
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Wu Yurong | -- | 2626 | 2022-04-08 09:28:25 | | | |
| 2 | Lindsay Dong | Meta information modification | 2626 | 2022-04-08 09:40:20 | | |
Video Upload Options
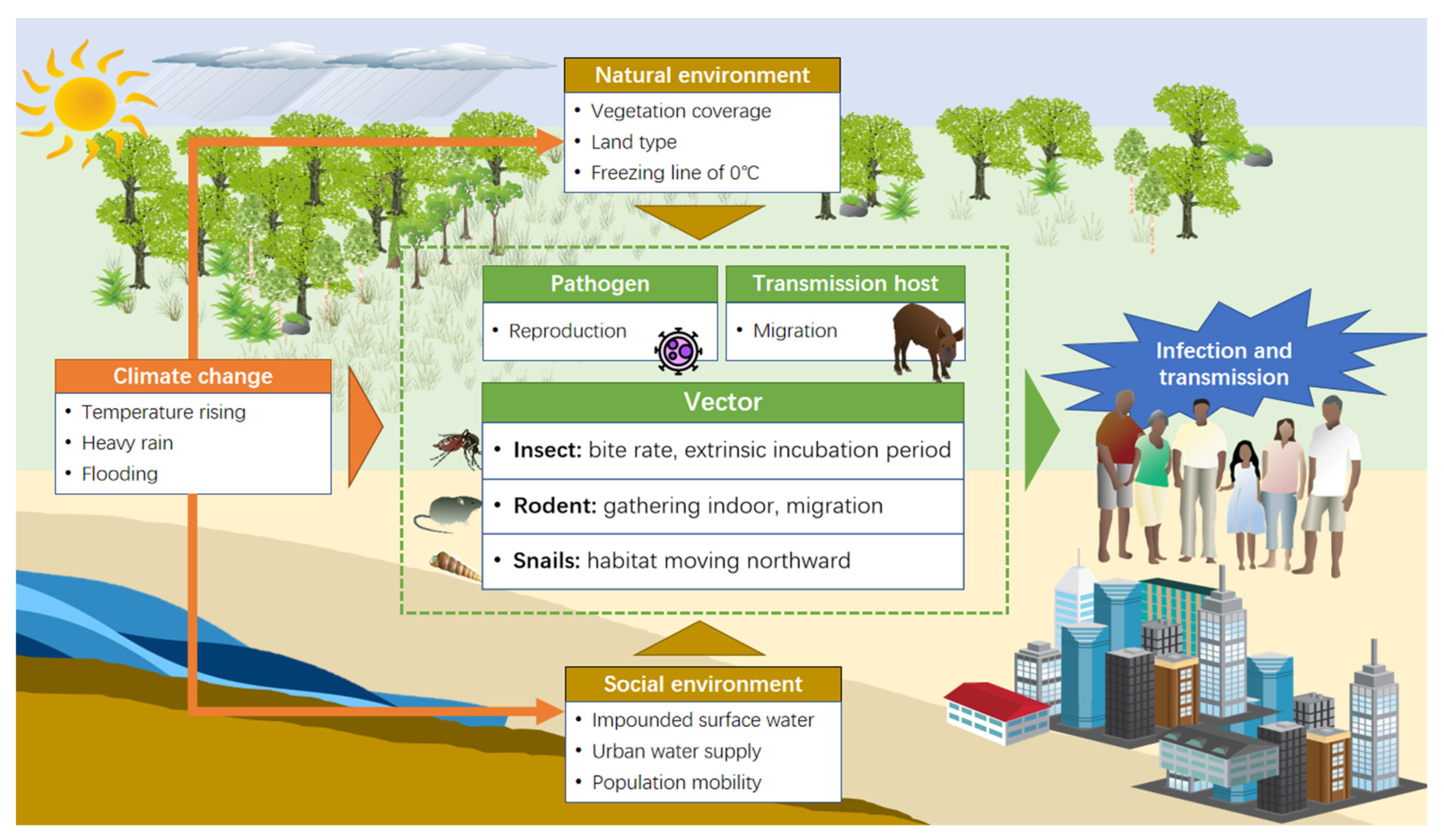
Vector-borne diseases are among the most rapidly spreading infectious diseases and are widespread all around the world. In China, many types of vector-borne diseases have been prevalent in different regions, which is a serious public health problem with significant association with meteorological factors and weather events. Under the background of current severe climate change, the outbreaks and transmission of vector-borne diseases have been proven to be impacted greatly due to rapidly changing weather conditions.
