
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Nicolò Brandi | -- | 2820 | 2022-04-07 17:50:31 | | | |
| 2 | Amina Yu | -17 word(s) | 2803 | 2022-04-08 04:51:11 | | |
Video Upload Options
A significant proportion of patients with COVID-19 pneumonia could develop acute respiratory distress syndrome (ARDS), thus requiring mechanical ventilation and resulting in a high rate of intensive care unit (ICU) admission. Several complications can arise during ICU stay, from both COVID-19 infection and respiratory supporting system, including barotraumas (pneumothorax and pneumomediastinum), superimposed pneumonia, coagulation disorders (pulmonary embolism, venous thromboembolism, hemorrhages, and acute ischemic stroke), abdominal involvement (acute mesenteric ischemia, pancreatitis, and acute kidney injury) and sarcopenia. Imaging plays a pivotal role in the detection and monitoring of ICU complications and is expanding even to prognosis prediction.
1. Pneumothorax
2. Pneumomediastinum, Pneumopericardium and Subcutaneous Emphysema
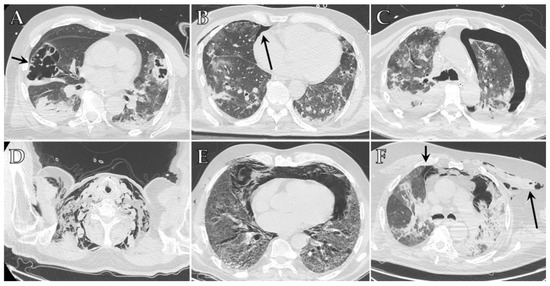
3. Ventilator-Associated Pneumonia (VAP) and Invasive Pulmonary Aspergillosis (IPA)
4. Vascular Complications
5. Gastrointestinal Complications
6. Renal Complications
7. Neurological Complications
8. Sarcopenia
References
- Shrestha, D.B.; Sedhai, Y.R.; Budhathoki, P.; Adhikari, A.; Pokharel, N.; Dhakal, R.; Kafle, S.; Mir, W.A.Y.; Acharya, R.; Kashiouris, M.G.; et al. Pulmonary barotrauma in COVID-19: A systematic review and meta-analysis. Ann. Med. Surg. 2022, 73, 103221.
- Gupta, V.K.; Alkandari, B.M.; Mohammed, W.; Tobar, A.M.; Abdelmohsen, M.A. Ventilator associated lung injury in severe COVID-19 pneumonia patients—Case Reports: Ventilator associated lung injury in COVID-19. Eur. J. Radiol. Open 2020, 8, 100310.
- Udwadia, Z.F.; Toraskar, K.K.; Pinto, L.; Mullerpatan, J.; Wagh, H.D.; Mascarenhas, J.M.; Gandhi, B.M.; Tripathi, A.; Sunavala, A.; Agrawal, U.; et al. Increased frequency of pneumothorax and pneumomediastinum in COVID-19 patients admitted in the ICU: A multicentre study from Mumbai, India. Clin. Med. 2021, 21, e615–e619.
- Chopra, A.; Al-Tarbsheh, A.H.; Shah, N.J.; Yaqoob, H.; Hu, K.; Feustel, P.J.; Ortiz-Pacheco, R.; Patel, K.M.; Oweis, J.; Kozlova, N.; et al. Pneumothorax in critically ill patients with COVID-19 infection: Incidence, clinical characteristics and outcomes in a case control multicenter study. Respir. Med. 2021, 184, 106464.
- Protti, A.; Greco, M.; Filippini, M.; Vilardo, A.M.; Langer, T.; Villa, M.; Frutos-Vivar, F.; Santini, A.; Caruso, P.F.; Spano, S.; et al. Barotrauma in mechanically ventilated patients with Coronavirus disease 2019: A survey of 38 hospitals in Lombardy, Italy. Minerva Anestesiol. 2021, 87, 193–198.
