Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | David Aebisher | + 5205 word(s) | 5205 | 2022-02-15 10:10:46 | | | |
| 2 | Conner Chen | -158 word(s) | 5047 | 2022-03-01 07:08:19 | | | | |
| 3 | Conner Chen | -158 word(s) | 5047 | 2022-03-01 07:09:15 | | | | |
| 4 | Conner Chen | + 2 word(s) | 5049 | 2022-03-04 01:28:56 | | | | |
| 5 | Conner Chen | Meta information modification | 5049 | 2022-03-07 02:11:02 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Aebisher, D. Natural Photosensitizers in Photodynamic Therapy. Encyclopedia. Available online: https://encyclopedia.pub/entry/20027 (accessed on 07 February 2026).
Aebisher D. Natural Photosensitizers in Photodynamic Therapy. Encyclopedia. Available at: https://encyclopedia.pub/entry/20027. Accessed February 07, 2026.
Aebisher, David. "Natural Photosensitizers in Photodynamic Therapy" Encyclopedia, https://encyclopedia.pub/entry/20027 (accessed February 07, 2026).
Aebisher, D. (2022, March 01). Natural Photosensitizers in Photodynamic Therapy. In Encyclopedia. https://encyclopedia.pub/entry/20027
Aebisher, David. "Natural Photosensitizers in Photodynamic Therapy." Encyclopedia. Web. 01 March, 2022.
Copy Citation
Photodynamic therapy (PDT) is a therapy for the treatment of many diseases, including cancer. This therapy uses a combination of a photosensitizer (PS), light irradiation of appropriate length and molecular oxygen. The photodynamic effect kills cancer cells through apoptosis, necrosis, or autophagy of tumor cells.
photodynamic therapy (PDT)
1. Introduction
Cancer is one of the most frequently occurring diseases and, apart from heart and circulatory system disease, is the greatest threat to health worldwide. It is estimated that, in 2020, almost 20 million cancer cases were reported. Statistically, mortality from malignant neoplasms is about 50%. Today, 30–50% of cancer cases are preventable by reducing risk factors and implementing preventive strategies. The cancer burden can also be reduced through early detection and the appropriate treatment and care of patients who develop cancer. Many cancers have a good chance of being cured if they are diagnosed early and properly treated [1].
The methods of cancer treatment used currently in oncology, such as chemotherapy and radiotherapy, lead to numerous complications related to damage of healthy tissues. Patients often experience local recurrence of the disease or develop secondary tumors via metastases. An inability to selectively act on neoplastic tissue motivates the search for new, more effective methods of treatment of this dangerous disease.
More than 100 years have passed since the discovery and description of photodynamic therapy (PDT). PDT has received widespread interest in recent years as a non-invasive and highly selective approach to cancer treatment.
The basis of PDT is to introduce an appropriate photosensitizer (PS) that accumulates in the tumor tissue or local vasculature and then illuminate it with light. The essence of PDT is the destruction of neoplastic cells by reaction with reactive oxygen species such as singlet oxygen or hydroxyl radicals that are generated by photodynamic action. PDT for the treatment of cancer and precancerous conditions it is an alternative treatment but may be used, and usually is, in combination with the other treatment options to traditional methods of treatment (Figure 1).
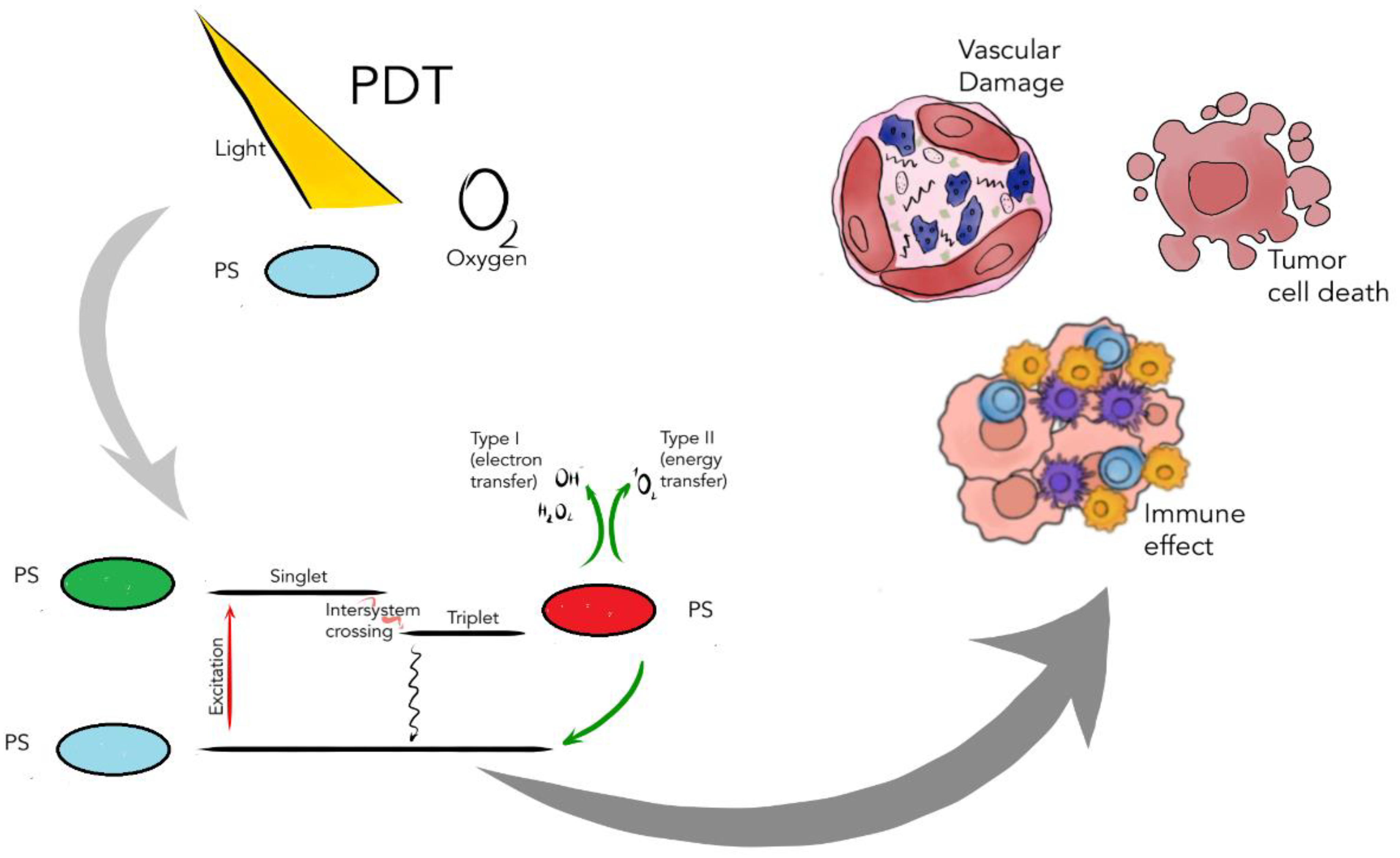
Figure 1. Mechanisms of action of PDT such as inducing immune responses, damaging vascular structures and direct killing of tumor cells. PS’s generate ROS only after exposure to specific light and light activation in the presence of oxygen. Generated ROS mainly cause effector functions (e.g., killing cancer cells, inducing immune responses, damaging vascular structures and direct killing of tumor cells). Following light absorption, the PS reaches an excited singlet state. After an intersystem crossing, the PS, now in a triplet excited state, can react in two ways: react with biomolecules through a hydrogen atom (electron) transfer to form radicals, which react with molecular oxygen to generate ROS (Type I reaction), or the PS in its triplet state can react directly with oxygen through energy transfer, generating singlet oxygen (Type II reaction).
PDT requires the presence of three basic ingredients. The first component is the presence of PS, i.e., a light-sensitive compound that is delivered to neoplastic tissue. The second is the presence of oxygen (O2) dissolved in the tissues, and the third necessary component is the selection of a light source with an appropriate wavelength adapted to the absorption spectrum of a given photosensitizer [2].
The presence of three basic ingredients (PS, O2 and light) leads to tumor necrosis [3]. PDT is approved for treatment of neoplastic diseases such as bladder cancer [4][5], skin cancer [6][7], lung cancer [8][9], gastrointestinal tract cancers [10][11][12][13], and cancers of the oral cavity [14][15]. There are also studies on the use of PDT for breast cancer treatment [16][17][18]. To date, PDT has been used successfully in dermatology, gynecology and urology [19].
Historically, Tappeiner and Jesionek were the first to successfully treat skin cancer with eosin in combination with white light. Soon after, Figge demonstrated that hemoporphyrin (HP) has tumor localization properties; Lipson and colleagues initiated PDT in clinical use in the 1960s in the USA [20].
Hematoporphyrin gave rise to the first generation of compounds used as PS in PDT. Currently, second-generation compounds are also used, including synthetic photosensitizers (porphyrin and porphyrin-like compounds). Third-generation drugs combine the high efficiency of the second-generation compounds with greater affinity for tumors, which results in reduced damage to surrounding tissues.
Over the years, many compounds that possess photosensitizing properties have been discovered or synthesized. The search is still ongoing on for photosensitizers that selectively accumulate in neoplastic tissues and do not cause side effects after therapy, e.g., cytotoxicity or mutagenicity. Scientists synthesize new photosensitizers with better biological properties and with absorption in the near infrared (the optimal spectral range for light penetration into tissue) that accumulate in neoplastic tissue and have high quantum yields of reactive oxygen species (ROS). The redox balance is maintained in cancer cells due to their marked antioxidant capacity.
2. Photochemical Reactions in Photodynamic Therapy
A PS is introduced into the patient’s body (intravenously or locally, e.g., on the skin) which accumulates in cancer cells. After a certain period of time, the photosensitizer reaches its maximum concentration in the tumor in relation to the surrounding healthy tissue. After this time, the area is exposed to radiation of wavelength corresponding to the absorption of the PS. The light source must be chosen so that the emission bandwidth of the light source coincides with the PS band absorption necessary for photochemical reaction [21].
As a result of photon absorption, the photosensitizer molecule is excited from the singlet ground state to the excited singlet state. From the point of view of PDT or photodynamic diagnosis (PDD), there are two deactivation pathways that are of importance. The first is transferring excess energy to the environment through the fluorescence process. In PDD, fluorescence detection of a cumulative drug in neoplastic tissue allows for a precise diagnosis with the determination of the shape, size and location of the neoplastic lesion.
The second pathway is intersystem crossing from the exited singlet state to the triplet state. The lifetime of a photosensitizer molecule in the triplet state is sufficiently long to interact with oxygen. Molecular oxygen in the ground state is a triplet and in the process of energy capture it effectively deactivates the triplet state of the PS, in turn generating a strong oxidant known as singlet oxygen [22][23].
The literature describes in detail two mechanisms (Type I and Type II) of the photodynamic effect (Figure 2).
