
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sofia Lima | -- | 3909 | 2022-04-21 17:35:31 | | | |
| 2 | Vivi Li | Meta information modification | 3909 | 2022-04-22 05:08:04 | | |
Video Upload Options
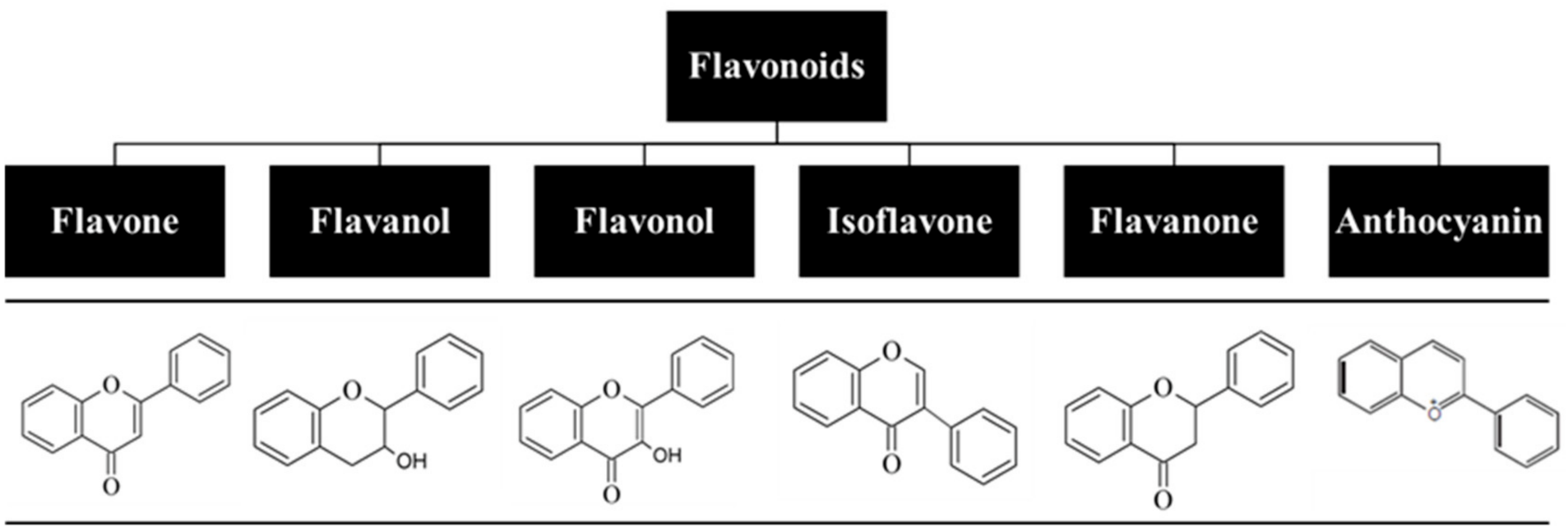
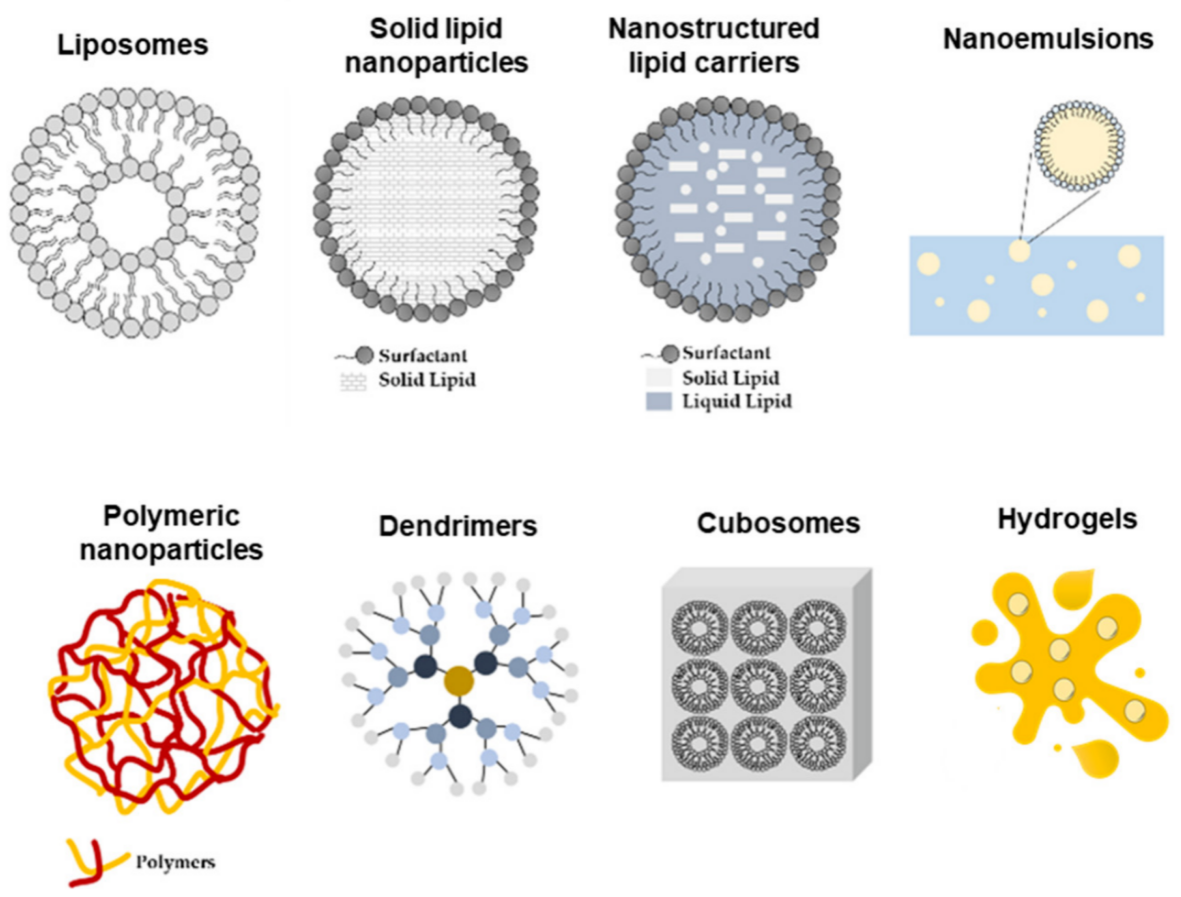
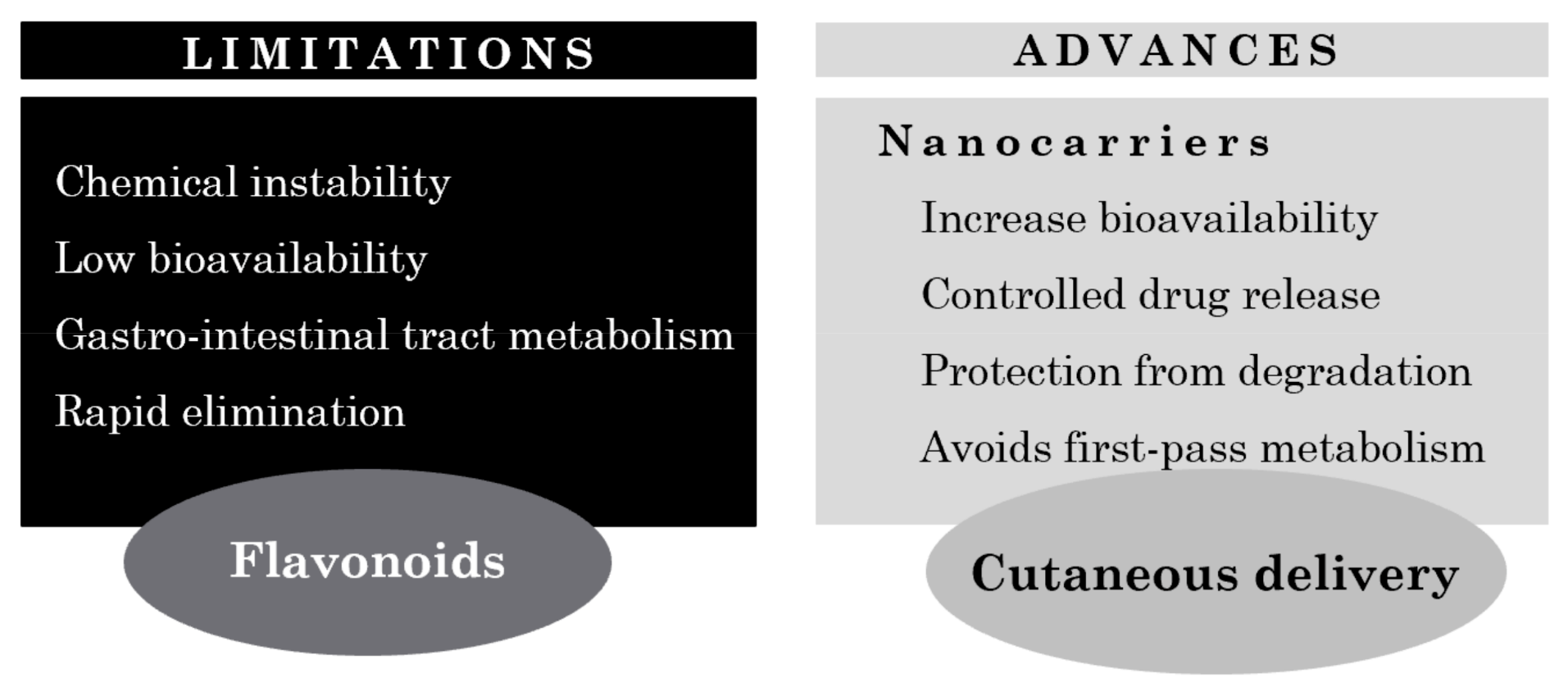
Flavonoids are one of the vital classes of natural polyphenolic compounds abundantly found in plants. Due to their wide range of therapeutic properties, which include antioxidant, anti-inflammatory, photoprotective, and depigmentation effects, flavonoids have been demonstrated to be promising agents in the treatment of several skin disorders. However, their lipophilic nature and poor water solubility invariably lead to limited oral bioavailability. In addition, they are rapidly degraded and metabolized in the human body, hindering their potential contribution to the prevention and treatment of many disorders. Thus, to overcome these challenges, several cutaneous delivery systems have been extensively studied. Topical drug delivery besides offering an alternative administration route also ensures a sustained release of the active compound at the desired site of action. Incorporation into lipid or polymer-based nanoparticles appears to be a highly effective approach for cutaneous delivery of flavonoids with good encapsulation potential and reduced toxicity.
