Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Luca Giannoni and Version 2 by Jason Zhu.
CO2 laser transoral laryngeal microsurgery (TLM) is the preferred option for the majority of small–medium size glottic and supraglottic cancers and may also be used for bigger tumors, especially in older patients.
- transoral laryngeal microsurgery
- laser in ENT
- laryngeal cancer
- CO2 laser
- Scanning micromanipulators
1. Introduction
The CO2 laser, targeting water with its 10,600 wavelength, guarantees excellent cutting properties and low thermal spread [2][3][2,3]. It started to be used in microsurgery and endoscopic surgery, mainly in the field of otolaryngology and head and neck diseases [4].
Wolfgang Steiner holds the well-deserved title of father of the transoral laryngeal oncologic CO2 laser microsurgery [5].
From the 1980s onwards, several researcheuthors significantly contributed to this field [6][7][8][9][6,7,8,9], and the technology and performance of laser systems improved significantly. Micro-spot micromanipulators and electronic scanning units were introduced, thus optimizing and simplifying the surgical techniques and encouraging more and more surgeons to adopt the CO2 laser, which became the gold standard in transoral laryngeal microsurgery (TLM) [10].
In 2000, on behalf of the European Laryngological Society (ELS), an ad hoc committee proposed a classification of the cordectomies [11] that was widely adopted. This contributed to the analysis and comparison of the oncologic and functional results of TLM or, as recently proposed [12], CO2 TOLMS (CO2 transoral laser microsurgery).
This classification was further updated in 2007 [13] with the introduction of a new category of cordectomy, type VI, and in 2009 [14] with a classification for supraglottic procedures.
This paper analyses and compares the experience gained with the SmartXide® HS and SmartXide2® CO2 laser systems in a series of 91 laryngeal cancers treated with TLM during the years 2009–2016 (Table 1).
Table 1. Case series.
| Type I | Type II | Type III | Type IV | Type V | Type VI | Enlarged | Total | |
|---|---|---|---|---|---|---|---|---|
| Number of patients (2009–2011) |
M 11 F - |
M 5 F 1 |
M 6 F - |
M 2 F 1 |
M 6 F1 |
M 3 F - |
M 6 F - |
M 39 F 3 |
| Number of patients (2012–2016) |
M 11 F - |
M 4 F - |
M 9 F - |
M 4 F - |
M 12 F - |
M 6 F - |
M 3 F - |
M 49 F - |
| Age range | ||||||||
| <50 | 1 | 1 | - | - | - | 1 | - | 3 (3%) |
| 51–60 | 8 | 4 | 4 | 1 | 3 | 4 | - | 24 (26%) |
| 61–70 | 4 | 1 | 3 | 2 | 6 | 1 | 1 | 18 (20%) |
| 71–80 | 6 | 3 | 5 | 2 | 7 | 2 | - | 28 (29%) |
| >80 | 3 | 1 | 3 | 2 | 3 | 1 | 5 | 18 (22%) |
The focus is on the technical characteristic of the CO2 laser equipment and the long-term oncologic results.
2. Laser Performance
In order to test the cutting properties and thermal damage of both laser systems used, histologies belonging to patients operated on with both the SmartXide HS and the SmartXide2 were revised, pointing out the (lateral) thermal damage on the various tissues (epithelium, vocal ligament/connective tissue and muscle). The analysis was carried out both on “light” procedures (type I cordectomies) and big excisions (enlarged procedures). As shown in Figure 1 and Figure 2, the thermal damage is minimal and the mean coagulation along the incision line is 20 ± 6 µm for the SP mode and 16 ± 7 µm for the UP mode, with negligible charring effects in specimens treated in the SP mode. The median values were 17 µm for the SP mode and 13 µm for the UP mode.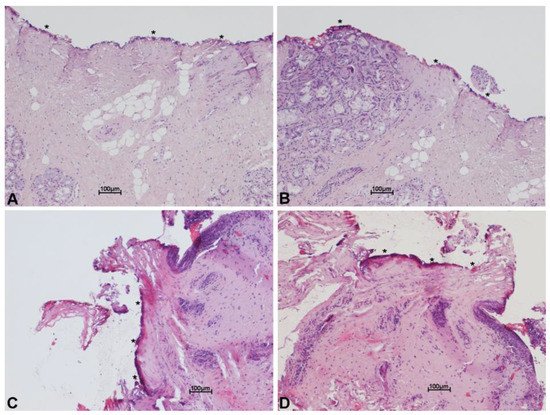
Figure 1. Histological images with hematoxylin and eosin stain, showing minimal thermal effects on the margin of the specimen excised with scanning micromanipulator and superpulsed technology. Thermal damage (*) on the connective tissue (A–D) and on the glandular epithelium (B), along incision line. Scale bars ×10 (A–D).
