
M 12 F - |
M 6 F - |
M 3 F - |
M 49 F - |
| Age range | ||||||||
| <50 | 1 | 1 | - | - | - | 1 | - | 3 (3%) |
| 51–60 | 8 | 4 | 4 | 1 | 3 | 4 | - | 24 (26%) |
| 61–70 | 4 | 1 | 3 | 2 | 6 | 1 | 1 | 18 (20%) |
| 71–80 | 6 | 3 | 5 | 2 | 7 | 2 | - | 28 (29%) |
| >80 | 3 | 1 | 3 | 2 | 3 | 1 | 5 | 18 (22%) |
The focus is on the technical characteristic of the CO2 laser equipment and the long-term oncologic results.
2. Laser Performance
In order to test the cutting properties and thermal damage of both laser systems used, histologies belonging to patients operated on with both the SmartXide HS and the SmartXide2 were revised, pointing out the (lateral) thermal damage on the various tissues (epithelium, vocal ligament/connective tissue and muscle). The analysis was carried out both on “light” procedures (type I cordectomies) and big excisions (enlarged procedures). As shown in Figure 1 and Figure 2, the thermal damage is minimal and the mean coagulation along the incision line is 20 ± 6 µm for the SP mode and 16 ± 7 µm for the UP mode, with negligible charring effects in specimens treated in the SP mode. The median values were 17 µm for the SP mode and 13 µm for the UP mode.
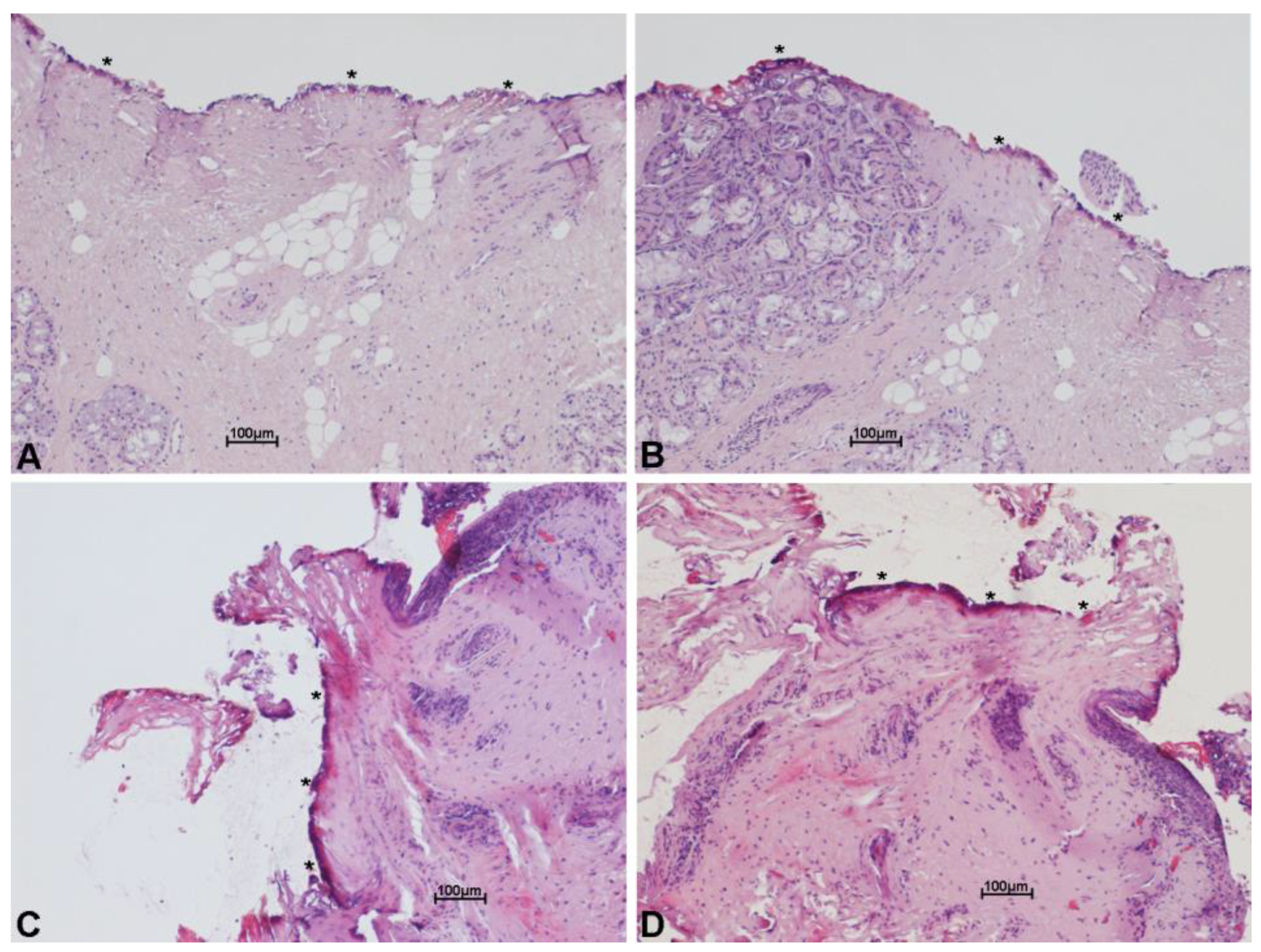
Figure 1. Histological images with hematoxylin and eosin stain, showing minimal thermal effects on the margin of the specimen excised with scanning micromanipulator and superpulsed technology. Thermal damage (*) on the connective tissue (A–D) and on the glandular epithelium (B), along incision line. Scale bars ×10 (A–D).
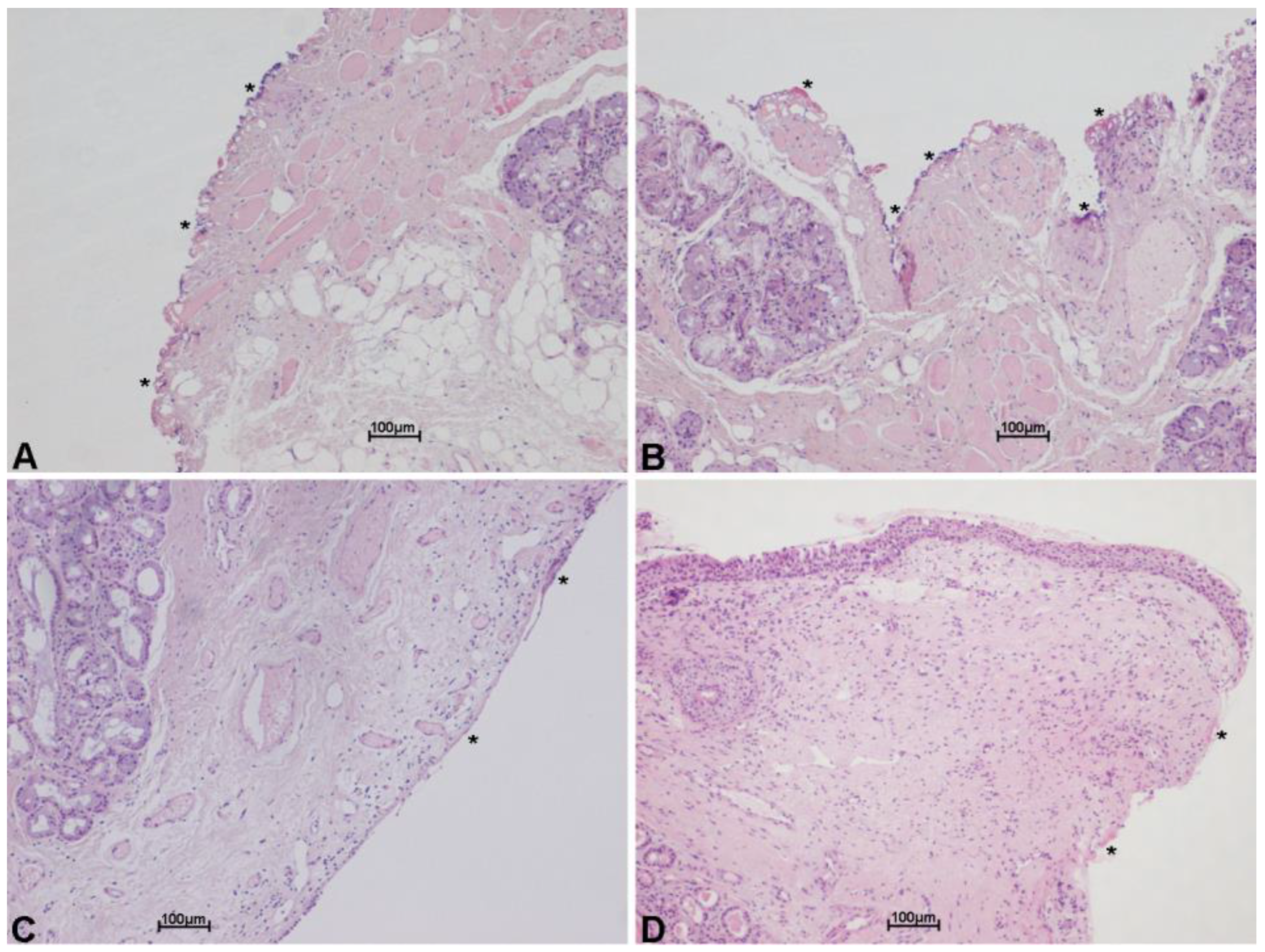
Figure 2. Histological images with hematoxylin and eosin stain, showing minimal thermal effects on the margin of the specimen excised with scanning micromanipulator and ultrapulsed technology. Thermal damage (*) on the connective tissue, along incision line. Scale bars ×10 (A–D).
3. Clinical Experience
The whole series was analyzed according to the type of surgery performed (I–V cordectomy and enlarged procedures).
For each type of surgery, several items were considered: histology at the first operation with regard to the margins; necessity of a safety cervicotomy or tracheotomy; histologic results after a repeated (planned) MLS; and the type of surgery performed to treat tumor recurrence/persistence.
The oncologic results and the follow-up data are reported. A survival curve of patients during the follow-up period was also evaluated and reported in Figure 3. Oncologic results describe the final outcome, that is how many patients were cured with the first operation, how many required further surgery to be cured and how many were not cured despite multiple surgeries. With regard to the follow-up, the series was divided into two groups: 42 patients were operated on between 2009 and 2011, and 49 from 2012 to 2016. The former group had a ten-year follow-up while the latter had five years of follow-up.
