
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ayataka Fujimoto | + 2498 word(s) | 2498 | 2021-12-09 07:59:51 | | | |
| 2 | Lindsay Dong | + 1170 word(s) | 3668 | 2022-01-17 03:01:01 | | |
Video Upload Options
Epileptic spasms (ESs) are a type of epileptic seizure characterized as brief muscle contractions with ictal polyphasic slow waves on an electroencephalogram and a main feature of West syndrome. Resection surgeries, including frontal/posterior disconnections and hemispherotomy, have been established for the treatment of medically intractable ES in patients with unilaterally localized epileptogenic regions. Corpus callosotomy (CC) has been mainly used to treat drop attacks, which are classified as generalized tonic or atonic seizures. However, CC has also been adopted for ES treatment.
1. Introduction
2. Corpus Callosotomy for Epileptic Spasms
3. Efficacy of Corpus Callosotomy for Epileptic Spasms
3.1. Seizure Outcomes Post-Corpus Callosotomy for Epileptic Spasms
| Authors | N: CC for ES (Total N of Any Size) | Age at 1st CC | Seizure Types (ES and Others) | MRI Lesion (+/-) | Procedures of Resection | |
|---|---|---|---|---|---|---|
| 1 | Pinard et al. 1999 [23] | 14 (17) | 1.7–14.3 years | ES only: 36% ES + generalized: 64% |
Unknown | ACC only: 2 ACC→TCC: 10 PCC→TCC: 2 |
| 2 | Ono et al. 2011 [3] | 7 (19) | 0.4–3 years | ES only: 86% ES + focal + generalized: 14% |
MRI lesion (+): 28% Bilateral: 28% |
ACC→CR: 14% ACC→TCC→CR: 14% TCC→CR: 57% TCC→PQD: 14% |
| 3 | Otsuki et al. 2016 [4] | 10 (30) | Unknown | Unknown | Unknown | TCC only: 100% |
| 4 | Iwasaki et al. 2016 [32] | 8 (26) | 1–14 years | ES only: 50% ES + generalized: 50% |
MRI lesion (+): 50% Unilateral: 13% Bilateral: 38% |
TCC only: 100% |
| 5 | Baba et al. 2018 [6] | 56 | 0.4–1.9 years | ES only: 84% ES + generalized: 16% |
MRI lesion (+): 0% | ACC only: 4% ACC→TCC: 5% TCC only: 91% |
| 6 | Baba et al. 2019 [8] | 42 | 0.6–7 years | ES only: 43% ES + focal: 7% ES + generalized: 50% |
MRI lesion (+): 21% | TCC only: 79% TCC→AQD/PQD/SHR/HR: 21% |
| 7 | Okanishi et al. 2019 [9] | 7 | 2.1–21.5 years | ES only: 29% ES + focal: 29% ES + generalized: 43% |
MRI lesion (+): 100% (bilateral tubers only) | TCC only: 71% TCC + CR/PQD: 29% |
| 8 | Kanai et al. 2019 [10] Oguri et al. 2020 [11] (Using the same patient data) |
17 | 1.4–19.8 years | ES only: 18% ES + others: 82% |
MRI lesion (+): 65% | ACC only: 18% TCC only: 82% |
| 9 | Uda et al. 2021 [12] | 8 (10) | 0.8–9.1 years | Unknown | MRI lesion (+): 0% | TCC only: 63% (5/8) TCC→AQD/PQD/HR: 37% (3/8) |
| ES outcomes | Good prognostic factor | Others | ||||
| 1 | Seizure free: 79% (after final CC) | NA | - | |||
| 2 | Seizure free: 71% (TCC + others) | NA | This study reported only cases involving additional resection/disconnection. | |||
| 3 | Seizure free: 70% | NA | Described as part of 67 surgical study cases | |||
| 4 | Seizure free: 38% | MRI lesion (-) | - | |||
| 5 | Seizure free: 43% > 80% reduction: 23% |
low DQ | This study included only non-lesional cases | |||
| 6 | Seizure free: 26% (after TCC) Seizure free: 43% (TCC ± others) |
Low gamma power and connectivity (scalp EEG) | - | |||
| 7 | Seizure free: 43% (after TCC) Seizure free: 71% (TCC ± others) |
NA | Involved only patients with TSC. One patient achieved seizure freedom after taking everolimus additionally | |||
| 8 | Seizure free: 41% | Symmetrical ictal slow waves (scalp EEG) Low interhemispheric phase lags (scalp EEG) |
Some epileptic spasms were described as tonic spasms in Kanai et al.’s study [7] | |||
| 9 | Seizure free: 25% (after TCC) Seizure free: 63% (TCC ± others) |
NA | AQD without CC was selected for two patients based on a presurgical evaluation | |||