1. Introduction
2. Climate Change and Vector-Borne Diseases in China
2.1. The Relationship between Meteorological Factors and Vector-Borne Diseases
2.2. Potential Pathway of Meteorological Factors on Vector-Borne Diseases
2.3. The Regional Differentiation of the Relationship between Meteorological Factors and Vector-Borne Diseases
| Disease | Area | Time Period | Meteorological Factors | ||
|---|---|---|---|---|---|
| Temperature | Precipitation | Humidity | |||
| Malaria | Shandong | ||||
| Jinan City | 1959–1979 | Max T (+) ** | P (+) | H (+) * | |
| Min T (+) ** | |||||
| Henan | |||||
| Yongcheng County | 2006–2010 | Monthly avg max T (+) *** | - | Monthly avg H (+) ** | |
| Anhui | 1990–2009 | Monthly avg T(+) * | Monthly avg P (+) ** | Monthly avg RH (+) * | |
| Shuchen County | 1980–1991 | Monthly avg max T (+) *** Monthly avg min T (+) *** |
Monthly P (+) *** | Monthly avg RH (+) *** | |
| Hefei city | 1999–2009 | Monthly avg T (+) Monthly avg max T (+) *** Monthly avg min T (+) *** |
P (+) * | H (+) *** | |
| Hefei City | 1990–2011 | Monthly min T (+) *** | P | RH (+) *** | |
| Yunnan | |||||
| Mengla County | 1971–1999 | Monthly max T (+) * Monthly min T (+) * |
Monthly P (−) | Monthly RH (−) | |
| 125 counties | 2012 | Yearly avg T (+) ** | Yearly P (+) ** | ||
| Guangdong | 2005–2013 | High T (+) | P (J) | - | |
| Guangzhou city | 2006–2012 | Daily avg T (+) * | - | Daily RH (+) * | |
| Hainan | 1995–2008 | Monthly avg T (+) * Monthly avg max T (+) * Monthly min T (+) * |
Monthly total P (+) * | - | |
| Dengue | Guangdong | ||||
| Guangzhou City | 2006–2015 | Extremely high T (+) * | Extremely high P (+) * | Extremely high H (+) * | |
| Guangzhou City | 2005–2015 | Monthly avg max T (+) ** | Monthly total P (+) ** | - | |
| Guangzhou City | 2007–2012 | Monthly avg T (+) ** | - | Monthly avg RH (+) ** | |
| Guangzhou City | 2001–2006 | Min T (+) *** | Monthly total P (+) | Min H (+) | |
| Guangzhou City | 2000–2012 | Monthly avg min T (+) * | Monthly total P (+) * | Monthly avg RH (+) * | |
| Guangzhou City | 2005–2011 | Daily avg T (+) * Daily min T (+) * Daily max T (−) * |
Daily P (+) | Daily H (+) | |
| Zhongshan City | 2001–2013 | Monthly max T (+) * Monthly max DTR (+) * |
- | Monthly avg RH (+) * Monthly max RH (+) * |
|
| Fujian | 1978–2017 | Monthly avg T (+) * | Monthly total P (+) * | - | |
| Guangxi | 1978–2017 | Monthly avg T (+) * | Monthly total P (+) * | - | |
| Yuanan | 1978–2017 | Monthly avg T (+) * | Monthly total P (+) * | - | |
| Japanese encephalitis | Shandong | ||||
| Jinan City | 1959–1979 | Monthly avg max T (+) *** Monthly avg min T (+) *** |
Monthly total P (+) * | Monthly avg RH (+) *** | |
| Linyi City | 1956–2004 | Monthly min T (+) ** | - | Monthly avg RH (+) * | |
| Shannxi | 2006–2014 | Monthly min T (−) | Monthly P (+) | - | |
| Anhui | |||||
| Jieshou County | 1980–1996 | Monthly avg max T (+) * Monthly avg min T (+) * |
Monthly total P (+) ** | - | |
| Hunan | |||||
| Changsha city | 2004–2009 | Monthly avg max T (+) * Monthly avg min T (+) * |
Monthly total P (+) * | Monthly avg AH (+) * | |
| Sichuan | |||||
| Nanchong City | 2007–2012 | Daily avg T (+) * | - | Daily avg RH (+) * | |
| Chongqin | |||||
| 12 counties along the Yangtze River | 1997–2008 | Monthly avg T (+) *** | Monthly total P (−) *** | - | |
| Scrub typhus | Shandong | 2006–2013 | Monthly avg T (reversed U) *** | Monthly total P (−) *** | Monthly avg RH (−) *** |
