
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Thomas Wilkinson | + 1521 word(s) | 1521 | 2022-03-09 06:40:11 | | | |
| 2 | Dean Liu | -3 word(s) | 1518 | 2022-03-10 07:29:23 | | |
Video Upload Options
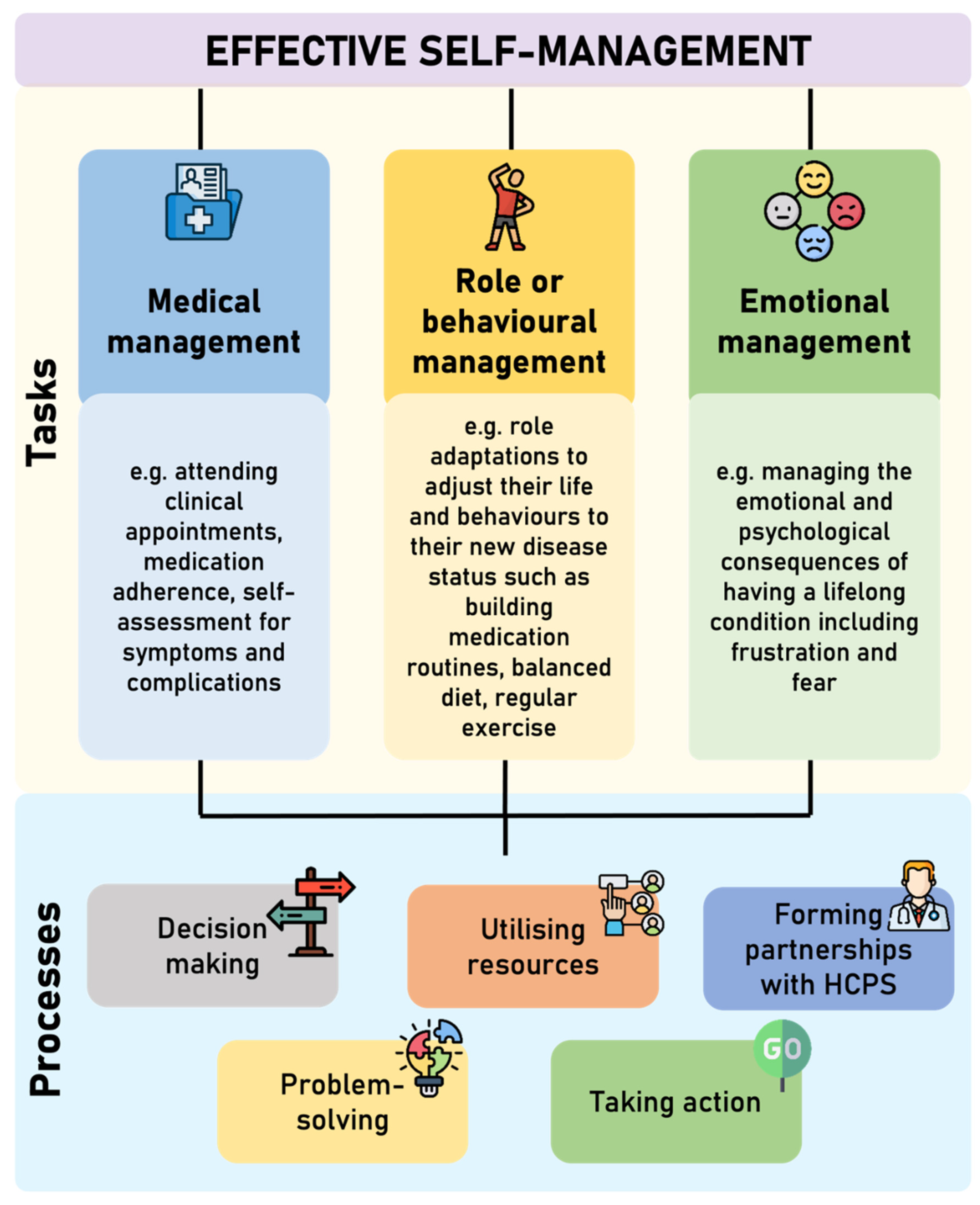
The role of self-management is gaining increasing attention in the management of long-term conditions, including chronic kidney disease (CKD). Self-management refers to the means by which people take an active role in their healthcare. In the UK, supported self-management is part of the National Health Service’s (NHS’s) commitment to make personalised care the norm. This emphasises the need to encourage, support and empower people to manage their ongoing health themselves In order for an individual to be able to look after their health and effectively manage their long-term condition, they need to have the knowledge to understand what to do and why, the skills to be able to perform the required tasks or behaviours, and the confidence that they can do it—this has been termed patient activation.
