
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Yosif Almoshari | + 4995 word(s) | 4995 | 2022-03-14 09:30:29 | | | |
| 2 | Beatrix Zheng | Meta information modification | 4995 | 2022-03-24 03:17:01 | | |
Video Upload Options
Cancer is a group of disorders characterized by aberrant gene function and alterations in gene expression patterns. In 2020, it was anticipated that 19 million new cancer cases would be diagnosed globally, with around 10 million cancer deaths. Late diagnosis and interventions are the leading causes of cancer-related mortality. In addition, the absence of comprehensive cancer therapy adds to the burden. Many lyotropic non-lamellar liquid-crystalline-nanoparticle-mediated formulations have been developed in the last few decades, with promising results in drug delivery, therapeutics, and diagnostics. Cubosomes are nano-structured liquid-crystalline particles made of specific amphiphilic lipids in particular proportions. Their ability to encapsulate lipophilic, hydrophilic, and amphiphilic molecules within their structure makes them one of a kind. They are biocompatible, versatile drug carriers that can deliver medications through various routes of administration. Many preclinical studies on the use of cubosomes in cancer treatment and theranostic applications have been conducted. However, before cubosomes may be employed in clinical practice, significant technical advances must be accomplished.
1. Physiological Properites and Drug Delivery of Cubosome
2. Anticancer Activity of Cubosome
| Sl No. | Cancer/ Cells Type |
Chemicals/Drugs | Polymer Used | Stabilizer | Findings | Ref |
|---|---|---|---|---|---|---|
| 1 | Colorectal/HCT-116 | Cisplatin | GMO | Pluronic F127 | Cisplatin-loaded nano-cubosomes decreased the cell viability of HCT 116 and augmentation of their cytotoxicity in the presence of metformin. | [14] |
| 2 | Colorectal/HCT-116 and Caco-2 | Metformin | GMO | Pluronic F127 | The cubosomes formulation significantly lowered the IC50 concentration at which viable cells were destroyed compared to metformin alone. | [15] |
| 3 | Colorectal/HT-29 | Cornelian cherry | GMO | Poloxamer® 407 | After 24 and 48 hours of incubation, Cornus mas extract cubosome improved IC50 value 1.33 and 1.47 times higher than free Cornus mas extract. The cubosome formulation stopped G1 phase cell growth and produced apoptosis in the cancer cell line HT-29. |
[16] |
| 4 | Colorectal/Caco-2 | 20(S)- protopanaxadiol | GMO | Poloxamer® 407 | The PPD-cubosome showed higher bioavailability, and better release was which is likely owing to greater absorption by the cubic nanoparticles. | [17] |
| 5 | Hepatic/HepG2 | 5-Fluorouracil | GMO | Poloxamer® 407 | 5-FU-loaded cubosomes performed well in vitro cell culture. The cubosomes formulation also boosted bio distribution concentration of 5-FU in the liver compared to the 5-FU solution alone in the rat. | [18] |
| 6 | Hepatic/rat model | Albendazole | GMO | Poloxamer® 407 | The cubosome formulation of the drug resulted in a two-fold increase in bioavailability and greater tumor regression in a rat model of cancer. | [19] |
| 7 | Hepatic/SMMC-7721 | Gambogenic acid | GMO | Poloxamer® 407 | The prepared spherical or ellipsoidal monocellular cubosomes showed remarkable cytotoxicity in the SMMC-7721 cells. | [20] |
| 8 | Hepatic/HepG2 | Resveratrol | GMO | Poloxamer® 407 | The cubosome formulation had higher cytotoxicity against hepatic HepG2 cells in vitro, and superior cell internalization of drugs was observed. | [21] |
| 9 | Breast/MDA-MB-231 | 5- Fluorouracil | Phytantriol | Pluronic F127 | In vitro cytotoxicity testing in the MDA-MB-231 cell line demonstrated that cubosomes containing 5-fluorouracil exhibit more cytotoxicity in the chosen cells than the medication alone. | [22] |