1. Introduction
2. Bioavailability of Flavonoids
3. The Need for Nanocarriers in Cutaneous Flavonoid Delivery
4. Cutaneous Delivery Systems of Flavonoids for Treatment of Skin Pathologies
4.1. Examples of Nanocarriers Designed for Flavonol Cutaneous Delivery
4.2. Examples of Nanocarriers Designed for Other Flavonoid Classes’ Topical Delivery
| Flavonoid | Nanoformulation | Skin Model | Therapeutic Application | Ref. |
|---|---|---|---|---|
| Quercetin | Solid lipid nanoparticles |
Human skin | Delay UVB radiation-mediated cell damage and necrosis | [30] |
| Non-ionic emulsion with high lipid content | Pig ear skin | Inhibition of UVB-induced cutaneous oxidative stress and inflammation | [4] | |
| Anionic emulsion with low lipid content | Pig ear skin | Inhibition of UVB-induced cutaneous oxidative stress and inflammation | [4] | |
| Lecithin-chitosan nanoparticles | Male Kunming mice | Topical delivery system with a wide range of applications | [28] | |
| Lipid microparticles | n.a. | Enhance quercetin stability in topical formulations | [27] | |
| Colloidal silica emulsion |
Human skin | Optimization of a formulation with enhance penetration into human SC | [48] | |
| Chitosan nanoparticles | HaCaT cells | Potential therapeutic agent for topical use against UVB radiation | [29] | |
| Penetration Enhancer containing Vesicles (PEVs) | New born pig skin | New formulation for dermal delivery of quercetin, with various therapeutic applications | [31] | |
| Polylactide nanocapsules; Multilamellar liposomes; Niosomes | Subcutaneous injection in amistogote-infected hamsters | Antileishmanial agent | [3][49] | |
| Liposomes with penetration enhancing vesicles (PEV) | Female CD-1 mice | Anti-inflammatory agent | [5][49] | |
| Lipid nanocapsules | Acute monocytic leukemia cell line (THP1–1 cell) | Antioxidant, anti-inflammatory agent | [5][50] | |
| Nanoparticle suspension | Mice | Antioxidant agent | [5][41] | |
| Catechins | Multilamellar phosphatidylcholine-liposomes | Female nude mouse (Balb/c-nu, 6–8 weeks old) | Use of liposomes for the local delivery, including skin and tumor deposition, of polyphenols | [3][43] |
| Ethanol enriched liposomes | Female nude mouse (Balb/c-nu, 6–8 week) | Antioxidant and chemopreventive activity | [44] | |
| Cream | Iranian rabbits | Wound healing effect | [5][51] | |
| Tansfersomes containing EGCG and hyaluronic acid (HA) | HaCaT cells | Synergize the UV radiation-protective ability of EGCG and HA along with imparting antioxidant and antiaging effects | [5][42] | |
| Genistein | Nanoemulsion | Pig ear skin | New formulation for dermal delivery of genistein, with various therapeutic applications | [3][52] |
| Kaempferol | Submicron emulsions | Sprague Dawley rat | Promising vehicle for topical kaempferol application | [33] |
| Resveratrol | Solid lipid Nanoparticles |
Porcine skin | Protection from photodegradation | [53] |
| Resveratrol + curcumin | Lipid-core Nanocapsules |
Human skin | Increase skin delivery of resveratrol | [54] |
| Niosomes | Cell rabbit skin | Increase skin delivery of resveratrol Increased antioxidant activity |
[55] | |
| Hesperetin, hesperidin | Microemulsion | Guinea pigs | Whitening effect | [5][56] |
| Topical matrix film | Albino rabbits | Release of hesperetin in posterior of eye | [5][57] | |
| Microemulsion based ointment | Wistar rats | Skin irritation | [5][58] | |
| Naringenin | Gel | HRS/J mice | Antioxidant and anti-inflammatory agent | [5][54] |
| Nanoparticles | Wistar rats | Photoprotective, antioxidant agent | [5][54] | |
| Apigenin | Phospholipid phytosomes | Albino rats | Antioxidant agent | [5][59] |
| Ethosomes | Konmin mice | Anti-inflammatory agent | [5][60] | |
| Anthocyanin | Niosome gel | Male Wistar rats | Anti-inflammatory agent | [5][61] |
| Luteolin | Luteolin in olive oil | ICR mice | Anti-inflammatory agent | [5][62] |
| Luteolin-loaded niosomes/Niosomal transgel | Albino Wistar rats | Treatment of arthritis | [40] | |
| Nanoemulsion | C57BL/6 mice | Growth promoting effect | [41] |
References
- Kumar, S.; Pandey, A.K. Chemistry and Biological Activities of Flavonoids: An Overview. Sci. World J. 2013, 4, 1–16.
- Panche, A.N.; Diwan, A.D.; Chandra, S.R. Flavonoids: An overview. J. Nutr. Sci. 2016, 5, e47.
- Leonarduzzi, G.; Testa, G.; Sottero, B.; Gamba, P.; Poli, G. Design and Development of Nanovehicle-Based Delivery Systems for Preventive or Therapeutic Supplementation with Flavonoids. Curr. Med. Chem. 2009, 17, 74–95.
