Anal stenosis (AS) is defined as anatomical or functional narrowing of the anal canal, which can result from inflammatory bowel diseases, radiation therapy, congenital malformations, or excisional hemorrhoidectomy. The anatomical AS is related to the increased fibrous scar tissue forming, which disables stretching of the anal canal. The leading cause of the anatomical AS is excisional hemorrhoidectomy that is often the chosen treatment for grade III and IV hemorrhoidal disease.
1. Mucosal Advancement Flap
The mucosal advancement flap is mainly preferred for the treatment of mid-level AS. Good functional outcomes have been reported by a couple of studies that include different samples sizes
[1][2]. Rakhmanine et al. reported outcomes of 95 patients in a retrospective study, and the overall complication rate was found to be 3%
[3].
Technical notes of Mucosal advancement flap:
The technique starts with the excision of the scar tissue; then, a transverse incision is made proximally to the dentate line. The rectal mucosa is dissected to the level of submucosa and advanced to the anal canal to cover the excised stricture area. The exterior wound is preferred to be left open to minimize the ectropion formation
[4].
-
2. House Flap
The house flap is recommended if the stenosis extends from the dentate line to the perianal skin. The creation of a wide-based flap increases the anal canal diameter along its length and allows primary closure of the donor site [4]. Alver et al. reported complete healing in all 28 patients [5], whereas Sentovich et al. demonstrated healing rates of 89% with a median follow-up of 28 months [6]. A prospective randomized study revealed a clinical improvement rate of 90% with the house flap when compared to rhomboid flap (80%) and Y-V anoplasty (65%) during 1-year follow-up [7].
Technical notes of House flap:
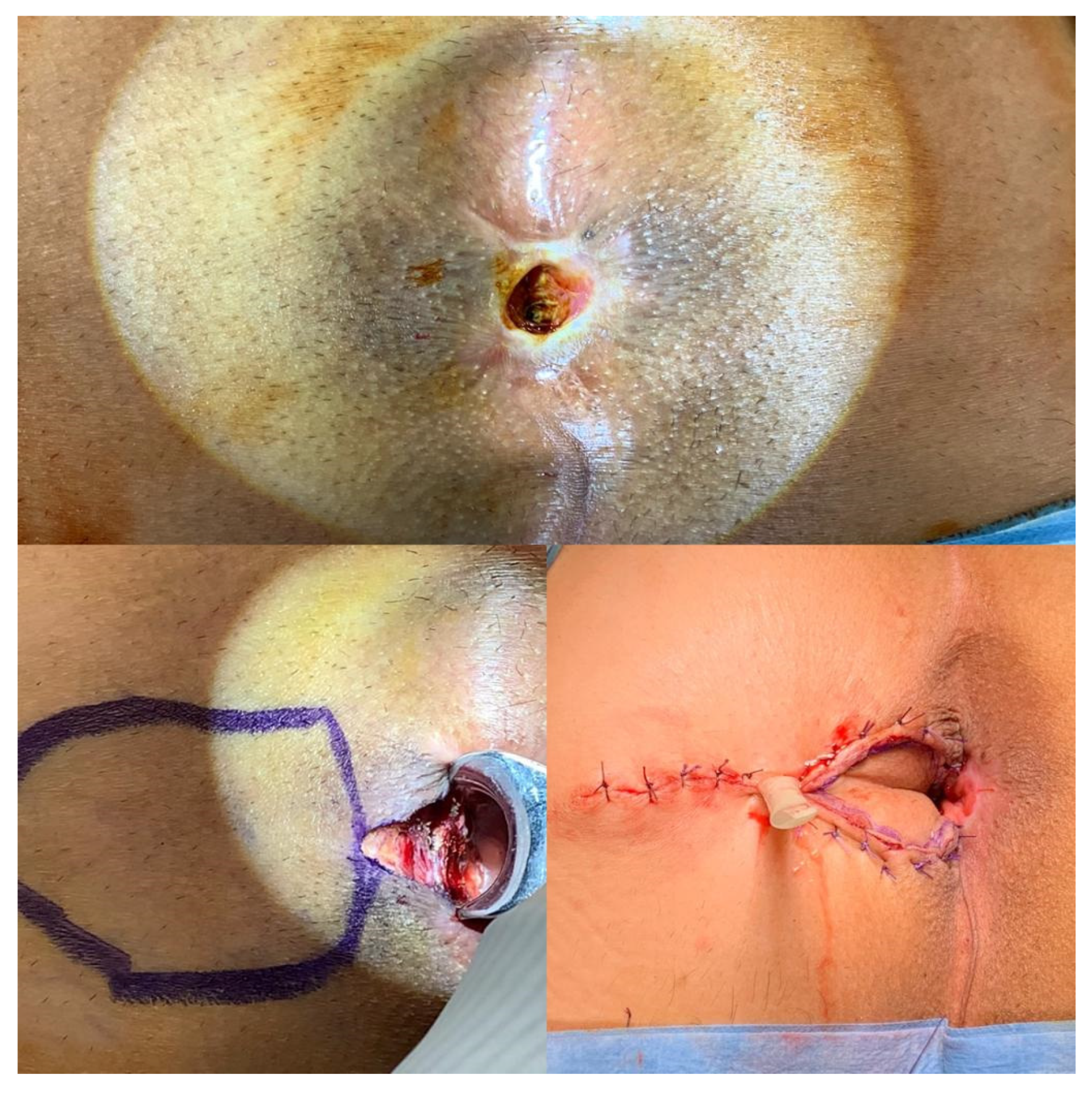
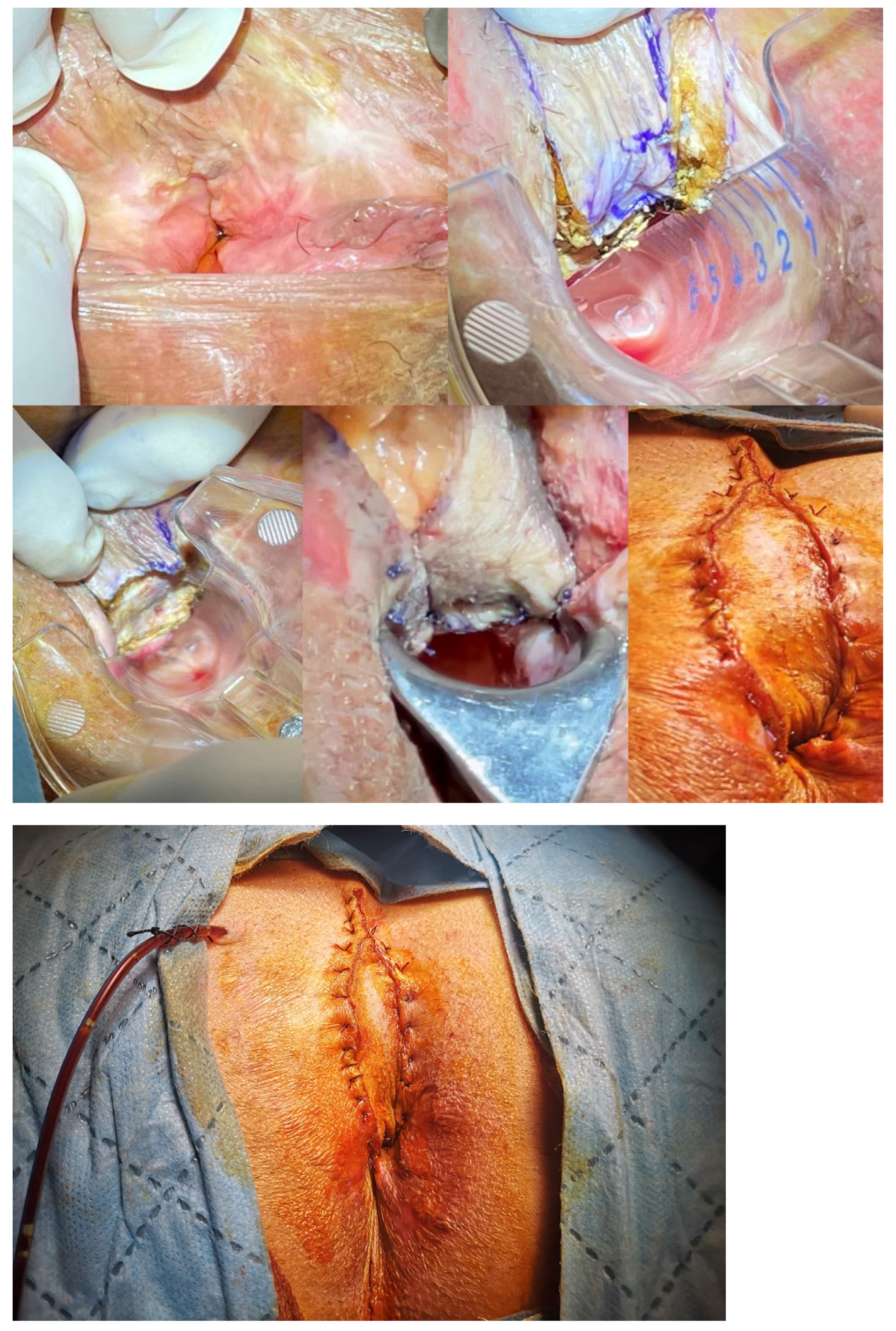
The patient is placed in the prone jack-knife position. The longitudinal incision is made from the dentate line to the end of the stenosis. Then the flap is designed as in the house shape, with the length of the “walls” of the flap corresponding to the length of the incision and the “roof” of the flap reaching the healthy perianal skin (
Figure 1 and
Figure 2). The flap is dissected to the depth of the ischiorectal fat to advance it into the anal canal without tension and to preserve the vascular pedicle
[4][5].