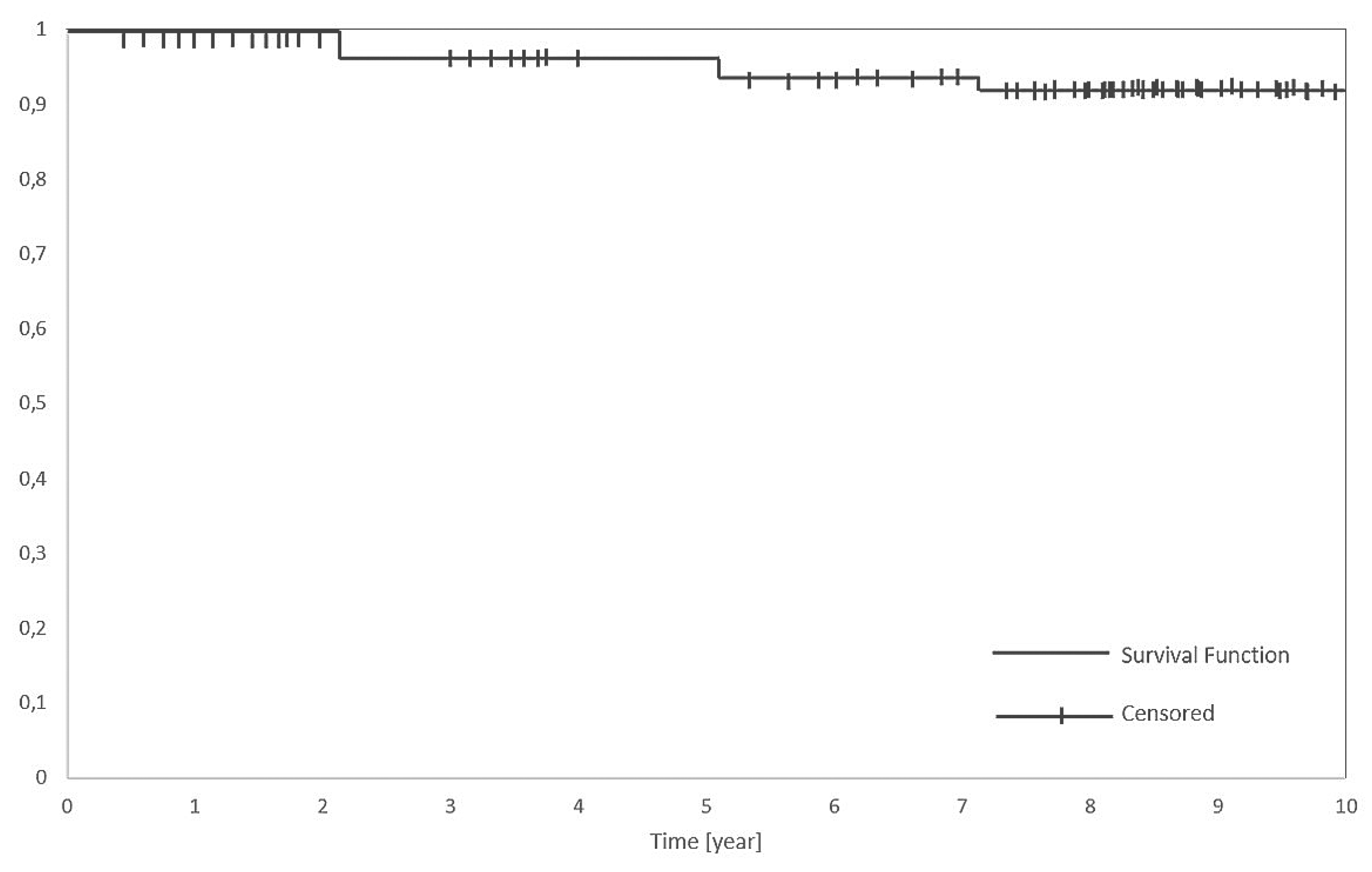
Figure 3. Kaplan-Meier disease-specific survival analysis in a series of 91 patients.
Figure 4 summarize the statistical analysis in terms of overall survival rate (OSR), that is the patients alive without any sign of diseases; Disease-specific survival (DSS), that is the whole series of patients except the ones dead with the specific disease; and disease-free survival (DFS), that accounts for the patients alive after the first operation.