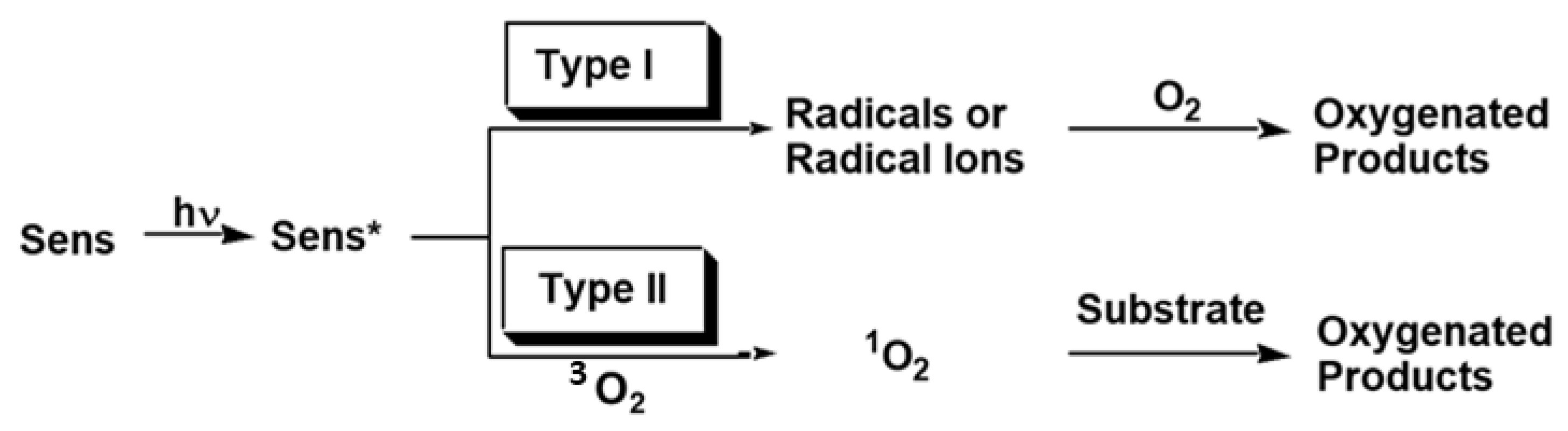
Figure 2. Type I and Type II photosensitized reactions. * Excited state of sens.
Type I photosensitized reactions involve electron transfer and lead to the initial formation of radicals and the participation of O2 in subsequent steps involved in the oxidation process. Additionally, the Type I mechanism can occur when the environment is hypoxic. The photooxidation reaction leads to the formation of free radicals in tumor tissue. In the type I mechanism, an electron or a hydrogen atom is transferred between the molecule of the excited dye and the neoplastic tissue in which the photochemical reaction takes place. As a result of these reactions, a radical anion or substrate radical is formed.
On the other hand, the type II mechanism involves an initial energy transfer from the triplet excited state of the sensitizer to dissolved O2, which is in its ground triplet state.
The Type II mechanism is the dominant mechanism for the destruction of neoplastic tissue. Singlet oxygen (1O2, refers to the 1Δ state) is the predominant type II reactive oxygen species that is able to react with nucleic acids (exclusively guanine), unsaturated lipids and amino acids such as Trp, His and Met. Biological 1O2 reactions often lead to endoperoxides from [2 + 4] cycloadditions, dioxetanes from [2 + 2] cycloadditions, hydroperoxides from “ene” reactions or phenol oxidations, and sulfoxides from sulfides [24].
Excited singlet oxygen is the result of energy transfer from the triplet form of the photosensitizer molecule to the oxygen molecule. Energy transfer is allowed, and the dye molecule returns to its ground state [25][26][27]. Ideal sensitizer properties and conditions for PDT can lead to cell death in three ways, i.e., apoptosis, necrosis, and autophagy. The response to PDT may differ according to the cell type, its genetic or metabolic potential, and PS intracellular location. The tumor site treated with PDT may initially determine which cell death pathway will be activated. In the beginning, a rescue mechanism is triggered, possibly the process of autophagy. On the other hand, when the PDT damage is sufficiently strong (the concentration of the PS is lower and the incubation time is longer), the cells cannot be repaired and the apoptosis mechanism is activated. If cell damage by PDT is too high (high concentration of photosensitizer and a short incubation time), then it may also lead to necrosis. In this process, proteins involved in both autophagy and apoptosis can be destroyed immediately, and cellular integrity can be broken [28][29].
The EPR (electron paramagnetic resonance) also known as electron magnetic resonance (EMR) or electron spin resonance (ESR), is often used as the “gold standard” in the biological, chemical, and medical systems to detect and characterize radicals. EPR is based on the principle of the absorption of electromagnetic radiation by using electrons with unpaired spins falling under a magnetic field to transition from low to high energy levels, which can be designated as a −1/2 and +1/2, respectively [30].
3. The Role of Photosensitizers in PDT
Plant species that are considered toxic are often a source of pharmaceutically active compounds that are some of our drugs and are isolated from plants. Due to the presence of chromophores, they easily absorb light and fluoresce in blue–yellow under long-wave ultraviolet light. These compounds can be produced by the plant as a protective mechanism against a large dose of sunlight, which is why they are often placed in sunscreen and cosmetics for this purpose. Psoralens are typical of the citrus and celery families. Some plants belonging to these groups are known as bladder bushes because the psoralens they contain are known to be phototoxic. This can prove difficult for farmers who remove large amounts of giant hogweed and come into contact with the sap of a psoralen-rich plant, and in the presence of sunlight can cause inflammation and, in severe cases, blistering of the skin. Other species known to be phototoxic are borscht, rue and some Citruss spp. A number of culinary-relevant apiaceus herbs, such as celery, parsley, parsnips and angelica, may even be phototoxic due to the presence of furanocoumarins. Psoralens, e.g., form adducts with DNA pyrimidine bases such as thymine via cycloaddition.
Many plants contain photoactive chemicals and have been identified as phototoxic plants that have the ability to cause skin reactions in humans or animals when they come into contact with the skin followed by exposure to the sun.
As early as 1942, Klaber [31] observed sunburn in people exposed to sunlight. They then studied many phototoxic plants or phototoxic phytochemicals that, when exposed to sunlight, were susceptible to phototoxic and photogenotoxic skin effects, such as skin irritation, sensitization, allergy, mutations and skin cancers. Photoxins can be found in many different plant families (Table 1), and it follows that the vast majority of phototoxins in the plant kingdom are not related.
Table 1. Examples of photototoxic plant species and their reported some phototoxins.
| Common Name | Plant Species | Phototoxin(s) | References |
|---|---|---|---|
| Ammi majus L. | Bishop’s weed | e.g., Xanthotoxin, bergapten, oxypeucedanin |
[32] |
| Ammi visnaga (L.) | Apiaceae | e.g., Xanthotoxin; 8-hydroxybergapten; imperatorin |
[33] |
| Pastinaca sativa | Wild parsnip | e.g., Xanthotoxin; bergapten; imperatorin | [34] |
| Cymopterus watsonii | Apiaceae | e.g., Xanthotoxin; bergapten | [35] |
| Cullen cinereum | Hoary Scurf-pea | e.g., Psoralen | [36] |
| Ruta graveolens L. | Rua | e.g., Psoralen; bergapten; isorutarin | [37] |
Photosensitizers accumulate in cancer cells and, to a lesser extent, in healthy tissues. The effectiveness of PDT largely depends on the properties of the photosensitizer used. A lot of research is carried out to synthesize and optimize the physicochemical properties of photoactive compounds. Often, new photosensitizers of natural origin, e.g., from plants, are obtained. In order for a PS to be used in the diagnosis or treatment of neoplastic diseases, it must meet several conditions [38][39][40][41][42].
- The PS should selectively accumulate in neoplastic tissue;
- The PS should preferably be readily available, in the form of a pure compound, and its chemical properties must be carefully established beforehand;
- The PS should not have phototoxic effects in healthy tissue;
- The PS should be characterized by a high coefficient of absorption in the spectral range of 600–800 nm, with maximum light penetration through the tissue;
- The absorption bands of the photosensitizer must not overlap the absorption bands of endogenous dyes such as melanin or hemoglobin and the water absorption bands in the near infrared region;
- The PS should react efficiently with light to generate singlet oxygen or radicals;
- The PS and these photoproducts should be characterized by optimal pharmacokinetic properties;
- The PS should have few side effects;
- The PS should be of low toxicity and easily excreted from the body to avoid phototoxicity after treatment.
Many dyes, both known and newly synthesized, have been tested for utility in PDT. The requirements that must be met by PS are high and therefore no dye has been discovered that satisfies all of the above criteria [43]. Most PS’s and PS’s photoproducts used in PDT anti-cancer therapy are porphyrin compounds or their derivatives.
3.1. Naturally Occurring Photosensitizers in PDT
Since ancient times, herbal medicine from natural products has been utilized for treating various human ailments. Most current medicines are derived from various medicinal plants, and it is evident that herbal extracts and their compounds should be examined as possible active lead components in cancer drug discoveries. Nature is a valuable reserve for medicinal plants, and many of the pharmaceutically active compounds isolated from medicinal plants have not been tested for photoactive properties. There have been few studies attempting to identify new chemical compounds with photoactivity from plant extracts that can be used as potent natural PSs and in order to achieve the bioavailability and cytotoxicity induction, the drugs are administrated in high concentrations.
Current analytical methods allow for the extraction, purification, determination of the chemical structure, as well as the determination of the pharmacology of active ingredients obtained from natural materials. The natural products are a very useful source for the development of drugs and discovery of new photosensitizers [44][45]. Nature hides a huge amount of pharmaceutically active compounds, some of which are described in the scientific literature.
In recent decades, numerous efforts have been made to isolate new products of natural origin from microbes, plants and other living organisms. Their pharmacological properties are studied, and their anti-cancer properties are assessed. The efforts made have led to the discovery of a number of anti-cancer drugs. It is estimated that in the years 1981–2019, approximately 25% of all newly registered anticancer drugs were derived from natural products [46][47].
In a 2019 review published by Hamblin et al., it is presented that about 400 individual compounds have been recognized as possible candidates for use as PSs [27].
In a 2020 review published by Muniyandi et al., more than 300 chemical compounds have already been identified as potential candidates to be used as PSs and the largest group about 700 of anthraquinones possess photoactive properties [45].
In natural extracts, researchers have found new active chemical compounds that display efficient PS properties [48][49][50]. Jong et al. presented the results of screening 2400 extracts from 888 plants for their photosensitizing activity. The study looked at terrestrial plants in the Sarawak forests of Borneo with the goal of finding new photosensitizers for PDT [51]. In 2014, a group of researchers examined the phototoxic properties of 278 extracts. Finally, they described two new PS that showed activity in PDT. Finally, they identified two new photosensitizers with cyclic tetrapyrrole structures [52]. In other studies, the hydrophobic extract of the Arrabidaea chica (Crajiru) plant was presented as a rich collection of PS that could be used in PDT [44]. In 2017, three extracts were tested with the use of MCF-7 breast adenocarcinoma cells for their potential as a source of PS’s in PDT. Photoactivated L. racemosa and A. procera extracts were found to be more cytotoxic to MCF-7 than the non-tumor human neonatal skin fibroblast lineage [53].