- Wang, X.H.; Duan, J.; Han, X.; Liu, X.; Zhou, J.; Wang, X.; Zhu, L.; Mou, H.; Guo, S. High incidence and mortality of pneumothorax in critically Ill patients with COVID-19. Heart Lung 2021, 50, 37–43.
- Alhumaid, S.; Al Mutair, A.; Alghazal, H.A.; Alhaddad, A.J.; Al-Helal, H.; Al Salman, S.A.; Alali, J.; Almahmoud, S.; Alhejy, Z.M.; Albagshi, A.A.; et al. Extracorporeal membrane oxygenation support for SARS-CoV-2: A multi-centered, prospective, observational study in critically ill 92 patients in Saudi Arabia. Eur. J. Med. Res. 2021, 26, 141.
- Martinelli, A.W.; Ingle, T.; Newman, J.; Nadeem, I.; Jackson, K.; Lane, N.D.; Melhorn, J.; Davies, H.E.; Rostron, A.J.; Adeni, A.; et al. COVID-19 and pneumothorax: A multicentre retrospective case series. Eur. Respir. J. 2020, 56, 2002697.
- McGuinness, G.; Zhan, C.; Rosenberg, N.; Azour, L.; Wickstrom, M.; Mason, D.M.; Thomas, K.M.; Moore, W.H. Increased Incidence of Barotrauma in Patients with COVID-19 on Invasive Mechanical Ventilation. Radiology 2020, 297, E252–E262.
- Zantah, M.; Castillo, E.D.; Townsend, R.; Dikengil, F.; Criner, G.J. Pneumothorax in COVID-19 disease- incidence and clinical characteristics. Respir. Res. 2020, 21, 236.
- Gosangi, B.; Rubinowitz, A.N.; Irugu, D.; Gange, C.; Bader, A.; Cortopassi, I. COVID-19 ARDS: A review of imaging features and overview of mechanical ventilation and its complications. Emerg. Radiol. 2022, 29, 23–34, Erratum in Emerg. Radiol. 2022, 29, 225.
- Kohli, A.; Hande, P.C.; Chugh, S. Role of chest radiography in the management of COVID-19 pneumonia: An overview and correlation with pathophysiologic changes. Indian J. Radiol. Imaging 2021, 31 (Suppl. 1), S70–S79.
- Ziter, F.M., Jr.; Westcott, J.L. Supine subpulmonary pneumothorax. Am. J. Roentgenol. 1981, 137, 699–701.
- Bonato, M.; Fraccaro, A.; Landini, N.; Zanardi, G.; Catino, C.; Savoia, F.; Malacchini, N.; Zeraj, F.; Peditto, P.; Catalanotti, V.; et al. Pneumothorax and/or Pneumomediastinum Worsens the Prognosis of COVID-19 Patients with Severe Acute Respiratory Failure: A Multicenter Retrospective Case-Control Study in the North-East of Italy. J. Clin. Med. 2021, 10, 4835.
- Gahona, C.C.T.; Raj, K.; Bhandari, K.; Nuguru, S.; Bukhari, A. Subcutaneous Emphysema in Patients With COVID-19 Infection: A Report of Three Cases. Cureus 2020, 12, e10559.
- Scacciavillani, R.; Iannaccone, G.; Del Buono, M.G.; Bello, G. Pneumopericardium following mechanical ventilation in COVID-19 pneumonia. Eur. Heart J.-Case Rep. 2020, 4, 1–2.
- Belletti, A.; Palumbo, D.; Zangrillo, A.; Fominskiy, E.V.; Franchini, S.; Dell’Acqua, A.; Marinosci, A.; Monti, G.; Vitali, G.; Colombo, S.; et al. Predictors of Pneumothorax/Pneumomediastinum in Mechanically Ventilated COVID-19 Patients. J. Cardiothorac. Vasc. Anesth. 2021, 35, 3642–3651.