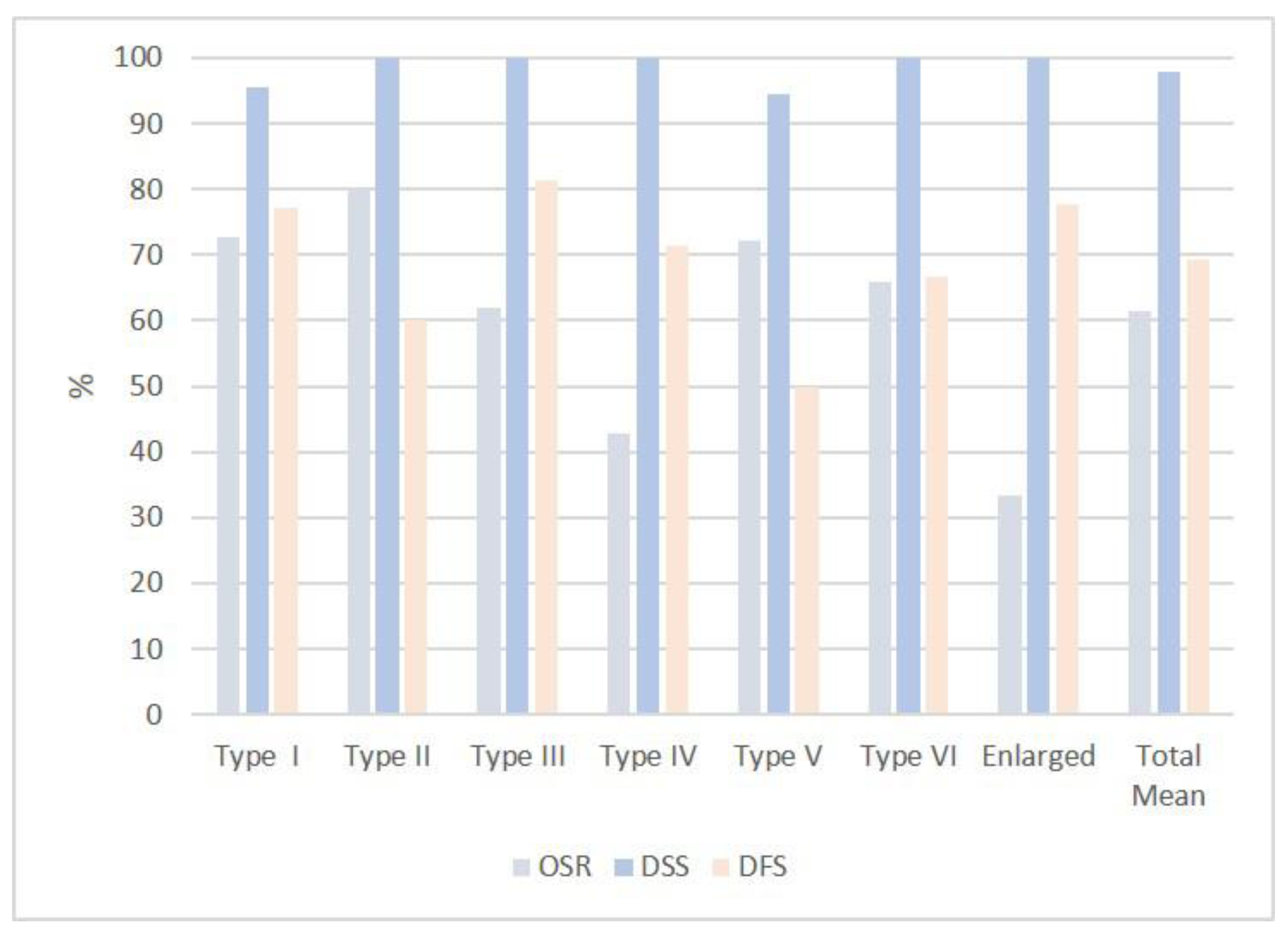
Figure 4. Graphical representation of the percentage of OSR, DSS and DFS rates in all type of cordectomies and enlarged procedures.
3.1. Type I Cordectomy
When performing a type I cordectomy, the senior researcher routinely injects saline into the Reinke’s space (“hydrodissection”) in order to better expose the lesion, better find and develop the plane of dissection and further preserve the vocal ligament.
A total of 22 patients, all males, underwent CO2 TLM.
A total of 21/22 (95%) patients were cured with 5/21 (23%) patients requiring further surgery. Only one patient (4.5%), who underwent an additional laser excision and subsequent subtotal laryngectomy with neck dissection, died from tracheal relapse while remaining free from tumors at the neo-larynx. At the time, 7 patients are alive with more than a ten-year follow-up, 9 with more than a five-year follow-up and 5 died from other causes, in most of the cases from senectus.