The above examples and Figure 3 show how important it is to study extracts from various plants for the detection of new PS’s that can be used in PDT.
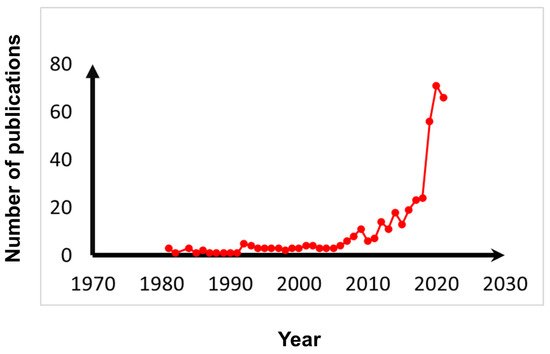
Figure 3. The numbers of publications regarding natural compounds used in PDT.
Several PSs were approved for clinical applications or under clinical trials, e.g., Photogem [54], Photodithazine [55], and Photosan [56]. PDT, through the use of PS’s that allow them to interact with many cell receptors and induce cell death, can be used in the treatment of bacterial and viral diseases, autoimmune diseases, and cancer. The antimicrobial PDT has been known for over 30 years and has proven effective against a wide variety of bacteria. Advances in PDT development confirm that it has the ability to kill bacteria, fungi and viruses. ROS generated by the PDT process can deactivate several classes of microbial cells, including Gram-negative bacteria such as Pseudomonas aeruginosa, which are typically characterized by an impermeable outer cell membrane that contains endotoxins and blocks antibiotics, dyes and detergents, protecting the sensitive inner membrane and wall cellular [57]. PDT can be used in infections that do not respond well to antibiotic therapy. There are several features of PDT that make it potentially ideal for treating diabetic feet. The photosensitizer is non-toxic in the dark, but becomes a very effective topical antimicrobial agent when irradiated [58]. PDT was also effective in seventy-seven non-smoking periodontitis patients for acting PDT as an adjuvant treatment. PDT has a positive effect in significantly reducing the periodontal microbial load [59]. The anti-inflammatory and antibacterial action were possible due to the effect of toothpaste containing Polish propolis and plant oils on oral cavity health in patients with oral cleft treated orthodontically [60].
The chemical formulas of natural photoactive compounds described in the work are presented in Figure 4 and in Figure 5.
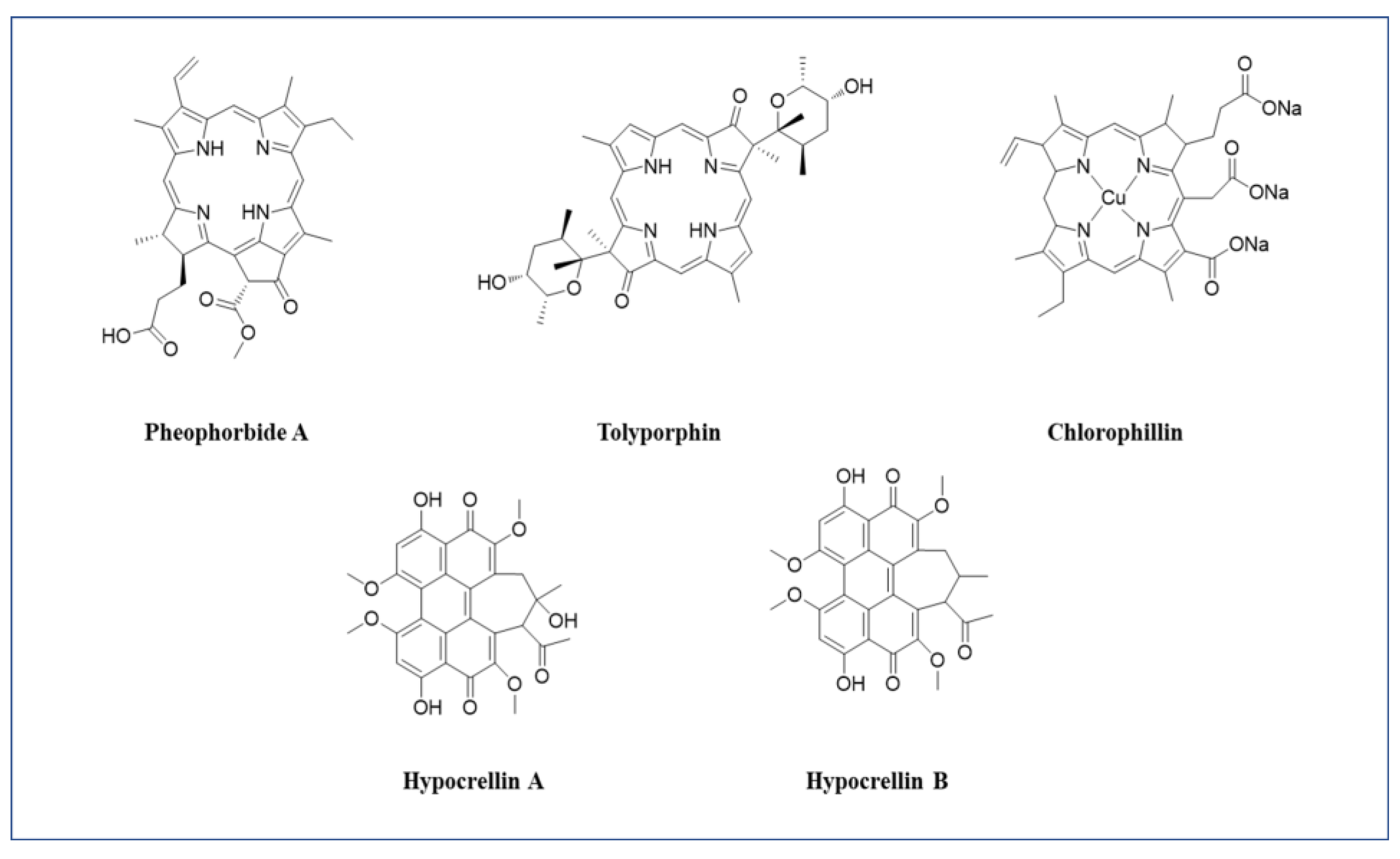
Figure 4. Chemical formulas of the most common photoactive natural PS’s discussed.
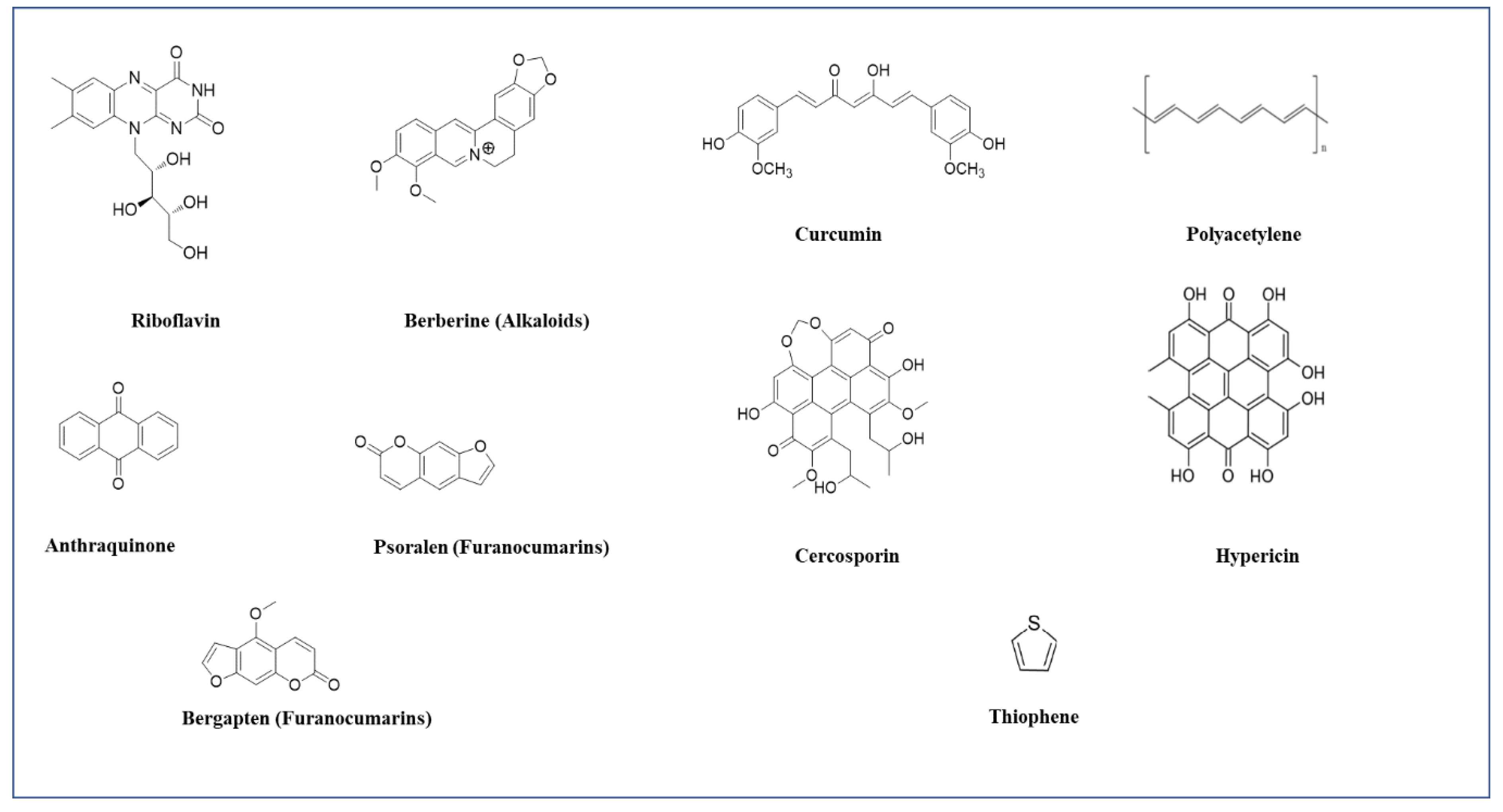
Figure 5. The chemical formulas of the most common photoactive natural PS’s discussed.
3.1.1. Pheophorbide A
For example, phototrophs are able to capture the energy in light thanks to photosynthetic pigments, such as chlorophyll and bacteriochlorophyll. Chlorophyll breakdown products are usually tested for their antioxidant and anti-inflammatory effects. The chlorophyll derivative pheophorbide a (PPBa) is a photosensitizer that can induce significant antiproliferative effects in several human cancer cell lines [61]. This compound is isolated from silkworm excreta [62] and Chinese medicinal herb Scutellaria barbarta [63]. Pheophorbide-b methyl ester, 13(2)-hydroxyl (13(2)-S) pheophorbide-a methyl ester and 13(2)-hydroxyl (13(2)-R) pheophorbide-b methyl ester all demonstrated dark cytotoxic activity against leukemia cells with IC(50) values in the range of 46–79 µM, whereas the compound pheophorbide—a methyl ester exhibited only weak dark cytotoxic activity [64].
