The role of self-management is gaining increasing attention in the management of long-term conditions, including chronic kidney disease (CKD). Self-management refers to the means by which people take an active role in their healthcare. In the UK, supported self-management is part of the National Health Service’s (NHS’s) commitment to make personalised care the norm. This emphasises the need to encourage, support and empower people to manage their ongoing health themselves In order for an individual to be able to look after their health and effectively manage their long-term condition, they need to have the knowledge to understand what to do and why, the skills to be able to perform the required tasks or behaviours, and the confidence that they can do it—this has been termed patient activation.
1. Introduction
Self-management is an essential component in chronic disease management to empower patients to take a more active role their health [
4]. There is no universally accepted definition of self-management; however, many definitions include the maintenance of wellness and the management of chronic conditions [
5], whereby an individual takes responsibility for all, or some, aspects of the day-to-day management of their condition [
6]. Originally identified by Corbin and Strauss [
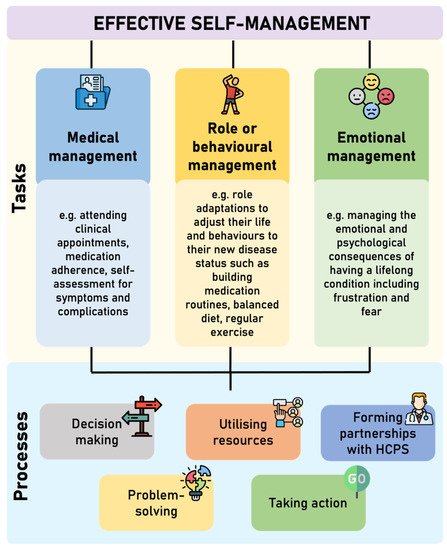
7], effective self-management comprises of three core tasks (medical management, role or behavioural management, and emotional management), which are underpinned by five key processes (decision making, utilising resources, forming partnerships with healthcare professionals, problem solving, and taking action) [
6]; this is displayed in
Figure 1. Self-efficacy is required to execute and engage with this complex set of tasks and processes.
The prioritisation of self-management is becoming increasingly prevalent in clinical guidelines for long-term conditions. The NHS Long Term Plan incorporates supported self-management within personalised care to encourage, support, and empower people to manage their ongoing physical and mental health conditions themselves to live well with their condition [
2]. This includes the provision of self-management education to help people with long-term conditions to develop the knowledge, skills, and confidence they need to manage their own health care effectively [
2].
Self-Management and CKD
The promotion of self-management behaviours is increasingly being considered as a standard of care in the effort to decelerate CKD progression and prevent complications in CKD management guidelines. Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines include self-management as a component of CKD models of care, and recommend information, advice, and education to support self-management behaviours should be incorporated into the treatment plan at all stages of CKD [
8]. The UK National Institute of Care and Excellence (NICE) guidelines for CKD assessment and management recommend that systems are in place to support self-management and enable people with CKD to make informed choices [
9]; one method is to provide people access to their medical data through information systems, such as Renal Patient View/Patient Knows Best (secure online record of own health and care information, linked to medical records), to encourage and help them self-manage their CKD [
9].
The goal of self-management education is to identify strategies that can be used to help patients manage their condition(s) whilst leading full, active, and productive lives. For those living with CKD, self-management behaviours range from medication adherence, health monitoring, and symptom monitoring to lifestyle modifications (e.g., increasing physical activity and eating an appropriate diet), which reduce cardiovascular, CKD progression and general health risk factors [
10]. Learning to live with and coping with the emotional consequences associated with CKD are important in looking after one’s mental health [
11] and can facilitate an optimistic view and positive attitude towards their condition, health, and life [
12]. Engaging in self-management behaviours can reduce symptom burden, improve quality of life, and potentially slow the progression of CKD [
13,
14]. To help people with CKD self-manage, it is widely recommended that individuals are aware of their diagnosis, involved in shared treatment decisions, provided access to their medical data, and given information on blood pressure control, exercise, diet, medication management and smoking cessation [
9].
Figure 1. Core tasks and processes involved in effective self-management (adapted from Corbin and Strauss [
7] and Lorig and Hoffman [
6]. HCPs = Healthcare professionals.
2. Patient Activation and Its Role in Effective Self-Management
As discussed previously, effective self-management involves a multifaceted set of tasks and processes. It is now becoming evident that having the appropriate knowledge, skills, and confidence (i.e., patient activation) and the ability to utilise these to manage their disease, identify and access resources and support may be a fundamental component of effective self-management behaviour [
11,
41]. Patient activation for self-management is only the first step in the process about how best to meet the needs of self-management [
42]. Activating individuals to be a participant in their own health and engage in self-management activities is of critical importance in improving overall health and health-related quality of life [
43].