The overall survival rate (OSR) was 73%, disease-specific survival (DSS) rate was 95% and disease-free survival rate was 77%.
3.2. Type II Cordectomy
When adhesions to the vocal ligament and/or difficulties in dissecting the Reinke’s space were encountered, the senior researcher preferred to perform a subligamental cordectomy.
There were a total of 10 patients: 9 males and 1 female.
A total of 10/10 (100%) patients were cured. Of these, 4/10 (40%) patients recovered with further surgery. A total of 8 patients were still alive and NED and 2 patients died from other causes.
OSR was 80%, DSS 100% and DFS 60%.
3.3. Type III Cordectomy
There were a total of 16 patients, all males.
A total of 16/16 (100%) patients were cured. Of these, 3/16 (18.7%) patients recovered with further surgery. A total of 10/16 patients were alive and NED (6 with more than a ten-year follow-up and 4 with more than a five-year follow-up). A total of 1/16 patient died from neck recurrence after further surgery and 5/16 died from other causes (senectus).
One safety cervicotomy was performed.
OSR was 62%, DSS 100% and DFS 81%.
3.4. Type IV Cordectomy
When performing a type IV cordectomy, the senior researcher always completely removes the internal pericondrium.
There were a total of 7 patients: 6 males and 1 female.
All patients (100%) were locally cured. A total of 2/7 (28%) patients recovered with further surgery. A total of 3/7 patients were alive and NED. A total of 4/7 patients died from senectus or other causes.
Four safety cervicotomies were performed.
OSR was 43%, DSS 100% and DFS 71%.
3.5. Type V Cordectomy
There were a total of 18 patients: 17 males, 1 female.
A total of 17/18 (94%) patients were cured. A total of 9 patients (50%) were cured with the cordectomy and 8 patients (45%) were cured with further surgery. One patient, despite further open surgery, was not cured and died from the disease. A total of 13 patients were still alive and NED. Two patients, despite additional surgery, died from other reasons (one from a heart attack, the other from long-term post-operative complications) while they were negative at the neo-larynx level. Two patients died from senectus.
Five safety cervicotomies and one tracheotomy were performed.
OSR was 72%, DSD 94% and DFS 50%.
3.6. Type VI Cordectomy
There were a total of 9 patients, all males.
All 9 (100%) patients were locally cured: 6/9 patients with the cordectomy (67%) and 3/9 patients (33%) with further surgery. A total of 6/9 are still alive and NED. One patient died from metastatic lung disease, one of cerebral hemorrhage and one of senectus.
Two safety cervicotomies and Two tracheotomies were performed.
OSR was 67%, DSS 100% and DFS 67%.
3.7. Enlarged Procedures
There were a total of 9 patients, all males.
This small group included wide CO2 laser excisions involving the supraglottis and partially extended to the glottis. They have been divided into lateral supraglottic/glottic surgery (8 males) and medial anterior supraglottic/glottic surgery (1 male).
All 9 patients were locally cured: 7/9 (78%) patients with the first operation while 2/9 (23%) patients needed a second surgery. Only 1/9 patient died from metastatic disease, while 3/9 patients are still alive with a five-year follow-up.
A total of 5/9 patients (55%) died from other causes.
Two safety cervicotomies and three tracheotomies were performed.
OSR was 33%, DSS 100% and DFS 78%.
References
- Strong, M.S.; Jako, G.J. Laser Surgery in the Larynx Early Clinical Experience with Continuous Co2 Laser. Ann. Otol. Rhinol. Laryngol. 1972, 81, 791–798.
- Nisticò, S.P.; Bennardo, L.; Sannino, M.; Negosanti, F.; Tamburi, F.; Del Duca, E.; Giudice, A.; Cannarozzo, G. Combined CO2 and dye laser technique in the treatment of outcomes due to flap necrosis after surgery for basal cell carcinoma on the nose. Lasers Surg. Med. 2021, 1–7.