| 10 | Breast/MDA-MB-231/MCF-7 | Thymoquinone | GMO | Poloxamer® 407 | A dose and time-dependent increase in apoptotic cells was observed when treated with Thymoquinone-cubosome formulation against Thymoquinone alone. | [23] |
| 11 | Lung/A549 | Bedaquiline | GMO | Poloxamer 188 | The findings revealed that the cubosome formulation containing the medication exhibited considerable cytotoxicity in A549 cells, in addition to inducing apoptotic cell death, and had anti-invasive properties. | [24] |
| 12 | Lung/A549 | Lumefantrine | GMO | Poloxamer | In A549 cells, the cubosomes formulation demonstrated significantly greater anticancer and anti-angiogenesis action than the medication alone. | [25] |
| 13 | Cervical/Hela | Doxorubicin | GMO | Pluronic F127 | There was somewhat higher IC50 (15 MBq/mL) but statistically significant cytotoxicity at shorter time points, such as 24 h, with the cubosomes formulation. | [26] |
| 14 | Cervical/Hela | Paclitaxel | GMO | PF108-B | The biotinylated cubosome facilitated drug uptake at the cellular level. | [27] |
| 15 | Ovary/SKOV-3 and Caov 3 | Icariin | GMO | Poloxamer® 407 | The findings indicate that Icariin-cubosomes exhibit considerably increased cytotoxicity in both SKOV-3 and Caov 3 cells, but not in normal EA.hy926 endothelial cells. | [28] |
| 16 | Ovary/HEY | Paclitaxel | GMO | Pluronic F127 | The paclitaxel cubosomes demonstrated increased cytotoxicity in ovarian cells (HEY) and a 50% reduction in tumor burden in an animal xenograft model with more safety feature. | [29] |
| 17 | Skin/A431 cells | Paclitaxel | GMO | Pluronic F127 | Loaded paclitaxel accumulated preferentially at the tumor location. Additionally, when paclitaxel was loaded, the average tumor size was decreased to half of its original size when compared to the medication alone. | [30] |
| 18 | Skin/mice | Resveratrol | GMO | Pluronic F127 | The formulation improved skin permeability and deposition at the place of application in the mouse skin layer. | [31] |
2.1. Cubosomes in Colorectal Cancer
2.2. Cubosomes in Liver Cancer
2.3. Cubosomes in Breast Cancer
2.4. Cubosomes in Lung Cancer
2.5. Cubosomes in Cervical Cancer
2.6. Cubosomes in Ovarian Cancer
2.7. Cubosomes in Skin Cancer
References
- Boyd, B.J.; Khoo, S.-M.; Whittaker, D.V.; Davey, G.; Porter, C.J. A lipid-based liquid crystalline matrix that provides sustained release and enhanced oral bioavailability for a model poorly water soluble drug in rats. Int. J. Pharm. 2007, 340, 52–60.
- Lai, J.; Chen, J.; Lu, Y.; Sun, J.; Hu, F.; Yin, Z.; Wu, W. Glyceryl monooleate/Poloxamer 407 cubic nanoparticles as oral drug delivery systems: I. In vitro evaluation and enhanced oral bioavailability of the poorly water-soluble drug simvastatin. AAPS PharmSciTech 2009, 10, 960–966.
- Mohsen, A.M.; Younis, M.M.; Salama, A.; Darwish, A.B. Cubosomes as a potential oral drug delivery system for enhancing the hepatoprotective effect of Coenzyme Q10. J. Pharm. Sci. 2021, 110, 2677–2686.
- Chung, H.; Kim, J.-s.; Um, J.; Kwon, I.C.; Jeong, S. Self-assembled “nanocubicle” as a carrier for peroral insulin delivery. Diabetologia 2002, 45, 448–451.
- Morsi, N.M.; Abdelbary, G.A.; Ahmed, M.A. Silver sulfadiazine based cubosome hydrogels for topical treatment of burns: Development and in vitro/in vivo characterization. Eur. J. Pharm. Biopharm. 2014, 86, 178–189.
- Nasr, M.; Younes, H.; Abdel-Rashid, R.S. Formulation and evaluation of cubosomes containing colchicine for transdermal delivery. Drug Deliv. Transl. Res. 2020, 10, 1302–1313.
- Azhari, H.; Younus, M.; Hook, S.M.; Boyd, B.J.; Rizwan, S.B. Cubosomes enhance drug permeability across the blood–brain barrier in zebrafish. Int. J. Pharm. 2021, 600, 120411.