Many studies report the inhibitory effect of pheophorbide a on the growth of human neoplastic cells. Studies regarding dark toxicities of pheophorbides are performed in hepatocellular carcinoma [65], human uterine cancer [66], glioblastoma multiforme [67] and bladder cancer [68]. PDT studies with the inhibitory effect of pheophorbide are reported in head and neck cancer [69], Barrett’s esophagus [70], leukemia [71], prostate cancer [72][73][74] and esophageal cancer [75].
Overall, the research suggests that PDT in combination with Pheophorbide a with the appropriate wavelength (670 nm) turns out to be a potential therapeutic strategy against many cancers.
3.1.2. Curcumins
Curcumin has recently been classified as both a PAINS (pan-assay interference compounds) and an IMPS (invalid metabolic panaceas) candidate [76].
Curcumin is a photosensitizer that is usually found in ketone and enol forms and is isolated from the Curcuma longa rhizome. Curcuminoids used in PDT significantly inhibited cell viability in breast cancer cell lines [77]. Demethoxycurcumin is known to have the highest anti-proliferative effect [78]; broad pharmacological activity of curcumin has been described, such as antibacterial, antiviral, anti-inflammatory and anti-tumor activities [79].
Koon et al., showed that the biological activity of curcumin can be magnified by the combination of light [80]. Subsequently, Dujiic et al. investigated the photodynamic effect of curcumin as an anticancer drug on a tumor model of A431 (human cell epithelial carcinoma). They showed that tumor growth was significantly inhibited in PDT, whereas the control group showed no reduction in tumor volume [81]. Several studies have been carried out with the use of curcumin in PDT and confirmed its anticancer and antibacterial properties [82][83][84][85]. The antiviral activity of photoactivated curcumin was presented in treatment of norovirus surrogates, feline calicivirus (FCV), and murine norovirus (MNV). Results showed that photoactivated curcumin at 50 µg/mL reduced FCV titers by almost 5 log after incubation at 37 °C for 30 min. Lower antiviral activity (0.73 log TCID50/mL reduction) was reported for MNV. At room temperature, curcumin at 5 µg/mL reduced FCV titers by 1.75 log TCID50/mL. These results represent a step forward in improving food safety using photoactivated curcumin as an alternative natural additive to reduce viral contamination [86].
3.1.3. Anthraquinones
Anthraquinones are a group of compounds that have been isolated from the leaves and stems of the Heterophyllaea pustulata Hook f. (Rubiaceae) plant. They show a natural phototoxic effect, and the photosensitizing properties are due to the production of singlet oxygen and/or a superoxide anion radical [89]. Comini et al. [45] anthraquinones such as soranjidiol, soranjidiol 1-methyl ether, rubiadin and rubiadin 1-methyl were found to exhibit PDT activity against human breast cancer cells transfected with caspase-3 (MCF-7) [78]. The AQs were reported as kinase and tyrosinase inhibitors as well as cytotoxicity agents. The M. elliptica AQs such as morindone, soranjidiol and rubiadin were also reported for their antitumor activity against lymphocytic leukemia (P-388) cells.
Rumie Vittar et al. [90] presented innovative evidence confirming the anti-tumor activity of rubiadin in combination with soranjidiol in in vitro photodynamic therapy, triggering the process of apoptosis in human cancer cells. They showed that the combination can be an effective therapeutic strategy.
3.1.4. Polyacetylene and Thiophenes
Thiophene derivatives are characterized by cytotoxic and phototoxic properties towards neoplastic cells [91]. The cytotoxic properties of the thiophenes were not observed in the absence of light. Polyacetylene and thiophene compounds are activated or excited by light with a wavelength of 314–350 nm [92]. Thiophenes derived from Echinops latifolius Tausch root are cytotoxic to human cancer cell lines including A375-S2, HeLa, HL-60, K562 and MCF-7 [93][94][95]. Apart from a strong cytotoxic effect on human tumor cell lines, strong analgesic, anti-inflammatory and antibacterial properties are mentioned. After irradiation with near UV light, α-terthienyl and most of its analogues had significant toxicity, with minimum inhibitory concentrations in the range of 0.02–40 μM. Without irradiation Thiophene compounds had no significant toxicity [96].
3.1.5. Tolyporphin
Cyanobacteria are the source of tolyporphins, a member of the porphyrin family. It locates in the endoplasmic reticulum (ER) and is associated with strong phototoxicity in PDT. After the use of tolyporphins, damage to the nuclear membrane has been observed, which may damage neoplastic cells, and indirectly also affect vascular damage [95][97].
3.1.6. Chlorophyllin
Cyanobacteria are also a source of chlorophyllin, which is a derivative of chlorophyll. Chlorophyllin is mainly localized in lysosomes and mitochondria, whereby cancer cells are destroyed by autophagy and apoptosis in PDT. Studies have shown that chlorophyllin has favorable optical properties (600–670 nm) and solubility in aqueous solutions. It is also readily available and chlorophyllin has been successfully used against cancer cells of the bladder [98][99] and of the MCF7 breast cancer cell line [100].
3.1.7. Hypericin
Hypericin is an anthraquinone derivative, isolated from the herb Hipericum perforatum. It is widely used in folk medicine, as an antiviral, antidepressant, natural antibiotic and as an anti-cancer drug [101].
The photodynamic activity of hypericin is attributed to its high cell uptake due to high lipophilicity. It is a molecule that requires a carrier in the form of liposomes, micelles or nanoparticles [102]. Theodossiou et al. investigated the hypericin-PDT mechanism and showed that hypericin accumulates mainly in the membranes of various organelles, especially the mitochondria and the endoplasmic reticulum (ER)–Golgi complex, inducing cell death through both Type I and Type II reactions [103]. In photodynamic therapy with hypericin, the produced reactive oxygen species can cause oxidative damage and destroy neoplastic tumors [104]. According to studies, the main mechanisms of cancer cell death after hypericin-PDT are apoptosis, autophagy and necrosis [105][106].
Due to the low solubility of hypericin and the short absorption wavelength (590 nm), a large number of analogues was synthesized, which improved its physicochemical properties [107].
Hypericin-mediated PDT has been used in the treatment of skin [108] cervical [109][110] glioblastoma [111] and bladder tumors [112]. Treatment with activated hypericin of patients with nasopharyngeal carcinoma cells [113] and human pancreatic cells [114] is promising. In summary, hypericin is one of the strongest PS extracted from natural sources [115].
Liposomal meso-tetrahydroxyphenyl chlorin derivative (Foslipos®) and hypericin was used in 1:1 combination to treat head and neck squamous cell carcinoma (HNSCC) cell lines (UMB-SCC 745 and UMB-SCC). Foslipos®-treated cells showed cellular toxicity at the highest concentration (10 µg/mL). In contrast, hypericin was toxic at all concentrations (10–0.6 µg/mL). The combination of photosensitizer was nontoxic at all concentrations (10–0.6 µg/mL). Data have shown that combinatorial use reduces the toxicity of the PS, which may be beneficial in the treatment of PDT [116].
ROS fluorescence was only visible after hypericin and mixture-induced PDT. Cell viability was also more affected with these two treatment options under the selected conditions. Examination of death pathways showed that hypericin-mediated cell death was apoptotic, with mTHPC necrotic and the 1:1 mixture showed features of both [117].
3.1.8. Hypocrellin
Hypocrellins are isolated from the parasitic fungi Hypocrella bambusae and Shiraia bambusicola, found mainly in Asia. There is hypocrellin a and b which belong to the general class of perylene quinonoid pigments. These compounds have been extensively studied as photosensitizers in PDT. Hypocrellins are characterized by high singlet oxygen quantum efficiency, which has attracted attention as potential PS for PDT. Activated hypocrellins produce reactive oxygen species and hypocrellin radicals, which may contribute to phototoxicity of cells. Hypocrellins have the property of easy chemical modification to increase phototoxicity, pharmacokinetics, solubility and light absorption in the red spectral region [118]. The absorption of the wavelength of the hypocrellins is below 600nm, which is considered a disadvantage as PS. Hypocrellins have an affinity for binding to lipids and may also be located in lysosomal compartments, mitochondria and cell membranes [119]. Cell death occurs through apoptosis or necrosis through peroxidation of lipid membranes [120].
3.1.9. Cercosporin
The toxic effect of cercosporin as PS is the production of singlet oxygen, which causes the formation of free radicals, which in turn damage the cytoplasmic membrane and ultimately cell lysis [124]. Cercospora kikuchii is a source of cercosporin extraction, while related elsinochromes are derived from the Elsinoe fungus family [125]. Mastrangelopoulou et al. showed that cercosporin is localized in both the endoplasmic reticulum and mitochondrial membranes and cell death occurs through apoptosis and necrosis [125]. The disadvantage of cercosporin in clinical use is its short activation wavelength (below 532 nm) and poor water solubility.
The photocytotoxicity of cyclosporine was assessed positively against two human glioblastoma cell lines (T98G and U87) and one breast adenocarcinoma (MCF7) with positive results [126].
Cercosporin is a strong photosensitizer, but with a short activation wavelength, making it mainly suitable for superficial PDT treatments [127].
3.1.10. Riboflavin
Leafy vegetables are a main rich source of riboflavin (vitamin B2), but also mushrooms and dairy products also contain it. It is a promising alternative PS molecule which generates ROS after exposure to blue light. Riboflavin has two peaks in the UVA (360 nm) and blue (440 nm) wavelength regions [128].
Due to its favorable and well-known toxicological and pharmacokinetic properties [102][103], riboflavin is recognized by the FDA as generally safe [129]. Hassan et al. [130][131] reported that riboflavin-PDT may support cisplatin-based chemotherapy by alleviating cisplatin-induced toxicity. Riboflavin increased the sensitivity of cisplatin-resistant tumor cells in a mouse model. Cancer cells entered the path of apoptosis and autophagy under the influence of a riboflavin–PDT adjuvant. The results suggest that in PDT therapy, cisplatin in combination with riboflavin may be a better treatment option in cancer patients than cisplatin alone.
3.1.11. Alkaloids
Alkaloids are a diverse group of secondary metabolites obtained from higher plants. The chemical structure classifies them as heterocyclic compounds with a nitrogen atom in the ring. The representative alkaloid considered to be the most photochemical is berberine [135][136]. Numerous studies demonstrate that berberine has anti-cancer properties enhanced by UV radiation and blue light [137][138]. Photoactivation of berberine occurs at a wavelength of 410 nm and has been shown to be effective in controlling the growth of brain cancer cells [139]. Lopes et al. confirmed that berberine has promising potential as a photosensitizer in PDT. Their proposed treatment induced changes in metabolites related to cell proliferation, tumor formation and angiogenesis in renal cell carcinoma (RCC) [139] and in cervical cancer cells (HaCaT) [140].
