
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Hongxing Liu | -- | 1961 | 2022-04-22 15:58:22 | | | |
| 2 | Jason Zhu | -95 word(s) | 1866 | 2022-04-24 03:36:57 | | |
Video Upload Options
The diagnosis of myocardial injury inflammatory lesions is a difficult and challenging task, and despite various imaging modalities, myocardial injury inflammatory lesions are still a diagnosis of exclusion. Currently, endomyocardial biopsy (EMB) combined with genomics and immunohistochemistry can be used to evaluate myocardial inflammatory lesions in clinical practice. However, due to its invasiveness, sampling variability, limited spatial information, and low clinical implementation, it is difficult to apply in clinical practice and has great limitations. For inflammatory lesions of myocardium injury, clinical treatment strategies are supportive treatment or treatment of the primary underlying diseases, which are focused on delaying the disease process, are unable to reverse and repair the myocardial injury, and have limited effects on reducing morbidity and mortality. Therefore, it is of clinical urgency to actively seek effective treatment methods for myocardial injury and inflammation.
1. Existing Methods of Diagnosis for Myocardial Injury Inflammatory Lesions
2. Current Treatment Methods for Myocardial Injury and Inflammatory Lesions
3. Problems That Need to Be Solved
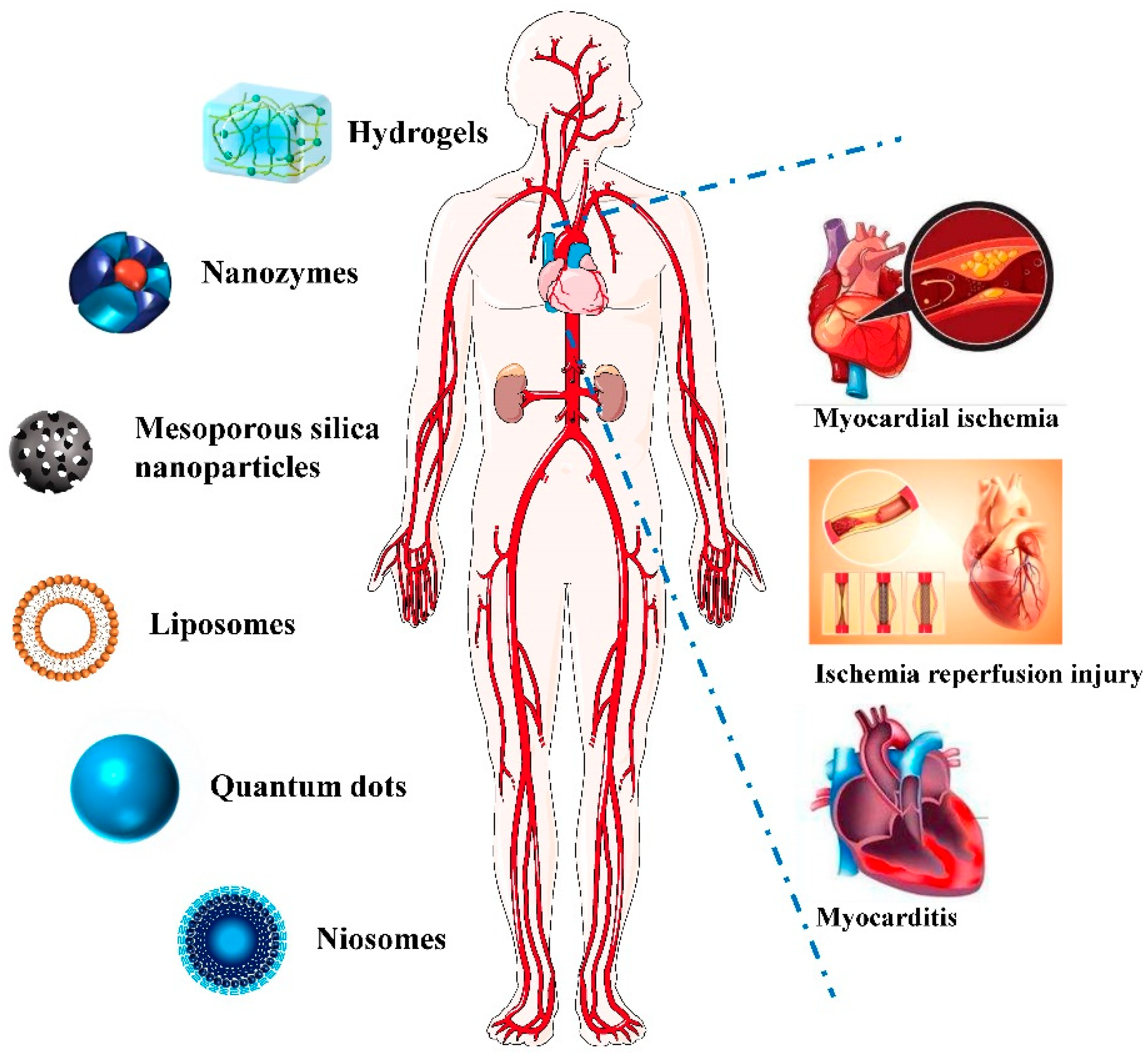
3.1. Hydrogel
3.2. Nano-Enzyme
3.3. Extracellular Vesicles
3.4. Other Nanomaterials
References
- Buggey, J.; ElAmm, C.A. Myocarditis and cardiomyopathy. Curr. Opin. Cardiol. 2018, 33, 341–346.
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Helio, T.; Heymans, S.; Jahns, R.; et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648.
- Caforio, A.L.; Marcolongo, R.; Basso, C.; Iliceto, S. Clinical presentation and diagnosis of myocarditis. Heart 2015, 101, 1332–1344.