- Verri, W.A.; Vicentini, F.T.M.C.; Baracat, M.M.; Georgetti, S.R.; Cardoso, R.D.R.; Cunha, T.M.; Ferreira, S.H.; Cunha, F.Q.; Fonseca, M.J.V.; Casagrande, R. Studies in Natural Products Chemistry, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2012; Volume 36.
- Nagula, R.L.; Wairkar, S.J. Recent advances in topical delivery of flavonoids: A review. Control. Release 2019, 296, 190–201.
- Domaszewska-Szostek, A.; Puzianowska-Kuźnicka, M.; Kuryłowicz, A. Flavonoids in Skin Senescence Prevention and Treatment. Int. J. Mol. Sci. 2021, 22, 6814.
- Yang, B.; Liu, H.; Yang, J.; Gupta, V.K.; Jiang, Y. New insights on bioactivities and biosynthesis of flavonoid glycosides. Trends Food Sci. Technol. 2018, 79, 116–124.
- Yang Wang, T.; Li, Q.; Shun Bi, K. Bioactive flavonoids in medicinal plants: Structure, activity and biological fate. Asian J. Pharm. Sci. 2017, 13, 12–23.
- Rengasamy, K.R.R.; Khan, H.S.; Gowrishankar, S.; Lagoa, R.J.L.; Mahomoodally, F.M.; Khan, Z.; Suroowan, S.; Tewari, D.; Zengin, G.; Hassan, S.T.S.; et al. The role of flavonoids in autoimmune diseases: Therapeutic updates. Pharmacol. Ther. 2018, 194, 107–131.
- Perez-Vizcaino, F.; Fraga, C.G. Research trends in flavonoids and health. Arch. Biochem. Biophys. 2018, 646, 107–112.
- Shelke, S.J.; Shinkar, D.M.; Saudagar, R.B. Topical gel: A novel approach for development of topical drug delivery system. Int. J. Pharm. Technol. 2013, 5, 2739–2763.
- Menaa, F.; Menaa, A.; Menaa, B. Polyphenols Nano-Formulations for Topical Delivery and Skin Tissue Engineering. In Polyphenols in Human Health and Disease; Elsevier Inc: Amsterdam, The Netherlands, 2014; pp. 839–848.
- Khan, H.; Ullah, H.; Martorell, M.; Valdes, S.E.; Belwal, T.; Tejada, S.; Sureda, A.; Kamal, M.A. Flavonoids nanoparticles in cancer: Treatment, prevention and clinical prospects. Semin. Cancer Biol. 2021, 69, 200–211.
- Ruenroengklin, N.; Zhong, J.; Duan, X.; Yang, B.; Li, J.; Jiang, Y. Effects of Various Temperatures and pH Values on the Extraction Yield of Phenolics from Litchi Fruit Pericarp Tissue and the Antioxidant Activity of the Extracted Anthocyanins. Int. J. Mol. 2008, 9, 1333–1341.
- Palafox-Carlos, H.; Ayala-Zavala, J.F.; González-Aguilar, G.A. The role of dietary fiber in the bioaccessibility and bioavailability of fruit and vegetable antioxidants. J. Food Sci. 2011, 76, R6–R15.
- Li, C.; Lee, M.J.; Sheng, S.; Meng, X.; Prabhu, S.; Winnik, B.; Huang, B.; Chung, J.Y.; Yan, S.; Ho, C.T.; et al. Structural identification of two metabolites of catechins and their kinetics in human urine and blood after tea ingestion. Chem. Res. Toxicol. 2000, 13, 177–184.
- Lambert, J.D.; Sang, S.; Yang, C.S. Biotransformation of green tea polyphenols and the biological activities of those metabolites. Mol. Pharm. 2007, 4, 819–825.
- Schubert, W.; Eriksson, U.; Edgar, B.; Cullberg, G.; Hedner, T. Flavonoids in grapefruit juice inhibit the in vitro hepatic metabolism of 17β-estradiol. Eur. J. Drug Metab. Pharmacok. 1995, 20, 219–224.