- Cannarozzo, G.; Bennardo, L.; Negosanti, F.; Nisticò, S.P. CO2 Laser Treatment in Idiopathic Scrotal Calcinosis: A Case Series. J. Lasers Med. Sci. 2020, 11, 500–501.
- Simpson, G.T.; Polanyi, T.G. History of the Carbon Dioxide Laser in Otolaryngologic Surgery. Otolaryngol. Clin. N. Am. 1983, 16, 739–752.
- Steiner, W. Results of curative laser microsurgery of laryngeal carcinomas. Am. J. Otolaryngol. 1993, 14, 116–121.
- Motta, G.; Villari, G.; Motta, G., Jr.; Ripa, G.; Salerno, G. The CO2 laser in the laryngeal microsurgery. Acta Otolaryngol. Suppl. 1986, 433, 1–30.
- Shapshay, S.M.; Hybels, R.L.; Bohigian, R.K. Laser Excision of Early Vocal Cord Carcinoma: Indications, Limitations, and Precautions. Ann. Otol. Rhinol. Laryngol. 1990, 99, 46–50.
- Peretti, G.; Nicolai, P.; De Zinis, L.O.R.; Berlucchi, M.; Bazzana, T.; Bertoni, F.; Antonelli, A.R. Endoscopic CO2 Laser Excision for Tis, T1, and T2 Glottic Carcinomas: Cure Rate and Prognostic Factors. Otolaryngol. Neck Surg. 2000, 123, 124–131.
- Peretti, G.; DE Zinis, L.O.R.; Nicolai, P.; Valentini, S.; Piazza, C.; Antonelli, A.R. Oncological Results of Endoscopic Resections of Tis and T1 Glottic Carcinomas by Carbon Dioxide Laser. Ann. Otol. Rhinol. Laryngol. 2001, 110, 820–826.
- Remacle, M.; Lawson, G.; Nollevaux, M.-C.; Delos, M. Current State of Scanning Micromanipulator Applications with the Carbon Dioxide Laser. Ann. Otol. Rhinol. Laryngol. 2008, 117, 239–244.
- Remacle, M.; Eckel, H.E.; Antonelli, A.; Brasnu, D.; Chevalier, D.; Friedrich, G.; Olofsson, J.; Rudert, H.H.; Thumfart, W.; de Vincentiiset, M.; et al. Endoscopic cordectomy. A proposal for a classification by the Working Committee, European Laryngological Society. Eur. Arch. Otorhinolaryngol. 2000, 257, 227–231.
- Remacle, M.; Arens, C.; Eldin, M.B.; Campos, G.; Estomba, C.C.; Dulguerov, P.; Fiz, I.; Hantzakos, A.; Keghian, J.; Moraet, F.; et al. Laser-assisted surgery of the upper aero-digestive tract: A clarification of nomenclature. A consensus statement of the European Laryngological Society. Eur. Arch. Otorhinolaryngol. 2017, 274, 3723–3727.
- Remacle, M.; Van Haverbeke, C.; Eckel, H.; Bradley, P.; Chevalier, D.; Djukic, V.; de Vicentiis, M.; Friedrich, G.; Olofsson, J.; Peretti, G.; et al. Proposal for revision of the European Laryngological Society classification of endoscopic cordectomies. Eur. Arch. Otorhinolaryngol. 2007, 264, 499–504.
- Remacle, M.; Hantzakos, A.; Eckel, H.; Evrard, A.S.; Bradley, P.J.; Chevalier, D.; Djukic, V.; de Vincentiis, M.; Friedrich, G.; Olofssonet, J.; et al. Endoscopic supraglottic laryngectomy: A proposal for a classification by the working committee on nomenclature, European Laryngological Society. Eur. Arch. Otorhinolaryngol. 2009, 266, 993–998.
More
Information
Subjects:
Otorhinolaryngology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
808
Revisions:
2 times
(View History)
Update Date:
05 May 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