Knowledge about a long-term condition and its treatment is an important component of self-management and patient activation [
17]. Having the necessary skills and knowledge of one’s own condition will result in better levels of activation [
44], and increased activation is followed by improvements in self-management behaviours [
18,
45]. However, differing levels of self-management can be influenced by levels of activation. Accompanying symptoms can adversely influence patient activation impacting on daily living and self-management activities [
46]. In addition, a high burden from disease and treatments may challenge patient activation and a patient’s ability to self-manage [
39], which can be further complicated by a high prevalence of depression and anxiety [
47]. Given the individual symptoms and outcomes in each condition, the use of patient activation to promote successful movement across levels of activation is key [
43].
Increasing patient activation aims to facilitate behaviour change and improve health outcomes. Positive changes in activation are related to positive changes in a variety of self-management skills in individuals with long-term conditions, such as engaging in regular exercise, managing stress, paying attention to diet, and taking medications [
48]. In addition, activation levels have been shown to be correlated with disease specific behaviours; highly activated individuals with diabetes are more likely to take medication as directed, read food labels, and read potential side effects when prescribed a new medication [
48]. Similar findings have also been reported in other conditions such as cardiovascular disease [
49]. To our knowledge, the relationship between patient activation and CKD-specific behaviours has not yet been explored; however, this has previously been identified as an area for future research [
50].
3. Measuring Patient Activation and Self-Management
There are a number of measures that assess self-management and patient activation (summarised in Table 2), these include the Chronic Kidney Disease—Self-Management Knowledge Tool (CKD-SMKT) and Patient Assessment of Care (PACIC). However, it is the Patient Activation Measure (PAM) that has become the most used instrument to assess patient activation.
Table 2. Commonly used tools or measures that assess self-management and patient activation.
| Measure |
Description |
Chronic Kidney Disease—Self-Management Knowledge Tool (CKD-SMKT)
[51] |
The CKD-SMKT is a validated 11-item questionnaire, which comprises of several statements of self-management behaviours to which the respondent must indicate if they believe this is ‘true’, ‘false’ or ‘I do not know’, and if they have done this in the last six months (yes or no). Respondents are asked how much they know about their kidney health and to rate this on a five-point Likert scale from “I know everything I need to know” to “I know nothing”. The CKD-SMKT assess CKD disease-specific knowledge of self-management, which is associated with higher patient activation and improved self-management behaviours. |
Patient Assessment of Care (PACIC)
[52] |
The PACIC is a validated 20-item tool to assess the extent to which patients with a long-term condition receive care that aligns with the Chronic Care Model (CCM). The items are aggregated to form five subscales: (1) patient activation, (2) delivery system design/decision support, (3) goal setting/tailoring, (4) problem solving/contextual, and (5) follow-up/coordination. Whilst these subscales are congruent to the components of CCM, they do not perfectly map onto the CCM components. Respondents rate how often they experienced the content described in each item during the past six months. Each item is scored on a five-point Likert scale from “almost never to “almost always”. Patient activation (i.e., actions that solicit patient input and involvement in decision-making), goal setting (i.e., acquiring information for and setting of specific, collaborative goal), and problem-solving/contextual (i.e., considering potential barriers and the patient’s social and cultural environment in making treatment plans) counselling all map onto self- management support in the CCM. |
Patient Activation Measure (PAM)
[16] |
The PAM-13 is the short form of the 22-item PAM [17] measuring the knowledge, skills, and confidence for self-management. Individuals respond to items such as ‘I know how to prevent further problems with my health condition’ using a 4-point Likert scale ranging from ‘strongly disagree’ (1) to ‘strongly agree’ (4). A ‘not applicable’ (N/A) response is also available. Responses of N/A are scored as 0 and are reported to distinguish those left blank. A continuous activation score is computed from the raw score using an empirically derived calibration table by Insignia Health. The PAM-13 is scored along a Guttman scale (0–100) with higher scores along a unidimensional continuum signifying greater activation. Level 1 (PAM-13 score ≤47; disengagement and disbelief about one’s own role in self-management) encompasses items 1 and 2; Level 2 (47.1–55.1; increasing awareness, confidence, and knowledge in self-management tasks), items 3–8; Level 3 (55.2–67; readiness and taking action), 9–11; and Level 4 (≥67.1; sustainment). |
This entry is adapted from the peer-reviewed paper 10.3390/kidneydial2010012