- Lemmers, D.H.; Abu Hilal, M.; Bnà, C.; Prezioso, C.; Cavallo, E.; Nencini, N.; Crisci, S.; Fusina, F.; Natalini, G. Pneumomediastinum and subcutaneous emphysema in COVID-19: Barotrauma or lung frailty? ERJ Open Res. 2020, 6, 00385–02020.
- Bejvan, S.M.; Godwin, J.D. Pneumomediastinum: Old signs and new signs. AJR Am. J. Roentgenol. 1996, 166, 1041–1048.
- Zylak, C.M.; Standen, J.R.; Barnes, G.R.; Zylak, C.J. Pneumomediastinum Revisited. RadioGraphics 2000, 20, 1043–1057, Erratum in Radiographics 2001, 21, 1616.
- Kouritas, V.K.; Papagiannopoulos, K.; Lazaridis, G.; Baka, S.; Mpoukovinas, I.; Karavasilis, V.; Lampaki, S.; Kioumis, I.; Pitsiou, G.; Papaiwannou, A.; et al. Pneumomediastinum. J. Thorac. Dis. 2015, 7 (Suppl. 1), S44–S49.
- Rouyer, M.; Strazzulla, A.; Youbong, T.; Tarteret, P.; Pitsch, A.; de Pontfarcy, A.; Cassard, B.; Vignier, N.; Pourcine, F.; Jochmans, S.; et al. Ventilator-Associated Pneumonia in COVID-19 Patients: A Retrospective Cohort Study. Antibiotics 2021, 10, 988.
- Wicky, P.-H.; Niedermann, M.S.; Timsit, J.-F. Ventilator-associated pneumonia in the era of COVID-19 pandemic: How common and what is the impact? Crit. Care 2021, 25, 153.
- Maes, M.; Higginson, E.; Pereira-Dias, J.; Curran, M.D.; Parmar, S.; Khokhar, F.; Cuchet-Lourenço, D.; Lux, J.; Sharma-Hajela, S.; Ravenhill, B.; et al. Ventilator-associated pneumonia in critically ill patients with COVID-19. Crit. Care 2021, 25, 25, Erratum in Crit. Care 2021, 25, 130.
- Lansbury, L.; Lim, B.; Baskaran, V.; Lim, W.S. Co-infections in people with COVID-19: A systematic review and meta-analysis. J. Infect. 2020, 81, 266–275.
- Razazi, K.; Arrestier, R.; Haudebourg, A.F.; Benelli, B.; Carteaux, G.; Decousser, J.-W.; Fourati, S.; Woerther, P.L.; Schlemmer, F.; Charles-Nelson, A.; et al. Risks of ventilator-associated pneumonia and invasive pulmonary aspergillosis in patients with viral acute respiratory distress syndrome related or not to Coronavirus 19 disease. Crit. Care 2020, 24, 699, Erratum in Crit. Care 2021, 25, 118.
- Blonz, G.; Kouatchet, A.; Chudeau, N.; Pontis, E.; Lorber, J.; Lemeur, A.; Planche, L.; Lascarrou, J.-B.; Colin, G. Epidemiology and microbiology of ventilator-associated pneumonia in COVID-19 patients: A multicenter retrospective study in 188 patients in an un-inundated French region. Crit. Care 2021, 25, 72.
- Moretti, M.; Van Laethem, J.; Minini, A.; Pierard, D.; Malbrain, M.L. Ventilator-associated bacterial pneumonia in coronavirus 2019 disease, a retrospective monocentric cohort study. J. Infect. Chemother. 2021, 27, 826–833.
- Póvoa, H.C.C.; Chianca, G.C.; Iorio, N.L.P.P. COVID-19: An Alert to Ventilator-Associated Bacterial Pneumonia. Infect. Dis. Ther. 2020, 9, 417–420.