Figure 1. The house flap anoplasty is shown in a patient with severe anal stenosis.
Figure 2. A tailored house flap anoplasty in a patient with chronic unhealing wound in the posterior anal canal.
3. Diamond Flap
The diamond flap was first described by Caplin and Kodner in 1986 and has been performed for the treatment of moderate and severe AS
[8]. Although the final target for anal caliber has not been standardized, Gulen et al. reported a clinical success rate of 88.9% with an eventual anal caliber of 25 to 26 mm in 18 consecutive patients. After 12-months of follow-up, the obstructed defecation syndrome scores were found to be significantly improved
[9].
Technical notes of Diamond flap:
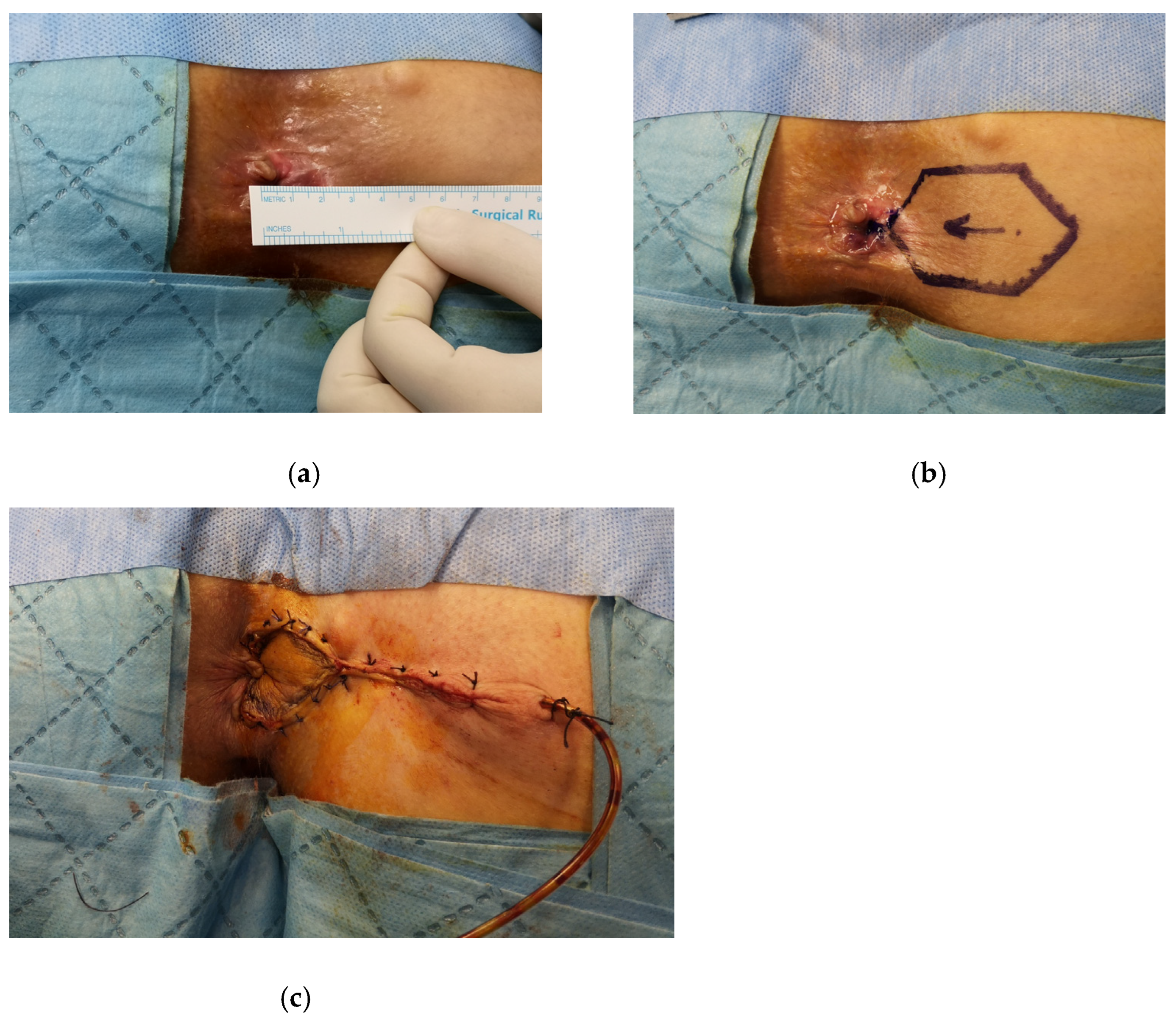
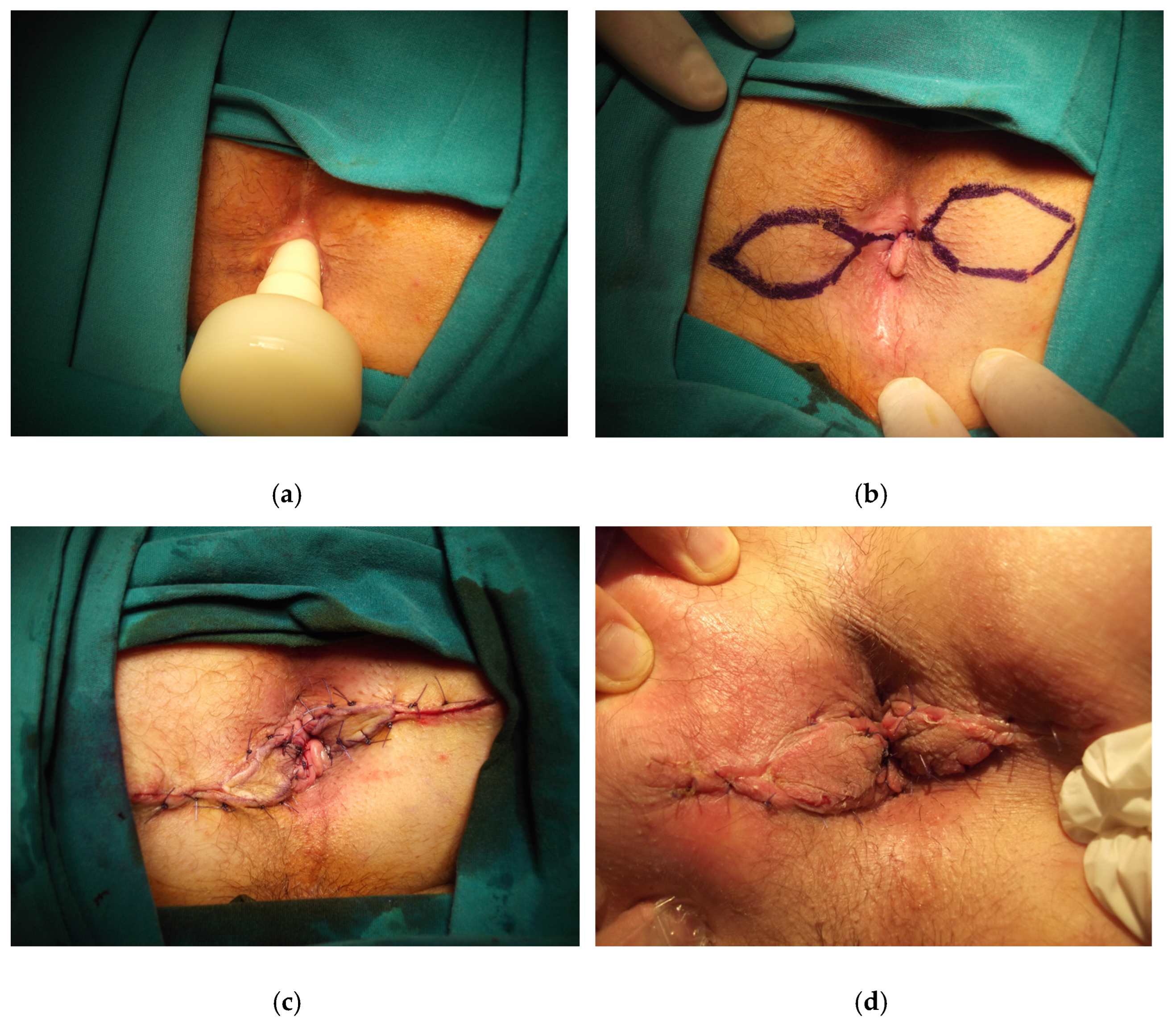
The patient is placed in the prone jack-knife position. The incision is made on the scar tissue longitudinally until it reaches the dentate line. The anal caliber is recommended to be checked during this step, and the external sphincter should be spared
[10]. The diamond flap is designed as adjacent to the diseased anal canal. The flap is dissected out together with its vascular pedicle and advanced into the anal canal. The flap should be tension-free to avoid any postoperative wound complications (
Figure 3,
Figure 4 and
Figure 5).