| Laiwu City | 2006–2012 | Monthly avg T (+) ** | Monthly avg P (+) ** | Monthly avg RH (+) ** | |
| Anhui | 2006–2013 | Monthly avg T (reversed U) *** | Monthly total P (−) *** | Monthly avg RH (+) *** | |
| Jiangsu | 2006–2013 | Monthly avg T (reversed U) *** | Monthly total P (−) *** | Monthly avg RH (+) *** | |
| Yancheng City | 2005–2014 | Monthly avg min T (+) *** | Monthly total P (+) *** | Monthly avg RH (−) *** | |
| Guangdong | |||||
| Guangzhou City | 2006–2012 | Daily avg T (+) ** | Daily P (+) ** | Daily avg RH (−) * | |
| Typhus group rickettsiosis | Yunan | ||||
| Xishuangbanna | 2005–2017 | Weekly avg T (J) * | Weekly avg P (reversed U) * | - | |
| SFTS | Jiangsu | 2010–2016 | Max T in warmest month (+) * | P in warmest month (+) * | - |
| Leishmaniasis | Xinjiang | ||||
| Jiashi County | 2005–2015 | Monthly avg T (+) ** | Monthly total P | Monthly avg RH (−) ** | |
| Plague | Gansu | ||||
| Sunan County, Subei County | 1973–2016 | Monthly avg T (+) * | Monthly avg P (+) * | Monthly avg RH (−) * | |
| Yunnan | 1982–2013 | Extreme max T (−) ** | - | Avg RH (+) ** | |
| HFRS | Guizhou | 1982–2013 | Extreme max T (−) ** | - | Avg RH (+) ** |
| Guangxi | 1982–2013 | Extreme max T (−) ** | - | Avg RH (+) ** | |
| Liaoning | 2005–2014 | Weekly max T (+) * | Weekly P (+) * | Weekly avg RH (+) * | |
| Shenyang City | 2004–2009 | Monthly avg T (−) * Monthly avg max T (−) * Monthly avg min T (−) * |
Monthly total P (−) * | Monthly avg RH (−) * | |
| Heilongjiang | 2005–2014 | Weekly max T (+) * | Weekly P (+) * | Weekly avg RH (+) * | |
| Anhui | 2005–2014 | Weekly max T (+) * | Weekly P (+) * | Weekly avg RH (+) * | |
| Schistosomiasis | Hubei | 1976–1989 | Avg T in July (−) * | Avg P in July (−) * | - |
| Anhui | 1997–2010 | Monthly avg T (−) * | Monthly total P (−) * | ||
| Jiangxi | 2008 | - | Monthly min P (−) ** Monthly max P (−) ** |
||
3. Summary
The most significant health threat faced from climate-related vector-borne diseases in China is mosquito-borne diseases, while the concern and health threat from rodent-borne diseases is decreasing. Aedes aegypti and Aedes albopictus are the main mosquito vectors transmitting viruses. Globally, Aedes aegypti, mainly distributed in South America, play an active role in increasing Zika transmission risks. Aedes albopictus, on the other hand, is mainly distributed in the southeastern United States, southern China, and the northern summer season in southern Europe; it is the main vector of mosquito-borne diseases in China [62]. In the last few decades, the mosquito-borne disease malaria once posed a high infection risk in China. However, on June 3th 2021, China was declared malaria-free by the World Health Organization, although today 40% of the world’s population still lives in malaria-endemic regions, with Africa being the most severe malaria-endemic region. Within the past few years, dengue fever has become the most important mosquito-borne disease health threat facing China, especially in Guangdong Province. The transmission risk of dengue is significantly increasing since it has been spreading from the coastal areas of southern China to northern areas in recent years [63].
References
- Coronavirus Disease (COVID-19): Climate Change. 2020. Available online: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-climate-change (accessed on 22 April 2020).