- Elsenosy, F.M.; Abdelbary, G.A.; Elshafeey, A.H.; Elsayed, I.; Fares, A.R. Brain Targeting of Duloxetine HCL via Intranasal Delivery of Loaded Cubosomal Gel: In vitro Characterization, ex vivo Permeation, and in vivo Biodistribution Studies. Int. J. Nanomed. 2020, 15, 9517.
- Zhai, J.; Hinton, T.M.; Waddington, L.J.; Fong, C.; Tran, N.; Mulet, X.; Drummond, C.J.; Muir, B.W. Lipid–PEG conjugates sterically stabilize and reduce the toxicity of phytantriol-based lyotropic liquid crystalline nanoparticles. Langmuir 2015, 31, 10871–10880.
- Muir, B.W.; Acharya, D.P.; Kennedy, D.F.; Mulet, X.; Evans, R.A.; Pereira, S.M.; Wark, K.L.; Boyd, B.J.; Nguyen, T.-H.; Hinton, T.M. Metal-free and MRI visible theranostic lyotropic liquid crystal nitroxide-based nanoparticles. Biomaterials 2012, 33, 2723–2733.
- Shen, H.-H.; Crowston, J.G.; Huber, F.; Saubern, S.; McLean, K.M.; Hartley, P.G. The influence of dipalmitoyl phosphatidylserine on phase behaviour of and cellular response to lyotropic liquid crystalline dispersions. Biomaterials 2010, 31, 9473–9481.
- Hinton, T.M.; Grusche, F.; Acharya, D.; Shukla, R.; Bansal, V.; Waddington, L.J.; Monaghan, P.; Muir, B.W. Bicontinuous cubic phase nanoparticle lipid chemistry affects toxicity in cultured cells. Toxicol. Res. 2014, 3, 11–22.
- Murgia, S.; Falchi, A.M.; Mano, M.; Lampis, S.; Angius, R.; Carnerup, A.M.; Schmidt, J.; Diaz, G.; Giacca, M.; Talmon, Y. Nanoparticles from lipid-based liquid crystals: Emulsifier influence on morphology and cytotoxicity. J. Phys. Chem. B 2010, 114, 3518–3525.