- Ammirati, E.; Frigerio, M.; Adler, E.D.; Basso, C.; Birnie, D.H.; Brambatti, M.; Friedrich, M.G.; Klingel, K.; Lehtonen, J.; Moslehi, J.J.; et al. Management of Acute Myocarditis and Chronic Inflammatory Cardiomyopathy: An Expert Consensus Document. Circ. Heart Fail. 2020, 13, e007405.
- Tschope, C.; Cooper, L.T.; Torre-Amione, G.; Van Linthout, S. Management of Myocarditis-Related Cardiomyopathy in Adults. Circ. Res. 2019, 124, 1568–1583.
- Putschoegl, A.; Auerbach, S. Diagnosis, Evaluation, and Treatment of Myocarditis in Children. Pediatr. Clin. N. Am. 2020, 67, 855–874.
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017, 43, 304–377.
- L’Heureux, M.; Sternberg, M.; Brath, L.; Turlington, J.; Kashiouris, M.G. Sepsis-Induced Cardiomyopathy: A Comprehensive Review. Curr. Cardiol. Rep. 2020, 22, 35.
- Liang, Y.W.; Zhu, Y.F.; Zhang, R.; Zhang, M.; Ye, X.L.; Wei, J.R. Incidence, prognosis, and risk factors of sepsis -induced cardiomyopathy. World J. Clin. Cases 2021, 9, 9452–9468.
- Weintraub, R.G.; Semsarian, C.; Macdonald, P. Dilated cardiomyopathy. Lancet 2017, 390, 400–414.
- Marwick, T.H.; Ritchie, R.; Shaw, J.E.; Kaye, D. Implications of Underlying Mechanisms for the Recognition and Management of Diabetic Cardiomyopathy. J. Am. Coll. Cardiol. 2018, 71, 339–351.
- Dillmann, W.H. Diabetic Cardiomyopathy. Circ. Res. 2019, 124, 1160–1162.
- Patel, K.V.; Pandey, A.; de Lemos, J.A. Conceptual Framework for Addressing Residual Atherosclerotic Cardiovascular Disease Risk in the Era of Precision Medicine. Circulation 2018, 137, 2551–2553.
- Saucerman, J.J.; Tan, P.M.; Buchholz, K.S.; McCulloch, A.D.; Omens, J.H. Mechanical regulation of gene expression in cardiac myocytes and fibroblasts. Nat. Rev. Cardiol. 2019, 16, 361–378.
- Tang, X.; Chen, X.F.; Chen, H.Z.; Liu, D.P. Mitochondrial Sirtuins in cardiometabolic diseases. Clin. Sci. 2017, 131, 2063–2078.