- Blot, S.I.; Taccone, F.S.; Van den Abeele, A.-M.; Bulpa, P.; Meersseman, W.; Brusselaers, N.; Dimopoulos, G.; Paiva, J.A.; Misset, B.; Rello, J.; et al. A Clinical Algorithm to Diagnose Invasive Pulmonary Aspergillosis in Critically Ill Patients. Am. J. Respir. Crit. Care Med. 2012, 186, 56–64, Erratum in Am. J. Respir. Crit. Care Med. 2012, 186, 808.
- Jenks, J.D.; Nam, H.H.; Hoenigl, M. Invasive aspergillosis in critically ill patients: Review of definitions and diagnostic approaches. Mycoses 2021, 64, 1002–1014.
- Aggarwal, A.; Tandon, A.; Bhatt, S.; Aggarwal, A.; Dagar, S.; Bansal, H. COVID19 pneumonia with cavitation and cystic lung changes: Multi-detector computed tomography spectrum of a gamut of etiologies. BJR Open 2021, 3, 20210007.
- Zoumot, Z.; Bonilla, M.-F.; Wahla, A.S.; Shafiq, I.; Uzbeck, M.; El-Lababidi, R.M.; Hamed, F.; Abuzakouk, M.; ElKaissi, M. Pulmonary cavitation: An under-recognized late complication of severe COVID-19 lung disease. BMC Pulm. Med. 2021, 21, 24.
- Brandi, N.; Bartalena, L.; Mosconi, C.; Golfieri, R. A unique case of miliary pulmonary tuberculosis induced by bacillus Calmette-Guérin intravesical instillation with COVID-19 superinfection. S. Afr. J. Radiol. 2021, 25, 3.
- Amaral, L.T.W.; Beraldo, G.L.; Brito, V.M.; Rosa, M.E.E.; De Matos, M.J.R.; Fonseca, E.K.U.N.; Yokoo, P.; Silva, M.M.A.; Teles, G.B.D.S.; Shoji, H.; et al. Lung cavitation in COVID-19: Co-infection complication or rare evolution? Einstein 2020, 18, eAI5822.
- Adams, H.J.; Kwee, T.C.; Yakar, D.; Hope, M.D.; Kwee, R.M. Chest CT Imaging Signature of Coronavirus Disease 2019 Infection: In Pursuit of the Scientific Evidence. Chest 2020, 158, 1885–1895.
- Wang, I.E.; Cooper, G.; Mousa, S.A. Diagnostic Approaches for COVID-19 and Its Associated Complications. Diagnostics 2021, 11, 2071.
- Moll, M.; Zon, R.L.; Sylvester, K.W.; Chen, E.C.; Cheng, V.; Connell, N.; Fredenburgh, L.E.; Baron, R.M.; Cho, M.H.; Woolley, A.E.; et al. VTE in ICU Patients With COVID-19. Chest 2020, 158, 2130–2135.
- Zheng, M.-H.; Feng, G.; Liu, W.; Targher, G.; Byrne, C.D.; Zheng, M. Extrapulmonary complications of COVID-19: A multisystem disease? J. Med. Virol. 2021, 93, 323–335.
- Llitjos, J.-F.; Leclerc, M.; Chochois, C.; Monsallier, J.-M.; Ramakers, M.; Auvray, M.; Merouani, K. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J. Thromb. Haemost. 2020, 18, 1743–1746.
- Helms, J.; Tacquard, C.; Severac, F.; Leonard-Lorant, I.; Ohana, M.; Delabranche, X.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Gandet, F.F.; et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensive Care Med. 2020, 46, 1089–1098.
- Poissy, J.; Goutay, J.; Caplan, M.; Parmentier-Decrucq, E.; Duburcq, T.; Lassalle, F.; Jeanpierre, E.; Rauch, A.; Labreuche, J.; Susen, S.; et al. Pulmonary Embolism in Patients With COVID-19: Awareness of an Increased Prevalence. Circulation 2020, 142, 184–186.