1. Introduction
Self-Management and CKD
2. Patient Activation and Its Role in Effective Self-Management
3. Measuring Patient Activation and Self-Management
| Measure | Description |
|---|---|
| Chronic Kidney Disease—Self-Management Knowledge Tool (CKD-SMKT) [26] |
The CKD-SMKT is a validated 11-item questionnaire, which comprises of several statements of self-management behaviours to which the respondent must indicate if they believe this is ‘true’, ‘false’ or ‘I do not know’, and if they have done this in the last six months (yes or no). Respondents are asked how much they know about their kidney health and to rate this on a five-point Likert scale from “I know everything I need to know” to “I know nothing”. The CKD-SMKT assess CKD disease-specific knowledge of self-management, which is associated with higher patient activation and improved self-management behaviours. |
| Patient Assessment of Care (PACIC) [27] |
The PACIC is a validated 20-item tool to assess the extent to which patients with a long-term condition receive care that aligns with the Chronic Care Model (CCM). The items are aggregated to form five subscales: (1) patient activation, (2) delivery system design/decision support, (3) goal setting/tailoring, (4) problem solving/contextual, and (5) follow-up/coordination. Whilst these subscales are congruent to the components of CCM, they do not perfectly map onto the CCM components. Respondents rate how often they experienced the content described in each item during the past six months. Each item is scored on a five-point Likert scale from “almost never to “almost always”. Patient activation (i.e., actions that solicit patient input and involvement in decision-making), goal setting (i.e., acquiring information for and setting of specific, collaborative goal), and problem-solving/contextual (i.e., considering potential barriers and the patient’s social and cultural environment in making treatment plans) counselling all map onto self- management support in the CCM. |
| Patient Activation Measure (PAM) [28] |
The PAM-13 is the short form of the 22-item PAM [16] measuring the knowledge, skills, and confidence for self-management. Individuals respond to items such as ‘I know how to prevent further problems with my health condition’ using a 4-point Likert scale ranging from ‘strongly disagree’ (1) to ‘strongly agree’ (4). A ‘not applicable’ (N/A) response is also available. Responses of N/A are scored as 0 and are reported to distinguish those left blank. A continuous activation score is computed from the raw score using an empirically derived calibration table by Insignia Health. The PAM-13 is scored along a Guttman scale (0–100) with higher scores along a unidimensional continuum signifying greater activation. Level 1 (PAM-13 score ≤47; disengagement and disbelief about one’s own role in self-management) encompasses items 1 and 2; Level 2 (47.1–55.1; increasing awareness, confidence, and knowledge in self-management tasks), items 3–8; Level 3 (55.2–67; readiness and taking action), 9–11; and Level 4 (≥67.1; sustainment). |
References
- Wagner, E.H. Chronic disease management: What will it take to improve care for chronic illness? Eff. Clin. Pract. 1998, 1, 2–4.
- Grady, P.A.; Gough, L.L. Self-management: A comprehensive approach to management of chronic conditions. Am. J. Public Health 2014, 104, e25–e31.
- Lorig, K.R.; Holman, H. Self-management education: History, definition, outcomes, and mechanisms. Ann. Behav. Med. 2003, 26, 1–7.
- Corbin, J.M.; Strauss, A. Unending Work and Care: Managing Chronic Illness at Home; Jossey-Bass: San Francisco, CA, USA, 1988.
- NHS England. The NHS Long Term Plan. BMJ 2019, 364, 184.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clincial Practice Guideline for Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2013, 3, 1–150.
- National Institute for Health and Care Excellence (NICE). Chronic Kidney Disease: Assessment and Management; NICE: London, UK, 2021.
- Peng, S.; He, J.; Huang, J.; Lun, L.; Zeng, J.; Zeng, S.; Zhang, L.; Liu, X.; Wu, Y. Self-management interventions for chronic kidney disease: A systematic review and meta-analysis. BMC Nephrol. 2019, 20, 142.
- Novak, M.; Costantini, L.; Schneider, S.; Beanlands, H. Approaches to self-management in chronic illness. Semin. Dial. 2013, 26, 188–194.
- Havas, K.; Bonner, A.; Douglas, C. Self-management support for people with chronic kidney disease: Patient perspectives. J. Ren. Care 2016, 42, 7–14.