Figure 3. The diamond flap anoplasty is shown in a patient with severe anal stenosis, (a) the anal caliber is measured as 10 mm, (b) the right-sided anoplasty is decided according to the location of scar tissue in the anal verge, (c) the anoplasty is performed and the negative pressure drain is placed.
Figure 4. Contralateral diamond flap anoplasty in a patient with recurrent anal stenosis.
Figure 5. Bilateral diamond flap anoplasty in severe anal stenosis is shown, (a) the anal caliber is measured using an anal calibrator, (b) the technique is drawn, (c) the postoperative image after anoplasty, (d) the image in postoperative 1st week.
-
4. Y-V flap/V-Y Flap
The Y-V advancement flap is performed for low and localized strictures below the dentate line, whereas the V-Y flap is used for mild to severe stricture at the dentate line
[4]. Maria et al. reported 29 patients who had Y-V anoplasty in a comparative study with diamond flap, with a healing rate of 90% and an ischemic contracture of the leading edge of the flap and wound dehiscence in two patients
[11]. The authors suggested that the diamond flap is a more reliable technique due to the reduced tension in the suture line and the better blood supply of the flap. Farid et al. observed less clinical improvement (65%) and higher ischemic wound complications (15%) with this technique
[7].
Technical notes of Y-V flap/V-Y flap:
Initially, the vertical limb of the Y is performed to the area of stricture. The incision is extended to the perianal skin in two directions creating a V shape. Then, the tip of the V is advanced to the vertical limb of the Y incision. It can also be done in either a lateral position or just in the posterior midline. The main disadvantage regarding this technique is the tip of the V flap being prone to ischemic necrosis
[12].
For the V-Y advancement flap, the first few steps are the same as the Y-V flap, but in this procedure, the wider base of the triangular Y flap is sutured to the dentate line. Then the perianal skin is approximated with sutures longitudinally behind the V shape to form the Y shape
[4].
-
4.1. Rhomboid Flap/Modified Rhomboid Flap
The rhomboid flap has been modified in terms of the flap size to be adjusted to each patient. Sloane et al. observed good functional results in a case series including nine patients, eight of whom underwent bilateral rhomboid flap with complete resolution of symptoms
[13]. The modified rhomboid flap is demonstrated as a safe and suitable technique for the treatment of moderate and severe AS. Gallo et al. reported 0% recurrence rate and 96% success rate in a study with 50 consecutive patients, and significant improvement in the obstructed defecation syndrome scores and the quality of life were observed at 12 months
[14]. The mean anal caliber was found to be 24 mm and significantly different compared to the preoperative measurement.
Technical notes of Rhomboid flap/Modified rhomboid flap:
The size of the rhomboid flap can vary between 8 to 9 cm in length and 5 cm in width at its largest point. A minimal left/right internal sphincterotomy can be performed by paying careful attention to the external sphincter. Then, the flap is relocated in the anal canal and fixed with a single-layer suture of absorbable stitches to the distal rectum. The skin sutures should be adequately spaced to avoid excessive tension with subsequent ischemia
[14].
-
4.2. U-Flap
The U-flap technique is mainly used for the treatment of AS with mucosal ectropion. The disadvantage of this technique is that the donor site is left open
[4]. Pearl et al. reported a good clinical result of 92% in 25 patients during a mean follow-up of 19 months
[15].
Technical notes of U-flap:
The procedure starts with the excision of the ectropion; then, a U-shaped incision is made at the adjacent perianal skin. The U flap is advanced into the anal canal to cover the wide defect resulting from the excised area of ectropion.
-
4.3. Rotational S-Plasty
Rotational S-plasty was first described by Ferguson in 1959 for the repair of the whitehead deformity of the anus
[16]. Corman et al. in 1976 adapted this technique for the treatment of AS
[17]. This technique enables covering large areas of skin with an adequate blood supply. Gonzalez et al. revealed that 94% of patients had good results during a mean follow-up of 18 months
[18].
Technical notes of Rotational S-plasty:
The technique starts with outlining the semicircular incision in the perianal skin, with a length of 12 to 13 cm. The base of the incision should not be shorter than its length. Then skin incision is done to the layer of subcutaneous fat lobules to preserve the blood supply of the skin flaps. The flap is then rotated and fixed to the mucosa by interrupted sutures
[19].