- Semenza, J.C.; Paz, S. Climate change and infectious disease in Europe: Impact, projection and adaptation. Lancet Reg. Health Eur. 2021, 9, 100230.
- Franklinos, L.H.V.; Jones, K.E.; Redding, D.W.; Abubakar, I. The effect of global change on mosquito-borne disease. Lancet Infect. Dis. 2019, 19, e302–e312.
- Vector-Borne Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/vector-borne-diseases (accessed on 2 March 2020).
- Rocklöv, J.; Dubrow, R. Climate change: An enduring challenge for vector-borne disease prevention and control. Nat. Immunol. 2020, 21, 479–483.
- Ogden, N.H.; Radojevic, M.; Wu, X.; Duvvuri, V.R.; Leighton, P.A.; Wu, J. Estimated effects of projected climate change on the basic reproductive number of the Lyme disease vector Ixodes scapularis. Environ. Health Perspect. 2014, 122, 631–638.
- Fischer, D.; Thomas, S.M.; Suk, J.E.; Sudre, B.; Hess, A.; Tjaden, N.B.; Beierkuhnlein, C.; Semenza, J.C. Climate change effects on Chikungunya transmission in Europe: Geospatial analysis of vector’s climatic suitability and virus’ temperature require-ments. Int. J. Health Geogr. 2013, 12, 51.
- Fouque, F.; Reeder, J.C. Impact of past and on-going changes on climate and weather on vector-borne diseases transmission: A look at the evidence. Infect. Dis. Poverty 2019, 8, 51.
- Semenza, J.C.; Suk, J.E. Vector-borne diseases and climate change: A European perspective. FEMS Microbiol. Lett. 2018, 365, fnx244.
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Beagley, J.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D.; et al. The 2020 report of The Lancet Countdown on health and climate change: Responding to converging crises. Lancet 2021, 397, 129–170.
- Climate Change Center of China Meteorological Administration. Blue Book on Climate Change in China (2020); China Meteorological Administration: Beijing, China, 2020.
- Xu, J.; Xu, K.; Li, Z.; Ayeb-Karlsson, S.; Beagley, J.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D.; et al. Forecast of Dengue Cases in 20 Chinese Cities Based on the Deep Learning Method. Int. J. Environ. Res. Public Health 2020, 17, 453.
- Gao, Y.; Niu, Y.; Sun, W.; Liu, K.; Liu, X.; Zhao, N.; Yue, Y.; Wu, H.; Meng, F.; Wang, J.; et al. Climate factors driven typhus group rickettsiosis incidence dynamics in Xishuangbanna Dai autonomous prefecture of Yunnan province in China, 2005–2017. Environ. Health 2020, 19, 3.
- Yi, B.; Zhang, Z.; Xu, D.; Xi, Y. Relationship of dengue fever epidemic to Aedes density changed by climate factors in Guangdong Province. Wei Sheng Yan Jiu 2003, 32, 152–154.
- Liu, Z.; Zhang, Y.; Tong, M.X.; Zhang, Y.; Xiang, J.; Gao, Q.; Wang, S.; Sun, S.; Jiang, B.; Bi, P. Nonlinear and Threshold Effect of Meteorological Factors on Japanese Encephalitis Transmission in Southwestern China. Am. J. Trop. Med. Hyg. 2020, 103, 2442–2449.
- Cao, L.; Huo, X.; Xiang, J.; Lu, L.; Liu, X.; Song, X.; Jia, C.; Liu, Q. Interactions and marginal effects of meteorological factors on haemorrhagic fever with renal syndrome in different climate zones: Evidence from 254 cities of China. Sci. Total Environ. 2020, 721, 137564.
- Chen, Y.Z.; Li, F.; Xu, H.; Huang, L.C.; Gu, Z.G.; Sun, Z.Y.; Yan, G.J.; Zhu, Y.J.; Tang, C. Spatio-temporal distribution of scrub typhus and related influencing factors in coastal beach area of Yancheng, China. Zhonghua Liu Xing Bing Xue Za Zhi 2016, 37, 232–237.
- Liu, X.; Jiang, B.; Gu, W.; Liu, Q. Temporal trend and climate factors of hemorrhagic fever with renal syndrome epidemic in Shenyang City, China. BMC Infect. Dis. 2011, 11, 331.