- Costantino, S.; Paneni, F.; Cosentino, F. Ageing, metabolism and cardiovascular disease. J. Physiol. 2016, 594, 2061–2073.
- Akbar, N.; Digby, J.E.; Cahill, T.J.; Tavare, A.N.; Corbin, A.L.; Saluja, S.; Dawkins, S.; Edgar, L.; Rawlings, N.; Ziberna, K.; et al. Endothelium-derived extracellular vesicles promote splenic monocyte mobilization in myocardial infarction. JCI Insight 2017, 2, e93344.
- Tang, X.; Luo, Y.X.; Chen, H.Z.; Liu, D.P. Mitochondria, endothelial cell function, and vascular diseases. Front. Physiol. 2014, 5, 175.
- Eelen, G.; de Zeeuw, P.; Simons, M.; Carmeliet, P. Endothelial cell metabolism in normal and diseased vasculature. Circ. Res. 2015, 116, 1231–1244.
- Fung, G.; Luo, H.; Qiu, Y.; Yang, D.; McManus, B. Myocarditis. Circ. Res. 2016, 118, 496–514.
- Correa, S.; Grosskopf, A.K.; Lopez Hernandez, H.; Chan, D.; Yu, A.C.; Stapleton, L.M.; Appel, E.A. Translational Applications of Hydrogels. Chem. Rev. 2021, 121, 11385–11457.
- Jiang, Y.; Krishnan, N.; Heo, J.; Fang, R.H.; Zhang, L. Nanoparticle-hydrogel superstructures for biomedical applications. J. Control. Release 2020, 324, 505–521.
- Zeng, Q.; Qi, X.; Shi, G.; Zhang, M.; Haick, H. Wound Dressing: From Nanomaterials to Diagnostic Dressings and Healing Evaluations. ACS Nano 2022, 16, 1708–1733.
- Zhao, C.; Tian, S.; Liu, Q.; Xiu, K.; Lei, I.; Wang, Z.; Ma, P.X. Biodegradable nanofibrous temperature-responsive gelling microspheres for heart regeneration. Adv. Funct. Mater. 2020, 30, 2000776.
- Ghanta, R.K.; Aghlara-Fotovat, S.; Pugazenthi, A.; Ryan, C.T.; Singh, V.P.; Mathison, M.; Jarvis, M.I.; Mukherjee, S.; Hernandez, A.; Veiseh, O. Immune-modulatory alginate protects mesenchymal stem cells for sustained delivery of reparative factors to ischemic myocardium. Biomater. Sci. 2020, 18, 5061–5070.
- Li, H.; Yu, B.; Yang, P.; Zhan, J.; Fan, X.; Chen, P.; Liao, X.; Ou, C.; Cai, Y.; Chen, M. Injectable AuNP-HA matrix with localized stiffness enhances the formation of gap junction in engrafted human induced pluripotent stem cell-derived cardiomyocytes and promotes cardiac repair. Biomaterials 2021, 279, 121231.
- Wu, J.J.X.; Wang, X.Y.; Wang, Q.; Lou, Z.P.; Li, S.R.; Zhu, Y.Y.; Qin, L.; Wei, H. Nanomaterials with enzyme-like characteristics (nanozymes): Next-generation artificial enzymes (II). Chem. Soc. Rev. 2019, 48, 1004–1076.
- Liang, M.; Yan, X. Nanozymes: From New Concepts, Mechanisms, and Standards to Applications. Acc. Chem. Res. 2019, 52, 2190–2200.
- Wang, H.; Wan, K.; Shi, X. Recent Advances in Nanozyme Research. Adv. Mater. 2019, 31, e1805368.
- Zhang, Y.; Khalique, A.; Du, X.; Gao, Z.; Wu, J.; Zhang, X.; Zhang, R.; Sun, Z.; Liu, Q.; Xu, Z.; et al. Biomimetic Design of Mitochondria-Targeted Hybrid Nanozymes as Superoxide Scavengers. Adv. Mater. 2021, 33, e2006570.
- Li, H.Y.; Yan, J.; Meng, D.J.; Cai, R.; Gao, X.S.; Ji, Y.L.; Wang, L.M.; Chen, C.Y.; Wu, X.C. Gold Nanorod-Based Nanoplatform Catalyzes Constant NO Generation and Protects from Cardiovascular Injury. ACS Nano 2020, 14, 12854–12865.