3.2. Effects on Developments in Patients with Epileptic Spasms
4. Prognostic Factors for Seizure Outcomes Post-Corpus Callosotomy
5. Surgical Treatment Selection: Resection Surgery or Corpus Callosotomy First?
5.1. Resection Surgeries and Adaptations for Epileptic Spasms
| Authors | N | Age at Surgery | Seizure Types or Symmetry of ES | MRI Lesion | Procedures of Resection | |
|---|---|---|---|---|---|---|
| 1 | Chugani et al. 2015 [16] | 65 | 5.1 ± 4.4 years (0.2–19 years) |
ES only: 23% ES + focal: 58% ES + generalized: 11% |
Lesion (+): 92% | Hemispherectomy: 31% Subtotal hemispherotomy: 26% Multilobar: 20% Lobar ± tuberectomy: 14% Tuberectomy: 9% |
| 2 | Barba et al. 2016 [17] | 80 | 5.8 ± 4.0 years | Symmetric ES: 49% Asymmetric ES: 24% Both types: 28% |
Lesion (+): 96% | Lobectomy: 72.5% Multilobar/hemispherotomy: 27.5% |
| 3 | Chipaux et al. 2017 [18] | 59 | 4.6 ± 3.5 years (0.3–16 years) |
ES only: 15% ES + others: 85% |
Lesion (+): 96% | Hemispherotomy: 34% Lesionectomy: 8% Lesionectomy + cortical resection *: 46% Frontal disconnection: 8% Posterior disconnection: 3% Endoscopic HH removal: 3% |
| 4 | Erdemir et al. 2021 [19] | 70 | 1.9 ± 1.6 years | ES only: 46% ES + others: 54% Symmetric: 54% Asymmetric: 40% Unknown symmetry: 6% |
Lesion (+): 100% Bilateral: 24% Unilateral: 76% |
Hemispherectomy: 44% Lobectomy/lesionectomy: 33% Multilobar resection: 23% |
| 5 | Liu et al. 2021 [20] | 64 | 3.3 ± 2.7 years | ES only: 64% ES + others: 36% |
Lesion (+): 83% | Hemispherotomy/subtotal hemispherotomy: 27% Multilobar: 11% Lobar: 34% Tuberectomy: 23% Unknown: 3% |
| Outcomes | Good Prognostic Factor | Others | ||||
| 1 | Seizure free: 71% | Short epilepsy duration MRI lesion (+) |
22 patients discontinued medication after surgery | |||
| 2 | Seizure free: 61% | Complete resection of SOZ MRI lesion (+) Low age at surgery/short epilepsy duration |
ECoG monitoring: 30% | |||
| 3 | Seizure free: 75% | Low age at surgery | Visible epileptogenic lesions on MRI in most cases. Eight patients were declined surgery following presurgical evaluation because of multiple foci. | |||
| 4 | Seizure free: 60% Improvement: 24% |
Lobar/sublobar epileptogenic lesion | MRI-oriented surgery No invasive EEG (ECoG) |
|||
| 5 | Seizure free: 83% ** | Concordances: between MRI and scalp EEG between PET and scalp EEG Frequent interictal gamma activities (scalp EEG) Intraoperative continuous discharges (ECoG) |