Thus, they confirmed a significant anti-cancer effect on kidney cancer cells. Activa berberine promotes autophagy and apoptosis by producing ROS [137][138][139][140]. Berberine can be used as a natural PS in PDT applications with minimal side effects [141].
Among the alkaloids, carboline [142] and harmine [143] are distinguished as strong photosensitizers. They are highly photoactive compounds and after irradiation they produce a significant amount of ROS [143].
Jantova et al. confirmed the ability of alkaloids to photosensitize and generate ROS in the presence of a light source [144].
3.1.12. Furanocoumarins
Furanocoumarins are a structurally diverse group of natural substances, i.e., secondary metabolites isolated from higher plants, showing a number of bioactivities, including anti-cancer [145].
The most active photoactive substance is psoralen, sensitive to UVA light in the wavelength range of 300–400 nm. It has been shown to be effective in the treatment of psoriasis, dermatitis, eczema and other skin problems [146]. Numerous studies indicate the anti-cancer activity of furanocoumarins against various types of cancer, such as breast, skin and leukemia. When exposed to light, furanocoumarins induce cancer cell death by inhibiting the signal transducer and activator of transcription3 (STAT3), nuclear factor B (NF-B), phosphatidylinositol-3 kinase and AKT protein expression. These pathways play a key role in tumor development by activating several inflammatory genes. Panno et al. investigated the efficacy of furanocoumarins against breast cancer. They found inhibition of tumor growth by inhibiting STAT3 protein expression [147].
On the other hand, the team of Kim et al. [148][149] showed that in leukemia cells, furanocoumarins inactivated JAK (Janus-activated kinase), c-Src and STAT3 proteins and lowered the concentrations of Bcl-xl and Bcl-2 proteins, which are responsible for the apoptosis process. Increased activity of furanocoumarins, bergapten and citroptenhas, also been demonstrated after UV irradiation against malignant melanoma (A375) [150].
Psoralen and its derivatives like 5-methoxypsoralen (5-MOP) and 8-methoxypsoralen (8-MOP) increase cytotoxicity after UV irradiation with a wavelength of 320–400 nm and are effective against cutaneous T-cell lymphoma [151][152].
PUVA (Psoralen Ultra-Violet A) treatment has been shown furocoumarins having a methoxy group to be effective against B16F10 mouse melanoma cells [153].
References
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M. Global Cancer Observatory: Cancer Today. Lyon: International Agency for Research on Cancer. 2020. Available online: https://gco.iarc.fr/today/data/factsheets/cancers/39-All-cancers-fact-sheet.pdf (accessed on 1 December 2021).
- Agostinis, P.; Berg, K.; Cengel, K.A.; Foster, T.H.; Girotti, A.W.; Gollnick, S.O.; Hahn, S.M.; Hamblin, M.R.; Juzeniene, A.; Kessel, D.; et al. Photodynamic therapy of cancer: An update. CA Cancer J. Clin. 2011, 61, 250–281.
- Allison, R.R.; Moghissi, K. Photodynamic Therapy (PDT): PDT Mechanisms. Clin. Endosc. 2013, 46, 24–29.
- Yavari, N.; Andersson-Engels, S.; Segersten, U.; Malmstrom, P.U. An overview on preclinical and clinical experiences with photodynamic therapy for bladder cancer. Can. J. Urol. 2011, 18, 5778–5786.
- Railkar, R.; Agarwal, P.K. Photodynamic Therapy in the Treatment of Bladder Cancer: Past Challenges and Current Innovations. Eur. Urol. Focus 2018, 4, 509–511.
- Champeau, M.; Vignoud, S.; Mortier, L.; Mordon, S. Photodynamic therapy for skin cancer: How to enhance drug penetration? J. Photochem. Photobiol. B 2019, 197, 111544.
- Allegra, A.; Pioggia, G.; Tonacci, A.; Musolino, C.; Gangemi, S. Oxidative Stress and Photodynamic Therapy of Skin Cancers: Mechanisms, Challenges and Promising Developments. Antioxidants 2020, 9, 448.
- Ohtani, K.; Ikeda, N. Photodynamic Therapy for Lung Cancer. Kyobu Geka 2016, 69, 694–699.
- Wang, K.; Yu, B.; Pathak, J.L. An update in clinical utilization of photodynamic therapy for lung cancer. J. Cancer 2021, 12, 1154–1160.
- Shishkova, N.; Kuznetsova, O.; Berezov, T. Photodynamic Therapy in Gastroenterology. J. Gastrointest. Canc. 2013, 44, 251–259.
- Wu, H.; Minamide, T.; Yano, T. Role of photodynamic therapy in the treatment of esophageal cancer. Dig. Endosc. 2019, 31, 508–516.
- Yano, T.; Wang, K.K. Photodynamic Therapy for Gastrointestinal Cancer. Photochem. Photobiol. 2020, 96, 517–523.
- Sundaram, P.; Abrahamse, H. Effective Photodynamic Therapy for Colon Cancer Cells Using Chlorin e6 Coated Hyaluronic Acid-Based Carbon Nanotubes. Int. J. Mol. Sci. 2020, 21, 4745.
- Bicalho, L.S.; Figueiró Longo, J.P.; Villamizar, I.; Meneses de Almeida Santos, M.; Bentes Azevedo, R. Photodynamic Therapy, a new approach in the treatment of oral cancer. Rev. Univ. Ind. Santander. Salud 2010, 42, 167–174.
- Prażmo, E.J.; Kwaśny, M.; Łapiński, M.; Mielczarek, A. Photodynamic Therapy as a Promising Method Used in the Treatment of Oral Diseases. Adv. Clin. Exp. Med. 2016, 25, 799–807.
- Aniogo, E.C.; Plackal Adimuriyil George, B.; Abrahamse, H. The role of photodynamic therapy on multidrug resistant breast cancer. Cancer Cell Int. 2019, 19, 91.
- Banerjee, S.M.; El-Sheikh, S.; Malhotra, A.; Mosse, C.A.; Parker, S.; Williams, N.R.; MacRobert, A.J.; Hamoudi, R.; Bown, S.G.; Keshtgar, M.R. Photodynamic Therapy in Primary Breast Cancer. J. Clin. Med. 2020, 9, 483.
- Ostańska, E.; Aebisher, D.; Bartusik-Aebisher, D. The potential of photodynamic therapy in current breast cancer treatment methodologies. Biomed. Pharmacother. 2021, 137, 111302.
- Kwiatkowski, S.; Knap, B.; Przystupski, D.; Saczko, J.; Kędzierska, E.; Knap-Czop, K.; Kotlińska, J.; Michel, O.; Kotowski, K.; Kulbacka, J. Photodynamic therapy–mechanisms, photosensitizers and combinations. Biomed. Pharmacother. 2018, 106, 1098–1107.
- Juarranz, A.; Jaén, P.; Sanz-Rodríguez, F.; Cuevas, J.; González, S. Photodynamic therapy of cancer. Basic principles and applications. Clin. Transl. Oncol. 2008, 10, 148–154.
- Chilakamarthi, U.; Giribabu, L. Photodynamic Therapy: Past, Present and Future. Chem. Rec. 2017, 17, 775–802.
- Castano, A.P.; Demidova, T.N.; Hamblin, M.R. Mechanisms in photodynamic therapy: Part one-photosensitizers, photochemistry and cellular localization. Photodiagnosis Photodyn Ther. 2004, 1, 279–293.
- Bacellar, I.O.; Tsubone, T.M.; Pavani, C.; Baptista, M.S. Photodynamic Efficiency: From Molecular Photochemistry to Cell Death. Int. J. Mol. Sci. 2015, 16, 20523–20559.
- Greer, A. Christopher Foote’s discovery of the role of singlet oxygen 1O2 (1∆g) in photosensitized oxidation reactions. Acc. Chem. Res. 2006, 39, 797–804.
- Luksiene, Z. Photodynamic therapy: Mechanism of action and ways to improve the efficiency of treatment. Medicina 2003, 39, 1137–1150.
- Zhang, Q.; Li, L. Photodynamic combinational therapy in cancer treatment. J. BUON 2018, 23, 561–567.
- Mansoori, B.; Mohammadi, A.; Amin Doustvandi, M.; Mohammadnejad, F.; Kamari, F.; Gjerstorff, M.F.; Baradaran, B.; Hamblin, M.R. Photodynamic therapy for cancer: Role of natural products. Photodiagn. Photodyn. Ther. 2019, 26, 395–404.
- Mroz, P.; Yaroslavsky, A.; Kharkwal, G.B.; Hamblin, M.R. Cell death pathways in photodynamic therapy of cancer. Cancers 2011, 3, 2516–2539.
- Oniszczuk, A.; Wojtunik-Kulesza, K.A.; Oniszczuk, T.; Kasprzak, K. The potential of photodynamic therapy (PDT)-Experimental investigations and clinical use. Biomed. Pharmacother. 2016, 83, 912–929.
- Davies, M.J. Detection and characterisation of radicals using electron paramagnetic resonance (EPR) spin trapping and related methods. Methods 2016, 109, 21–30.
- Klaber, R. Phyto-photo-dermatitis. Br. J. Dermatol. 1942, 54, 193–211.
- Schild, A.L.; Motta, A.C.; Riet-Correa, F.; Karam, F.C.; Grecco, F.B. Photosensitization in cattle in Southern Brazil. In Poisonous Plants and Related Toxins; CABI International: London, UK, 2009; pp. 162–166.
- Le Quesne, W.; Do, M.N.; Ikram, M.; Israrkkhan, M.M.; Mir, I. Furocoumarins from the fruit of ammi visnaga. J. Nat. Prod. 1985, 48, 496.
- Stegelmeier, B.L.; Colegate, S.M.; Knoppel, E.L.; Rood, K.A.; Collett, M.G. Wild parsnip (Pastinaca sativa)-induced photosensitization. Toxicon 2019, 167, 60–66.
- Egyed, M.N.; Williams, M.C. Photosensitizing effects of cymopterus watsonii and cymopterus longipes in chickens and turkey poults. Avian Dis. 1977, 21, 566–575.
- Del Río, J.A.; Ortuño, A.; Pérez, I.; Bennett, R.G.; Real, D.; Correal, E. Furanocoumarin content in Bituminaria bituminosa varieties and Cullen species Options Méditerranéennes. Sér. A Mediterr. Semin. 2010, 92, 67–70.
- Schempp, C.M.; Schöpf, E.; Simon, J.C. Dermatitis bullosa striata pratensis durch Ruta graveolens L. (Gartenraute). Hautarzt 1999, 50, 432–434.
- Moan, J. Properties for optimal PDT sensitizers. J. Photochem. Photobiol. B 1990, 5, 521–524.
- Ormond, A.B.; Freeman, H.S. Dye Sensitizers for Photodynamic Therapy. Materials 2013, 6, 817–840.
- Allison, R.R.; Downie, G.H.; Cuenca, R.; Hu, X.H.; Childs, C.J.; Sibata, C.H. Photosensitizers in clinical PDT. Photodiagn. Photodyn. Ther. 2004, 1, 27–42.