- Ramadon, D.; McCrudden, M.T.C.; Courtenay, A.J.; Donnelly, R.F. Enhancement strategies for transdermal drug delivery systems: Current trends and applications. Drug Deliv. Transl. Res. 2021, 11, 1–34.
- Cermak, R.; Wolffram, S. Effect of dietary flavonoids on pathways involved in drug metabolism. Expert Opin. Drug Metab. Toxicol. 2008, 4, 17–35.
- Rahman, H.S.; Othman, H.H.; Hammadi, N.I.; Yeap, S.K.; Amin, K.M.; Samad, N.A.; Alitheen, N.B. Novel drug delivery systems for loading of natural plant extracts and their biomedical applications. Int. J. Nanomed. 2020, 15, 2439.
- Jain, K.K. Nanomedicine: Application of nanobiotechnology in medical practice. Med. Princ. Pract. 2008, 17, 89–101.
- Kreuter, J. Nanoparticles. In Encyclopaedia of Pharmaceutical Technology; Marcel Dekker Inc: New York, NY, USA, 1994.
- Casagrande, R.; Georgetti, S.R.; Verri, W.A., Jr.; Borin, M.F.; Lopez, R.F.; Fonseca, M.J. In vitro evaluation of quercetin cutaneous absorption from topical formulations and its functional stability by antioxidant activity. Int. J. Pharm. 2007, 328, 183–190.
- Casagrande, R.; Georgetti, S.R.; Verri, W.A., Jr.; Dorta, D.J.; dos Santos, A.C.; Fonseca, M.J. Protective effect of topical formulations containing quercetin against UVB-induced oxidative stress in hairless mice. J. Photochem. Photobiol. 2006, 84, 21–27.
- Vicentini, F.T.; Casagrande, R.; Verri, W.A., Jr.; Georgetti, S.R.; Bentley, M.V.; Fonseca, M.J. Quercetin in lyotropic liquid crystalline formulations: Physical, chemical and functional stability. AAPS Pharm. Sci. Technol. 2008, 9, 591–596.
- Scalia, S.; Mezzena, M.J. Incorporation of quercetin in lipid microparticles: Effect on photo-and chemical-stability. Pharm. Biomed. Anal. 2009, 49, 90–94.
- Tan, Q.; Liu, W.; Guo, C.; Zhai, G. Design of self-assembling peptides and their biomedical applications. Int. J. Nanomed. 2011, 6, 1621.
- Nan, W.; Ding, L.; Chen, H.; Khan, F.U.; Yu, L.; Sui, X.; Shi, X. Discovery of the consistently well-performed analysis chain for SWATH-MS based pharmacoproteomic quantification. Front. Pharmacol. 2018, 9, 1–11.
- Bose, S.; Michniak-Kohn, B. Preparation and characterization of lipid based nanosystems for topical delivery of quercetin. Eur. J. Pharm. Sci. 2013, 48, 442–452.
- Chessa, M.; Caddeo, C.; Valenti, D.; Manconi, M.; Sinico, C.; Fadda, A.M. Effect of penetration enhancer containing vesicles on the percutaneous delivery of quercetin through new born pig skin. Pharmaceutics 2011, 3, 497–509.
- Caddeo, C.; Díez-Sales, O.; Pons, R.; Fernàndez-Busquets, X.; Fadda, A.M.; Manconi, M. Topical Anti-Inflammatory Potential of Quercetin in Lipid-Based Nanosystems: In Vivo and In Vitro Evaluation. Pharmaceut. Res. 2014, 31, 959–968.
- Chao, Y.; Huang, C.-T.; Fu, L.-T.; Huang, Y.-B.; Tsai, Y.-H.; Wu, P.-C. The Effect of Submicron Emulsion Systems on Transdermal Delivery of Kaempferol. Chem. Pharmaceut. Bull. 2012, 60, 1171–1175.