ECoG monitoring: 95% Stereo-EEG: 20% |
|||
5.2. Characteristics of Patients Who Undergo Corpus Callosotomy
In previous studies regarding CC, patients tended not to have localized or lateralized signs or findings. The largest study concerning CC surgery for patients with ES by Baba et al. included 56 patients without MRI lesions. They reported that 43% of patients were seizure-free and that 23% of patients had a ≥80% seizure reduction postoperatively [6]. CC has also been performed for patients with bilateral diffuse or multiple lesions in patients with polymicrogyria, cortical tubers, or general atrophy on brain MRI [3][7][9][31]. Criteria for CC surgery to treat ES have included patients with no lesion or equally bilateral epileptogenic lesions selected for CC surgery. Factors such as presurgical severe developmental delay [6] and symmetrical ictal slow waves [10] on presurgical EEG findings have been associated with favorable CC outcomes. Based on advanced analyses for presurgical EEG, less power and less connectivity of high-gamma activities on presurgical scalp EEG [8] recordings and lower phase lags in ictal slow and gamma waves among bilateral hemispheres [11] have been associated with favorable seizure outcomes.
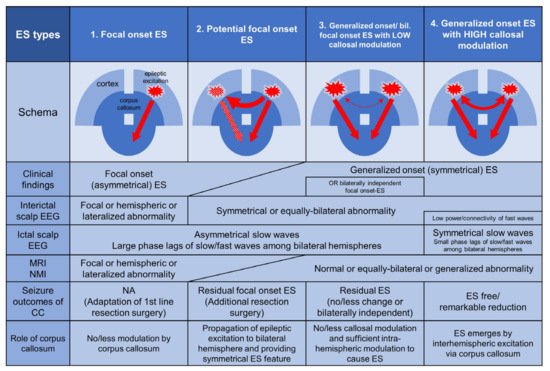
5.3. Types of Epileptic Spasms in Terms of Cortical Excitations and the Role of Corpus Callosum
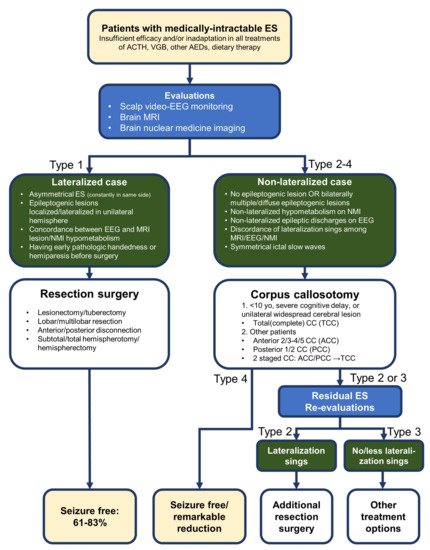
5.4. Surgical Selection Flow Proposals
References
- Van Wagenen, W.P.; Herren, R.Y. Surgical Divisions of Commissural Pathways in the Corpus Callosum. Arch. Neurol. Psychiatry 1940, 447, 740.
- Pinard, J.M.; Delalande, O.; Plouin, P.; Dulac, O. Callosotomy in West Syndrome Suggests a Cortical Origin of Hyp-sarrhythmia. Epilepsia 1993, 34, 780–787.
- Ono, T.; Baba, H.; Toda, K.; Ono, K. Callosotomy and Subsequent Surgery for Children with Refractory Epilepsy. Epilepsy Res. 2011, 93, 185–191.
- Otsuki, T.; Kim, H.D.; Luan, G.; Inoue, Y.; Baba, H.; Oguni, H.; Hong, S.C.; Kameyama, S.; Kobayashi, K.; Hirose, S.; et al. Surgical Versus Medical Treatment for Children with Epileptic Encephalopathy in Infancy and Early Childhood: Results of an International Multicenter Cohort Study in Far-East Asia (the FACE Study). Brain Dev. 2016, 38, 449–460.