- Lange, C.; Bednarski, P.J. Photosensitizers for Photodynamic Therapy: Photochemistry in the Service of Oncology. Curr. Pharm. Des. 2016, 22, 6956–6974.
- Abrahamse, H.; Hamblin, M.R. New photosensitizers for photodynamic therapy. Biochem. J. 2016, 473, 347–364.
- Yano, S.; Hirohara, S.; Obata, M.; Hagiya, Y.; Ogura, S.-I.; Ikeda, A.; Kataoka, H.; Tanaka, M.; Joh, T. Current states and future views in photodynamic therapy. J. Photochem. Photobiol. C Photochem. Rev. 2011, 12, 46–67.
- Rodrigues, M.C.; Muehlmann, L.A.; Longo, J.P.F.; Silva, R.C.; Graebner, I.B.; Degterev, I.A.; Lucci, C.M.; Azevedo, R.B.; Garci, M.P. Photodynamic Therapy Based on Arrabidaea chica (Crajiru) Extract Nanoemulsion: In vitro Activity against Monolayers and Spheroids of Human Mammary Adenocarcinoma MCF-7 Cells. J. Nanomed. Nanotechnol. 2015, 6, 286.
- Muniyandi, K.; George, B.; Parimelazhagan, T.; Abrahamse, H. Role of Photoactive Phytocompounds in Photodynamic Therapy of Cancer. Molecules 2020, 25, 4102.
- Newman, D.J.; Cragg, G.M. Natural Products as Sources of New Drugs over the Nearly Four Decades from 01/1981 to 09/2019. J. Nat. Prod. 2020, 83, 770–803.
- Huang, M.Y.; Zhang, L.L.; Ding, J.; Lu, J.J. Anticancer drug discovery from Chinese medicinal herbs. Chin. Med. 2018, 13, 35.
- Cordell, G.A.; Shin, Y.G. Finding the needle in the haystack. The dereplication of natural product extracts. Pure Appl. Chem. 1999, 71, 1089–1094.
- Alali, F.Q.; Tawaha, K. Dereplication of bioactive constituents of the genus hypericum using LC-(+,-)-ESI-MS and LC-PDA techniques: Hypericum triquterifolium as a case study. Saudi Pharm. J. 2009, 17, 269–274.
- Tan, P.J.; Appleton, D.R.; Mustafa, M.R.; Lee, H.B. Rapid identification of cyclic tetrapyrrolic photosensitisers for photodynamic therapy using on-line hyphenated LC-PDA-MS coupled with photo-cytotoxicity assay. Phytochem. Anal. 2012, 23, 52–59.
- Jong, W.W.; Tan, P.J.; Kamarulzaman, F.A.; Mejin, M.; Lim, D.; Ang, I.; Naming, M.; Yeo, T.C.; Ho, A.S.; Teo, S.H.; et al. Photodynamic activity of plant extracts from Sarawak, Borneo. Chem. Biodivers. 2013, 10, 1475–1486.
- Samat, N.; Tan, P.J.; Shaari, K.; Abas, F.; Lee, H.B. Prioritization of natural extracts by LC-MS-PCA for the identification of new photosensitizers for photodynamic therapy. Anal. Chem. 2014, 86, 1324–1331.
- Villacorta, R.B.; Roque, K.F.J.; Tapang, G.A.; Jacinto, S.D. Plant extracts as natural photosensitizers in photodynamic therapy: In vitro activity against human mammary adenocarcinoma MCF-7 cells. Asian Pac. J. Trop. Biomed. 2017, 7, 358–366.
- Sokolov, V.V.; Chissov, V.I.; Filonenko, E.V.; Sukhin, G.M.; Yakubovskaya, R.I.; Belous, T.A.; Zharkova, N.N.; Kozlov, D.N.; Smirnov, V.V. Photodynamic therapy of cancer with the photosensitizer PHOTOGEM. In Photodynamic Therapy of Cancer II; SPIE: Bellingham, WA, USA, 1995; Volume 2325.
- Romanko, Y.S.; Tsyb, A.F.; Kaplan, M.A.; Popuchiev, V.V. Effect of photodynamic therapy with photodithazine on morphofunctional parameters of M-1 sarcoma. Bull. Exp. Biol. Med. 2004, 138, 584–589.
- Wang, M.; Shengen, Y.; Liangwu, L.; He, H.; Tao, P.; Zhongtao, L.; Zhipeng, L.; Dongni, P.; Xiongying, M.; Yu, W.; et al. Anticancer Effect of Photodynamic Therapy with Photosan-Loaded Titanium Dioxide Nanoparticles on Panc-1 Pancreatic Cancer Cells. In Vitro. Sci. Adv. Mat. 2016, 8, 1145–1153.
- Sperandio, F.F.; Huang, Y.Y.; Hamblin, M.R. Antimicrobial photodynamic therapy to kill Gram-negative bacteria. Recent Pat. Antiinfect. Drug Discov. 2013, 8, 108–120.
- Tardivo, J.P.; Adami, F.; Correa, J.A.; Pinhal, M.A.; Baptista, M.S. A clinical trial testing the efficacy of PDT in preventing amputation in diabetic patients. Photodiagn. Photodyn. Ther. 2014, 11, 342–350.
- Petelin, M.; Perkič, K.; Seme, K.; Gašpirc, B. Effect of repeated adjunctive antimicrobial photodynamic therapy on subgingival periodontal pathogens in the treatment of chronic periodontitis. Lasers Med. Sci. 2015, 30, 1647–1656.
- Machorowska-Pieniążek, A.; Morawiec, T.; Olek, M.; Mertas, A.; Aebisher, D.; Bartusik-Aebisher, D.; Cieślar, G.; Kawczyk-Krupka, A. Advantages of using toothpaste containing propolis and plant oils for gingivitis prevention and oral cavity hygiene in cleft lip/palate patients. Biomed. Pharmacother. 2021, 142, 111992.
- Saide, A.; Lauritano, C.; Ianora, A. Pheophorbide a: State of the Art. Mar. Drugs 2020, 18, 257.
- Park, Y.J.; Lee, W.Y.; Hahn, B.S.; Han, M.J.; Yang, W.I.; Kim, B.S. Chlorophyll derivatives: A new photosensitizer for photodynamic therapy of cancer in mice. Yonsei Med. J. 1989, 30, 212–218.
- Chan, J.Y.; Tang, P.M.; Hon, P.M.; Au, S.W.; Tsui, S.K.; Waye, M.M.; Kong, S.K.; Mak, T.C.; Fung, K.P. Pheophorbide a, a major antitumor component purified from Scutellaria barbata, induces apoptosis in human hepatocellular carcinoma cells. Planta Med. 2006, 72, 28–33.
- Chou, S.T.; Chan, H.H.; Peng, H.Y.; Liou, M.J.; Wu, T.S. Isolation of substances with antiproliferative and apoptosis-inducing activities against leukemia cells from the leaves of Zanthoxylum ailanthoides Sieb. & Zucc. Phytomedicine 2011, 18, 344–348.
- Tang, P.M.; Chan, J.Y.; Au, S.W.; Kong, S.K.; Tsui, S.K.; Waye, M.M.; Mak, T.C.; Fong, W.P.; Fung, K.P. Pheophorbide a an active compound isolated from Scutellaria barbata, possesses photodynamic activities by inducing apoptosis in human hepatocellular carcinoma. Cancer Biol. Ther. 2006, 5, 1111–1116.
- Tang, P.M.; Liu, X.Z.; Zhang, D.M.; Fong, W.P.; Fung, K.P. Pheophorbide a based photodynamic therapy induces apoptosis via mitochondrial-mediated pathway in human uterine carcinosarcoma. Cancer Biol. Ther. 2009, 8, 533–539.
- Cho, M.; Park, G.M.; Kim, S.N.; Amna, T.; Lee, S.; Shin, W.S. Glioblastoma-specific anticancer activity of pheophorbide a from the edible red seaweed Grateloupia elliptica. J. Microbiol. Biotechnol. 2014, 24, 346–353.
- Bergstrom, L.C.; Vucenik, I.; Hagen, I.K.; Chernomorsky, S.A.; Poretz, R.D. In-vitro photocytotoxicity of lysosomotropic immunoliposomes containing pheophorbide a with human bladder carcinoma cells. J. Photochem. Photobiol. B 1994, 24, 17–23.
- Chung, P.S.; He, P.; Shin, J.I.; Hwang, H.J.; Lee, S.J.; Ahn, J.C. Photodynamic therapy with 9-hydroxypheophorbide alpha on AMC-HN-3 human head and neck cancer cells: Induction of apoptosis via photoactivation of mitochondria and endoplasmic reticulum. Cancer Biol. Ther. 2009, 8, 1343–1351.
- Qumseya, B.J.; David, W.; Wolfsen, H.C. Photodynamic therapy for barrett’s esophagus and esophageal carcinoma. Clin. Endosc. 2013, 46, 30–37.
- Lee, W.Y.; Lim, D.S.; Ko, S.H.; Park, Y.J.; Ryu, K.S.; Ahn, M.Y.; Kim, Y.R.; Lee, D.W.; Cho, C.W. Photoactivation of pheophorbide a induces a mitochondrial-mediated apoptosis in Jurkat leukaemia cells. J. Photochem. Photobiol. B 2004, 75, 119–126.
- Xu, D.D.; Lam, H.M.; Hoeven, R.; Xu, C.B.; Leung, A.W.; Cho, W.C. Photodynamic therapy induced cell death of hormone insensitive prostate cancer PC-3 cells with autophagic characteristics. Photodiagn. Photodyn. Ther. 2013, 10, 278–287.
- Della Pietra, E.; Simonella, F.; Bonavida, B.; Xodo, L.E.; Rapozzi, V. Repeated sub-optimal photodynamic treatments with pheophorbide a induce an epithelial mesenchymal transition in prostate cancer cells via nitric oxide. Nitric Oxide 2015, 45, 43–53.
- Gheewala, T.; Skwor, T.; Munirathinam, G. Photodynamic therapy using pheophorbide and 670 nm LEDs exhibits anti-cancer effects in-vitro in androgen dependent prostate cancer. Photodiagn. Photodyn. Ther. 2018, 21, 130–137.
- Wu, D.; Liu, Z.; Fu, Y.; Zhang, Y.; Tang, N.; Wang, Q.; Tao, L. Efficacy of 2-(1-hexyloxyethyl)-2-devinyl pyropheophorbide-a in photodynamic therapy of human esophageal squamous cancer cells. Oncol. Lett. 2013, 6, 1111–1119.
- Nelson, K.M.; Dahlin, J.L.; Bisson, J.; Graham, J.; Pauli, G.F.; Walters, M.A. The Essential Medicinal Chemistry of Curcumin. J. Med. Chem. 2017, 60, 1620–1637.
- Lin, H.-Y.; Lin, J.-N.; Ma, J.-W.; Yang, N.-S.; Ho, C.-T.; Kuo, S.-C.; Way, T.-D. Demethoxycurcumin induces autophagic and apoptotic responses on breast cancer cells in photodynamic therapy. J. Funct. Foods 2015, 12, 439–449.