- Wang, L.; Tu, Y.C.; Lian, T.W.; Hung, J.T.; Yen, J.H.; Wu, M.J. Distinctive Antioxidant and Antiinflammatory Effects of Flavonols. J. Agric. Food Chem. 2006, 54, 9798–9804.
- Simões, S.; Moreira, J.N.; Fonseca, C.; Düzgüneş, N.; de Lima, M.C. On the formulation of pH-sensitive liposomes with long circulation times. Adv. Drug Deliv. Rev. 2004, 56, 947–965.
- Huang, Z.-R.; Hung, C.-F.; Lin, Y.-K.; Fang, J.-Y. In vitro and in vivo evaluation of topical delivery and potential dermal use of soy isoflavones genistein and daidzein. Int. J. Pharm. 2008, 364, 36–44.
- Munyendo, W.L.L.; Zhang, Z.; Abbad, S.; Waddad, A.Y.; Lv, H.; Baraza, L.D.; Zhou, J. Micelles of TPGS modified apigenin phospholipid complex for oral administration: Preparation, in vitro and in vivo evaluation. J. Biomed. Nanotechnol. 2013, 9, 2034–2047.
- Shen, L.N.; Zhang, Y.T.; Wang, Q.; Xu, L.; Feng, N.P. Enhanced in vitro and in vivo skin deposition of apigenin delivered using ethosomes. Int. J. Pharm. 2014, 460, 280–288.
- Karthivashan, G.; Masarudin, M.J.; Umar Kura, A.; Abas, F.; Fakurazi, S. Optimization, formulation, and characterization of multiflavonoids-loaded flavanosome by bulk or sequential technique. Int. J. Nanomed. 2016, 11, 3417–3434.
- Abidin, L.; Mujeeb, M.; Imam, S.S.; Aqil, M.; Khurana, D. Enhanced transdermal delivery of luteolin via non-ionic surfactant-based vesicle: Quality evaluation and anti-arthritic assessment. Drug Deliv. 2016, 23, 1069–1074.
- Shin, K.; Choi, H.; Song, S.K.; Yu, J.W.; Lee, J.Y.; Choi, E.J.; Lee, D.H.; Do, S.H.; Kim, J.W. Nanoemulsion Vehicles as Carriers for Follicular Delivery of Luteolin. ACS Biomat. Sci. Eng. 2018, 4, 1723–1729.
- Avadhani, K.S.; Manikkath, J.; Tiwari, M.; Chandrasekhar, M.; Godavarthi, A.; Vidya, S.M.; Hariharapura, R.C.; Kalthur, G.; Udupa, N.; Mutalik, S. Skin delivery of epigallocatechin-3-gallate (EGCG) and hyaluronic acid loaded nano-transfersomes for antioxidant and anti-aging effects in UV radiation induced skin damage. Drug Deliv. 2017, 4, 61–74.
- Fang, J.Y.; Hung, C.F.; Hwang, T.L.; Huang, Y.L. Physicochemical characteristics and in vivo deposition of liposome-encapsulated tea catechins by topical and intratumor administrations. J. Drug Target 2005, 13, 19–27.
- Fang, J.Y.; Hwang, T.L.; Huang, Y.L.; Fang, C.L. Enhancement of the transdermal delivery of catechins by liposomes incorporating anionic surfactants and ethanol. Int. J. Pharm. 2006, 310, 131–138.
- Bhia, M.; Motallebi, M.; Abadi, B.; Zarepour, A.; Pereira-Silva, M.; Saremnejad, F.; Santos, A.C.; Zarrabi, A.; Melero, A.; Jafari, S.M.; et al. Naringenin Nano-Delivery Systems and Their Therapeutic Applications. Pharmaceutics 2021, 13, 291.
- Nasr, M.; Al-Karaki, R. Nanotechnological Innovations Enhancing the Topical Therapeutic Efficacy of Quercetin: A Succinct Review. Curr. Drug Deliv. 2020, 17, 270–278.
- Guan, F.; Wang, Q.; Bao, Y.; Chao, Y. Anti-rheumatic effect of quercetin and recent developments in nano formulation. RSC Adv. 2021, 11, 7280–7293.