- Zhai, J.X.; Lu, Q.; Hu, W.B.; Tong, S.L.; Wang, B.; Yang, F.T.; Xu, Z.W.; Xun, S.P.; Shen, X.H. Development of an empirical model to predict malaria outbreaks based on monthly case reports and climate variables in Hefei, China, 1990–2011. Acta Trop. 2018, 178, 148–154.
- Wang, L.; Hu, W.; Magalhaes, R.J.S.; Bi, P.; Ding, F.; Sun, H.; Li, S.; Yin, W.; Wei, L.; Liu, Q.; et al. The role of environmental factors in the spatial distribution of Japanese encephalitis in mainland China. Environ. Int. 2014, 73, 1–9.
- Li, T.; Yang, Z.; Dong, Z.; Bi, P.; Ding, F.; Sun, H.; Li, S.; Yin, W.; Wei, L.; Liu, Q.; et al. Meteorological factors and risk of scrub typhus in Guangzhou, southern China, 2006–2012. BMC Infect. Dis. 2014, 14, 139.
- Cheng, J.; Bambrick, H.; Yakob, L.; Devine, G.; Frentiu, F.D.; Williams, G.; Li, Z.; Yang, W.; Hu, W. Extreme weather conditions and dengue outbreak in Guangdong, China: Spatial heterogeneity based on climate variability. Environ. Res. 2021, 196, 110900.
- Li, C.; Zhao, Q.; Zhao, Z.; Liu, Q.; Ma, W. The association between tropical cyclones and dengue fever in the Pearl River Delta, China during 2013–2018: A time-stratified case-crossover study. PLoS Negl. Trop. Dis. 2021, 15, e0009776.
- Chan, E.Y.Y.; Lo, E.S.K.; Huang, Z.; Lam, H.C.Y.; Yeung, M.P.-S.; Kwok, K.-O.; Hung, K.K.C.; Tse, S.L.-A. Sociodemographic predictors of knowledge, mosquito bite patterns and protective behaviors concerning vector borne disease: The case of dengue fever in Chinese subtropical city, Hong Kong. PLoS Negl. Trop. Dis. 2021, 15, e0008993.
- Cai, W.; Zhang, C.; Suen, H.P.; Ai, S.; Bai, Y.; Bao, J.; Chen, B.; Cheng, L.; Cui, X.; Dai, H.; et al. The 2020 China report of the Lancet Countdown on health and climate change. Lancet Public Health 2020, 6, e64–e81.
- Song, Y.; Ge, Y.; Wang, J.; Ren, Z.; Liao, Y.; Peng, J. Spatial distribution estimation of malaria in northern China and its scenarios in 2020, 2030, 2040 and 2050. Malar. J. 2016, 15, 345.
- Sun, Y.; Fang, L.Q.; Cao, W.C. Study on the epidemiological characteristics and influencing factors of scrub typhus in the autumn-winter natural foci, from 2006 to 2013. Zhonghua Liu Xing Bing Xue Za Zhi 2016, 37, 1112–1116.
- Hou, X.; Liu, K.K.; Liu, X.B.; Gang, C.; Lei, X.; Qiyong, L. Nonlinear effects of climate factors on dengue epidemic in Guangdong province, China. Chin. J. Vector Biol. Control 2019, 30, 25–30.
- Lu, L.; Lin, H.; Tian, L.; Yang, W.; Sun, J.; Liu, Q. Time series analysis of dengue fever and weather in Guangzhou, China. BMC Public Health 2009, 9, 395.
- Xiang, J.; Hansen, A.; Liu, Q.; Tong, M.X.; Liu, X.; Sun, Y.; Cameron, S.; Hanson-Easey, S.; Han, G.-S.; Williams, C.; et al. Impact of meteorological factors on hemorrhagic fever with renal syndrome in 19 cities in China, 2005–2014. Sci. Total Environ. 2018, 636, 1249–1256.
- Liu, K.K.; Wang, T.; Huang, X.D.; Wang, G.-L.; Xia, Y.; Zhang, Y.-T.; Jing, Q.-L.; Huang, J.-W.; Liu, X.-X.; Lu, J.-H.; et al. Risk assessment of dengue fever in Zhongshan, China: A time-series regression tree analysis. Epidemiol. Infect. 2017, 145, 451–461.