- Comini, L.; Fernandez, I.; Vittar, N.R.; Montoya, S.N.; Cabrera, J.L.; Rivarola, V.A. Photodynamic activity of anthraquinones isolated from Heterophyllaea pustulata Hook f. (Rubiaceae) on MCF-7c3 breast cancer cells. Phytomedicine 2011, 18, 1093–1095.
- Ghosh, S.; Banerjee, S.; Sil, P.C. The beneficial role of curcumin on inflammation, diabetes and neurodegenerative disease: A recent update. Food Chem. Toxicol. 2015, 83, 111–124.
- Koon, H.; Leung, A.W.; Yue, K.K.; Mak, N.K. Photodynamic effect of curcumin on NPC/CNE2 cells. J. Environ. Pathol. Toxicol. Oncol. 2006, 25, 205–215.
- Dujic, J.; Kippenberger, S.; Ramirez-Bosca, A.; Diaz-Alperi, J.; Bereiter-Hahn, J.; Kaufmann, R.; Bernd, A.; Hofmann, M. Curcumin in combination with visible light inhibits tumor growth in a xenograft tumor model. Int. J. Cancer 2009, 124, 1422–1428.
- Jiang, Y.; Leung, A.W.; Hua, H.; Rao, X.; Xu, C. Photodynamic action of LED-activated curcumin against Staphylococcus aureus involving intracellular ROS increase and membrane damage. Int. J. Photoener. 2014, 2014, 637601.
- Wu, J.; Hou, W.; Cao, B.; Zuo, T.; Xue, C.; Leung, A.W.; Xu, C.; Tang, Q. Virucidal efficacy of treatment with photodynamically activated curcumin on murine norovirus bioaccumulated in oysters. Photodiagn. Photodyn. 2015, 12, 385–392.
- Wu, J.; Mou, H.; Xue, C.; Leung, A.W.; Xu, C.; Tang, Q. Photodynamic effect of curcumin on Vibrio parahaemolyticus. Photodiagn. Photodyn. 2016, 15, 34–39.
- Zeng, X.B.; Leung, A.W.N.; Xia, X.S.; Yu, H.P.; Bai, D.Q.; Xiang, J.Y.; Jiang, Y.; Xu, C.S. Effect of Blue Light Radiation on Curcumin-Induced Cell Death of Breast Cancer Cells. Laser Phys. 2010, 20, 1500–1503.
- Randazzo, W.; Aznar, R.; Sánchez, G. Curcumin-Mediated Photodynamic Inactivation of Norovirus Surrogates. Food Environ. Virol. 2016, 8, 244–250.
- Felouat, A.; D’Aléo, A.; Fages, F. Synthesis and photophysical properties of difluoroboron complexes of curcuminoid derivatives bearing different terminal aromatic units and a mesoaryl ring. J. Org. Chem. 2013, 78, 4446–4455.
- Fang, X.; Fang, L.; Gou, S.; Cheng, L. Design and synthesis of dimethylaminomethyl-substituted curcumin derivatives/analogues: Potent antitumor and antioxidant activity, improved stability and aqueous solubility compared with curcumin. Bioorg. Med. Chem. Lett. 2013, 23, 1297–1301.
- Montoya, S.C.; Comini, L.R.; Sarmiento, M.; Becerra, C.; Albesa, I.; Argüello, G.A.; Cabrera, J.L. Natural anthraquinones probed as Type I and Type II photosensitizers: Singlet oxygen and superoxide anion production. J. Photochem. Photobiol. B 2005, 78, 77–83.
- Rumie Vittar, N.B.; Comini, L.; Fernadez, I.M.; Agostini, E.; Nuñez-Montoya, S.; Cabrera, J.L.; Rivarola, V.A. Photochemotherapy using natural anthraquinones: Rubiadin and Soranjidiol sensitize human cancer cell to die by apoptosis. Photodiagn. Photodyn. Ther. 2014, 11, 182–192.
- Marles, R.J.; Hudson, J.B.; Graham, E.A.; Soucy-Breau, C.; Morand, P.; Compadre, R.L.; Compadre, C.M.; Towers, G.H.; Arnason, J.T. Structure-activity studies of photoactivated antiviral and cytotoxic tricyclic thiophenes. Photochem. Photobiol. 1992, 56, 479–487.
- Marles, R.J.; Compadre, R.L.; Compadre, C.M.; Soucy-Breau, C.; Redmond, R.W.; Duval, F.; Mehta, B.; Morand, P.; Scaiano, J.C.; Arnason, J.T. Thiophenes as mosquito larvicides: Structure-toxicity relationship analysis. Pestic. Biochem. Physiol. 1991, 41, 89–100.
- Zhang, P.; Jin, W.-R.; Shi, Q.; He, H.; Ma, Z.; Qu, H.-B. Two novel thiophenes from Echinops grijissi Hance. J. Asian Nat. Prod. Res. 2008, 10, 977–981.
- Morlière, P.; Mazière, J.C.; Santus, R.; Smith, C.D.; Prinsep, M.R.; Stobbe, C.C.; Fenning, M.C.; Golberg, J.L.; Chapman, J.D. Tolyporphin: A natural product from cyanobacteria with potent photosensitizing activity against tumor cells in vitro and in vivo. Cancer Res. 1998, 58, 3571–3578.
- Singh, R.K.; Tiwari, S.P.; Rai, A.K.; Mohapatra, T.M. Cyanobacteria: An emerging source for drug discovery. J. Antibiot. 2011, 64, 401–412.
- Naithani, R.; Mehta, R.G.; Shukla, D.; Chandersekera, S.N.; Moriarty, R.M. Antiviral Activity of Phytochemi-cals: A Current Perspective. Diet. Compon. Immune Funct. 2010, 421–468.
- Barnhart-Dailey, M.; Zhang, Y.; Zhang, R.; Anthony, S.M.; Aaron, J.S.; Miller, E.S.; Lindsey, J.S.; Timlin, J.A. Cellular localization of tolyporphins, unusual tetrapyrroles, in a microbial photosynthetic community determined using hyperspectral confocal fluorescence microscopy. Photosynth. Res. 2019, 141, 259–271.
- Gomaa, I.; Ali, S.E.; El-Tayeb, T.A.; Abdel-Kader, M.H. Chlorophyll derivative mediated PDT versus methotrexate: An in vitro study using MCF-7 cells. Photodiagn. Photodyn. Ther. 2012, 9, 362–368.
- Ichimaru, Y.; Kanaeda, N.; Tominaga, S.; Suzui, M.; Maeda, T.; Fujii, H.; Nakao, M.; Yoshioka, H. Sasa veitchii extract induces anticancer effects via inhibition of cyclin D1 expression in MCF-7 cells. Nagoya J. Med. Sci. 2020, 82, 509–518.
- Barnes, J.; Anderson, L.A.; Phillipson, J.D. St John’s wort (Hypericum perforatum L.): A review of its chemistry, pharmacology and clinical properties. J. Pharm. Pharmacol. 2001, 53, 583–600.
- Liu, X.; Jiang, C.; Li, Y.; Liu, W.; Yao, N.; Gao, M.; Ji, Y.; Huang, D.; Yin, Z.; Sun, Z.; et al. Evaluation of hypericin: Effect of aggregation on targeting biodistribution. J. Pharm. Sci. 2015, 104, 215–222.
- Theodossiou, T.A.; Hothersall, J.S.; De Witte, P.A.; Pantos, A.; Agostinis, P. The multifaceted photocytotoxic profile of hypericin. Mol. Pharm. 2009, 6, 1775–1789.
- Paba, V.; Quarto, M.; Varriale, L.; Crescenzi, E.; Palumbo, G. Photo-activation of hypericin with low doses of light promotes apparent photo-resistance in human histiocytic lymphoma U937 cells. J. Photochem. Photobiol. B 2001, 60, 87–96.
- Krammer, B.; Verwanger, T. Molecular response to hypericin-induced photodamage. Curr. Med. Chem. 2012, 19, 793–798.
- Davids, L.M.; Kleemann, B.; Cooper, S.; Kidson, S.H. Melanomas display increased cytoprotection to hypericin-mediated cytotoxicity through the induction of autophagy. Cell Biol. Int. 2009, 33, 1065–1072.
- Karioti, A.; Bilia, A.R. Hypericins as Potential Leads for New Therapeutics. Int. J. Mol. Sci. 2010, 11, 562–594.
- Schempp, C.M.; Winghofer, B.; Langheinrich, M.; Schöpf, E.; Simon, J.C. Hypericin levels in human serum and interstitial skin blister fluid after oral single-dose and steady-state administration of Hypericum perforatum extract (St. John’s wort). Skin Pharmacol. Appl. Skin Physiol. 1999, 12, 299–304.
- Vantieghem, A.; Xu, Y.; Declercq, W.; Vandenabeele, P.; Denecker, G.; Vandenheede, J.R.; Merlevede, W.; de Witte, P.A.; Agostinis, P. Different pathways mediate cytochrome c release after photodynamic therapy with hypericin. Photochem. Photobiol. 2001, 74, 133–142.
- Vantieghem, A.; Assefa, Z.; Vandenabeele, P.; Declercq, W.; Courtois, S.; Vandenheede, J.R.; Merlevede, W.; de Witte, P.; Agostinis, P. Hypericin-induced photosensitization of HeLa cells leads to apoptosis or necrosis. Involvement of cytochrome c and procaspase-3 activation in the mechanism of apoptosis. FEBS Lett. 1998, 440, 19–24.
- Weller, M.; Trepel, M.; Grimmel, C.; Schabet, M.; Bremen, D.; Krajewski, S.; Reed, J.C. Hypericin-induced apoptosis of human malignant glioma cells is light-dependent, independent of bcl-2 expression, and does not require wild-type p53. Neurol Res. 1997, 19, 459–470.
- Zupkó, I.; Kamuhabwa, A.R.; D’Hallewin, M.A.; Baert, L.; De Witte, P.A. In vivo photodynamic activity of hypericin in transitional cell carcinoma bladder tumors. Int. J. Oncol. 2001, 18, 1099–1105.
- Xu, C.; Leung, A. Light-activated hypericin induces cellular destruction of nasopharyngeal carcinoma cells. Laser. Phys. Lett. 2010, 7, 68.
- Liu, C.D.; Kwan, D.; Saxton, R.E.; McFadden, D.W. Hypericin and photodynamic therapy decreases human pancreatic cancer in vitro and in vivo. J. Surg. Res. 2000, 93, 137–143.
- Agostinis, P.; Vantieghem, A.; Merlevede, W.; de Witte, P.A. Hypericin in cancer treatment: More light on the way. Int. J. Biochem. Cell. Biol. 2002, 34, 221–241.
- Ali, S.M.; Olivo, M. Efficacy of hypocrellin pharmacokinetics in phototherapy. Int. J. Oncol. 2002, 21, 1229–1237.