- Tuttle, K.R.; Sunwold, D.; Kramer, H. Can comprehensive lifestyle change alter the course of chronic kidney disease? In Seminars in Nephrology; Elsevier: Amsterdam, The Netherlands, 2009; Volume 5, pp. 512–523.
- Teng, H.-L.; Yen, M.; Fetzer, S.; Sung, J.-M.; Hung, S.-Y. Effects of Targeted Interventions on Lifestyle Modifications of Chronic Kidney Disease Patients: Randomized Controlled Trial. West. J. Nurs. Res. 2013, 35, 1107–1127.
- Schulman-Green, D.; Jaser, S.; Martin, F.; Alonzo, A.; Grey, M.; McCorkle, R.; Redeker, N.S.; Reynolds, N.; Whittemore, R. Processes of self-management in chronic illness. J. Nurs. Scholarsh. Off. Publ. Sigma Tau Int. Honor. Soc. Nurs. 2012, 44, 136–144.
- Rodriguez, H.P.; Poon, B.Y.; Wang, E.; Shortell, S.M. Linking Practice Adoption of Patient Engagement Strategies and Relational Coordination to Patient-Reported Outcomes in Accountable Care Organizations. Milbank Q. 2019, 97, 692–735.
- Newland, P.; Lorenz, R.; Oliver, B.J. Patient activation in adults with chronic conditions: A systematic review. J. Health Psychol. 2020, 26, 103–114.
- Hibbard, J.H.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Serv. Res. 2004, 39, 1005–1026.
- Ritter, P.L.; Lorig, K. The English and Spanish Self-Efficacy to Manage Chronic Disease Scale measures were validated using multiple studies. J. Clin. Epidemiol. 2014, 67, 1265–1273.
- Greene, J.; Hibbard, J.H. Why Does Patient Activation Matter? An Examination of the Relationships Between Patient Activation and Health-Related Outcomes. J. Gen. Intern. Med. 2012, 27, 520–526.
- Aung, E.; Donald, M.; Williams, G.M.; Coll, J.R.; Doi, S.A. Influence of patient-assessed quality of chronic illness care and patient activation on health-related quality of life. Int. J. Qual. Health Care 2016, 28, 306–310.
- Chauvet-Gelinier, J.-C.; Bonin, B. Stress, anxiety and depression in heart disease patients: A major challenge for cardiac rehabilitation. Ann. Phys. Rehabil. Med. 2017, 60, 6–12.
- Cukor, D.; Zelnick, L.; Charytan, D.; Shallcross, A.; Mehrotra, R. Patient Activation Measure in Dialysis Dependent Patients in the United States. J. Am. Soc. Nephrol. 2021, 32, 3017–3019.
- Cukor, D.; Coplan, J.; Brown, C.; Friedman, S.; Cromwell-Smith, A.; Peterson, R.A.; Kimmel, P.L. Depression and Anxiety in Urban Hemodialysis Patients. Clin. J. Am. Soc. Nephrol. 2007, 2, 484–490.
- Hibbard, J.H.; Mahoney, E.R.; Stock, R.; Tusler, M. Do increases in patient activation result in improved self-management behaviors? Health Serv. Res. 2007, 42, 1443–1463.
- Hibbard, J.H.; Tusler, M. Assessing activation stage and employing a “next steps” approach to supporting patient self-management. J. Ambul. Care Manag. 2007, 30, 2–8.
- Lightfoot, C.J.; Wilkinson, T.J.; Memory, K.E.; Palmer, J.; Smith, A.C. Reliability and Validity of the Patient Activation Measure in Kidney Disease: Results of Rasch Analysis. Clin. J. Am. Soc. Nephrol. 2021, 16, 880–888.
- Devraj, R.; Wallace, L.S. Application of the content expert process to develop a clinically useful low-literacy Chronic Kidney Disease Self-Management Knowledge Tool (CKD-SMKT). Res. Soc. Adm. Pharm. 2013, 9, 633–639.
- Glasgow, R.E.; Wagner, E.H.; Schaefer, J.; Mahoney, L.D.; Reid, R.J.; Greene, S.M. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Med. Care 2005, 43, 436–444.
- Hibbard, J.H.; Mahoney, E.R.; Stockard, J.; Tusler, M. Development and testing of a short form of the patient activation measure. Health Serv. Res. 2005, 40, 1918–1930.