- Mirsadraee, S.; Gorog, D.A.; Mahon, C.F.; Rawal, B.; Semple, T.R.; Nicol, E.D.; Arachchillage, D.R.J.; Devaraj, A.; Price, S.; Desai, S.R.; et al. Prevalence of Thrombotic Complications in ICU-Treated Patients with Coronavirus Disease 2019 Detected with Systematic CT Scanning. Crit. Care Med. 2021, 49, 804–815.
- Suh, Y.J.; Hong, H.; Ohana, M.; Bompard, F.; Revel, M.-P.; Valle, C.; Gervaise, A.; Poissy, J.; Susen, S.; Hékimian, G.; et al. Pulmonary Embolism and Deep Vein Thrombosis in COVID-19: A Systematic Review and Meta-Analysis. Radiology 2021, 298, E70–E80.
- Longhitano, Y.; Racca, F.; Zanza, C.; Piccioni, A.; Audo, A.; Muncinelli, M.; Santi, R.; Kozel, D.; Geraci, C.; Taverna, M.; et al. Venous thromboembolism in critically ill patients affected by ARDS related to COVID-19 in Northern-West Italy. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9154–9160.
- Lamarche, Y.; Chow, B.; Bédard, A.; Johal, N.; Kaan, A.; Humphries, K.H.; Cheung, A. Thromboembolic events in patients on extracorporeal membrane oxygenation without anticoagulation. Innovations 2010, 5, 424–429.
- Schmidt, M.; Hajage, D.; Lebreton, G.; Monsel, A.; Voiriot, G.; Levy, D.; Baron, E.; Beurton, A.; Chommeloux, J.; Meng, P.; et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: A retrospective cohort study. Lancet Respir. Med. 2020, 8, 1121–1131.
- Revzin, M.V.; Raza, S.; Srivastava, N.C.; Warshawsky, R.; D’Agostino, C.; Malhotra, A.; Bader, A.S.; Patel, R.D.; Chen, K.; Kyriakakos, C.; et al. Multisystem Imaging Manifestations of COVID-19, Part 2: From Cardiac Complications to Pediatric Manifestations. RadioGraphics 2020, 40, 1866–1892.
- Vaidya, T.; Nanivadekar, A.; Patel, R. Imaging spectrum of abdominal manifestations of COVID-19. World J. Radiol. 2021, 13, 157–171.
- Bhayana, R.; Som, A.; Li, M.D.; Carey, D.E.; Anderson, M.A.; Blake, M.A.; Catalano, O.; Gee, M.S.; Hahn, P.F.; Harisinghani, M.; et al. Abdominal Imaging Findings in COVID-19: Preliminary Observations. Radiology 2020, 297, E207–E215.
- Muñoz, C.A.; Zapata, M.; Gómez, C.I.; Pino, L.F.; Herrera, M.A.; González-Hadad, A. Large intestinal perforation secondary to COVID-19: A case report. Int. J. Surg. Case Rep. 2021, 87, 106362.
- Keshavarz, P.; Rafiee, F.; Kavandi, H.; Goudarzi, S.; Heidari, F.; Gholamrezanezhad, A. Ischemic gastrointestinal complications of COVID-19: A systematic review on imaging presentation. Clin. Imaging 2020, 73, 86–95.
- Kaafarani, H.M.A.; El Moheb, M.; Hwabejire, J.O.; Naar, L.; Christensen, M.A.; Breen, K.; Gaitanidis, A.; Alser, O.; Mashbari, H.; Bankhead-Kendall, B.; et al. Gastrointestinal Complications in Critically Ill Patients with COVID-19. Ann. Surg. 2020, 272, e61–e62.
- El Moheb, M.; Naar, L.; Christensen, M.A.; Kapoen, C.; Maurer, L.R.; Farhat, M.; Kaafarani, H.M.A. Gastrointestinal Complications in Critically Ill Patients with and without COVID-19. JAMA 2020, 324, 1899–1901, Erratum in JAMA 2021, 325, 1113.