- Iwasaki, M.; Nakasato, N.; Kakisaka, Y.; Kanno, A.; Uematsu, M.; Haginoya, K.; Tominaga, T. Lateralization of Inter-ictal Spikes After Corpus Callosotomy. Clin. Neurophysiol. 2011, 122, 2121–2127.
- Baba, H.; Toda, K.; Ono, T.; Honda, R.; Baba, S. Surgical and Developmental Outcomes of Corpus Callosotomy for West Syndrome in Patients Without MRI Lesions. Epilepsia 2018, 59, 2231–2239.
- Baba, S.; Okanishi, T.; Nishimura, M.; Kanai, S.; Itamura, S.; Suzuki, T.; Masuda, Y.; Enoki, H.; Fujimoto, A. Effectiveness of Total Corpus Callosotomy for Diffuse Bilateral Polymicrogyria: Report of Three Pediatric Cases. Brain Dev. 2018, 40, 719–723.
- Baba, S.; Vakorin, V.A.; Doesburg, S.M.; Nagamori, C.; Cortez, M.A.; Honda, R.; Ono, T.; Toda, K.; Nishimoto, H.; Ebihara, T.; et al. EEG Before and After Total Corpus Callosotomy for Pharmacoresistant Infantile Spasms: Fast Oscillations and Slow-Wave Connectivity in Hypsarrhythmia. Epilepsia 2019, 60, 1849–1860.
- Okanishi, T.; Fujimoto, A.; Okanari, K.; Baba, S.; Ichikawa, N.; Nishimura, M.; Enoki, H. Corpus Callosotomy for Drug-Resistant Spasms Associated with Tuberous Sclerosis Complex. Epilepsy Behav. 2019, 98, 228–232.
- Kanai, S.; Oguri, M.; Okanishi, T.; Itamura, S.; Baba, S.; Nishimura, M.; Homma, Y.; Maegaki, Y.; Enoki, H.; Fujimoto, A. Symmetry of Ictal Slow Waves May Predict the Outcomes of Corpus Callosotomy for Epileptic Spasms. Sci. Rep. 2019, 9, 19733.
- Oguri, M.; Okanishi, T.; Kanai, S.; Baba, S.; Nishimura, M.; Ogo, K.; Himoto, T.; Okanari, K.; Maegaki, Y.; Enoki, H.; et al. Phase Lag Analyses on Ictal Scalp Electroencephalography May Predict Outcomes of Corpus Callosotomy for Epileptic Spasms. Front. Neurol. 2020, 11, 576087.
- Uda, T.; Kuki, I.; Inoue, T.; Kunihiro, N.; Suzuki, H.; Uda, H.; Kawashima, T.; Nakajo, K.; Nakanishi, Y.; Maruyama, S.; et al. Phase-Amplitude Coupling of Interictal Fast Activities Modulated by Slow Waves on Scalp EEG and Its Correlation with Seizure Outcomes of Disconnection Surgery in Children with Intractable Nonlesional Epileptic Spasms. J. Neurosurg. Pediatr. 2021, 26, 1–9.
- Fusco, L.; Vigevano, F. Ictal Clinical Electroencephalographic Findings of Spasms in West Syndrome. Epilepsia 1993, 34, 671–678.
- Vigevano, F.; Fusco, L.; Pachatz, C. Neurophysiology of Spasms. Brain Dev. 2001, 23, 467–472.
- Chugani, H.T. Pathophysiology of Infantile Spasms. Adv. Exp. Med. Biol. 2002, 497, 111–121.
- Chugani, H.T.; Ilyas, M.; Kumar, A.; Juhász, C.; Kupsky, W.J.; Sood, S.; Asano, E. Surgical Treatment for Refractory Epileptic Spasms: The Detroit Series. Epilepsia 2015, 56, 1941–1949.