- Besic Gyenge, E.; Forny, P.; Lüscher, D.; Laass, A.; Walt, H.; Maake, C. Effects of hypericin and a chlorin based photosensitizer alone or in combination in squamous cell carcinoma cells in the dark. Photodiagn. Photodyn. Ther. 2012, 9, 321–331.
- Gyenge, E.B.; Lüscher, D.; Forny, P.; Antoniol, M.; Geisberger, G.; Walt, H.; Patzke, G.; Maake, C. Photodynamic mechanisms induced by a combination of hypericin and a chlorin based-photosensitizer in head and neck squamous cell carcinoma cells. Photochem. Photobiol. 2013, 89, 150–162.
- Jin, S.; Zhou, L.; Gu, Z.; Tian, G.; Yan, L.; Ren, W.; Yin, W.; Liu, X.; Zhang, X.; Hu, Z.; et al. A new near infrared photosensitizing nanoplatform containing blue-emitting up-conversion nanoparticles and hypocrellin A for photodynamic therapy of cancer cells. Nanoscale 2013, 5, 11910–11918.
- Jiang, Y.; Leung, A.W.; Wang, X.; Zhang, H.; Xu, C. Effect of photodynamic therapy with hypocrellin B on apoptosis, adhesion, and migration of cancer cells. Int. J. Radiat. Biol. 2014, 90, 575–579.
- Jiang, Y.; Leung, W.; Tang, Q.; Zhang, H.; Xu, C. Effect of light-activated hypocrellin B on the growth and membrane permeability of gram-negative Escherichia coli cells. Int. J. Photoenergy 2014, 2014, 521209.
- Jiang, Y.; Leung, A.W.; Wang, X.; Zhang, H.; Xu, C. Inactivation of Staphylococcus aureus by photodynamic action of hypocrellin B. Photodiagn. Photodyn. 2013, 10, 600–606.
- Miller, G.G.; Brown, K.; Ballangrud, A.M.; Barajas, O.; Xiao, Z.; Tulip, J.; Lown, J.W.; Leithoff, J.M.; Allalunis-Turner, M.J.; Mehta, R.D.; et al. Preclinical assessment of hypocrellin B and hypocrellin B derivatives as sensitizers for photodynamic therapy of cancer: Progress update. Photochem. Photobiol. 1997, 65, 714–722.
- Jiang, Y.; Xia, X.; Leung, A.W.; Xiang, J.; Xu, C. Apoptosis of breast cancer cells induced by hypocrellin B under light-emitting diode irradiation. Photodiagn. Photodyn. 2012, 9, 337–343.
- Dolmans, D.E.; Fukumura, D.; Jain, R.K. Photodynamic therapy for cancer. Nat. Rev. Cancer 2003, 3, 380–387.
- Mastrangelopoulou, M.; Grigalavicius, M.; Berg, K.; Ménard, M.; Theodossiou, T.A. Cytotoxic and Photocytotoxic Effects of Cercosporin on Human Tumor Cell Lines. Photochem. Photobiol. 2019, 95, 387–396.
- Bouillaguet, S.; Wataha, J.C.; Zapata, O.; Campo, M.; Lange, N.; Schrenzel, J. Production of reactive oxygen species from photosensitizers activated with visible light sources available in dental offices. Photomed. Laser Surg. 2010, 28, 519–525.
- Corbin, F., 3rd. Pathogen inactivation of blood components: Current status and introduction of an approach using riboflavin as a photosensitizer. Int. J. Hematol. 2002, 76, 253–257.
- Zempleni, J.; Galloway, J.R.; McCormick, D.B. Pharmacokinetics of orally and intravenously administered riboflavin in healthy humans. Am. J. Clin. Nutr. 1996, 63, 54–66.
- Administration USFaD. Listing of Specific Substances Affirmed as GRAS. Available online: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=184.1695 (accessed on 6 December 2021).
- Hassan, I.; Chibber, S.; Khan, A.A.; Naseem, I. Riboflavin ameliorates cisplatin induced toxicities under photoillumination. PLoS ONE 2012, 7, e36273.
- Hassan, I.; Chibber, S.; Naseem, I. Vitamin B2: A promising adjuvant in cisplatin based chemoradiotherapy by cellular redox management. Food Chem. Toxi. 2013, 59, 715–723.
- Juarez, A.V.; Sosa Ldel, V.; De Paul, A.L.; Costa, A.P.; Farina, M.; Leal, R.B.; Torres, A.I.; Pons, P. Riboflavin acetate induces apoptosis in squamous carcinoma cells after photodynamic therapy. J. Photochem. Photobiol. B 2015, 153, 445–454.
- Yang, M.Y.; Chang, C.J.; Chen, L.Y. Blue light induced reactive oxygen species from flavin mononucleotide and flavin adenine dinucleotide on lethality of HeLa cells. J. Photochem. Photobiol. B 2017, 173, 325–332.
- Akasov, R.A.; Sholina, N.V.; Khochenkov, D.A.; Alova, A.V.; Gorelkin, P.V.; Erofeev, A.S.; Generalova, A.N.; Khaydukov, E.V. Photodynamic therapy of melanoma by blue-light photoactivation of flavin mononucleotide. Sci. Rep. 2019, 4, 9679.
- Benyhe, S. Morphine: New aspects in the study of an ancient compound. Life Sci. 1994, 55, 969–979.
- Och, A.; Podgórski, R.; Nowak, R. Biological Activity of Berberine-A Summary Update. Toxins 2020, 12, 713.
- Inbaraj, J.J.; Kukielczak, B.M.; Bilski, P.; Sandvik, S.L.; Chignell, C.F. Photochemistry and Photocytotoxicity of Alkaloids from Goldenseal (Hydrastis canadensis L.) 1. Berberine. Chem. Res. Toxicol. 2001, 14, 1529–1534.
- Andreazza, N.L.; Vevert-Bizet, C.; Bourg-Heckly, G.; Sureau, F.; Salvador, M.J.; Bonneau, S. Berberine as a Photosensitizing Agent for Antitumoral Photodynamic Therapy: Insights into its Association to Low Density Lipoproteins. Int. J. Pharm. 2016, 510, 240–249.
- Lopes, T.Z.; de Moraes, F.R.; Tedesco, A.C.; Arni, R.K.; Rahal, P.; Calmon, M.F. Berberine associated photodynamic therapy promotes autophagy and apoptosis via ROS generation in renal carcinoma cells. Biomed. Pharmacother. 2020, 123, 109794.
- Oliveira, P.M.; Lopes, T.Z.; Tedesco, A.C.; Rahal, P.; Calmon, M.F. Effect of berberine associated with photodynamic therapy in cell lines. Photodiagn. Photodyn. Ther. 2020, 32, 102045.
- Cheng, L.-L.; Wang, M.; Zhu, H.; Li, K.; Zhu, R.-R.; Sun, X.-Y.; Yao, S.-D.; Wu, Q.-S.; Wang, S.-L. Characterization of the transient species generated by the photoionization of Berberine: A laser flash photolysis study. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2009, 73, 955–959.
- Bhattacharyya, R.; Gupta, P.; Bandyopadhyay, S.K.; Patro, B.S.; Chattopadhyay, S. Coralyne, a protoberberine alkaloid, causes robust photosenstization of cancer cells through ATR-p38 MAPK-BAX and JAK2-STAT1-BAX pathways. Chem. Interact. 2018, 285, 27–39.
- Martín, J.P.; Labrador, V.; Freire, P.F.; Molero, M.L.; Hazen, M. Ultrastructural changes induced in HeLa cells after phototoxic treatment with harmine. J. Appl. Toxicol. 2004, 24, 197–201.
- Jantova, S.; Letašiová, S.; Brezová, V.; Cipak, L.; Lábaj, J. Photochemical and phototoxic activity of berberine on murine fibroblast NIH-3T3 and Ehrlich ascites carcinoma cells. J. Photochem. Photobiol. B 2006, 85, 163–176.
- Kubrak, T.; Podgórski, R.; Stompor-Gorący, M. Natural and Synthetic Coumarins and their Pharmacological Activity. Eur. J. Clin. Exp. Med. 2017, 15, 169–175.
- Panno, M.L.; Giordano, F.; Palma, M.G.; Bartella, V.; Rago, V.; Maggiolini, M.; Sisci, D.; Lanzino, M.; De Amicis, F.; Ando, S. Evidence that bergapten, independently of its photoactivation, enhances p53 gene expression and induces apoptosis in human breast cancer cells. Curr. Cancer Drug Targets 2009, 9, 469–481.
- Panno, M.L.; Giordano, F.; Rizza, P.; Pellegrino, M.; Zito, D.; Giordano, C.; Mauro, L.; Catalano, S.; Aquila, S.; Sisci, D.; et al. Bergapten induces ER depletion in breast cancer cells through SMAD4-mediated ubiquitination. Breast Cancer Res. Treat. 2012, 136, 443–455.
- Kim, S.-M.; Lee, J.H.; Sethi, G.; Kim, C.; Baek, S.H.; Nam, D.; Chung, W.-S.; Shim, B.S.; Ahn, K.S.; Kim, S.-H. Bergamottin, a natural furanocoumarin obtained from grapefruit juice induces chemosensitization and apoptosis through the inhibition of STAT3 signaling pathway in tumor cells. Cancer Lett. 2014, 354, 153–163.
- Kim, S.-M.; Lee, E.-J.; Lee, J.H.; Yang, W.M.; Nam, D.; Lee, J.H.; Lee, S.-G.; Um, J.-Y.; Shim, B.S.; Ahn, K.S. Simvastatin in combination with bergamottin potentiates TNF-induced apoptosis through modulation of NF-kB signalling pathway in human chronic myelogenous leukaemia. Pharm. Biol. 2016, 54, 2050–2060.
- Menichini, F.; Tundis, R.; Loizzo, M.R.; Bonesi, M.; Provenzano, E.; de Cindio, B.; Menichini, F. In vitro photo-induced cytotoxic activity of Citrus bergamia and C. medica L. cv. Diamante peel essential oils and identified active coumarins. Pharm Biol. 2010, 48, 1059–1065.
- Nagatani, T.; Matsuzaki, T.; Kim, S.; Baba, N.; Ichiyama, S.; Miyamoto, H.; Nakajima, H. Treatment of cutaneous T-cell lymphoma (CTCL) with extracorporeal photochemotherapy. J. Dermatol. Sci. 1990, 1, 226.
- Bethea, D.; Fullmer, B.; Syed, S.; Seltzer, G.; Tiano, J.; Rischko, C.; Gillespie, L.; Brown, D.; Gasparro, F.P. Psoralen photobiology and photochemotherapy: 50 years of science and medicine. J. Dermatol. Sci. 1999, 19, 78–88.
- Sumiyoshi, M.; Sakanaka, M.; Taniguchi, M.; Baba, K.; Kimura, Y. Anti-tumor effects of various furocoumarins isolated from the roots, seeds and fruits of Angelica and Cnidium species under ultraviolet A irradiation. J. Nat. Med. 2014, 68, 83–94.
More
Information
Subjects:
Allergy
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.9K
Revisions:
5 times
(View History)
Update Date:
29 Mar 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