- Théry, C.; Witwer, K.W.; Aikawa, E.; Alcaraz, M.J.; Anderson, J.D.; Andriantsitohaina, R.; Antoniou, A.; Arab, T.; Archer, F.; Atkin-Smith, G.K.; et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles 2018, 7, 1535750.
- Bandu, R.; Oh, J.W.; Kim, K.P. Mass spectrometry-based proteome profiling of extracellular vesicles and their roles in cancer biology. Exp. Mol. Med. 2019, 51, 30.
- Wang, C.; Li, Z.; Liu, Y.; Yuan, L. Exosomes in atherosclerosis: Performers, bystanders, biomarkers, and therapeutic targets. Theranostics 2021, 11, 3996–4010.
- Sahoo, S.; Adamiak, M.; Mathiyalagan, P.; Kenneweg, F.; Kafert-Kasting, S.; Thum, T. Therapeutic and Diagnostic Translation of Extracellular Vesicles in Cardiovascular Diseases Roadmap to the Clinic. Circulation 2021, 143, 1426–1449.
- Liu, C.; He, D.; Cen, H.; Chen, H.; Li, L.; Nie, G.; Zhong, Z.; He, Q.; Yang, X.; Guo, S.; et al. Nucleic acid functionalized extracellular vesicles as promising therapeutic systems for nanomedicine. Extracell. Vesicles Circ. Nucleic Acids 2022, 3, 14–30.
- Anselmo, A.; Frank, D.; Papa, L.; Viviani Anselmi, C.; Di Pasquale, E.; Mazzola, M.; Panico, C.; Clemente, F.; Soldani, C.; Pagiatakis, C.; et al. Myocardial hypoxic stress mediates functional cardiac extracellular vesicle release. Eur. Heart J. 2021, 42, 2780–2792.
- Li, X.; Yang, Z.; Nie, W.; Jiang, J.; Li, S.; Li, Z.; Tian, L.; Ma, X. Exosomes derived from cardiac progenitor cells attenuate CVB3-induced apoptosis via abrogating the proliferation of CVB3 and modulating the mTOR signaling pathways. Cell Death Dis. 2019, 10, 691.
- Mulder, W.J.M.; Jaffer, F.A.; Fayad, Z.A.; Nahrendorf, M. Imaging and nanomedicine in inflammatory atherosclerosis. Sci. Transl. Med. 2014, 6, 239sr1.
- Koo, H.; Huh, M.S.; Ryu, J.H.; Lee, D.E.; Sun, I.C.; Choi, K.; Kim, K.; Kwon, I.C. Nanoprobes for biomedical imaging in living systems. Nano Today 2011, 2, 204–220.
- Ma, T.; Hou, Y.; Zeng, J.; Liu, C.; Zhang, P.; Jing, L.; Shangguan, D.; Gao, M. Dual-Ratiometric Target-Triggered Fluorescent Probe for Simultaneous Quantitative Visualization of Tumor Microenvironment Protease Activity and pH In Vivo. J. Am. Chem. Soc. 2018, 140, 211–218.
- Zhao, X.L.; Luo, W.; Hu, J.; Zuo, L.; Wang, J.; Hu, R.; Wang, B.; Xu, L.; Li, J.; Wu, M.; et al. Cardiomyocyte-targeted and 17 beta-estradiol-loaded acoustic nanoprobes as a theranostic platform for cardiac hypertrophy. J. Nanobiotechnol. 2018, 16, 36.
- Solaiyappan, M.; Weiss, R.G.; Bottomley, P.A. Neural-network classification of cardiac disease from P-31 cardiovascular magnetic resonance spectroscopy measures of creatine kinase energy metabolism. J. Cardiovasc. Magn. R 2019, 21, 49.
- Li, X.J.; Zhou, S.Y.; Lu, S.; Tu, D.T.; Zheng, W.; Liu, Y.; Li, R.F.; Chen, X.Y. Lanthanide Metal-Organic Framework Nanoprobes for the In Vitro Detection of Cardiac Disease Markers. ACS Appl. Mater. Interfaces 2019, 11, 43989–43995.