- Bi, Y.; Yu, W.; Hu, W.; Lin, H.; Guo, Y.; Zhou, X.-N.; Tong, S. Impact of climate variability on Plasmodium vivax and Plasmodium falciparum malaria in Yunnan Province, China. Parasites Vectors 2013, 6, 357.
- Tian, H.Y.; Bi, P.; Cazelles, B.; Zhou, S.; Huang, S.-Q.; Yang, J.; Pei, Y.; Wu, X.-X.; Fu, S.-H.; Tong, S.-L.; et al. How environmental conditions impact mosquito ecology and Japanese encephalitis: An eco-epidemiological approach. Environ. Int. 2015, 79, 17–24.
- Yang, L.P.; Liu, J.; Wang, X.J.; Ma, W.; Jia, C.X.; Jiang, B.F. Effects of meteorological factors on scrub typhus in a temperate region of China. Epidemiol. Infect. 2014, 142, 2217–2226.
- Gao, F.; Ward, M.P.; Wang, Y.; Zhang, Z.; Hu, Y. Implications from assessing environmental effects on spatio-temporal pattern of schistosomiasis in the Yangtze Basin, China. Geospat. Health 2018, 13, 1–6.
- Zhang, Y.; Wang, T.; Liu, K.; Xia, Y.; Lu, Y.; Jing, Q.; Yang, Z.; Hu, W.; Lu, J. Developing a Time Series Predictive Model for Dengue in Zhongshan, China Based on Weather and Guangzhou Dengue Surveillance Data. PLoS Negl. Trop. Dis. 2016, 10, e0004473.
- Huang, F.; Zhou, S.; Zhang, S.; Zhang, H.; Li, W. Meteorological factors-based spatio-temporal mapping and predicting malaria in central China. Am. J. Trop. Med. Hyg. 2011, 85, 560–567.
- Liu, J.; Xue, F.Z.; Wang, J.Z.; Liu, Q.Y. Association of haemorrhagic fever with renal syndrome and weather factors in Junan County, China: A case-crossover study. Epidemiol. Infect. 2013, 141, 697–705.
- Gu, H.; Leung, R.K.; Jing, Q.; Zhang, W.; Yang, Z.; Lu, J.; Hao, Y.; Zhang, D. Meteorological Factors for Dengue Fever Control and Prevention in South China. Int. J. Environ. Res. Public Health 2016, 13, 867.
- Xu, L.; Stige, L.C.; Kausrud, K.L.; Ari, T.B.; Wang, S.; Fang, X.; Schmid, B.V.; Liu, Q.; Stenseth, N.C.; Zhang, Z. Wet climate and transportation routes accelerate spread of human plague. Proc. Biol. Sci. 2014, 281, 20133159.
- Li, T.G.; Yang, Z.C.; Luo, L.; Di, B.; Wang, M. Dengue Fever epidemiological status and relationship with meteorological variables in Guangzhou, Southern China, 2007–2012. Biomed. Environ. Sci. 2013, 26, 994–997.
- Guo, C.; Yang, L.; Ou, C.Q.; Li, L.; Zhuang, Y.; Yang, J.; Zhou, Y.-X.; Qian, J.; Chen, P.-Y.; Liu, Q.-Y. Malaria incidence from 2005-2013 and its associations with meteorological factors in Guangdong, China. Malar. J. 2015, 14, 116.
- Huang, C.R.; Deng, S.Z. Climate change may increase the risk of emerging infectious diseases. J. Shandong Univ. Health Sci. 2020, 58, 1–6.
- Fan, J.; Lin, H.; Wang, C.; Bai, L.; Yang, S.; Chu, C.; Yang, W.; Liu, Q. Identifying the high-risk areas and associated meteorological factors of dengue transmission in Guangdong Province, China from 2005 to 2011. Epidemiol. Infect. 2014, 142, 634–643.
- Bangs, M.J.; Larasati, R.P.; Corwin, A.L.; Wuryadi, S. Climatic factors associated with epidemic dengue in Palembang, Indonesia: Implications of short-term meteorological events on virus transmission. Southeast Asian J. Trop. Med. Public Health 2006, 37, 1103–1116.