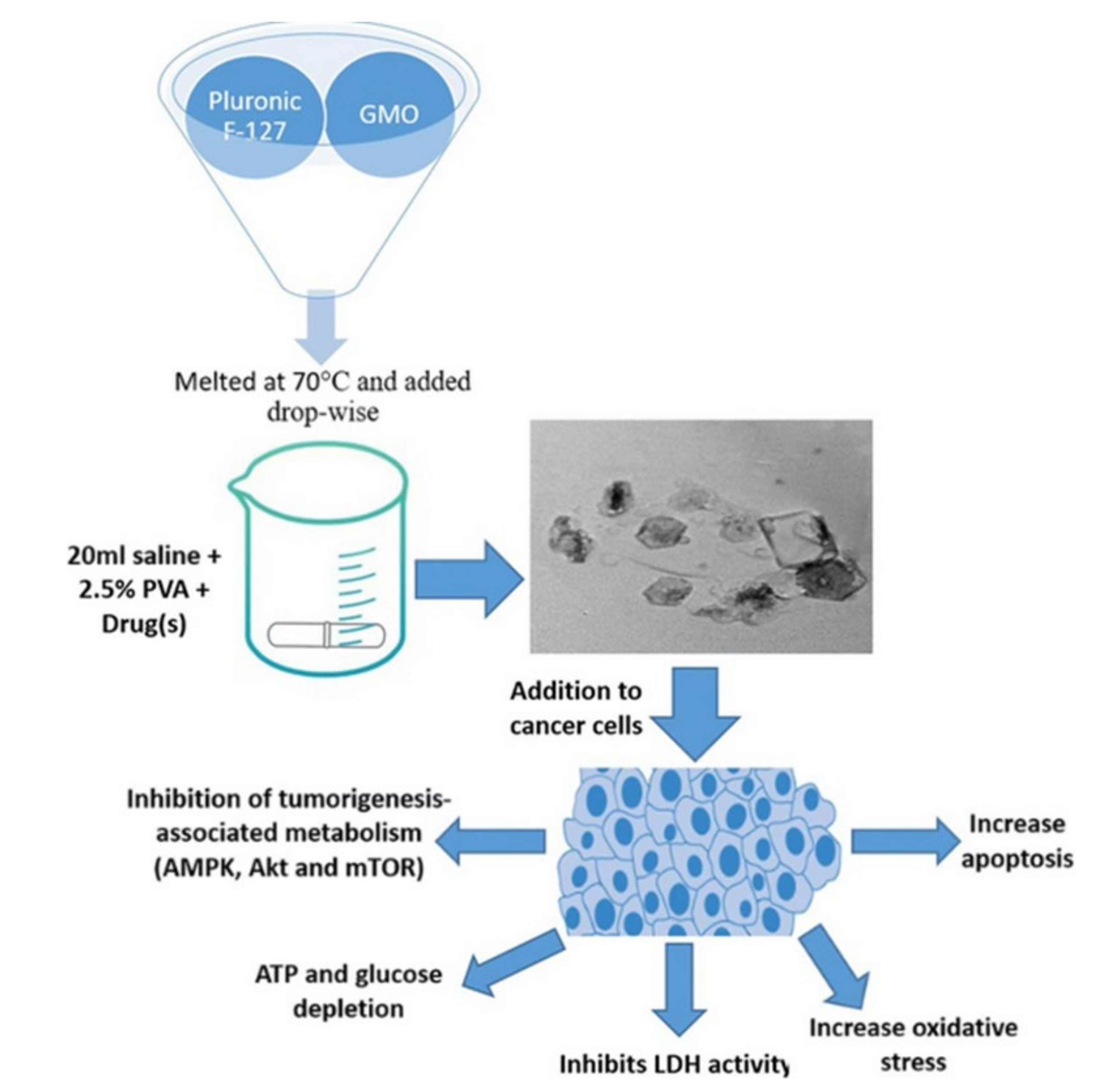
- Saber, M.M.; Al-Mahallawi, A.M.; Nassar, N.N.; Stork, B.; Shouman, S.A.J.B. Targeting colorectal cancer cell metabolism through development of cisplatin and metformin nano-cubosomes. BMC Cancer 2018, 18, 822.
- Magdy, M.; Almahallawi, A.; Nassar, N.; Shouman, S.J.C.T. Pluronic based cubosomes enhance metformin cytotoxicity in colon cancer cell lines. Clin. Ther. 2017, 39, e27.
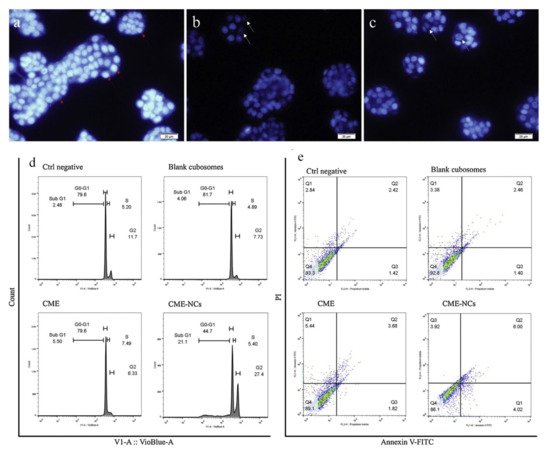
- Radbeh, Z.; Asefi, N.; Hamishehkar, H.; Roufegarinejad, L.; Pezeshki, A. Novel carriers ensuring enhanced anti-cancer activity of Cornus mas (cornelian cherry) bioactive compounds. Biomed. Pharmacother. 2020, 125, 109906.
- Jin, X.; Zhang, Z.-h.; Li, S.-l.; Sun, E.; Tan, X.-b.; Song, J.; Jia, X.-b. A nanostructured liquid crystalline formulation of 20 (S)-protopanaxadiol with improved oral absorption. Fitoterapia 2013, 84, 64–71.
- Li, L.; Han, S.; Yang, C.; Liu, L.; Zhao, S.; Wang, X.; Liu, B.; Pan, H.; Liu, Y. Glycyrrhetinic acid modified MOFs for the treatment of liver cancer. Nanotechnology 2020, 31, 325602.
- Saber, S.; Nasr, M.; Saad, A.S.; Mourad, A.A.; Gobba, N.A.; Shata, A.; Hafez, A.-M.; Elsergany, R.N.; Elagamy, H.I.; El-Ahwany, E. Albendazole-loaded cubosomes interrupt the ERK1/2-HIF-1α-p300/CREB axis in mice intoxicated with diethylnitrosamine: A new paradigm in drug repurposing for the inhibition of hepatocellular carcinoma progression. Biome. Pharmacother. 2021, 142, 112029.