- Serban, D.; Tribus, L.C.; Vancea, G.; Stoian, A.P.; Dascalu, A.M.; Suceveanu, A.I.; Tanasescu, C.; Costea, A.C.; Tudosie, M.S.; Tudor, C.; et al. Acute Mesenteric Ischemia in COVID-19 Patients. J. Clin. Med. 2021, 11, 200.
- Caruso, D.; Zerunian, M.; Pucciarelli, F.; Lucertini, E.; Bracci, B.; Polidori, T.; Guido, G.; Polici, M.; Rucci, C.; Iannicelli, E.; et al. Imaging of abdominal complications of COVID-19 infection. BJR Open 2021, 3, 20200052.
- Bozdag, A.; Eroglu, Y.; Tartar, A.S.; Bozdag, P.G.; Aglamis, S. Pancreatic Damage and Radiological Changes in Patients with COVID-19. Cureus 2021, 13, e14992.
- Wang, F.; Wang, H.; Fan, J.; Zhang, Y.; Wang, H.; Zhao, Q. Pancreatic Injury Patterns in Patients With Coronavirus Disease 19 Pneumonia. Gastroenterology 2020, 159, 367–370.
- Kurihara, Y.; Maruhashi, T.; Wada, T.; Osada, M.; Oi, M.; Yamaoka, K.; Asari, Y. Pancreatitis in a Patient with Severe Coronavirus Disease Pneumonia Treated with Veno-venous Extracorporeal Membrane Oxygenation. Intern. Med. 2020, 59, 2903–2906.
- Hadi, A.; Werge, M.; Kristiansen, K.T.; Pedersen, U.G.; Karstensen, J.G.; Novovic, S.; Gluud, L.L. Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members. Pancreatology 2020, 20, 665–667.
- Kumaran, N.K.; Karmakar, B.K.; Taylor, O.M. Coronavirus disease-19 (COVID-19) associated with acute necrotising pancreatitis (ANP). BMJ Case Rep. 2020, 13, e237903.
- Ronco, C.; Reis, T.; Husain-Syed, F. Management of acute kidney injury in patients with COVID-19. Lancet Respir. Med. 2020, 8, 738–742.
- Wang, P.; Tan, X.; Li, Q.; Qian, M.; Cheng, A.; Ma, B.; Zhang, X.; Guo, C.; Sheng, M.; Yi, M.; et al. Extra-pulmonary complications of 45 critically ill patients with COVID-19 in Yichang, Hubei province, China: A single-centered, retrospective, observation study. Medicine 2021, 100, e24604.
- Yuan, H.; Liu, J.; Gao, Z.; Hu, F. Clinical Features and Outcomes of Acute Kidney Injury in Patients Infected with COVID-19 in Xiangyang, China. Blood Purif. 2021, 50, 513–519.
- Batlle, D.; Soler, M.J.; Sparks, M.A.; Hiremath, S.; South, A.M.; Welling, P.A.; Swaminathan, S. COVID-19 and ACE2 in Cardiovascular, Lung, and Kidney Working Group Acute Kidney Injury in COVID-19: Emerging Evidence of a Distinct Pathophysiology. J. Am. Soc. Nephrol. 2020, 31, 1380–1383.
- Liu, Q.; Song, N.C.; Zheng, Z.K.; Li, J.S.; Li, S.K. Laboratory findings and a combined multifactorial approach to predict death in critically ill patients with COVID-19: A retrospective study. Epidemiol. Infect. 2020, 148, e129.
- Ahmad, Z.; Goswami, S.; Paneerselvam, A.; Kabilan, K.; Choudhury, H.; Roy, A.; Guleria, R.; Soni, K.D.; Baruah, U.; Das, C.J. Imaging of Coronavirus Disease 2019 Infection From Head to Toe: A Primer for the Radiologist. Curr. Probl. Diagn. Radiol. 2021, 50, 842–855.
- Akin, I.B.; Altay, C.; Kutsoylu, O.E.; Secil, M. Possible radiologic renal signs of COVID-19. Abdom. Radiol. 2021, 46, 692–695.