- Wang, C.; Jiang, B.; Fan, J.; Wang, F.; Liu, Q. A study of the dengue epidemic and meteorological factors in Guangzhou, China, by using a zero-inflated Poisson regression model. Asia Pac. J. Public Health 2014, 26, 48–57.
- Zhang, F.; Liu, Z.; Zhang, C.; Jiang, B. Short-term effects of floods on Japanese encephalitis in Nanchong, China, 2007–2012: A time-stratified case-crossover study. Sci. Total Environ. 2016, 563, 1105–1110.
- Jetten, T.H.; Focks, D.A. Potential changes in the distribution of dengue transmission under climate warming. Am. J. Trop. Med. Hyg. 1997, 57, 285–297.
- Fan, W.J.; Lu, Q.; Yang, F.T. Relationship between morbidity of Plasmodium vivax malaria infection and meteorologicaI factors in Hefei City of Anhui Province in 1999–2009. China Trop. Med. 2012, 12, 1058–1061.
- Hu, F.; Liu, Y.M.; Li, Z.J.; Yuan, M. Effect of environmental factors on temporal and spatial distribution of schistosomiasis in Poyang Lake region. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi 2012, 24, 393–396, 403.
- Yang, G.J.; Vounatsou, P.; Zhou, X.N.; Tanner, M.; Utzinger, J. A potential impact of climate change and water resource development on the transmission of Schistosoma japonicum in China. Parassitologia 2005, 47, 127–134.
- Yang, G.J.; Gemperli, A.; Vounatsou, P.; Tanner, M.; Zhou, X.-N.; Utzinger, J. A growing degree-days based time-series analysis for prediction of Schistosoma japonicum transmission in Jiangsu province, China. Am. J. Trop. Med. Hyg. 2006, 75, 549–555.
- Li, Y.; Zheng, C. Associations between Meteorological Factors and Visceral Leishmaniasis Outbreaks in Jiashi County, Xinjiang Uygur Autonomous Region, China, 2005–2015. Int. J. Environ. Res. Public Health 2019, 16, 1775.
- Zhang, S.; Hu, W.; Qi, X.; Zhuang, G. How Socio-Environmental Factors Are Associated with Japanese Encephalitis in Shaanxi, China-A Bayesian Spatial Analysis. Int. J. Environ. Res. Public Health 2018, 15, 608.
- Liu, K.; Sun, J.; Liu, X.; Li, R.; Wang, Y.; Lu, L.; Wu, H.; Gao, Y.; Xu, L.; Liu, Q. Spatiotemporal patterns and determinants of dengue at county level in China from 2005–2017. Int. J. Infect. Dis. 2018, 77, 96–104.
- Lin, H.; Yang, L.; Liu, Q.; Wang, T.; Hossain, S.R.; Ho, S.C.; Tian, L. Time series analysis of Japanese encephalitis and weather in Linyi City, China. Int. J. Public Health 2012, 57, 289–296.
- Wu, Y.; Qiao, Z.; Wang, N.; Yu, H.; Feng, Z.; Li, X.; Zhao, X. Describing interaction effect between lagged rainfalls on malaria: An epidemiological study in south-west China. Malar. J. 2017, 16, 53.
- Chen, S.C.; Liao, C.M.; Chio, C.P.; Chou, H.-H.; You, S.-H.; Cheng, Y.-H. Lagged temperature effect with mosquito transmission potential explains dengue variability in southern Taiwan: Insights from a statistical analysis. Sci. Total Environ. 2010, 408, 4069–4075.
- Teklehaimanot, H.D.; Lipsitch, M.; Teklehaimanot, A.; Schwartz, J. Weather-based prediction of Plasmodium falciparum malaria in epidemic-prone regions of Ethiopia, I. Patterns of lagged weather effects reflect biological mechanisms. Malar. J. 2004, 3, 41.
- Li, X.; Gao, X.; Ren, Z.; Cao, Y.; Wang, J.; Liang, G. A spatial and temporal analysis of Japanese encephalitis in mainland China, 1963-1975: A period without Japanese encephalitis vaccination. PLoS ONE 2014, 9, e99183.
- Xu, L.; Liu, Q.; Stige, L.C.; Ari, T.B.; Fang, X.; Chan, K.S.; Wang, S.; Stenseth, N.C.; Zhang, Z. Nonlinear effect of climate on plague during the third pandemic in China. Proc. Natl. Acad. Sci. USA 2011, 108, 10214–10219.