- Barba, C.; Mai, R.; Grisotto, L.; Gozzo, F.; Pellacani, S.; Tassi, L.; Francione, S.; Giordano, F.; Cardinale, F.; Guerrini, R. Unilobar Surgery for Symptomatic Epileptic Spasms. Ann. Clin. Transl. Neurol. 2017, 4, 36–45.
- Chipaux, M.; Dorfmüller, G.; Fohlen, M.; Dorison, N.; Metten, M.A.; Delalande, O.; Ferrand-Sorbets, S.; Taussig, D. Refractory Spasms of Focal Onset-A Potentially Curable Disease That Should Lead to Rapid Surgical Evaluation. Seizure 2017, 51, 163–170.
- Erdemir, G.; Pestana-Knight, E.; Honomichl, R.; Thompson, N.R.; Lachhwani, D.; Kotagal, P.; Wyllie, E.; Gupta, A.; Bingaman, W.E.; Moosa, A.N.V. Surgical Candidates in Children with Epileptic Spasms Can Be Selected Without Invasive Monitoring: A Report of 70 Cases. Epilepsy Res. 2021, 176, 106731.
- Liu, Y.; Zhou, W.; Hong, B.; Wang, H.; Lin, J.; Sun, Z.; Wang, S. Analysis of Surgical Strategies for Children with Epileptic Spasms. Epileptic Disord. 2021, 23, 85–93.
- Talwar, D.; Baldwin, M.A.; Hutzler, R.; Griesemer, D.A. Epileptic Spasms in Older Children: Persistence Beyond Infancy. Epilepsia 1995, 36, 151–155.
- Pinard, J.M.; Delalande, O.; Chiron, C.; Soufflet, C.; Plouin, P.; Kim, Y.; Dulac, O. Callosotomy for epilepsy after West syndrome. Epilepsia 1999, 40, 1727–1734.
- Wong, T.T.; Kwan, S.Y.; Chang, K.P.; Hsiu-Mei, W.; Yang, T.F.; Chen, Y.S.; Yi-Yen, L. Corpus Callosotomy in Children. Childs Nerv. Syst. 2006, 22, 999–1011.
- Kwan, S.Y.; Lin, J.H.; Wong, T.T.; Chang, K.P.; You, C.H. A comparison of seizure outcome after callosotomy in patients with Lennox-Gastaut syndrome and a positive or negative history for West syndrome. Seizure 2006, 15, 552–557.
- Lee, Y.J.; Lee, J.S.; Kang, H.C.; Kim, D.S.; Shim, K.W.; Eom, S.; Kim, H.D. Outcomes of Epilepsy Surgery in Childhood-Onset Epileptic Encephalopathy. Brain Dev. 2014, 36, 496–504.
- Itamura, S.; Okanishi, T.; Nishimura, M.; Kanai, S.; Baba, S.; Masuda, Y.; Homma, Y.; Enoki, H.; Fujimoto, A. Analysis for the Association Between Corpus Callosum Thickness and Corpus Callosotomy Outcomes for Patients with Epileptic Spasms or Tonic Spasms. Pediatr. Neurol. 2019, 95, 79–83.
- Honda, R.; Baba, H.; Adachi, K.; Koshimoto, R.; Ono, T.; Toda, K.; Tanaka, S.; Baba, S.; Yamasaki, K.; Yatsuhashi, H. Developmental Outcome After Corpus Callosotomy for Infants and Young Children with Drug-Resistant Epilepsy. Epilepsy Behav. 2021, 117, 107799.
- Iwasaki, M.; Uematsu, M.; Sato, Y.; Nakayama, T.; Haginoya, K.; Osawa, S.; Itabashi, H.; Jin, K.; Nakasato, N.; Tominaga, T. Complete remission of seizures after corpus callosotomy. J. Neurosurg. Pediatr. 2012, 10, 7–13.