- Ronco, C.; Reis, T. Kidney involvement in COVID-19 and rationale for extracorporeal therapies. Nat. Rev. Nephrol. 2020, 16, 308–310.
- Post, A.; den Deurwaarder, E.S.G.; Bakker, S.J.L.; de Haas, R.J.; van Meurs, M.; Gansevoort, R.T.; Berger, S.P. Kidney Infarction in Patients With COVID-19. Am. J. Kidney Dis. 2020, 76, 431–435.
- Su, H.; Yang, M.; Wan, C.; Yi, L.-X.; Tang, F.; Zhu, H.-Y.; Yi, F.; Yang, H.-C.; Fogo, A.B.; Nie, X.; et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020, 98, 219–227.
- Alves, V.D.P.V.; Altoé, A.; Veloso, V.; Ferreira, C.L.S.; Ventura, N.; Corrêa, D.G. Computed tomography features of cerebrovascular complications in intensive care unit patients with severe COVID-19. Radiol. Bras. 2021, 54, 283–288.
- Sklinda, K.; Dorobek, M.; Wasilewski, P.G.; Dreżewski, K.; Dȩbicka, M.; Walecki, J.; Mruk, B. Radiological Manifestation of Neurological Complications in the Course of SARS-CoV-2 Infection. Front. Neurol. 2021, 12, 711026.
- Choi, Y.; Lee, M.K. Neuroimaging findings of brain MRI and CT in patients with COVID-19: A systematic review and meta-analysis. Eur. J. Radiol. 2020, 133, 109393.
- Li, Y.C.; Bai, W.Z.; Hashikawa, T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J. Med. Virol. 2020, 92, 552–555.
- Helms, J.; Kremer, S.; Merdji, H.; Schenck, M.; Severac, F.; Clere-Jehl, R.; Studer, A.; Radosavljevic, M.; Kummerlen, C.; Monnier, A.; et al. Delirium and encephalopathy in severe COVID-19: A cohort analysis of ICU patients. Crit. Care 2020, 24, 491.
- Helms, J.; Kremer, S.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Kummerlen, C.; Collange, O.; Boulay, C.; Fafi-Kremer, S.; Ohana, M.; et al. Neurologic Features in Severe SARS-CoV-2 Infection. N. Engl. J. Med. 2020, 382, 2268–2270.
- Vogrig, A.; Gigli, G.L.; Bnà, C.; Morassi, M. Stroke in patients with COVID-19: Clinical and neuroimaging characteristics. Neurosci. Lett. 2020, 743, 135564.
- Heman-Ackah, S.M.; Su, Y.S.; Spadola, M.; Petrov, D.; Chen, H.I.; Schuster, J.; Lucas, T. Neurologically Devastating Intraparenchymal Hemorrhage in COVID-19 Patients on Extracorporeal Membrane Oxygenation: A Case Series. Neurosurgery 2020, 87, E147–E151.
- Peek, G.J.; Mugford, M.; Tiruvoipati, R.; Wilson, A.; Allen, E.; Thalanany, M.M.; Hibbert, C.L.; Truesdale, A.; Clemens, F.; Cooper, N.; et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): A multicentre randomised controlled trial. Lancet 2009, 374, 1351–1363.
- Masur, J.; Freeman, C.; Mohan, S. A Double-Edged Sword: Neurologic Complications and Mortality in Extracorporeal Membrane Oxygenation Therapy for COVID-19–Related Severe Acute Respiratory Distress Syndrome at a Tertiary Care Center. Am. J. Neuroradiol. 2020, 41, 2009–2011.
- Goldberg, M.F.; Goldberg, M.F. Neuroradiologic manifestations of COVID-19: What the emergency radiologist needs to know. Emerg. Radiol. 2020, 27, 737–745.