- Butterworth, M.K.; Morin, C.W.; Comrie, A.C. An Analysis of the Potential Impact of Climate Change on Dengue Transmission in the Southeastern United States. Environ. Health Perspect. 2017, 125, 579–585.
- Li, C.; Wu, X.; Sheridan, S.; Lee, J.; Wang, X.; Yin, J.; Han, J. Interaction of climate and socio-ecological environment drives the dengue outbreak in epidemic region of China. PLoS Negl. Trop. Dis. 2021, 15, e0009761.
- Sun, W.; Liu, X.; Li, W.; Mao, Z.; Sun, J.; Lu, L. Effects and interaction of meteorological factors on hemorrhagic fever with renal syndrome incidence in Huludao City, northeastern China, 2007–2018. PLoS Negl. Trop. Dis. 2021, 15, e0009217.
- Yang, Z.; Jing, Q.; Huang, J.; Huang, J.; Guo, C.; Yang, K.; Chen, A.; Lu, J. Effects of natural and socioeconomic factors on dengue transmission in two cities of China from 2006 to 2017. Sci. Total Environ. 2020, 724, 138200.
- Liu, X.; Liu, K.; Yue, Y.; Wu, H.; Yang, S.; Guo, Y.; Ren, D.; Zhao, N.; Yang, J.; Liu, Q. Determination of Factors Affecting Dengue Occurrence in Representative Areas of China: A Principal Component Regression Analysis. Front. Public Health 2020, 8, 603872.
- Lowe, R.; Lee, S.A.; O’Reilly, K.M.; Bastos, L.; Carrasco-Escobar, G.; de Castro Catão, R.; Colón-González, F.J.; Barcellos, C.; Carvalho, M.S.; Blangiardo, M.; et al. Combined effects of hydrometeorological hazards and urbanisation on dengue risk in Brazil: A spatiotemporal modelling study. Lancet Planet. Health 2021, 5, E209–E219.
- Xiang, J.; Hansen, A.; Liu, Q.; Liu, X.; Tong, M.X.; Sun, Y.; Cameron, S.; Hanson-Easey, S.; Williams, C.; Han, G.-S.; et al. Association between dengue fever incidence and meteorological factors in Guangzhou, China, 2005–2014. Environ. Res. 2017, 153, 17–26.
- Li, T.; Yang, Z.; Wang, M. Temperature, relative humidity and sunshine may be the effective predictors for occurrence of malaria in Guangzhou, southern China, 2006–2012. Parasites Vectors 2013, 6, 155.
- Wang, X.; Qi, C.; Zhang, D.D.; Li, C.-Y.; Zheng, Z.-L.; Wang, P.-Z.; Xu, Q.-Q.; Ding, S.-J.; Li, X.-J. Epidemic character and environmental factors in epidemic areas of severe fever with thrombocytopenia syndrome in Shandong Province. Ticks Tick Borne Dis. 2021, 12, 101593.
- Huang, Y.X.; Ren, Z.Y.; Hang, D.R.; Hong, Q.; Gao, Y.; Sun, D.-K.; Zuo, Y.-P. Potential effect of climate changes on schistosomiasis japonica transmission in east route of South-to-North Water Diversion Project. Chin. J. Schistosomiasis Control 2009, 21, 197–204.
- Zhou, S.S.; Huang, F.; Wang, J.J.; Zhang, S.S.; Su, Y.P.; Tang, L.H. Geographical, meteorological and vectorial factors related to malaria re-emergence in Huang-Huai River of central China. Malar. J. 2010, 9, 337.
- Bi, P.; Tong, S.; Donald, K.; Parton, K.A.; Ni, J. Climatic variables and transmission of malaria: A 12-year data analysis in Shuchen County, China. Public Health Rep. 2003, 118, 65–71.
- Liu, Z.; Wang, S.; Zhang, Y.; Xiang, J.; Tong, M.X.; Gao, Q.; Zhang, Y.; Sun, S.; Liu, Q.; Jiang, B.; et al. Effect of temperature and its interactions with relative humidity and rainfall on malaria in a temperate city Suzhou, China. Environ. Sci. Pollut. Res. Int. 2021, 28, 16830–16842.