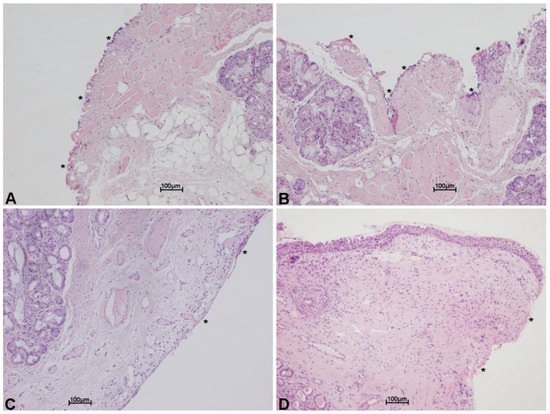
Figure 2. Histological images with hematoxylin and eosin stain, showing minimal thermal effects on the margin of the specimen excised with scanning micromanipulator and ultrapulsed technology. Thermal damage (*) on the connective tissue, along incision line. Scale bars ×10 (A–D).
3. Clinical Experience
The whole series was analyzed according to the type of surgery performed (I–V cordectomy and enlarged procedures). For each type of surgery, several items were considered: histology at the first operation with regard to the margins; necessity of a safety cervicotomy or tracheotomy (see discussion, 4.7); histologic results after a repeated (planned) MLS; and the type of surgery performed to treat tumor recurrence/persistence. The oncologic results and the follow-up data are reported. A survival curve of patients during the follow-up period was also evaluated and reported in Figure 3. Oncologic results describe the final outcome, that is how many patients were cured with the first operation, how many required further surgery to be cured and how many were not cured despite multiple surgeries. With regard to the follow-up, the series was divided into two groups: 42 patients were operated on between 2009 and 2011, and 49 from 2012 to 2016. The former group had a ten-year follow-up while the latter had five years of follow-up.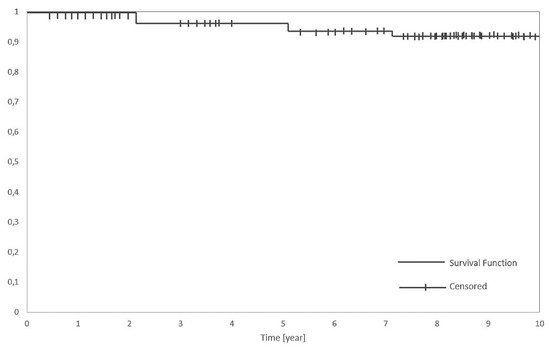
Figure 3.
Kaplan-Meier disease-specific survival analysis in a series of 91 patients.
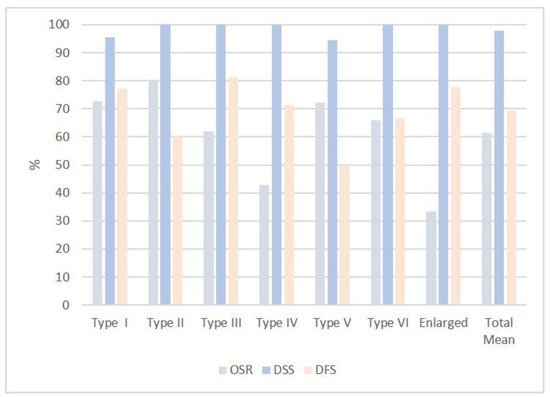
Figure 46.
Graphical representation of the percentage of OSR, DSS and DFS rates in all type of cordectomies and enlarged procedures.