- Luo, Q.; Lin, T.; Zhang, C.Y.; Zhu, T.; Wang, L.; Ji, Z.; Jia, B.; Ge, T.; Peng, D.; Chen, W. A novel glyceryl monoolein-bearing cubosomes for gambogenic acid: Preparation, cytotoxicity and intracellular uptake. Int. J. Pharm. 2015, 493, 30–39.
- Abdel-Bar, H.M.; Abd el Basset Sanad, R. Endocytic pathways of optimized resveratrol cubosomes capturing into human hepatoma cells. Biomed. Pharmacother. 2017, 93, 561–569.
- Astolfi, P.; Giorgini, E.; Gambini, V.; Rossi, B.; Vaccari, L.; Vita, F.; Francescangeli, O.; Marchini, C.; Pisani, M. Lyotropic liquid-crystalline nanosystems as drug delivery agents for 5-fluorouracil: Structure and cytotoxicity. Langmuir 2017, 33, 12369–12378.
- Mehanna, M.M.; Sarieddine, R.; Alwattar, J.K.; Chouaib, R.; Gali-Muhtasib, H. Anticancer activity of thymoquinone cubic phase nanoparticles against human breast cancer: Formulation, cytotoxicity and subcellular localization. Int. J. Nanomed. 2020, 15, 9557.
- Patil, S.M.; Sawant, S.S.; Kunda, N.K. Inhalable bedaquiline-loaded cubosomes for the treatment of non-small cell lung cancer (NSCLC). Int. J. Pharm. 2021, 607, 121046.
- Sethuraman, V.; Janakiraman, K.; Krishnaswami, V.; Natesan, S.; Kandasamy, R. pH responsive delivery of lumefantrine with calcium phosphate nanoparticles loaded lipidic cubosomes for the site specific treatment of lung cancer. Chem. Phys. Lipids 2019, 224, 104763.
- Cytryniak, A.; Nazaruk, E.; Bilewicz, R.; Górzyńska, E.; Żelechowska-Matysiak, K.; Walczak, R.; Mames, A.; Bilewicz, A.; Majkowska-Pilip, A.J.N. lipidic cubic-phase nanoparticles (cubosomes) loaded with doxorubicin and labeled with 177Lu as a potential tool for combined chemo and internal radiotherapy for cancers. Nanomaterials 2020, 10, 2272.
- Aleandri, S.; Bandera, D.; Mezzenga, R.; Landau, E.M. Biotinylated cubosomes: A versatile tool for active targeting and codelivery of paclitaxel and a fluorescein-based lipid dye. Langmuir 2015, 31, 12770–12776.
- Fahmy, U.A.; Fahmy, O.; Alhakamy, N.A. Optimized Icariin Cubosomes Exhibit Augmented Cytotoxicity against SKOV-3 Ovarian Cancer Cells. Pharmaceutics 2021, 13, 20.
- Zhai, J.; Luwor, R.B.; Ahmed, N.; Escalona, R.; Tan, F.H.; Fong, C.; Ratcliffe, J.; Scoble, J.A.; Drummond, C.J.; Tran, N. Paclitaxel-loaded self-assembled lipid nanoparticles as targeted drug delivery systems for the treatment of aggressive ovarian cancer. ACS Appl. Mater. Interfaces 2018, 10, 25174–25185.
- Zhai, J.; Tan, F.H.; Luwor, R.B.; Srinivasa Reddy, T.; Ahmed, N.; Drummond, C.J.; Tran, N. In Vitro and In Vivo Toxicity and Biodistribution of Paclitaxel-Loaded Cubosomes as a Drug Delivery Nanocarrier: A Case Study Using an A431 Skin Cancer Xenograft Model. ACS Appl. Bio Mater. 2020, 3, 4198–4207.
- Kurangi, B.; Jalalpure, S.; Jagwani, S. Formulation and evaluation of resveratrol loaded cubosomal nanoformulation for topical delivery. Curr. Drug Deliv. 2021, 18, 607–619.
- Cisterna, B.A.; Kamaly, N.; Choi, W.I.; Tavakkoli, A.; Farokhzad, O.C.; Vilos, C.J.N. Targeted nanoparticles for colorectal cancer. Nanomedicine 2016, 11, 2443–2456.