- Garg, R.K.; Paliwal, V.K.; Malhotra, H.S.; Sharma, P.K. Neuroimaging Patterns in Patients with COVID-19-Associated Neurological Complications: A Review. Neurol. India 2021, 69, 260–271.
- Rapalino, O.; Pourvaziri, A.; Maher, M.; Jaramillo-Cardoso, A.; Edlow, B.; Conklin, J.; Huang, S.; Westover, B.; Romero, J.; Halpern, E.; et al. Clinical, Imaging, and Lab Correlates of Severe COVID-19 Leukoencephalopathy. Am. J. Neuroradiol. 2021, 42, 632–638.
- Radmanesh, A.; Derman, A.; Lui, Y.W.; Raz, E.; Loh, J.P.; Hagiwara, M.; Borja, M.J.; Zan, E.; Fatterpekar, G.M. COVID-19—Associated Diffuse Leukoencephalopathy and Microhemorrhages. Radiology 2020, 297, E223–E227.
- Soares, M.N.; Eggelbusch, M.; Naddaf, E.; Gerrits, K.H.L.; van der Schaaf, M.; van den Borst, B.; Wiersinga, W.J.; van Vugt, M.; Weijs, P.J.M.; Murray, A.J.; et al. Skeletal muscle alterations in patients with acute Covid-19 and post-acute sequelae of Covid-19. J. Cachex. Sarcopenia Muscle 2022, 13, 11–22.
- Schiaffino, S.; Albano, D.; Cozzi, A.; Messina, C.; Arioli, R.; Bnà, C.; Bruno, A.; Carbonaro, L.A.; Carriero, A.; Carriero, S.; et al. CT-derived Chest Muscle Metrics for Outcome Prediction in Patients with COVID-19. Radiology 2021, 300, E328–E336.
- Levy, D.; Giannini, M.; Oulehri, W.; Riou, M.; Marcot, C.; Pizzimenti, M.; Debrut, L.; Charloux, A.; Geny, B.; Meyer, A. Long Term Follow-Up of Sarcopenia and Malnutrition after Hospitalization for COVID-19 in Conventional or Intensive Care Units. Nutrients 2022, 14, 912.
- Welch, C.; Greig, C.; Masud, T.; Wilson, D.; Jackson, T.A. COVID-19 and Acute Sarcopenia. Aging Dis. 2020, 11, 1345–1351.
- Pironi, L.; Sasdelli, A.S.; Ravaioli, F.; Baracco, B.; Battaiola, C.; Bocedi, G.; Brodosi, L.; Leoni, L.; Mari, G.A.; Musio, A. Malnutrition and nutritional therapy in patients with SARS-CoV-2 disease. Clin. Nutr. 2020, 40, 1330–1337.
- Cruz-Jentoft, A.J.; Sayer, A.A. Sarcopenia. Lancet 2019, 393, 2636–2646, Erratum in Lancet 2019, 393, 2590.
- Lee, K.; Shin, Y.; Huh, J.; Sung, Y.S.; Lee, I.-S.; Yoon, K.-H.; Kim, K.W. Recent Issues on Body Composition Imaging for Sarcopenia Evaluation. Korean J. Radiol. 2019, 20, 205–217.
- Giraudo, C.; Librizzi, G.; Fichera, G.; Motta, R.; Balestro, E.; Calabrese, F.; Carretta, G.; Cattelan, A.M.; Navalesi, P.; Pelloso, M.; et al. Reduced muscle mass as predictor of intensive care unit hospitalization in COVID-19 patients. PLoS ONE 2021, 16, e0253433.
- Damanti, S.; Cristel, G.; Ramirez, G.A.; Bozzolo, E.P.; Da Prat, V.; Gobbi, A.; Centurioni, C.; Di Gaeta, E.; Del Prete, A.; Calabrò, M.G.; et al. Influence of reduced muscle mass and quality on ventilator weaning and complications during intensive care unit stay in COVID-19 patients. Clin. Nutr. 2021, in press.