- Graham, D.; Gill, D.; Dale, R.C.; Tisdall, M.M. Corpus Callosotomy Outcomes Study Group. Seizure outcome after corpus callosotomy in a large paediatric series. Dev. Med. Child Neurol. 2018, 60, 199–206.
- Hur, Y.J.; Kang, H.C.; Kim, D.S.; Choi, S.R.; Kim, H.D.; Lee, J.S. Uncovered primary seizure foci in Lennox-Gastaut syndrome after corpus callosotomy. Brain Dev. 2011, 33, 672–677.
- Iwasaki, M.; Uematsu, M.; Hino-Fukuyo, N.; Osawa, S.; Shimoda, Y.; Jin, K.; Nakasato, N.; Tominaga, T. Clinical profiles for seizure remission and developmental gains after total corpus callosotomy. Brain Dev. 2016, 38, 47–53.
- Kobayashi, K.; Endoh, F.; Toda, Y.; Oka, M.; Baba, H.; Ohtsuka, Y.; Yoshinaga, H. Occurrence of bilaterally independent epileptic spasms after a corpus callosotomy in West syndrome. Brain Dev. 2016, 38, 132–135.
- Stigsdotter-Broman, L.; Olsson, I.; Flink, R.; Rydenhag, B.; Malmgren, K. Long-term follow-up after callosotomy—A prospective, population based, observational study. Epilepsia 2014, 55, 316–321.
- Camfield, P.; Camfield, C. Long-term prognosis for symptomatic (secondarily) generalized epilepsies: A population-based study. Epilepsia 2007, 48, 1128–1132.
- Graham, D.; Tisdall, M.M.; Gill, D. Corpus Callosotomy Outcomes in Pediatric Patients: A Systematic Review. Epilepsia 2016, 57, 1053–1068.
- Horsley, V. British Medical Association. Br. Med. J. 1886, 2, 670–677.
- Snead, O.C., 3rd. Surgical Treatment of Medically Refractory Epilepsy in Childhood. Brain Dev. 2001, 23, 199–207.
- Go, C.; Snead, O.C., 3rd. Pharmacologically Intractable Epilepsy in Children: Diagnosis and Preoperative Evaluation. Neurosurg. Focus 2008, 25, E2.
- Consales, A.; Casciato, S.; Asioli, S.; Barba, C.; Caulo, M.; Colicchio, G.; Cossu, M.; de Palma, L.; Morano, A.; Vatti, G.; et al. The Surgical Treatment of Epilepsy. Neurol. Sci. 2021, 42, 2249–2260.
- Luders, H.O. Textbook of Epilepsy Surgery, 1st ed.; CRC Press: Boca Raton, FL, USA, 2008.
- Zentner, J. Surgical Treatment of Epilepsies: Diagnosis, Surgical Strategies, Results, 1st ed.; Springer: Cham, Switzerland, 2020.
- Costello, D.J.; Shields, D.C.; Cash, S.S.; Eskandar, E.N.; Cosgrove, G.R.; Cole, A.J. Consideration of epilepsy surgery in adults should be independent of age. Clin. Neurol. Neurosurg. 2009, 111, 240–245.
- Iimura, Y.; Jones, K.; Takada, L.; Shimizu, I.; Koyama, M.; Hattori, K.; Okazawa, Y.; Nonoda, Y.; Asano, E.; Akiyama, T.; et al. Strong Coupling Between Slow Oscillations and Wide Fast Ripples in Children with Epileptic Spasms: Investigation of Modulation Index and Occurrence Rate. Epilepsia 2018, 59, 544–554.
- Iimura, Y.; Jones, K.; Hattori, K.; Okazawa, Y.; Noda, A.; Hoashi, K.; Nonoda, Y.; Asano, E.; Akiyama, T.; Go, C.; et al. Epileptogenic high-frequency oscillations skip the motor area in children with multilobar drug-resistant epilepsy. Clin. Neurophysiol. 2017, 128, 1197–1205.