- Scalia, S.; Franceschinis, E.; Bertelli, D.; Iannuccelli, V. Comparative Evaluation of the Effect of Permeation Enhancers, Lipid Nanoparticles and Colloidal Silica on in vivo Human Skin Penetration of Quercetin. Skin Pharmacol. Physiol. 2013, 25, 57–67.
- Sarkar, S.; Mandal, S.; Sinha, J.; Mukhopadhyay, S.; Das, N.; Basu, M.K. Quercetin: Critical evaluation as an antileishmanial agent in vivo in hamsters using different vesicular delivery modes. J. Drug Target 2002, 10, 573–578.
- Hatahet, T.; Morille, M.; Shamseddin, A.; Aubert-Pouëssel, A.; Devoisselle, J.M.; Begu, S. Dermal quercetin lipid nanocapsules: Influence of the formulation on antioxidant activity and cellular protection against hydrogen peroxide. Int. J. Pharm. 2017, 518, 167–176.
- Tan, Q.; Liu, W.; Zhai, G. Preparation and evaluation of quercetin-loaded lecithin-chitosan nanoparticles for topical delivery. Int. J. Nanomed. 2011, 6, 1621–1630.
- Silva, A.P.; Nunes, B.R.; De Oliveira, M.C.; Koester, L.S.; Mayorga, P.; Bassani, V.L.; Teixeira, H.F. Development of topical nanoemulsions containing the isoflavone genistein. Pharmazie 2009, 64, 32–35.
- Carlotti, M.; Sapino, S.; Ugazio, E.; Gallarate, M.; Morel, S.J. Resveratrol in Solid Lipid Nanoparticles. Dispers. Sci. Technol. 2012, 33, 465–471.
- Friedrich, R.B.; Kann, B.; Coradini, K.; Offerhaus, H.L.; Beck, R.C.; Windbergs, M. Skin penetration behavior of lipid-core nanocapsules for simultaneous delivery of resveratrol and curcumin. Eur. J. Pharm. Sci. 2015, 78, 204–213.
- Tavano, L.; Muzzalupo, R.; Picci, N.; de Cindio, B. Co-encapsulation of lipophilic antioxidants into niosomal carriers: Percutaneous permeation studies for cosmeceutical applications. Colloids Surf. B. 2014, 114, 144–149.
- Tsai, Y.; Lee, K.; Huang, Y.; Huang, C. In vitro permeation and in vivo whitening effect of topical hesperetin microemulsion delivery system. Int. J. Pharm. 2010, 388, 257–262.
- Adelli, G.R.; Hingorani, T.; Punyamurthula, N.; Prachetan, S.; Majumdar, S. Evaluation of topical hesperetin matrix film for back-of-the-eye delivery. Eur. J. Pharm. Biopharm. 2015, 92, 74–82.
- Kilor, V.; Sapkal, N.; Vaidya, G. Design and development of novel microemulsion based topical formulation of Hesperidin. Int. J. Pharm. Pharm. Sci. 2015, 7, 142–148.
- Haritima, J. Papr reduction using scs-slm technique in stfbc mimo-ofdm. ARPN J. Eng. Appl. Sci. 2017, 12, 3218–3221.
- Telange, D.R.; Patin, A.T. Formulation and characterization of an apigenin-phospholipid phytosome (APLC) for improved solubility, in vivo bioavailability, and antioxidant potential. Eur. J. Pharm. Sci. 2016, 108, 36–49.
- Priprem, A.; Limsitthichaikoon, S.; Thappasarapong, S.; Complex, A.A. Preparation, Anti-inflammatory Activity of Topical Anthocyanins by Complexation and Niosomal Encapsulation. Int. J. Chem. Mol. Eng. 2015, 9, 133–137.
- Baolin, L.; Weiwei, W.; Ning, T. Topical Application of Luteolin Inhibits Scratching Behavior Associated with Allergic Cutaneous Reaction in Mice. Planta Med. 2005, 71, 424–428.