- Hu, C.-M.J.; Aryal, S.; Zhang, L. Nanoparticle-assisted combination therapies for effective cancer treatment. Ther. Deliv. 2010, 1, 323–334.
- Barani, M.; Bilal, M.; Rahdar, A.; Arshad, R.; Kumar, A.; Hamishekar, H.; Kyzas, G.Z. Nanodiagnosis and nanotreatment of colorectal cancer: An overview. J. Nanoparticle Res. 2021, 23, 18.
- Moawad, M.M.S. Pharmacological study of the combinatorial cytotoxic effect of certain drugs in human colon cancer cell lines. Ph.D. Theses, Cairo University, Giza, Egypt, 2018.
- Anwanwan, D.; Singh, S.K.; Singh, S.; Saikam, V.; Singh, R. Challenges in liver cancer and possible treatment approaches. Biochim. Biophys. Acta BBA Rev. Cancer 2020, 1873, 188314.
- Nasr, M.; Ghorab, M.K.; Abdelazem, A. In vitro and in vivo evaluation of cubosomes containing 5-fluorouracil for liver targeting. Acta Pharm. Sin. B 2015, 5, 79–88.
- Noorani, L.; Stenzel, M.; Liang, R.; Pourgholami, M.H.; Morris, D.L. Albumin nanoparticles increase the anticancer efficacy of albendazole in ovarian cancer xenograft model. J. Nanobiotechnology 2015, 13, 25.
- Dorling, L.; Carvalho, S.; Allen, J.; González-Neira, A.; Luccarini, C.; Wahlström, C.; Pooley, K.A.; Parsons, M.T.; Fortuno, C.; Wang, Q. Breast Cancer Risk Genes-Association Analysis in More than 113,000 Women. N. Engl. J. Med. 2021, 384, 428–439.
- Hussain, Z.; Khan, J.A.; Murtaza, S. Nanotechnology: An Emerging Therapeutic Option for Breast Cancer. Crit. Rev. Eukaryot. Gene Expr. 2018, 28, 163–175.
- Di Paolo, A.; Danesi, R.; Falcone, A.; Cionini, L.; Vannozzi, F.; Masi, G.; Allegrini, G.; Mini, E.; Bocci, G.; Conte, P. Relationship between 5-fluorouracil disposition, toxicity and dihydropyrimidine dehydrogenase activity in cancer patients. Ann. Oncol. 2001, 12, 1301–1306.
- Bade, B.C.; Cruz, C.S.D. Lung cancer 2020: Epidemiology, etiology, and prevention. Clin. Chest Med. 2020, 41, 1–24.
- Sharma, P.; Mehta, M.; Dhanjal, D.S.; Kaur, S.; Gupta, G.; Singh, H.; Thangavelu, L.; Rajeshkumar, S.; Tambuwala, M.; Bakshi, H.A. Emerging trends in the novel drug delivery approaches for the treatment of lung cancer. Chem. Biol. Interact. 2019, 309, 108720.
- Shafabakhsh, R.; Reiter, R.J.; Mirzaei, H.; Teymoordash, S.N.; Asemi, Z. Melatonin: A new inhibitor agent for cervical cancer treatment. J. Cell. Physiol. 2019, 234, 21670–21682.
- Yuan, Y.-G.; Peng, Q.-L.; Gurunathan, S. Silver nanoparticles enhance the apoptotic potential of gemcitabine in human ovarian cancer cells: Combination therapy for effective cancer treatment. Int. J. Nanomedicine 2017, 12, 6487–6502.
- Li, J.; Jiang, K.; Zhao, F. Icariin regulates the proliferation and apoptosis of human ovarian cancer cells through microRNA-21 by targeting PTEN, RECK and Bcl-2. Oncol. Rep. 2015, 33, 2829–2836.
- Leiter, U.; Keim, U.; Garbe, C. Epidemiology of skin cancer: Update 2019. In Sunlight, Vitamin D and Skin Cancer; Springer: Berlin/Heidelberg, Germany, 2020; pp. 123–139.
- Kalal, B.S.; Upadhya, D.; Pai, V.R. Chemotherapy resistance mechanisms in advanced skin cancer. Oncol. Rev. 2017, 11, 326.




